By regularly engaging with PN NCLEX Questions students can stay updated on current evidence-based practices in nursing.
NCLEX Preoperative Care Questions - NCLEX Questions on Preoperative Care
Preoperative Care NCLEX Practice Questions
Question 1.
A nurse is responsible for obtaining informed consent from a client before surgery. Which of the following procedure is correct regarding obtaining informed consent?
(a) Surgeon explains surgery and answers questions.
(b) Minors may need parent/guardian to sign consent.
(c) Older clients may need legal guardian to sign consent.
(d) Psychiatric clients can refuse treatment until legally determined unable to decide.
(e) No sedation before client signs consent.
(f) Phone consent from legal guardian/POA acceptable with witness.
(g) Nurse ensures client understands surgery before signing consent.
(h) Nurse documents witnessed consent after client acknowledges understanding.
Answer:
(g) Nurse ensures client understands surgery before signing consent.
(h) Nurse documents witnessed consent after client acknowledges understanding.
Explanation:
option (g) is incorrect because the nurse, not the surgeon, is responsible for obtaining the client's signature on the consent form. option (h) is correct because the nurse may witness the client's signing of the consent form, but the nurse must be sure that the client has understood the surgeon's explanation of the surgery. The nurse must ensure that the client is fully informed about the procedure and that the client's consent is given voluntarily.
option (a) is correct because the nurse needs to document the witnessing of the signing of the consent form alter the client acknowledges understanding the procedure. Documentation is important to ensure that the client's informed consent is properly recorded in the medical record. option (b) is incorrect because minors may need parental or legal guardian consent, but this is not a statement made by the nurse about obtaining informed consent.
option (c) is incorrect because this is also not a statement made by the nurse about obtaining informed consent. option (d) is incorrect because this statement is about the right of psychiatric clients to refuse treatment and is not related to obtaining informed consent. option (e) is incorrect because sedation should not be administered before the client signs the consent form.
option (f) is partially correct because obtaining telephone consent from a legal guardian or power of attorney for healthcare is an acceptable practice if clients are unable to give consent themselves. However, the nurse must engage another nurse as a witness to the consent given over the telephone.
Question 2.
A nurse is preparing to administer medication to a patient with a history of severe allergic reactions. The medication prescribed is penicillin, which the patient has not received before. The nurse has already obtained the medication from the pharmacy and is now reviewing the steps for medication administration.
Which of the following statements made by the nurse is correct?
(a) The nurse should administer the medication as quickly as possible to ensure it takes effect.
(b) The nurse should not administer the medication to the patient due to the risk of an allergic reaction.
(c) The nurse should closely monitor the patient for any signs of an allergic reaction after administering the medication.
(d) The nurse does not need to obtain informed consent from the patient since the medication is not a high-risk drug.
Answer:
(c) The nurse should closely monitor the patient for any signs of an allergic reaction after administering the medication.
Explanation:
(a) The nurse should not rush to administer the medication as quickly as possible. Instead, the nurse should take time to review the medication order, verify the patient's identity, and check the medication for accuracy and expiration date. Rushing through the medication administration process can lead to errors and adverse events. (b) While it is true that the patient has a history of severe allergic reactions, the nurse should not automatically withhold medication based on this information.
Instead, the nurse should assess the patient's current condition and consider any potential benefits and risks of administering the medication. If the medication is deemed necessary, the nurse should closely monitor the patient for any adverse reactions. (c) This statement is correct. Since the patient has a history of severe allergic reactions and is receiving a medication to which they have not been exposed before, the nurse should closely monitor the patient for any signs of an allergic reaction.
The nurse should remain with the patient for at least 30 minutes after administering the medication to observe for any adverse effects. (d) This statement is incorrect. Even though penicillin is not considered a high-risk drug, informed consent is still required before administering any medication. The nurse should explain the purpose, potential risks, benefits, and alternatives to the medication to the patient or their legal guardian before obtaining informed consent.
Question 3.
A nurse is preparing a client for surgery and must obtain informed consent, review nutrition guidelines, address elimination needs, clean the surgical site, and provide preoperative teaching.
Which of the following statements from the patient indicates that they understand the surgical procedure and have given informed consent?
(a) “I signed the consent form, but I'm not sure what the surgery is for.”
(b) “The nurse explained the surgery to me, and I understand what it involves.”
(c) “I don’t want to have the surgery, but my family is making me do it.”
(d) “I didn’t sign anything yet, but the surgeon told me I need this surgery.”
Answer:
(b) “The nurse explained the surgery to me, and I understand what it involves.”
Explanation:
Informed consent is a process in which the client has been provided with information regarding the risks and benefits of the procedure, as well as any alternative options. The client must understand this information and be able to make a voluntary decision to proceed with the procedure. Therefore, the correct statement is (b) indicating that the patient understands the surgery and has given informed consent.
Question 4.
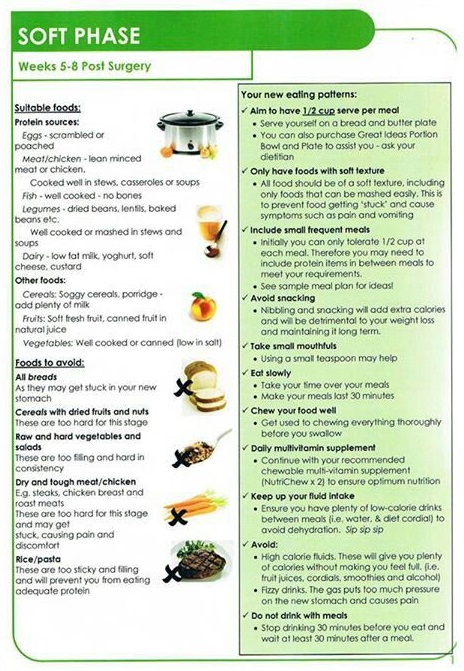
Which of the following statements given by the nurse regarding nutrition before surgery' is incorrect?
(a) “Review the surgeon’s prescriptions regarding the NPO (nothing by mouth) status before surgery."
(b) “Withhold solid foods and liquids as prescribed to avoid aspiration, usually for 6 to 8 hours before general anesthesia and for approximately 3 hours before surgery with local anesthesia (as prescribed).”
(c) “Insert an intravenous (IV) line and administer IV fluids, if prescribed; per agency policy, the IV catheter size should be large enough to administer blood products if they are required.”
(d) “Offer a large meal to the client immediately before surgery to ensure adequate energy for the procedure.”
Answer:
(d) “Offer a large meal to the client immediately before surgery to ensure adequate energy for the procedure.”
Explanation:
Before surgery, the client should be NPO for a specified amount of time to prevent aspiration during anesthesia. The nurse should review the surgeon's prescriptions regarding the NPO status and withhold solid foods and liquids as prescribed.
The nurse should also insert an IV line and administer IV fluids if prescribed, with the IV catheter size being large enough to administer blood products if required. Option (d) is incorrect, as offering a large meal immediately before surgery would increase the risk of aspiration during anesthesia.
Question 5.
Which of the following statements regarding elimination before surgery is incorrect?
(a) "If the client is to have intestinal or abdominal surgeiy, per surgeon’s preference an enema, laxative, or both may be prescribed for the day or night before surgery.”
(b) “The client should void immediately before surgery .”
(c) "Insert an indwelling urinary catheter, if prescribed; urinary catheter collection bags should be emptied immediately before surgeiy, and the nurse should document the amount and characteristics of the urine.”
(d) “Administer a sedative to the client to prevent anxiety and promote relaxation before surgery."
Answer:
(d) “Administer a sedative to the client to prevent anxiety and promote relaxation before surgery.”
Explanation:
Before surgery, the client may need to have an enema, laxative, or both, per the surgeon’s preference. The client should also void immediately before surgery and an indwelling urinary catheter may be inserted if prescribed.
Urinary catheter collection bags should be emptied immediately before surgery, and the nurse should document the amount and characteristics of the urine. Option (d) is incorrect, as no sedation should be administered to the client before they sign the consent form.
Question 6.
A 60-year-old patient is scheduled to undergo abdominal surgery. The nurse provides instructions to the patient regarding preoperative care. The nurse instructs the patient on deep-breathing and coughing exercises, incentive spirometry, leg and foot exercises, and splinting the incision. The nurse also provides instructions on postoperative care and the importance of early ambulation.
Which of the following statements from the patient indicates that the patient has understood the instructions on incentive spirometry?
(a) "I will inhale through my nose and exhale through my mouth."
(b) "I will hold my breath for 10 seconds after inhaling."
(c) "I will place the mouthpiece loosely in my mouth."
(d) "I will inhale slowly to raise the flow rate indicator and hold my breath for 5 seconds."
Answer:
(d) "I will inhale slowly to raise the flow rate indicator and hold my breath for 5 seconds."
Explanation:
The correct answer is (d) because it accurately describes the steps for using incentive spirometry. Incentive spirometry is a device used to encourage deep breathing and prevent respiratory complications after surgery. The device measures the amount of air the patient inhales and helps them achieve maximal inspiration.
The patient is instructed to inhale slowly through the mouthpiece and raise the flow rate indicator. The patient should then hold their breath for 5 seconds and exhale through pursed lips. Options (a), (b) and (c) are incorrect because they do not accurately describe the steps for using incentive spirometry.
Question 7.
A 45-year-old female patient is scheduled for abdominal surgery in the morning. The nurse is providing preoperative teaching to the patient. Which of the following statements from the patient indicates that she understands the instructions for deep-breathing and coughing exercises?
(a) "I should take three deep breaths and then cough three times, holding the third breath for 3 seconds before coughing."
(b) "I should inhale through my mouth and exhale through my nose."
(c) "I only need to perform the exercises once every 4 hours."
(d) "I should lie flat in bed while performing the exercises."
(e) "I should only perform the exercises while lying on my side."
(f) "I should exhale forcefully during the coughing part of the exercise."
(g) "I should perform the exercises for 5 minutes every' hour."
(h) "I should cough first and then take three deep breaths."
Answer:
(a) "I should take three deep breaths and then cough three times, holding the third breath for 3 seconds before coughing."
(f) "I should exhale forcefully during the coughing part of the exercise."
(h) "I should cough first and then take three deep breaths."
Explanation:
(a) This statement indicates that the patient understands the correct sequence of the deep-breathing and coughing exercises and the correct duration of holding the third breath before coughing. (f) . This statement indicates that the patient understands the importance of exhaling forcefully during the coughing part of the exercise to promote the removal of secretions from the lungs. (h).
This statement indicates that the patient understands the incorrect sequence of the deep-breathing and coughing exercises and the need to cough after taking three deep breaths. (b), (c), (d), (e), (g). These options are incorrect because they contain incorrect information about the deep-breathing and coughing exercises or the frequency or position of performing the exercises.
Question 8.
Mr. Ranjan is a 58-year-old man who is scheduled for elective surgery. He has a medical history of type 2 diabetes, hypertension, and chronic obstructive pulmonary disease (COPD). During the preoperative assessment, the nurse asks Mr. Ranjan about his medical conditions and any medications he is currently taking. Which of the following statements from the patient indicates that he may be at increased risk during surgery?
(a) "I have a history of bleeding disorders like thrombocytopenia or hemophilia."
(b) "I have been diagnosed with type 2 diabetes.”
(c) "I suffer from chronic pain."
(d) "I had a heart attack a year ago."
(e) "I have obstructive sleep apnea."
(f) "I currently have an upper respiratory infection."
(g) "I have liver disease."
(h) "I am running a fever."
(i) "I have chronic respiratory disease like emphysema, bronchitis, or asthma."
(j) "I have an immunological disorder like leukemia, HIV, or bone marrow' depression."
(k) "I use street drugs regularly."
Answer:
(a) "I have a history of bleeding disorders like thrombocytopenia or hemophilia."
(b) "I have been diagnosed with type 2 diabetes.”
(e) "I have obstructive sleep apnea."
Explanation:
(a) "I have a history of bleeding disorders like thrombocytopenia or hemophilia." This statement indicates that the patient may have a bleeding disorder, which increases the risk of bleeding during surgeiy.
(b) "I have been diagnosed with type 2 diabetes." Diabetes increases the risk of infections and delayed wound healing, which can lead to postoperative complications.
(e) "I have obstructive sleep apnea." Obstructive sleep apnea increases the risk of airway obstruction and respiratory complications during and after surgery.
(c) "I suffer from chronic pain." Chronic pain is not necessarily a risk factor for surgery, but it can complicate pain management during and after surgery.
(d) "I had a heart attack a year ago." A recent myocardial infarction is a significant risk factor for surgery, but the patient reports that the heart attack was a year ago.
(f) "I currently have an upper respiratory infection." Active respiratory infection can increase the risk of respirator complications during and after surgery.
(g) "I have liver disease." Liver disease can affect the metabolism of drugs used during surgery and increase the risk of bleeding.
(h) "I am running a fever." Active fever can indicate an underlying infection and increase the risk of complications during and after surgery.
(i) "I have chronic respiratory disease like emphysema, bronchitis, or asthma." Chronic respirator}' disease can increase the risk of respiratory complications during and after surgery.
(j) "I have an immunological disorder like leukemia, HIV, or bone marrow depression." Immunological disorders can increase the risk of infections and affect wound healing, which can lead to postoperative complications.
(k) "I use street drugs regularly." Drug abuse can affect the patient's overall health and increase the risk of anesthesia-related complications during and after surgery. It can also lead to poor wound healing and increase the risk of infections.
Question 9.
Mrs. Vimal is a 62-year-old woman who has been experiencing shortness of breath, chest pain, and fatigue. She has a history of chronic respiratory disease, specifically emphysema, and also suffers from type 2 diabetes. Her doctor recommends surgery to improve her breathing, but he is concerned about her medical conditions that could increase her risk during surgery.
Which of the following statements from Mrs. Vimal indicates that she is at an increased risk during surgery'?
(a) "I've been feeling pretty good lately, not too many symptoms."
(b) "I've been taking my diabetes medication regularly."
(c) "I stopped smoking a year ago."
(d) "Sometimes I have trouble breathing when I lay down at night."
Answer:
(d) "Sometimes I have trouble breathing when I lay down at night."
Explanation:
Mrs. Vimal's chronic respiratory' disease, specifically emphysema, is a medical condition that increases her risk during surgery. Option (d) shows that she has trouble breathing when she lays down at night, indicating that she may have obstructive sleep apnea, which further increases her risk during surgery. Options (a), (b), and (c) are incorrect because they do not provide any information about Mrs. Vimal's medical conditions that increase her risk during surgery.
Question 10.
Mr. Vimal is a 55-year-old man who is scheduled for elective surgery. During the pre-operative assessment, the nurse asks him about his medication history. Mr. Vimal reports that he takes clopidogrel for his heart condition. Which of the following statements from Mr. Vimal indicates that he understands the nurse's instructions regarding his medication?
(a) "I'll stop taking clopidogrel for 2 days before surgery'."
(b) "I'll stop taking clopidogrel for 5 days before surgery."
(c) "I'll continue taking clopidogrel until the day of surgery."
(d) "I'll stop taking clopidogrel after the surgery."
Answer:
(b) "I'll stop taking clopidogrel for 5 days before surgery."
Explanation:
Clopidogrel is an antiplatelet medication that can increase the risk of bleeding during surgery. Therefore, it is recommended that it be discontinued at least 5 days before surgery to decrease the risk of bleeding. Option (a) is incorrect because stopping clopidogrel for only 2 days is not sufficient to reduce the risk of bleeding.
Option (c) is incorrect because continuing clopidogrel until the day of surgery increases the risk of bleeding. Option (d) is incorrect because stopping clopidogrel after the surgery is unnecessary since it is the pre-operative period during which the medication needs to be discontinued.
Question 11.
Samantha is a 62-year-old woman scheduled for surgery to remove a benign tumor in her abdomen. During the pre-operative interview. Samantha mentions that she takes aspirin daily for her arthritis. What should the nurse do in response to this information?
(a) Discontinue aspirin at least 48 hours before surgery
(b) Consult with the surgeon about discontinuing aspirin
(c) Instruct Samantha to continue taking aspirin until the day of surgery
(d) Explain to Samantha that aspirin will not affect her surgery
Answer:
(b) Consult with the surgeon about discontinuing aspirin
Explanation:
Aspirin is a commonly used medication that can alter platelet aggregation, increasing the risk of bleeding during surgery. Therefore, it is recommended to discontinue aspirin at least 48 hours before surgery, as specified by the surgeon. Option (a) is partially correct, as it mentions discontinuing aspirin, but it does not include consulting with the surgeon.
Option (c) is incorrect, as it advises Samantha to continue taking aspirin, which could increase her risk of bleeding during surgery. Option (d) is also incorrect, as aspirin can affect the outcome of the surgery, and it is important to discuss this with the surgeon. Therefore, option (b) is the correct answer, as it emphasizes the importance of consulting with the surgeon about discontinuing aspirin before surgery.
Question 12.
Which of the following statements from the patient indicates that they are at risk of bleeding during surgery?
(a) "I have been taking aspirin for my arthritis for the past week."
(b) "I take medication for my high blood pressure every day."
(c) "I have been taking an herbal supplement for my anxiety."
(d) "I have a history of seizures and take medication for it."
Answer:
(a) "I have been taking aspirin for my arthritis for the past week."
Explanation:
Aspirin is a medication that can alter platelet aggregation, and therefore increase the risk of bleeding during surgery. It should be discontinued at least 48 hours before surgery. Option (b) is incorrect because while antihypertensive medications can interact with anesthetic agents and cause bradycardia, hypotension, and impaired circulation, they do not increase the risk of bleeding.
Option (c) is incorrect because while herbal substances can interact with anesthesia and cause adverse effects, they do not necessarily increase the risk of bleeding. Option (d) is incorrect because while long-term use of certain anticonvulsants can alter the metabolism of anesthetic agents, they do not necessarily increase the risk of bleeding.
Question 13.
Which of the following statements from the patient indicates that they may be at an increased risk of bleeding during surgery?
(a) "I take antibiotics daily for a chronic infection."
(b) "I take a medication for my high blood pressure."
(c) "I take aspirin daily to prevent heart attacks."
(d) "I take antidepressants for my depression."
(e) "I take a diuretic for my edema."
(f) "I take insulin for my diabetes."
(g) "I take an herbal supplement for my anxiety."
(h) "I take a medication for my irregular heartbeat."
(I) "I take a medication for my epilepsy."
Answer:
(c) "I take aspirin daily to prevent heart attacks.", (h) "I take a medication for my irregular heartbeat.", and (I) "I take a medication for my epilepsy."
Explanation:
Option (c) The use of acetylsalieylic acid (Aspirin), clopidogrel, and nonsteroidal anti-inflammatory drugs can alter platelet aggregation and increase the risk of bleeding during surgery. Option (h) Antidysrhythmic medications, such as those used to treat an irregular heartbeat, can reduce cardiac contractility and impair cardiac conduction during anesthesia, which can increase the risk of bleeding during surgery.
Option (I) Long-term use of certain anticonvulsants can alter the metabolism of anesthetic agents and increase the risk of bleeding during surgery. The other options may have an impact on the client's surgical outcome, but they do not directly increase the risk of bleeding during surgery.
Question 14.
Mrs. Jones has just had a cholecystectomy (gallbladder removal) and is being discharged from the hospital. The nurse is providing her with postoperative discharge teaching. Which statement from the patient indicates that the nurse's teaching on postoperative care was effective?
(a) "I should cover my incision with plastic when showering."
(b) "I can resume lifting heavy objects after 2 weeks."
(c) "I only need to see the surgeon again if I have a problem."
(d) "It's normal for the skin around the staples to turn black."
(e) "I don't need to drink any liquids for the next few days."
(f) "I can resume normal activities immediately after surgery."
(g) "I don’t need to take my pain medication unless I feel really bad."
Answer:
(a) "I should cover my incision with plastic when showering."and (c) "I only need to see the surgeon again if I have a problem."
Explanation:
Option (a) is correct because it shows that the patient has understood the instructions to cover the incision with plastic when showering to prevent it from getting wet. This is important for proper wound care to prevent infection. Option (c) is also correct because it shows that the patient has understood the importance of recognizing the signs and symptoms of complications and when to call the surgeon. This is important for timely intervention and prevention of serious postoperative complications.
Option (b) is incorrect because the patient should avoid lifting heavy objects for at least 6 weeks after a major surgical procedure, as lifting can cause strain on the incision site and delay the healing process. Option (d) is incorrect because it is not normal for the skin around the staples to turn black. It could be a sign of infection and should be reported to the surgeon.
Option (e) is incorrect because it is important for the patient to stay hydrated after surgery to promote healing and prevent complications such as constipation and dehydration. Option (f) is incorrect because the patient should gradually resume normal activities and avoid strenuous physical activities for a few weeks after surgery. Option (g) is incorrect because it is important for the patient to take their pain medication as prescribed to manage postoperative pain and promote healing.’
Question 15.
Which of the following statements from the nurse indicates that the client has been appropriately instructed on postoperative discharge teaching?
(a) "I have provided you with a 24-hour supply of dressings for home use."
(b) "You can resume your normal activities immediately after surgery."
(c) "Sutures are usually removed in the surgeon's office 7 to 14 days after surgery."
(d) "You do not need to worry about any signs and symptoms of complications."
Answer:
(c) "Sutures are usually removed in the surgeon's office 7 to 14 days after surgery."
Explanation:
Option (c) is the correct answer as it provides the client with the appropriate information about the time frame for removal of sutures. Options (a) and (b) are incorrect as they provide inaccurate information that may lead to complications. Option (d) is incorrect as it does not provide the client with important information about potential complications and when to seek medical attention.
Also Read: