RN NCLEX Questions focus on client care, health promotion, disease prevention, and the nursing process.
NCLEX Ingestion, Nutrition, or Diet Health Problems Questions
Ingestion, Nutrition, or Diet Health Problems NCLEX Practice Questions
Question 1.
A toddler is brought to the emergency department after ingesting an undetermined amount of drain cleaner. The nurse should expect to assist with which intervention first?
(a) administering an emetic
(b) securing the airway
(c) performing gastric lavage
(d) inserting an indwelling urinary catheter
Answer:
(b) securing the airway
Explanation:
Drain cleaner almost always contains lye, which can burn the mouth, pharynx, and esophagus on ingestion. The nurse would be prepared to assist with procedures to secure the airway, which may include intubation or performing a tracheostomy. An emetic is contraindicated because, as the substance burns on ingestion, so too would it burn when vomiting.
Additionally, the mucosa becomes necrotic, and vomiting could lead to perforations. Gastric lavage is contraindicated because the mucosa is burned from the ingestion of the caustic lye, causing necrosis. Gastric lavage also could lead to perforation of the necrotic mucosa. Insertion of an indwelling urinary catheter would be indicated after the measures to remove the caustic substance have been started.
Question 2.
After the acute stage following an ingestion of drain cleaner by a child, the nurse should be alert for the development of which likely complication?
(a) tracheal stenosis
(b) tracheal varices
(c) esophageal strictures
(d) esophageal diverticula
Answer:
(c) esophageal strictures
Explanation:
As the burn from the lye ingestion heals, scar tissue develops and can lead to esophageal strictures, a common complication of lye ingestion. Tracheal stenosis would occur if the child had vomited and aspirated. Tracheal varices do not commonly occur after the ingestion of lye or other substances. Although very rare, esophageal diverticula may occur. Diverticula are commonly found in the colon of adults.
Question 3.
The parents of a preschooler suspect that the child has recently ingested a large amount of acetaminophen. The child does not appear in immediate distress. The nurse should anticipate doing which intervention in order of priority, from first to last?
All options must be used.
(a) Draw acetaminophen serum levels.
(b) Determine the time and amount of drug ingested,
(c) Administer acetylcysteine IV.
(d) Administer activated charcoal.
Answer:
(b) Determine the time and amount of drug ingested,
(d) Administer activated charcoal.
(a) Draw acetaminophen serum levels.
(c) Administer acetylcysteine IV.
Explanation:
(b), (d), (a), (c) The nurse should first attempt to determine exactly when and how much acetaminophen the parents think the child has taken. Determining the time of ingestion helps establish the immediate care and when lab values should be drawn. Gastric decontamination with activated charcoal is used within 4 hours of ingestion to bind the drug and help prevent toxic serum levels.
Serum blood levels should be done after the gastric decontamination, but preferably not too soon after ingestion since levels drawn before 4 hours may not reflect maximum serum concentrations and will need to be repeated. The decision to administer acetylcysteine and prevent liver damage is based on serum levels.
Question 4.
When developing the plan of care for a toddler who has taken an acetaminophen overdose, which intervention should the nurse expect to include as part of the initial treatment?
(a) frequent serum drug levels
(b) gastric lavage
(c) tracheostomy
(d) electrocardiogram
Answer:
(b) gastric lavage
Explanation:
Initial management of a child who has ingested a large amount of acetaminophen would include inducing vomiting or performing gastric lavage with or without activated charcoal to aid in the removal of the substance. Frequent blood level determinations may be obtained during the followup phase, but they are not done as part of the initial treatment.
Tracheostomy is not typically part of the initial treatment for acetaminophen overdose. However, it may be necessary later if respiratory distress develops. Acetaminophen primarily affects the liver, not the heart. Therefore, an electrocardiogram would not be considered part of the initial treatment plan.
Question 5.
While assessing a preschooler brought by her parents to the emergency department after ingestion of kerosene, the nurse should be alert for which complication?
(a) uremia
(b) hepatitis
(c) carditis
(d) pneumonitis
Answer:
(d) pneumonitis
Explanation:
Chemical pneumonitis is the most common complication of ingestion of hydrocarbons, such as in kerosene. The pneumonitis is caused by irritation from the hydrocarbons aspirated into the lungs. Uremia is the result of renal insufficiency, which causes nitrogenous waste products to build up in the blood rather than being excreted. Hepatitis is caused by a viral infection. Carditis in a preschooler may be the result of rheumatic fever.
Question 6.
Which statement by the parent of an 18-month-old child most indicates to the nurse that the child needs laboratory testing for lead levels?
(a) “My child does not always wash after playing in the dirt.”
(b) “My child drinks two cups of milk every day.”
(c) “My child has more temper tantrums than other kids.”
(d) “My child is smaller than other kids of the same age.”
Answer:
(a) “My child does not always wash after playing in the dirt.”
Explanation:
Eating with dirty hands, especially after playing outside, can cause lead poisoning because lead is often present in soil surrounding homes. Also, children who eat lead-containing paint chips commonly develop lead poisoning. Milk is a major source of calcium, and diets high in calcium help prevent lead poisoning.
Temper tantrums are characteristic of 18-month-old children as they try to assert themselves. Determining whether the child is smaller than other children the same age requires measuring height and weight and plotting them on growth charts. In addition, inadequate growth could be a result of numerous causes, such as genetics, chronic illness, or chronic drug use (e.g., prednisone).
Question 7.
In an initial screening for lead poisoning, a toddler is found to have a minimally elevated lead level. What is the most important action the nurse should take?
(a) Arrange a follow-up appointment in 6 months.
(b) Obtain a consultation for chelation therapy.
(c) Educate parents on ways to reduce lead in the environment.
(d) Assure the parents this is not an unexpected finding.
Answer:
(c) Educate parents on ways to reduce lead in the environment.
Explanation:
Treatment for children with minimally elevated lead levels should include family lead education, follow-up testing, and a social service consultation if needed. Waiting 6 months for a follow-up screening is too long because the effects of lead are irreversible. Oral chelation therapy is not begun until levels approach high levels, 45 mcg/dL (2.2 pmol/L). There is no such thing as a “normal” lead level because there is no beneficial action in the body.
Question 8.
When teaching the mother of a toddler diagnosed with lead poisoning, what should the nurse include as the most serious complication if the condition goes untreated?
(a) liver cirrhosis
(b) stunted growth
(c) neurologic deficits
(d) heart failure
Answer:
(c) neurologic deficits
Explanation:
The most serious and irreversible consequence of lead poisoning is neurologic changes leading to an intellectual disability. It can be expected if lead poisoning is long-standing and goes untreated. Lead poisoning also affects the hematologic and renal systems. Cirrhosis is the end stage of several chronic liver diseases, such as biliary atresia and hepatitis. Lead poisoning is not associated with stunted growth. Chronic illnesses, such as cystic fibrosis, cause slowing of the growth velocity. Heart failure is associated with congenital heart disease and rheumatic fever.
Question 9.
The nurse is teaching dietary interventions to the parents of a child with an elevated blood lead level (EBLL). The nurse recognizes the need for more teaching when the parent makes which statement?
(a) “Diets high in calcium help prevent lead from depositing in the body.”
(b) “The body is less likely to absorb lead if iron intake is high.”
(c) “Adequate intake of vitamin A helps keep lead out of fatty tissues.”
(d) “Vitamin C deficiencies increase the risk of lead toxicity.”
Answer:
(c) “Adequate intake of vitamin A helps keep lead out of fatty tissues.”
Explanation:
Vitamin A is not known to play a significant role in preventing EBLL. Calcium intake inhibits lead absorption. Children with EBLL levels often are anemic. While this relationship is not well understood, iron supplementation has been shown to improve developmental outcomes. Vitamin C improves iron absorption. Increased vitamin intake is associated with decreased EBLL levels.
Question 10.
The nurse is conducting a health history on a school-age child. Which parent statement would suggest to the nurse that a child may have celiac disease?
(a) “His urine is so dark in color.”
(b) “His stools are large and smelly.”
(c) “His belly is so small.”
(d) “He is so short.”
Answer:
(b) “His stools are large and smelly.”
Explanation:
Celiac disease is a disorder involving intolerance to the protein gluten, which is found in wheat, rye, oats, and barley. The stools of a child with celiac disease are characteristically malodorous, pale, large (bulky), and soft (loose). Excessive flatus is common, and bouts of diarrhea may occur. Dark urine is commonly associated with concentrated urine, such as when a child has dehydration. The belly of a child with celiac disease, a malabsorption disorder, typically is protuberant. A small belly may be associated with a child who is thin. Short stature is not associated with this malabsorption disorder.
Question 11.
During the assessment of a child with celiac disease, the nurse would most likely note which physical finding.
(a) enlarged liver
(b) protuberant abdomen
(c) tender inguinal lymph nodes
(d) periorbital edema
Answer:
(b) protuberant abdomen
Explanation:
The intestines of a child with celiac disease fill with accumulated undigested food and flatus, causing the characteristic protuberant abdomen. Celiac disease is not usually associated with any liver dysfunction, including poor liver functioning leading to liver enlargement. Tender inguinal lymph nodes are often associated with an infection. Periorbital edema, swelling around the eyes, is associated with nephritis.
Question 12.
The nurse is teaching the parent of a child with celiac disease about dietary management. Which statement by the parent indicates successful teaching?
(a) “I will feed my child foods that contain wheat products.”
(b) “I will be sure to give my child lots of milk.”
(c) “I will plan to feed my child foods that contain rice.”
(d) “I will be sure my child gets oatmeal every day.”
Answer:
(c) “I will plan to feed my child foods that contain rice.”
Explanation:
Damage to intestinal mucosa in celiac disease is caused by gliadin, a part of the gluten protein found in wheat, rye, barley, and oats. Foods containing these grains must be eliminated entirely from the diet of children with celiac disease. Foods containing rice and corn are a good substitute. Although an adequate intake of milk is important for any child, children with celiac disease do not need an increased milk intake.
Question 13.
The nurse is teaching the parent of a preschool-age child with celiac disease about a gluten-free diet. The nurse determines that teaching has been successful when the parent tells the nurse she will prepare which breakfast for the child?
(a) eggs and orange juice
(b) wheat toast and grape jelly
(c) oatmeal and skim milk
(d) rye toast and peanut butter
Answer:
(a) eggs and orange juice
Explanation:
Children with celiac disease cannot digest the protein in common grains such as wheat, rye, and oats. Eggs and orange juice would be appropriate foods.
Question 14.
Which foods would be appropriate for a 12-month-old child with celiac disease?
(a) oatmeal
(b) pancakes
(c) rice cereal
(d) waffles
Answer:
(c) rice cereal
Explanation:
The child with celiac disease should not eat foods containing wheat, oats, rye, or barley. Pancakes and waffles are made from flour that typically is derived from wheat and therefore should be avoided. Foods containing rice, such as rice cereal, or corn are appropriate. Pancakes and waffles are made from flour that typically is derived from wheat and therefore should be avoided.
Question 15.
The parent of a child with celiac disease asks, “How long must he stay on this diet?” Which response by the nurse is best?
(a) “Until the jejunal biopsy is normal.”
(b) “Until his stools appear normal.”
(c) “For the next 6 months.”
(d) “For the rest of his life.”
Answer:
(d) “For the rest of his life.”
Explanation:
Most children with celiac disease have a lifelong sensitivity to gluten, which requires that they maintain some type of diet restriction for the rest of their lives.

Question 16.
When preparing to obtain a neonatal screen¬ing test for phenylketonuria (PKU), the nurse understands that the neonate must have been fed what to ensure reliable results?
(a) a feeding of an iron-rich formula
(b) nothing by mouth for 4 hours before the test
(c) initial formula or breast milk at least 24 hours before the test
(d) a feeding of glucose water.
Answer:
(c) initial formula or breast milk at least 24 hours before the test
Explanation:
PKU is an autosomal recessive disorder involving the absence of an enzyme needed to metabolize the essential amino acid phenylalanine to tyrosine. To ensure reliable results, the neonate must have ingested sufficient protein, such as breast milk or formula, for at least 24 hours. Testing the infant before that time, excessive vomiting, or poor intake can yield false-negative results. The infant does not need to fast 4 hours before the test. A loading dose of glucose water does not affect test values.
Question 17.
The nurse is assessing children at risk for phe-nylketonuria (PKU). Which child is at greatest risk?
(a) a blond, blue-eyed, fair-skinned child with eczema
(b) an African American, dark-eyed child with asthma
(c) a child with dark complexion who is overweight and has labile personalities
(d) a red-headed child who experiences frequent contact dermatitis
Answer:
(a) a blond, blue-eyed, fair-skinned child with eczema
Explanation:
Infants with PKU are usually blond, blueeyed, and fair and often have eczema. The other physical assessment findings are not typically found in children with PKU.
Question 18.
When developing the plan of care for a child diagnosed with phenylketonuria (PKU), the nurse should establish which goal?
(a) meeting the child’s nutritional needs for optimal growth
(b) ensuring that the special diet is started at age 3 weeks
(c) maintaining serum phenylalanine level higher than 12 mg/100 mL (720 pmol/L)
(d) maintaining serum phenylalanine level lower than 2 mg/100 mL (120 pmol/L)
Answer:
(a) meeting the child’s nutritional needs for optimal growth
Explanation:
The goal of care is to prevent intellectual disabilities by adjusting the diet to meet the infant's nutritional needs for optimal growth. The diet needs to be started upon diagnosis, ideally within a few days of birth. Serum phenylalanine level should be maintained between 3 and 7 mg/100 mL (180 to 420 pmol/L). Significant brain damage usually occurs if the level exceeds 10 to 15 mg/100 mL (600 to 900 pmol/L). If the level drops below 2 mg/100 mL (120 pmol/L), the body begins to catabolize its protein stores, causing growth restriction.
Question 19.
When taking a diet history from the mother of a 7-year-old child with phenylketonuria, a report of an intake of which food should cause the nurse to gather additional information?
(a) diet cola
(b) carrots
(c) orange juice
(d) bananas
Answer:
(a) diet cola
Explanation:
Foods with low phenylalanine levels include vegetables, fruits, and juices. Foods high in phenylalanine include meats and dairy products, which must be restricted or eliminated. Diet colas contain more phenylalanine than the fruits listed.
Question 20.
Which foods would the nurse teach the parents of a child with phenylketonuria (PKU) to avoid? Select all that apply.
(a) hamburger
(b) hot dog
(c) ice cream
(d) juice
(e) cereal
Answer:
(a) hamburger
(b) hot dog
(c) ice cream
Explanation:
(a), (b), (c) Children with PKU lack an enzyme to metabolize phenylalanine and convert it to tyrosine. Treatment is dietary management to control the amount of phenylalanine ingested. Foods with low phenylalanine levels include fruits, most vegetables, and cereals. High-protein foods have high levels of phenylalanine and include meats and dairy products.
Question 21.
When teaching the mother of a child diag¬nosed with phenylketonuria (PKU) about its transmission, the nurse should use knowledge of which factor as the basis for the discussion?
(a) chromosome translocation
(b) chromosome deletion
(c) autosomal recessive gene
(d) X-linked recessive gene
Answer:
(c) autosomal recessive gene
Explanation:
PKU is caused by an inborn error of metabolism. It is an autosomal recessive disorder that inhibits the conversion of phenylalanine to tyrosine. A form of Down syndrome, trisomy 21, is an example of a disorder caused by chromosomal translocation. Cri du chat is an example of a disorder caused by chromosomal deletion. Hemophilia A is an example of a disorder caused by an X-linked recessive gene.
Question 22.
A newborn diagnosed with phenylketonuria (PKU) is placed on a low-phenylalanine formula. The mother asks the nurse how long her infant will need to have dietary restriction. Which response would be most appropriate?
(a) “Your baby needs to stay on low phenylalanine formula until he is taking solid foods well.”
(b) “Once your child has stopped growing he can come off the phenylalanine restricted diet.”
(c) “He can switch to a regular diet when his phenylalanine levels remain normal for 6 months. ”
(d) “Most likely he will need to follow a low phenylalanine diet for the rest of his life.”
Answer:
(d) “Most likely he will need to follow a low phenylalanine diet for the rest of his life.”
Explanation:
Clients with PKU have better cognitive outcomes and long-term health when they remain on a low phenylalanine diet their entire lives. Clients who follow the PKU diet will not get enough essential nutrients from food. They will have to drink a special formula for the rest of their lives, but older children and adults will drink a different formula than infants and toddlers.
Older treatment plans permitted adolescents to come off the diet once they had stopped growing but advised female clients that they had to resume the diet before conception to lower risks to the fetus. It is now understood that rising phenylalanine levels in adolescents and young adults are associated with decreased mental well-being. The safe amount of dietary phenylalanine that clients with PKU can tolerate varies over time. Clients who stay on the diet will need regular phenylalanine monitoring for the rest of their lives.
Question 23.
Even though several teaching sessions have been documented in the client’s health record, the mother asks the nurse again what caused her child’s phenylketonuria (PKU). Which statement would best reflect the nurse’s interpretation of why the mother keeps asking for information that she has already received?
(a) Because the child’s condition is chronic, parents commonly want very detailed explanations about the causes of and treatments for their child’s disease.
(b) Parents of a chronically ill child commonly require a long time to work through the giving process for their child’s disease.
(c) Parents commonly test health workers’ knowledge about the causes of and treatments for their child’s disease.
(d) Parents commonly deal with their guilt about possibly causing their child’s disease by asking challenging questions.
Answer:
(b) Parents of a chronically ill child commonly require a long time to work through the giving process for their child’s disease.
Explanation:
PKU is considered a chronic illness. Parents typically grieve about the loss of health in their child afflicted with a chronic disease. Many times, they repeat questions, as though trying to deny what is really happening. This type of behavior represents an attempt to integrate the experience and their feelings with their self-image as they pass through the grieving process. Asking for detailed explanations, testing the competence of health workers, and expressing impatience with health workers may explain the parents’ behavior, but viewing the behavior as a part of the grieving process is the most plausible explanation.
Question 24.
When performing the nursing history, which information would be most important for the nurse to obtain from the mother of an infant with suspected colic?
(a) the type of formula the infant is taking
(b) the infant’s crying pattern
(c) the infant’s sleep position
(d) the position of the infant during burping
Answer:
(b) the infant’s crying pattern
Explanation:
Information on the crying pattern of the infant is most helpful in confirming the diagnosis of colic. Typically, the colic attack begins abruptly, with the infant crying loudly and continuously, possibly for hours. The attack may end when the child becomes exhausted. The child also may attain some relief after passing stool or flatus. Often, in an attempt to alleviate the infant’s crying, parents try to feed the infant, resulting in overfeeding, leading to discomfort and distention.
Asking about the type of formula, sleep position, or position for burping will not provide sufficient information to confirm the diagnosis of colic. However, the nurse can obtain additional information after determining the nature of the crying pattern.
Question 25.
The parents of a child with colic are asked to describe the infant’s bowel movements. Which description should the nurse expect?
(a) soft, yellow stools
(b) frequent watery stools
(c) ribbon-like stools
(d) foul-smelling stools
Answer:
(a) soft, yellow stools
Explanation:
Infants with colic usually pass normal stools, typically soft and yellowish. Frequent watery stools might indicate diarrhea. Ribbon-like stools are suggestive of a narrowing of the colon or the rectum. Foul-smelling stools by themselves are related to diet. When other symptoms such as large size and protuberant abdomen are present, malabsorption may be possible.

Question 26.
The mother tells the nurse that the diagnosis of colic upsets her because she knows her infant will continue to have colicky pain. Which response by the nurse would be most appropriate?
(a) “I know that your baby’s crying upsets you, but she needs your undivided attention for the next few months.”
(b) “It can be difficult to listen to your baby cry so loud and so long, so try to make sure that you get some free time.”
(c) “It must be distressing to see your baby in pain, but at least she does not have an intestinal obstruction.”
(d) “The next 3 months will be a difficult time for you, but your baby will outgrow the colic by this time.”
Answer:
(b) “It can be difficult to listen to your baby cry so loud and so long, so try to make sure that you get some free time.”
Explanation:
The nurse needs to provide the parents with support because of the infant’s crying. The parents are stressed and need to be encouraged to get out of the house and arrange for some free time. Although infants need lots of attention and care for the first few months, they do not need the mother’s undivided attention. Comparing colic with other problems is inappropriate. Parents have the right to be upset. Although colic usually disappears spontaneously by age 3 months, the nurse should not make any guarantees.
Question 27.
The nurse judges that the mother has understood the teaching about care of an infant with colic when the nurse observes the mother doing which action?
(a) holding the infant prone while feeding
(b) holding the infant in her lap to burp
(c) placing the infant prone after the feeding
(d) burping the infant during and after the feeding
Answer:
(d) burping the infant during and after the feeding
Explanation:
Infants with colic should be burped frequently during and after the feeding. Much of the discomfort of colic appears to be associated with the presence of air in the stomach and the intestines. Frequent burping helps to relieve the air. Infants with colic should be held fairly upright while being fed, to help air rise.
The preferred position for burping the infant with colic is to hold the infant at the mother’s shoulder so that the infant’s abdomen lies on the shoulder. This position causes more pressure to be exerted on the infant’s abdomen, leading to a more forceful burp. The child should be placed in an infant seat after feedings.
Question 28.
An 8-year-old has a body mass index (BMI) for age at the 90th percentile but has no other risk factors. What should the nurse do?
(a) Refer the family to a dietician.
(b) Recommend the child be reweighed in 1 year.
(c) Refer the child to a pediatric weight loss specialist.
(d) Recommend the child participate in a commercial diet program.
Answer:
(a) Refer the family to a dietician.
Explanation:
Children aged 2 to 20 years with a BMI- for-age at the 90th percentile are considered overweight. If no other risk factors are present, the family should receive dietary counseling to slow the child’s weight gain until an appropriate height for weight is attained. Without intervention, the child may become obese. An HCP who specializes in pediatric weight loss should be considered when the child is obese and has complicating factors. Commercial diet programs alone do not include the necessary monitoring for children, thus are rarely appropriate.
Question 29.
A parent brings a 7-month-old infant to the well-baby clinic for a check-up. The parent feeds the infant formula whenever the infant is hungry but is concerned that the infant is overweight. What instructions should the nurse give the parents?
(a) Give the infant 2% milk formula and add vitamins.
(b) Use skim milk because it is high in protein and lower in calories.
(c) Decrease the amount of formula feedings to 16 oz (480 mL) daily and supplement with juice and water.
(d) Bring a 3-day record of the infant’s intake back for further evaluation.
Answer:
(d) Bring a 3-day record of the infant’s intake back for further evaluation.
Explanation:
A 3-day diet history is the best way to accurately assess the child’s intake. Children under age 1 year should not drink cow’s milk because of the risk of allergy. Children over age 1 year should drink whole milk because skim milk and 2% milk do not contain all the essential fatty acids needed by young children. It is unknown at this time how much formula the child is actually taking, but an infant should not have more than 6 oz (177.4 mL) of juice per day, and additional water is usually not necessary. If an infant is taking no more than 32 oz (946 mL) of formula per day and is eating some baby food and cereal, additional fluids and frequent feeding should not be necessary.
Question 30.
The nurse is providing nutrition counseling for an obese adolescent. What is the most effective way for the nurse to obtain a nutrition history from this client?
(a) Ask her what she knows about good nutrition.
(b) Tell her to list what she plans to eat for the next 24 hours.
(c) Ask her what she ate yesterday if it was a typical day.
(d) Telephone her mother and ask her what she ate yesterday.
Answer:
(c) Ask her what she ate yesterday if it was a typical day.
Explanation:
A 24-hour recall history is the best method to obtain a dietary history from an adolescent. Open-ended questions tend not to provide sufficient details for a nutrition history. Asking what the client plans to eat in the future gives the client an opportunity to report the “right” answer. The nurse obtains the information directly from the client; asking the mother has the potential to undermine trust.
Question 31.
When counseling an obese adolescent, the nurse should advise the client that which complication is the most common?
(a) lifelong obesity
(b) gastrointestinal problems
(c) orthopedic problems
(d) psychosocial problems
Answer:
(a) lifelong obesity
Explanation:
The most common complication of adolescent obesity is its persistence into adulthood. The incidence of gastrointestinal and orthopedic problems, such as Legg-Calve-Perthes disease and genu valgum (knock knees), is greater for obese adolescents; however, they are not the most common complication. Although psychosocial problems do occur, they are not the most common complication.
Question 32.
When developing a teaching plan for the mother of an infant about introducing solid foods into the diet, the nurse should expect to include which measure in the plan to help prevent obesity?
(a) decreasing the amount of formula or breast milk intake as solid food intake increases
(b) introducing the infant to the taste of vegetables by mixing them with formula or breast milk
(c) mixing cereal and fruit in a bottle when offering solid food for the first few times
(d) using a large-bowled spoon for feeding solid foods during the first several months
Answer:
(a) decreasing the amount of formula or breast milk intake as solid food intake increases
Explanation:
Decreasing the amount of formula given as the infant begins to take solids helps prevent excess caloric intake. Because the infant is receiving calories from the solid foods, the formula no longer needs to provide the infant’s total caloric requirements. Mixing vegetables with formula or breast milk does not allow the child to become accustomed to new textures or tastes. Solid foods should be given with a spoon, not in a bottle.
Using a bottle with food allows the infant to ingest more food than is needed. Also, the infant needs to learn to eat from a spoon. A small-bowled spoon is recommended for infants because infants have a tendency to push food out with the tongue. The small-bowled spoon helps in placing the food at the back of the infant’s tongue when feeding.
Question 33.
A pregnant mother who has brought her toddler to the clinic for a checkup asks the nurse how she can keep her next baby from becoming obese. The mother plans to bottle-feed her next child. Which information should the nurse include in the teaching plan to help the mother avoid overnourishing her infant?
(a) recognizing clues indicating that the baby is full
(b) establishing a regular feeding schedule
(c) supplementing feedings with sterile water
(d) adding more water than directed when preparing formula
Answer:
(a) recognizing clues indicating that the baby is full
Explanation:
Infants generally do not overeat unless they are urged to do so. Parents should watch for clues indicating that the infant is full for example, stopping sucking and pushing the nipple out of the mouth. Bottle-feeding instead of breastfeeding is more likely to lead to excessive caloric intake. A demand schedule, rather than a regulated sched-ule, allows the infant to regulate intake according to individual needs.
Normally, giving an infant a regular supplementation of water is unnecessary; the infant’s sucking needs can be met by providing a pacifier. Adding more water to the formula than as directed decreases the caloric intake and also places the infant at risk for hyponatremia due to decreased sodium and increased water intake.
Question 34.
During a school party, a child with a known food allergy has an itchy throat, is wheezing, and is not feeling “quite right. ” The nurse should do what in order from first to last? All options must be used.
(a) Administer the child’s epinephrine.
(b) Assess vital signs.
(c) Position to facilitate breathing.
(d) Send someone to activate the Emergency Management Systems(EMS).
(e) Notify the parents.
Answer:
(d) Send someone to activate the Emergency Management Systems(EMS).
(a) Administer the child’s epinephrine.
(b) Assess vital signs.
(c) Position to facilitate breathing.
(e) Notify the parents.
Explanation:
(d), (a), (b), (c), (e) The child is exhibiting signs of anaphylaxis. The principles of emergency management involve activating EMS when an emergency is first realized. The nurse then follows the priorities of Circulation, Airway, Breathing (C, A, B). The epinephrine should then be given to reduce airway constriction and prevent cardiovascular collapse. The child should be assisted into the most comfort-able position to facilitate breathing, usually with the head elevated. Then the nurse can take the child’s vital signs to assess the effectiveness of the treatment. Lastly, the nurse should notify the family.
Question 35.
After teaching the parents of a child with lactose intolerance about the disorder, the nurse deter¬mines that the teaching was effective when the mother uses which statement to describe the condition?
(a) “The lack of an enzyme to break down lactose.”
(b) “An allergy to lactose found in milk.”
(c) “Inability to digest proteins completely.”
(d) “Inability to digest fats completely.”
Answer:
(a) “The lack of an enzyme to break down lactose.”
Explanation:
Lactose intolerance is not an allergy. Rather, it is caused by the lack of the digestive enzyme lactase. This enzyme, found in the intestines, is necessary for the digestion of lactose, the primary carbohydrate in cow’s milk. Protein and fat digestion are not affected.
Question 36.
After teaching the mother of a 2-year-old child with lactose intolerance about which dairy products to include in the child’s diet, the nurse understand that teaching has been effective if the mother states she will include which food?
(a) ice cream
(b) creamed soups
(c) pudding
(d) yogurt
Answer:
(d) yogurt
Explanation:
People who are lactose intolerant usually are able to tolerate dairy products in which lactose has been fermented, such as yogurt, cheese, and buttermilk. Pudding, ice cream, and creamed soups contain lactose that has not been fermented.
Question 37.
The breastfeeding mother of a 1-month-old diagnosed with cow’s milk sensitivity asks the nurse what she should do about feeding her infant. Which recommendation would be most appropriate?
(a) “Continue to breastfeed, but eliminate all milk products from your own diet.”
(b) “Discontinue breastfeeding, and start using a predigested formula.”
(c) “Limit breastfeeding to once per day and begin feeding an iron-fortified formula.”
(d) “Change to a soy-based formula exclusively and begin solid foods.”
Answer:
(a) “Continue to breastfeed, but eliminate all milk products from your own diet.”
Explanation:
Mothers of infants with a cow’s milk allergy can continue to breastfeed if they eliminate cow’s milk from their diet. It is important to encourage mothers to continue to breastfeed because breast milk is usually the least allergenic and most easily digested food for an infant. In addition, the infant is able to obtain protein through the mother’s milk.
If the mother stops breastfeeding, then a predigested protein hydrolysate formula would be the first choice. An iron-fortified formula is a cow’s milk-based formula. A soy-based formula is not used because approximately 20% of infants with cow’s milk sensitivity are also sensitive to soy. Solid foods are not introduced until the infant is 4 to 6 months of age.
Question 38.
The nurse teaches the parents of a preschool child diagnosed with lactose intolerance how to incorporate dairy products into their child’s diet. Which statement by the parent reflects the need for more teaching?
(a) “My child should limit milk consumption to one small glass at a time.”
(b) “It is best to drink milk alone, not with meals.”
(c) “Eating hard cheese, cottage cheese, or yogurt may cause fewer symptoms than drinking milk.”
(d) “Using lactase enzymes or milk products containing lactase may help decrease gas.”
Answer:
(b) “It is best to drink milk alone, not with meals.”
Explanation:
Children with lactose intolerance often tolerate small amounts of dairy products better when they are consumed at mealtime with other foods. Most people with lactose intolerance can consume 2 to 4 oz (60 to 120 mL) of milk at a time without symptoms. Larger quantities are more likely to cause gas and bloating.
Cheeses contain less lactose than milk and may be better tolerated. Yogurt also contains enzymes that are activated in the duodenum that substitute for natural lactase. Taking supplemental enzymes or drinking lactase-treated milk may also substitute for natural lactase.
Question 39.
The nurse is inserting a nasogastric tube in an infant to administer feedings. In the figure below, indicate the location for the correct placement of the distal end of the tube.
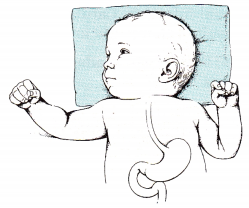
Answer:
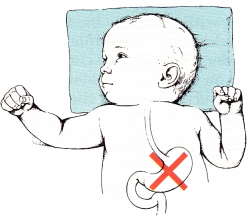
Explanation:
The nasogastric tube should reside in the stomach. The site placement can be verified by inserting 3 to 5 mL of air in the tube and auscultating the infant’s abdomen for the sound of air. The nurse should then aspirate the injected air and a small amount of stomach contents and then test the contents for acidity.
Question 40.
The nurse formulates a plan of care to address negative feeding patterns for a 5-month- old infant diagnosed with failure to thrive. To meet the short-term outcomes of the infant’s plan of care, the nurse should expect to implement which intervention?
(a) Instruct the parents in proper feeding techniques.
(b) Give the infant high-calorie formula.
(c) Provide consistent staff to care for the infant.
(d) Allow the infant to sit in a highchair during feedings.
Answer:
(c) Provide consistent staff to care for the infant.
Explanation:
In the short-term care of this infant, it is important that the same person feed the infant at each meal and that this person be able to assess for negative feeding patterns and replace them with positive patterns. Once the infant is gaining weight and shows progress in the feeding patterns, the parents can be instructed in proper feeding techniques.
This is a long-term outcome of nursing care. Because there is no organic reason for the failure to thrive, it should not be necessary to increase the formula calorie content. A 5-month-old infant is too young to be expected to sit in a high chair for feedings and should still be bottle-fed.
Question 41.
The health care team determines that the family of an infant with failure to thrive who is to be discharged will need follow-up care. Which approach would be the most effective method of follow-up?
(a) daily phone calls from the hospital nurse
(b) enrollment in community parenting classes
(c) twice-weekly clinic appointments
(d) weekly visits by a community health nurse
Answer:
(d) weekly visits by a community health nurse
Explanation:
The most effective follow-up care would occur in the home environment. The community health nurse can be supportive of the parents and will be able to observe parent-infant interactions in a natural environment. The community health nurse can evaluate the infant’s progress in gaining weight, offer suggestions to the parents, and help the family solve problems as they arise.
Question 42.
When providing intermittent nasogastric feedings to an infant with failure to thrive, which method is preferred to confirm tube placement before each feeding?
(a) obtaining a bedside chest X-ray
(b) verifying that the gastric pH is < 5.5
(c) auscultating the stomach while instilling an air bolus
(d) comparing the tube insertion length to a standardized chart
Answer:
(b) verifying that the gastric pH is < 5.5
Explanation:
For children receiving intermittent gavage feedings, the best method to verify the tube placement before each feeding is to aspirate a small amount of gastric contents to verify that the pH is acidic. A pH of 5.5 or less should indicate correct placement in most babies.
Depending on the type of feeding tube used, an X-ray may be used to confirm the original tube placement, but use before every feeding would expose the child to unnecessary radiation. Air boluses are misleading because placement in the esophagus or respiratory tract may make the same sound in small infants. Charts might be helpful in determining initial tube insertion length but do not substitute for nursing assessments.
Question 43.
When teaching parent workshops about measures to prevent lead poisoning in children, the nurse should identify which preventive measure as being the most effective.
(a) condemning old housing developments
(b) educating the public on common sources of lead
(c) conducting workshops on the importance of good nutrition
(d) keeping pregnant women out of old homes that are being remodeled
Answer:
(b) educating the public on common sources of lead
Explanation:
Public education about the sources of lead that could cause poisoning has been found to be the most effective measure to prevent lead poisoning. This includes recent efforts to alert the public to lead in certain types of window blinds. Condemning old housing developments has been ineffective because lead paint still exists in many other dwellings. Providing education about good nutrition, although important, is not an effective preventive measure. Pregnant women and children should not remain in an older home that is being remodeled because they may breathe in lead in the dust, but this is not the most effective preventive measure.
Question 44.
A child with a nut allergy presents with a severe reaction for the third time in 3 months. The parent says, “I am having trouble with the food labels.” What should the nurse do first?
(a) Assess the parent’s ability to read.
(b) Refer the client to the dietician.
(c) Notify the health care provider (HCP).
(d) Obtain a social service consult.
Answer:
(a) Assess the parent’s ability to read.
Explanation:
Three severe reactions in 3 months indicate a serious problem with adhering to the prevention plan. The nurse should first determine if the parent can actually read the label. The underlying problem may be that the parent is visually impaired or unable to read. The parent’s reading level determines what additional support is needed. Referrals to social services or dietary may be indicated, but the nurse does not yet have enough information about the problem. The nurse would communicate with the HCP after assessing the situation to recommend referrals.
Question 45.
During an admission history, the parents of a pediatric client explain that the family is Jewish and follows a kosher diet. Which food items would be appropriate for the client?
(a) sausage and pepperoni pizza and a glass of milk
(b) bacon and eggs and a glass of orange juice
(c) chicken, a cup of fruit, and a glass of water
(d) turkey sandwich and a glass of milk
Answer:
(c) chicken, a cup of fruit, and a glass of water
Explanation:
The kosher diet includes meat and fowl that are butchered using only humane methods. Meat and dairy may not be eaten together. Pigs are considered unclean and may not be eaten as part of a Kosher diet. Chicken is Kosher as long as it is butchered humanely. Fruits and vegetables are considered kosher as long as they are free from insects.
Also Read: