The PN NCLEX Questions are designed to reflect the types of scenarios and patient situations encountered in real-world nursing practice.
NCLEX Child with Gastrointestinal Tract Health Problems Questions
Child with Gastrointestinal Tract Health Problems NCLEX Practice Questions
Question 1.
When the nurse is developing the plan of care for an infant with a cleft lip before corrective surgery is performed, what should be a priority?
(a) maintaining skin integrity in the oral cavity
(b) using techniques to minimize crying
(c) altering the usual method of feeding
(d) preventing the infant from putting fingers in the mouth
Answer:
(c) altering the usual method of feeding
Explanation:
Before corrective surgery for a cleft lip, the infant needs to consume formula or breast milk. Methods for feeding may need to be adjusted to fit the infant’s needs because the infant with a cleft lip experiences a decreased ability to suck, which interferes with the infant’s ability to compress the nipple. A special feeder may be used to feed the infant to ensure adequate caloric intake.
Problems with infection and skin integrity in the mouth are uncommon because the areas of the defect are not open areas. Although crying may cause the infant to swallow more air because of the defect, crying poses no harm to the infant. There is no need to keep the infant’s fingers out of the mouth preoperatively. The fingers will not harm the defect or cause an infection.
Question 2.
Which measure would be most effective in helping the infant with a cleft lip and palate to retain oral feedings?
(a) Burp the infant at frequent intervals.
(b) Feed the infant small amounts at one time.
(c) Place the end of the nipple far to the back of the infant’s tongue.
(d) Maintain the infant in a supine position while feeding.
Answer:
(a) Burp the infant at frequent intervals.
Explanation:
An infant with a cleft lip and palate typically swallows large amounts of air while being fed and therefore should be burped frequently. The soft palate defect allows air to be drawn into the pharynx with each swallow of formula. The stomach becomes distended with air, and regurgitation, possibly with aspiration, is likely if the infant is not burped frequently.
Feeding frequently, even in small amounts, would not prevent swallowing of large amounts of air. A nipple placed in the back of the mouth is likely to cause the infant to gag and aspirate. Holding the infant in a supine position during feedings can also lead to regurgitation and aspiration of formula. The infant should be fed in an upright position.
Question 3.
After teaching the parent of an infant who has had a surgical repair for a cleft lip about the use of elbow restraints at home, the nurse determines that the teaching has been successful when the parent makes which statement?
(a) “We will only remove the restraints one at a time to check the skin under them for redness.”
(b) “We will keep the restraints on during the day while he is awake, but take them off when we put him to bed at night.”
(c) “After we get home, we will not have to use the restraints because our child does not suck on his hands or fingers.”
(d) “We will be sure to keep the restraints on all the time until we come to see the care provider for a follow-up visit.”
Answer:
(a) “We will only remove the restraints one at a time to check the skin under them for redness.”
Explanation:
To keep the infant from disturbing the suture line by placing fingers or other objects in the mouth, either intentionally or accidentally, the restraints should be in place at all times. They should be removed for a short period, however, so that the underlying skin can be checked for any redness or breakdown.
The best approach is to remove one restraint, complete the inspection, and reapply before checking the other arm. While the restraints are removed, the parents should be instructed to manually restrain the hands and arms.
Question 4.
The mother of an infant with a cleft lip asks when the repair will be scheduled. What is the nurse’s best response?
(a) at birth
(b) during the first 6 months of life
(c) after 6 months of age
(d) at 1 year of age
Answer:
(b) during the first 6 months of life
Explanation:
Cleft lips are typically repaired during the first 6 months of life. This allows the child to form a better seal around the nipple of a bottle for feeding and strengthens muscles needed for speech. If the surgery is delayed until after 6 months, the child may have possible dental issues and problems with sucking. The repair is not done at birth because the infant must first gain weight to safely undergo surgery. The pal¬ate should be closed by 18 months to protect the formation of tooth buds and allow the infant to develop more normal speech patterns.
Question 5.
On the 2nd postoperative day after repair of a cleft palate, what should the nurse use to feed a toddler?
(a) cup
(b) straw
(c) rubber-tipped syringe
(d) large-holed nipple
Answer:
(a) cup
Explanation:
A cup is the preferred drinking or eating utensil after repair of a cleft palate. At the age when repair is done, the child is ordinarily able to drink from a cup. Use of a cup avoids having to place a utensil in the mouth, which would increase the potential for injury to the suture lines.
Question 6.
The parents report that their 1-day-old is drooling and having choking episodes with excessive amounts of mucus and color changes, especially during feedings. The nurse should contact the health care provider (HCP) to further assess the baby and request which prescription?
(a) a lactation consultation
(b) an arterial blood gas
(c) an X-ray for gastric tube placement
(d) a serum blood glucose
Answer:
(c) an X-ray for gastric tube placement
Explanation:
The drooling and excessive mucus production is highly suggestive of a tracheoesophageal fistula (TEF). The initial diagnosis is made when a gastric tube cannot be passed to the stomach. A lactation consult would be warranted only after determining feedings were safe to continue. While cyanosis can be a sign of sepsis and hypoglycemia, cyanosis is most likely related to excessive secretions and airway patency. A blood gas may be needed, but only after ruling out a TEF.
Question 7.
The parents of a child with a tracheoesophageal fistula express feelings of guilt about their baby’s anomaly. Which approach by the nurse would best support the parents?
(a) helping the parents accept their feelings as a normal reaction
(b) explaining that the parents did nothing to cause the newborn’s defect
(c) encouraging the parents to concentrate on planning their baby’s care
(d) urging the parents to visit their newborn as often as possible
Answer:
(a) helping the parents accept their feelings as a normal reaction
Explanation:
The parents of children born with defects often have feelings of guilt and ask what they might have done to cause the condition or how they might have avoided it. It is important to allow parents to express their feelings and to accept these feelings as normal reactions. Explaining that the parents are not at fault would not be appropriate until they have dealt with their feelings of guilt.
Encouraging longterm planning generally is of little benefit to parents who are emotionally distraught. Additionally, the parents may interpret this as ignoring their feelings and confirming that they played a role in causing their child’s anomaly. Urging the parents to visit their infant as often as possible would generally be of little help and could appear to the parents as though they are being “talked out” of their feelings.
Question 8.
After teaching the parents of a neonate diagnosed with a tracheoesophageal fistula (TEF) about this anomaly, the nurse determines that the teaching was successful when the parent describes the condition in which way?
(a) “The muscle below the stomach is too tight, causing the baby to vomit forcefully.”
(b) “There is a blind upper pouch and an opening from the esophagus into the airway.”
(c) “The lower bowel is lacking certain nerves to allow normal function.”
(d) “A part of the bowel is on the outside without anything covering it.”
Answer:
(b) “There is a blind upper pouch and an opening from the esophagus into the airway.”
Explanation:
Although a TEF can include several different structural anomalies, the most common type involves a blind upper pouch and a fistula from the esophagus into the trachea. Other types include a blind pouch at the end of the esophagus with no connection to the trachea and a normal trachea and esophagus with an opening that connects them.
A tightened muscle below the stomach and projectile vomiting of normal amounts of formula are characteristic of pyloric stenosis. Aganglionic megacolon is a lack of autonomic parasympathetic ganglion cells in a portion of the lower intestine. Gastroschisis occurs when the bowel herniates through a defect in the abdominal wall and no membrane covers the exposed bowel.
Question 9.
Which finding would indicate that an infant with a tracheoesophageal fistula [TEF] most needs suctioning?
(a) barking cough
(b) substernal retractions
(c) decreased activity level
(d) increased respiratory rate
Answer:
(b) substernal retractions
Explanation:
With a TEF, overflow of secretions into the larynx leads to laryngospasm. This obstruction to inspiration stimulates the strong contraction of acces¬sory muscles of the thorax to assist the diaphragm in breathing. This produces substernal retractions. The laryngospasm that occurs with a TEF resolves quickly when secretions are removed from the oropharynx area.
A barking cough is related to a relatively constant laryngeal narrowing, usually caused by edema seen with croup. It is not an indication of the need to suction. A decreased activity level and an increased respiratory rate in an infant with a TEF are usually the result of hypoxia, a relatively long-term and constant phenomenon in infants with a TEF.
Question 10.
The nurse is administering bolus gastrostomy feedings to an infant after surgery to correct a tracheoesophageal fistula (TEF). What should the nurse do to prevent air from entering the stomach once the syringe barrel is attached to the gastrostomy tube?
(a) Unclamp the tube after pouring the complete amount of formula to be administered into the syringe barrel.
(b) Pour all of the formula to be administered into the syringe barrel after opening the clamp.
(c) Maintain a continuous flow of formula down the side of the syringe barrel once the clamp is opened.
(d) Allow a small amount of formula to enter the stomach before pouring more formula into the syringe barrel.
Answer:
(a) Unclamp the tube after pouring the complete amount of formula to be administered into the syringe barrel.
Explanation:
The best way to prevent air from entering the stomach when performing a bolus feeding on an infant through a gastrostomy tube is to open the clamp after all the formula has been placed in the syringe barrel. Doing so prevents air from mixing with the formula and thus being introduced into the stomach.
Pouring all the formula into the barrel after opening the clamp, maintaining a continuous flow of formula down the side of the barrel after unclamping the tube, and allowing a small amount of formula to enter the stomach before adding more formula to the barrel permit air to enter the stomach.
Question 11.
After surgery to repair a tracheoesophageal fistula, an infant receives gastrostomy tube feedings. The nurse continues holding the infant for about 15 minutes after the feeding primarily to help accomplish what need?
(a) Promote intestinal peristalsis.
(b) Prevent regurgitation of formula.
(c) Relieve pressure on the surgical site.
(d) Associate eating with a pleasurable experience.
Answer:
(d) Associate eating with a pleasurable experience.
Explanation:
The nurse can help meet the psychological needs of an infant being fed through a gastrostomy tube by rocking the infant after a feeding. The infant soon learns to associate eating with a pleasurable experience and learns to trust the caregiver. Rocking the infant will not promote peristalsis or prevent regurgitation. Holding the baby will not relieve pressure on the surgical site. However, holding the child right after feeding promotes comfort and pleasure.
Question 12.
A newborn who had a surgical repair of a tracheoesophageal fistula (TEF) is started on oral feedings. What should the nurse include in the teaching plan for the parent about oral feedings?
(a) They are better tolerated when larger but less frequent feedings are offered.
(b) They should be offered on a feeding schedule to help the infant accept the feedings more readily.
(c) They are best accepted by the infant when offered by the same nurse or by the infant’s parent.
(d) They are best planned in conjunction with observations of the infant’s behavioral cues.
Answer:
(d) They are best planned in conjunction with observations of the infant’s behavioral cues.
Explanation:
When initiating oral feedings after surgical repair of a TEF, it is best to follow a plan of care in conjunction with observation of the infant’s needs and behavior known as cue-based feedings. When sticking to a strict feeding schedule that overlooks the infant’s readiness, plans are likely to be unsatisfactory and are more likely to meet the nurse’s needs rather than the infant’s needs.
After a surgical procedure, infants initially tolerate small amounts of fluids offered more frequently than larger amounts offered less often. Smaller amounts cause less bloating as the infant becomes used to feeding again. Although infants accept feedings more readily from their mother or from someone who feeds the infant repeatedly, the priority is to meet the infant’s nutritional needs based on the infant’s behavior.
Question 13.
After completing diagnostic testing, the surgeon has scheduled a newborn with the diagnosis of an imperforate anus for surgery the next day. The infant’s parents do not want the surgery to take place unless the infant has first been baptized. What should the nurse ask the parents?
(a) “Are you worried your baby might die?”
(b) “How can I arrange the baptism?”
(c) “Do you want to speak with the social worker?”
(d) “Would you prefer to wait for the surgery?”
Answer:
(b) “How can I arrange the baptism?”
Explanation:
The nurse should honor the parent’s belief system and help arrange to have the infant baptized. This may be done through the hospital’s chaplaincy department or by the family’s clergy. The parents may indeed be worried that the infant may die during surgery. Having the infant baptized would help address the family’s spiritual needs.
At this time, there is an immediate need for chaplaincy, not social service. While surgery may be postponed briefly, the infant cannot begin feeding until an outlet for stool has been established. Therefore, it is not advisable to postpone the surgery for a prolonged period of time.
Question 14.
What should the nurse assess in a newborn diagnosed with an anorectal malformation? Select all that apply.
(a) abdominal distention
(b) loose stools
(c) vomiting
(d) meconium in the urine
(e) meconium stools
Answer:
(a) abdominal distention
(c) vomiting
(d) meconium in the urine
Explanation:
(a), (c), (d) Anorectal malformations present with lack of stool or evidence of meconium in the urine through a fistula. Meconium is not found in the stool. Because stool does not pass, abdominal distention and vomiting occur.
Question 15.
When performing discharge teaching with the parents of a neonate who has successfully undergone surgery to repair a low anorectal anomaly, which parent statement about the child’s prognosis indicates teaching has been successful?
(a) “My child will need to wear protective pads until puberty.”
(b) “My child will need extra fluids to prevent constipation.”
(c) “My child will probably always need a high- fiber diet.”
(d) “My child has a good chance of being potty trained.”
Answer:
(d) “My child has a good chance of being potty trained.”
Explanation:
Children who undergo surgical correction for low anorectal anomalies as infants usually are continent. Fecal continence can be expected after successful correction of anal membrane atresia. Therefore, this child probably has a good chance of being potty trained and will not need to wear protective pads. Extra fluids and a high-fiber diet are not required to prevent constipation. Children with high anorectal anomalies may or may not achieve continence.
Question 16.
The father of a neonate scheduled for gas-trointestinal surgery asks the nurse how newborns respond to painful stimuli. What is the nurse’s best response?
(a) “Newborns cry and cannot be distracted to stop crying.”
(b) “When faced with a pain, newborns try to roll away from it. ”
(c) “Newborns typically move their whole body in response to pain.”
(d) “Pain causes the newborn to withdraw the affected part.”
Answer:
(c) “Newborns typically move their whole body in response to pain.”
Explanation:
The neonate responds to pain with total body movement and brief, loud crying that ceases with distraction. After the age of 6 months, an infant reacts to pain with intense physical resistance and tries to escape by rolling away. A toddler reacts to pain by withdrawing the affected part.
Question 17.
When developing the plan of care for a neonate who was diagnosed with an anorectal malfor¬mation and who subsequently underwent surgery, what intervention would be most helpful in facilitating parent-infant bonding?
(a) explaining to the parents that they can visit at any time
(b) encouraging the parents to hold their infant
(c) asking the parents to help monitor the infant’s intake and output
(d) helping the parents plan for their infant’s discharge
Answer:
(b) encouraging the parents to hold their infant
Explanation:
Encouraging the parents to hold their neonate promotes parent-infant attachment. Parent- infant bonding is based on a relationship that begins when the parent first touches the infant. Both the parents and the infant have predictable steps that they go through in this process. Explaining that the parents can visit at any time promotes bonding only if they do visit with, talk to, and hold the newborn.
Asking the parents to help monitor intake and output at this time may be too anxiety producing, thus interfering with bonding. Helping the parents plan for the infant’s discharge involves them in the newborn’s care and is important. However, it is not the first step in the development of bonding.
Question 18.
A 4-week-old infant admitted with the diagnosis of hypertrophic pyloric stenosis presents with a history of vomiting. The nurse should anticipate that the infant’s vomitus would contain gastric contents and which other body substances?
(a) bile and streaks of blood
(b) mucus and stool
(c) mucus and streaks of blood
(d) stool and bile
Answer:
(c) mucus and streaks of blood
Explanation:
The vomitus of an infant with hypertrophic pyloric stenosis contains gastric contents, mucus, and streaks of blood. The vomitus does not contain bile or stool because the pyloric constriction is proximal to the ampulla of Vater.
Question 19.
When an infant with pyloric stenosis is admitted to the hospital, which aspect of the plan of care should the nurse implement first?
(a) Weigh the infant.
(b) Begin an intravenous infusion.
(c) Switch the infant to an oral electrolyte solution.
(d) Orient the mother to the hospital unit.
Answer:
(a) Weigh the infant.
Explanation:
Unless the infant is in hypovolemic shock, obtaining a baseline weight is an important first action because the weight is used to calculate the child’s fluid and electrolyte needs. The intravenous fluid rate and the amounts of electrolytes to be added to the fluid are based on the infant’s weight. The weight also helps determine the infant’s degree of dehydration.
The intravenous infusion is initiated once the weight has been obtained. A child with pyloric stenosis typically experiences vomiting and is at risk for fluid volume deficit and metabolic acidosis. As a result, oral food and fluids are withheld, and the infant is allowed nothing by mouth. Fluid replacement is given intravenously. Orientation can wait until treatment is underway.
Question 20.
After the nurse teaches the parent of an infant with pyloric stenosis about the condition, which cause if stated by the parent, indicates effective teaching?
(a) “an enlarged muscle below the stomach”
(b) “a telescoping of the large bowel into the smaller bowel”
(c) “a result of giving the baby more formula than is necessary”
(d) “a genetically smaller stomach than normal"
Answer:
(a) “an enlarged muscle below the stomach”
Explanation:
Pyloric stenosis involves hypertrophy of the pylorus muscle distal to the stomach and obstruction of the gastric outlet resulting in vomiting, metabolic acidosis, and dehydration. Telescoping of the bowel is called intussusception. Overfeeding, feeding too quickly, or underfeeding is not associated with pyloric stenosis. The stomach is obstructed, but it is not smaller than normal.
Question 21.
A newborn admitted with pyloric stenosis is lethargic and has poor skin turgor. The health care provider (HCP) has prescribed IV fluids of dex¬trose water with sodium and potassium. The baby’s admission potassium level is 3.4 mEq/L
(3.4 mmol/L). What should the nurse do first?
(a) Notify the HCP.
(b) Administer the prescribed fluids.
(c) Verify that the infant is urinating.
(d) Have the potassium level redrawn.
Answer:
(c) Verify that the infant is urinating.
Explanation:
Normal serum potassium levels are 3.5 to 4.5 mEq/L (3.5 to 4.5 mmol/L). Elevated potassium levels can cause life-threatening cardiac arrhythmias. The nurse must verify that the client has the ability to clear potassium through urination before administering the drug.
Infants with pyloric stenosis frequently have low potassium levels due to vomiting. A level of 3.4 mEq/L (3.4 mmol/L) is not unexpected and should be corrected with the prescribed fluids. The lab value does not need to be redrawn as the findings are consistent with the infant’s condition.
Question 22.
After undergoing surgical correction of pyloric stenosis, an infant is returned to the room in stable condition. While standing by the crib, the mother says, “Perhaps if I had brought my baby to the hospital sooner, the surgery could have been avoided.” What is the nurse’s best response?
(a) “Surgery is the most effective treatment for pyloric stenosis.”
(b) “Try not to worry; your baby will be fine.”
(c) “Do you feel that this problem indicates that you are not a good mother?”
(d) “Do you think that earlier hospitalization could have avoided surgery?”
Answer:
(d) “Do you think that earlier hospitalization could have avoided surgery?”
Explanation:
Restating or rephrasing a mother’s response provides the opportunity for clarification and validation. It also helps to focus on what the mother is saying and address her concerns and feelings. Although surgery is the most effective treatment for pyloric stenosis, stating this ignores the mother’s feelings and does not give her an opportunity to express them.
Telling the mother not to worry also ignores the mother’s feelings. Additionally, this type of statement gives the mother premature reassurance, which may turn out to be false. Asking the mother if she thinks the problem indicates that she is not a good mother implies such an idea. It does not allow her to express her concerns and feelings and therefore is not a therapeutic response.
Question 23.
After surgery to correct pyloric stenosis, the nurse instructs the parents about the postoperative feeding schedule for their infant. The parents exhibit an understanding of these instructions when they state that they can start feeding the child within which time frame?
(a) 6 hours
(b) 8 hours
(c) 10 hours
(d) 12 hours
Answer:
(a) 6 hours
Explanation:
Clear liquids containing glucose and electrolytes are usually prescribed 4 to 6 hours after surgery. If significant vomiting does not occur, formula or breast milk then can be gradually substituted for clear liquids until the infant is taking normal feedings.
Question 24.
Immediately after the first oral feeding after corrective surgery for pyloric stenosis, a 4-week-old infant is fussy and restless. Which action would be most appropriate at this time?
(a) Encourage the parents to hold the infant.
(b) Hang a mobile over the infant’s crib.
(c) Give the infant more to eat.
(d) Give the infant a pacifier to suck on.
Answer:
(d) Give the infant a pacifier to suck on.
Explanation:
Giving the infant a pacifier would help meet nonnutritive sucking needs and ensure oral gratification. Additionally, sucking aids in calming the infant. Holding the infant to decrease fussiness and restlessness is more effective in an older infant. Also, the reason for the infant's fussiness needs to be explored.
Hanging a mobile over the crib frequently does not decrease fussiness. After surgery to correct pyloric stenosis, feeding the infant more formula would lead to vomiting, putting additional stress on the operative site.
Question 25.
Which behavior exhibited by the parent of an infant with pyloric stenosis should the nurse correctly interpret as a positive indication of parental coping?
(a) telling the nurse that they have to get away for a while
(b) discussing the infant’s care realistically
(c) repeatedly asking if their child is normal
(d) exhibiting fear that they will disturb the infant
Answer:
(b) discussing the infant’s care realistically
Explanation:
The parents’ ability to verbalize the infant’s care realistically indicates that they are working through their fears and concerns. This behavior demonstrates an understanding of the infant’s condition and needs. Without further data, the fact that the parents have to get away could be interpreted as ineffective coping, possibly sug-gesting that they are unable to handle the situation.
Continuing to ask about the child’s general condition oven after answers have been given does not suggest effective coping. The parents are demonstrating that thoy are unsure of themselves as parents or are hoping for positive information. Exhibiting fear that they will disturb the infant does not suggest effective! coping. This behavior indicates that they are uncertain or lack knowledge about infants.
Question 26.
A 6-month-old has had a pyloromyotomy to correct a pyloric stenosis. Three days after surgery, the parents have placed their infant in his own infant seat (see figure). What should the nurse do?

(a) Reposition the infant to the left side.
(b) Ask the parents to put the infant back in his crib.
(c) Remind the parents that the infant cannot use a pacifier now.
(d) Tell the parents they have positioned their infant correctly.
Answer:
(d) Tell the parents they have positioned their infant correctly.
Explanation:
Following pyloromyotomy, the infant should be positioned with the head elevated and slightly on the right side to promote gastric emptying; the parents have positioned their infant corside, not the left side. When the child is in a crib, the head can be elevated, and the infant can be propped on the right side. The infant can use a paci-fier if needed.
Question 27.
When assessing a 4-month-old infant diagnosed with possible intussusception, the nurse should expect the parent to relate which information about the infant’s crying and episodes of pain?
(a) constant accompanied by leg extension
(b) intermittent with knees drawn to the chest
(c) shrill during ingestion of solids
(d) intermittent while being held in the mother’s arms
Answer:
(b) intermittent with knees drawn to the chest
Explanation:
The infant with intussusception experiences acute episodes of colic-like abdominal pain. Typically, the infant screams and draws the knees to the chest. Between these episodes of acute abdominal pain, the infant appears comfortable and normal. Feeding does not precipitate episodes of pain. Additionally, a 4-month-old infant typically would not be ingesting solid foods.
Pain exhibited by crying that occurs when the infant is placed in a reclining position, as in the mother’s arms, is not associated with intussusception. This type of cry may indicate that the infant wants attention, wants to be held, or needs to have a diaper change.
Question 28.
When obtaining the nursing history from the mother of an infant with suspected intussusception, which question would be most helpful?
(a) “What do the stools look like?”
(b) “When was the last time your child urinated?”
(c) “Is your child eating normally?”
(d) “Has your child had any episodes of vomiting?”
Answer:
(a) “What do the stools look like?”
Explanation:
For infant with intussusception, stools characteristically have the appearance of currant jelly because of the intestinal inflammation and hemorrhage resulting from intestinal obstruction. These stools occur later in the course of the disease process. Questions that focus on urination, vomiting, and food intake do not elicit information about the effects of intussusception.
Question 29.
A nasogastric tube inserted during surgical correction of an infant’s intussusception is no longer freely removing gastric secretions. What should the nurse do next?
(a) Verify the tube placement.
(b) Irrigate the tube.
(c) Increase the level of suction.
(d) Rotate the tube.
Answer:
(a) Verify the tube placement.
Explanation:
The first action is to check the placement of the tube to ensure that it is in the correct position. To check tube position, the nurse should aspirate the tube with a syringe. A return of gastric contents indicates that the end of the tube is in the stomach.
Another method is to inject a small amount of air while auscultating with a stethoscope over the epigastric area. The tube is irrigated only after the position of the tube is confirmed. The suction level should not be increased because doing so could damage the mucosa. Rotating the tube could irritate or traumatize the nasal mucosa.
Question 30.
Which assessment should be the priority for an infant who has had surgery to correct an intussusception and is now at risk for the development of a paralytic ileus postoperatively?
(a) measurement of urine specific gravity
(b) auscultation of bowel sounds
(c) inspection of the first stool passed
(d) measurement of gastric output
Answer:
(b) auscultation of bowel sounds
Explanation:
Development of a paralytic ileus postoperatively is a functional obstruction of the bowel. Bowel sounds initially may be hyperactive, but then they diminish and cease. Measurement of urine specific gravity provides information about fluid and electrolyte status. The first stool and the amount of gastric output provide information about the return of gastric function.
Question 31.
An infant is to be discharged after surgery for intussusception. What information should the nurse include in the discharge teaching plan?
(a) The infant will experience a change in the normal home routine.
(b) The infant can return to the prehospital routine immediately.
(c) The infant needs to ingest more calories at home than what was consumed in the hospital.
(d) The infant will continue to experience abdominal cramping for a few days.
Answer:
(a) The infant will experience a change in the normal home routine.
Explanation:
Infants who have had an interruption in their normal routine and experiences, such as hospitalization and surgery, typically manifest behavior changes when discharged. The infant’s normal routine has been significantly altered, so it will take time to reestablish another routine.
Calorie requirements at home will continue to be the same as those in the hospital. The infant does not need more calories at home. The surgical procedure corrected the problems, so the infant should not continue to have abdominal cramping.
Question 32.
When the nurse is assessing an infant with suspected inguinal hernia, which finding would be most concerning?
(a) The inguinal swelling is reddened, and the abdomen is distended.
(b) The infant is irritable, and a thickened spermatic cord is palpable.
(c) The inguinal swelling can be reduced, and the infant has a stool in the diaper.
(d) The infant’s diaper is wet with urine, and the abdomen is nontender.
Answer:
(a) The inguinal swelling is reddened, and the abdomen is distended.
Explanation:
Abdominal distention and a redness of the inguinal swelling are significant findings. Their presence in conjunction with area tenderness and inability to reduce the hernia indicate an incarcerated hernia. An incarcerated hernia can lead to strangulation, necrosis, and gangrene of the bowel. Other findings associated with strangulation include irritability, anorexia, and difficulty in defecation.
A strangulated hernia necessitates immediate surgical intervention. The ability to reduce the hernia and normal stooling do not indicate it is incarcerated. Irritability is nonspecific and could be caused by various factors. A palpable, thickened spermatic cord on the affected side is diagnostic of inguinal hernia and would be an expected finding. A wet diaper indicates that urine is being excreted, a finding unrelated to inguinal hernia.
Question 33.
Preoperatively, the nurse develops a plan to prepare a 7-month-old infant psychologically for a scheduled herniorrhaphy the next day. Which intervention should the nurse expect to implement to accomplish this goal?
(a) explaining the preoperative and postoperative procedures to the mother
(b) having the mother stay with the infant
(c) making sure the infant’s favorite toy is available
(d) allowing the infant to play with surgical equipment
Answer:
(b) having the mother stay with the infant
Explanation:
The best way to prepare a 7-month-old infant psychologically for surgery is to have the primary caretaker stay with the child. Infants in the second 6 months of life commonly develop separation anxiety. Therefore, the priority in this case is to support the child by having the parent present.
Teaching the mother what to expect may decrease her anxiety; this is important because infants sense anxiety and distress in parents, but the priority in this case is to have the parent present. Actual play and acting out life experiences are appropriate for preschool-age children. Allowing an infant to play with surgical equipment would be inappropriate and dangerous.
Question 34.
Which instruction should the nurse expect to include in the discharge teaching plan for the parent of an infant who has had an inguinal herniorrhaphy?
(a) Change diapers as soon as they become soiled.
(b) Apply an abdominal binder.
(c) Keep the incision covered with a sterile dressing.
(d) Restrain the infant’s hands.
Answer:
(a) Change diapers as soon as they become soiled.
Explanation:
Changing a diaper as soon as it becomes soiled helps prevent wound infection, the most common complication after inguinal hernia repair in an infant secondary to possible wound contamination with urine and stool. Because the surgical wound is unlikely to separate, an abdominal binder is unnecessary.
The incision may or may not be cov-ered with a dressing. If a dressing is not used, the health care provider (HCP) may apply a topical spray to protect the wound. Restraining the infant’s hands is unnecessary if the diaper is applied snugly. The infant would be unable to get the hands into the diaper close to the surgical site.
Question 35.
A parent asks, “How should I bathe my baby now that he has had surgery for his inguinal hernia?” Which instruction should the nurse give the parent?
(a) “Clean only his face and diaper area for next 2 weeks.”
(b) “Use sterile sponges to cleanse the inguinal incision until healed.”
(c) “Give him a sponge bath daily for 1 week."
(d) “Let him take a full tub bath daily.”
Answer:
(c) “Give him a sponge bath daily for 1 week."
Explanation:
The incision must be kept as clean and dry as possible. Therefore, daily sponge baths are given for about 1 week postoperatively. The infant can have more than just face and diaper area cleaned following surgery. Because this type of surgery results in a wound that heals through primary intention, the skin will heal and cover the wound in 2 to 3 days. Therefore, it is not necessary to use sterile gauze to cleanse the incision; clean technique is acceptable. Because the incision must be kept as clean and dry, full tub baths are inappropriate.
Question 36.
During physical assessment of a 4-month-old infant with Hirschsprung’s disease, the nurse would most likely note which finding?
(a) scaphoid-shaped abdomen
(b) weight less than expected for height and age
(c) cyanosis of the fingers and toes
(d) hyperactive deep tendon reflexes
Answer:
(b) weight less than expected for height and age
Explanation:
Infants with Hirschsprung’s disease typically display failure to thrive, with poor weight gain due to malabsorption of nutrients. Therefore, the nurse would expect to see a child who weighs less than that which is expected for height and age. A distended, rather than a scaphoid-shaped, abdomen would be noted. Cyanosis of fingers and toes is associated with congenital heart disease. Hyperactive deep tendon reflexes are associated with upper motor neuron problems, such as cerebral palsy.
Question 37.
An infant diagnosed with Hirschsprung’s disease is scheduled to receive a temporary colostomy. When the nurse is initially discussing the diagnosis and treatment with the parents, which action by the nurse would be most appropriate?
(a) assessing the adequacy of their coping skills
(b) reassuring them that their child will be fine
(c) encouraging them to ask questions
(d) giving them printed material on the procedure
Answer:
(c) encouraging them to ask questions
Explanation:
By encouraging parents to ask questions during information-sharing sessions, the nurse can clarify misconceptions and determine the parents’ understanding of information. A better understanding of what is happening allows the parents to feel some control over the situation. Assessing the adequacy of the parents’ coping skills is important but secondary to encouraging them to express their concerns.
The questions they ask and their interactions with the nurse may provide clues to the adequacy of their coping skills. The nurse should never give false reassurance to parents. At this point, there is no way for the nurse to know whether the child will be fine. Written materials are appropriate for augmenting the nurse’s verbal communication. However, these are secondary to encouraging questions.
Question 38.
After teaching the parents of an infant diagnosed with Hirschsprung’s disease, the nurse determines that the parents understand the diagnosis when the parent makes which statement?
(a) “There are congenital polyps obstructing the colon.”
(b) “A section of the colon is constricted.”
(c) “The nerves at the end of the large colon are missing.”
(d) “There is a weakened area in the colon that is inflamed.
Answer:
(c) “The nerves at the end of the large colon are missing.”
Explanation:
The primary defect in Hirschsprung’s disease is an absence of autonomic parasympathetic ganglion cells in the distal portion of the colon. Thus, the nerves at the end of the large colon are missing. Constipation is caused by decreased peristalsis, not a physical obstruction like polyps. The colon typically enlarges giving rise to the name “megacolon” versus being constricted.
Weakened areas of the colon are associated with diverticulosis. Absence of a rectal opening refers to an imperforate anus. A tube between the trachea and esophagus refers to a tracheoesophageal fistula. Presence of a tight muscle below the stomach refers to pyloric stenosis.
Question 39.
When developing the preoperative plan of care for an infant with Hirschsprung’s disease, the nurse should include which intervention?
(a) administering a tap water enema
(b) inserting a gastrostomy tube
(c) restricting oral intake to clear liquids
(d) using povidone-iodine solution to prepare the perineum
Answer:
(c) restricting oral intake to clear liquids
Explanation:
Before intestinal surgery, dietary intake is limited to clear liquids for 24 to 48 hours. A clear liquid diet meets the child’s fluid needs and avoids the formation of fecal material in the intestine. Typically, repeated saline enemas, not tap water enemas, are given to empty the bowel. Soapsuds enemas are contraindicated for infants, as are tap water enemas. A nasogastric tube may be inserted for gastric decompression. Insertion of a gastrostomy tube is outside the scope of nursing practice. Because the perineal area is not involved in the surgery, it does not need to be prepared
Question 40.
The nurse is showing the parent of a child with Hirschsprung’s disease where the aganglionic area is located. Identify the area the nurse should point out as being aganglionic.
Answer:
Explanation:
In most instances, the absence of ganglionic innervation occurs in the lower portion of the sigmoid colon just above the anus.
Question 41.
An infant diagnosed with Hirschsprung’s disease undergoes surgery with the creation of a temporary colostomy. Which statement by the parent regarding the colostomy indicates the need for further teaching?
(a) “The colostomy is only temporary.”
(b) “The colostomy will give time for the nerves to return to normal.”
(c) “The colostomy may include two separate abdominal openings.”
(d) “Right after the procedure, the stoma may appear purple.”
Answer:
(b) “The colostomy will give time for the nerves to return to normal.”
Explanation:
The goal of the surgery is to remove the aganglionic portion of the intestine. The remaining intestines should have normal innervation. Colostomies are used to relieve the obstruction and allow the remaining intestines to return to normal size.
A temporary loop or double-barreled colostomy has stomas for both the proximal and distal portion of the bowel. The final surgical repair is usually done when the infant is around 20 lb (9.1 kg). A new stoma is frequently swollen and bruised after surgery.
Question 42.
When teaching the mother of an infant who has received a temporary colostomy for treatment of Hirschsprung’s disease about how the stoma should normally appear, the nurse should include which description about the stoma’s appearance in the teaching?
(a) becoming dark brown in 2 months
(b) staying deep red in color
(c) changing to several shades of pink
(d) turning almost purple in color
Answer:
(b) staying deep red in color
Explanation:
Typically, the stoma should remain deep red in color as long as the infant has the colostomy. A dark red to purplish color may indicate impaired circulation to the stoma.
Question 43.
When teaching the parent of an infant with Hirschsprung’s disease who received a temporary colostomy about the types of foods the infant will be able to eat, which diet would the nurse recommend?
(a) high-fiber diet
(b) low-fat diet
(c) high-residue diet
(d) regular diet
Answer:
(d) regular diet
Explanation:
A regular diet would be recommended for the child with a colostomy; no special diet is needed. A high-fiber diet is not necessary. Fat is necessary for brain growth in the first year of life. A high-residue diet would result in bulkier stools and increased gas production, which will collect in the colostomy bag. Therefore, a high-residue diet is not indicated.
Question 44.
A child with Hirschsprung’s disease is to be discharged 1 or 2 days after a colostomy takedown surgery. After teaching the infant’s parents about the overall effects of their infant’s surgery, the nurse determines that the teaching has been effective when the parents make which statement?
(a) “His abdomen will be large for a while.”
(b) “Toilet training may be difficult.”
(c) “We need to limit his intake of dairy products.”
(d) “We will give him vitamin supplements until he is an adolescent.”
Answer:
(b) “Toilet training may be difficult.”
Explanation:
Toilet training is commonly more difficult for children who have undergone surgery for Hirschsprung’s disease than it is for other children. This is because of the trauma to the area and the associated psychological implications. Abdominal distention is an early sign of infection, and therefore the parents need to report it to the health care provider (HCP) m. Typically, dietary restrictions are not required, but fiber is encouraged. Usually, the infant is placed on an age-appropriate diet. Vitamin supplementation is not necessary if the infant’s dietary intake is adequate.
Question 45.
A parent of a 7-year-old child with Hirschsprung’s disease and chronic constipation asks about increasing dietary fiber in the child’s diet. Which food could the nurse recommend?
(a) ffuitjuice
(b) white bread
(c) popcorn
(d) pancakes
Answer:
(c) popcorn
Explanation:
Popcorn is high in fiber. Foods high in fiber help the bowels move. Constipation may be managed initially with increased fiber and fluids. White bread, fruit juice, and pancakes are foods that are not high in fiber.
Question 46.
A nurse is caring for a 10-month-old, weighing 8 kg, who was admitted for dehydration. The infant has an IV of D5W 0.45% normal saline infusing at the maintenance rate of 100 mL/kg/day for children weighing 10 kg or less. The infant has vomited 5 times in the last 3 hours and has had no wet diapers in the last 8 hours. The nurse informs the health care provider (HCP). Which prescription should the nurse question?
(a) Increase the intravenous fluids to 45 mL/h for 24 hours.
(b) Keep NPO while vomiting persists.
(c) Administer a 10 mL/kg fluid bolus of dextrose 25%.
(d) Maintain strict intake and output, weighing all diapers.
Answer:
(c) Administer a 10 mL/kg fluid bolus of dextrose 25%.
Explanation:
The infant is in need of a fluid bolus. A fluid bolus should consist of an isotonic fluid such as normal saline or lactated Ringer’s. Dextrose 25% is not an appropriate bolus for dehydrated children because it could cause a fluid shift that may result in cerebral edema and death; thus, the nurse should question the prescription. D5W0.45% normal saline is an appropriate IV fluid for infants.
The rate is 1.5 times maintenance for this child and is appropriate for the first 24 hours if the child is dehydrated. Once hydration is adequate, the infant’s IV rate should be reduced to a maintenance rate. Vomiting is persistent, so it is appropriate for the child to be NPO. Strict I and O is an appropriate prescription for all dehydrated children.
Question 47.
Which signs or symptoms suggest that an infant with diarrhea is dehydrated? Select all that apply.
(a) tacky mucous membranes
(b) sunken anterior fontanelle
(c) salty saliva
(d) restlessness
(e) increased urine output
Answer:
(a) tacky mucous membranes
(b) sunken anterior fontanelle
(d) restlessness
Explanation:
(a), (b), (d) Diarrhea in infants is a serious condition as it can proceed rapidly to dehydration. Clinical signs of dehydration are irritability and restlessness, weakness, stupor, loss of body weight, poor skin turgor, and sunken fontanelles. The urine output is decreased in dehydrated infants. The saliva decreases with dehydration and is not salty.
Question 48.
A child is admitted with a tentative diagnosis of shigella. The nurse performs which interventions? Select all that apply.
(a) Assess the child for nausea and vomiting.
(b) Collect a stool specimen for white blood cells (WBCs).
(c) Place the child on airborne precautions.
(d) Monitor the child for signs and symptoms of dehydration.
(e) Initiate an intake and output record.
Answer:
(a) Assess the child for nausea and vomiting.
(b) Collect a stool specimen for white blood cells (WBCs).
(d) Monitor the child for signs and symptoms of dehydration.
(e) Initiate an intake and output record.
Explanation:
(a), (b), (d), (e) Shigella is caused by the Shigella organism. Clinical manifestations of shigella include fever, nausea and vomiting, some cramping, headache, seizures, rectal prolapse, and loose, watery stools containing pus, mucus, and blood. The nurse should assess the child for these symptoms on an ongoing basis. Shigella is spread via direct contact with the organism, which is found in the stool.
A stool specimen will show increased numbers of WBCs, blood, and mucus. Vomiting and loose stools can result in severe dehydration and electrolyte imbalance. Thus, the nurse should record intake, output, and daily weights. There is no need for strict isolation; masks are not needed as shigella is not transmitted by airborne methods.
Question 49.
Which finding would most likely alert the nurse to the possibility that a preschooler is experiencing moderate dehydration?
(a) deep, rapid respirations
(b) diaphoresis
(c) absence of tear formation
(d) decreased urine specific gravity
Answer:
(c) absence of tear formation
Explanation:
The absence of tears is typically found when moderate dehydration is observed as the body attempts to conserve fluids. Other typical findings associated with moderate dehydration include a dry mouth, sunken eyes, poor skin turgor, and an increased pulse rate. Deep, rapid respirations are associated with severe dehydration. Decreased perspi-ration, not diaphoresis, would be seen with moderate dehydration. The specific gravity of urine increases with decreased output in the presence of dehydration.
Question 50.
Which finding would be most important in an 8-month-old infant admitted with severe diarrhea?
(a) bowel sounds every 5 seconds
(b) pale yellow urine
(c) normal skin elasticity
(d) depressed anterior fontanelle
Answer:
(d) depressed anterior fontanelle
Explanation:
An infant with severe diarrhea will experience some degree of dehydration. In an 8-month-old child, the anterior fontanelle has not closed. Therefore, a depressed anterior fontanelle would be an important finding. Additionally, the infant would exhibit dry mucous membranes, lethargy, hyperactive bowel sounds, dark urine, and sunken eyeballs. Skin turgor would be decreased or delayed (e.g., slow to return when pinched). Bowel sounds every 5 seconds would not be considered abnormal for an infant.
Question 51.
Which assessment would be the most important for the nurse to include in the plan of care for an infant experiencing severe diarrhea?
(a) monitoring the total 8-hour formula intake
(b) weighing the infant each day
(c) checking the anterior fontanelle every shift
(d) monitoring abdominal skin turgor every shift
Answer:
(b) weighing the infant each day
Explanation:
Because an infant experiencing severe diarrhea is at high risk for a fluid volume deficiency, the nurse needs to evaluate the infant’s fluid balance status by weighing the infant at least every day. Body weight is the best indicator of hydration status because a higher proportion of an infant’s body weight is water, compared with an adult. Initially, the infant with severe diarrhea is not allowed liquids but is given fluids intravenously. Therefore, monitoring the oral intake of formula
is inappropriate.
Although checking the anterior fontanelle for depression or bulging provides information about hydration status, this method is not considered the best indicator of the infant’s fluid balance. Monitoring skin turgor can provide information about fluid volume status. The abdomen is commonly used to assess skin turgor in an infant because it is a large surface area and can be accessed quickly. However, weight is the best indicator of fluid balance.
Question 52.
The health care provider (HCP) prescribes an intravenous infusion of 5% dextrose in 0.45 normal saline to be infused at 2 mL/kg/h in an infant who weighs 9 lb (4.1mL/kg/h). How many milliliters per hour of the solution should the nurse infuse? Round to one decimal place.
Answer:
8.2 mL/h
Explanation:
4.1 kg x 2 mL/kg = 8.2 mL/h
Question 53.
A 3-year-old with dehydration has vomited 3 times in the last hour and continues to have frequent diarrhea stools. The child was admitted 2 days ago with gastroenteritis caused by rotavirus. The child weighs 22 kg, has a normal saline lock in his right hand, and has had 30 mL of urine output in the last 4 hours. Using the situation-background- assessment-recommendation (SBAR) technique for communication, the nurse calls the health care provider (HCP) with the recommendation for which prescription?
(a) giving a dose of loperamide
(b) starting a fluid bolus of normal saline
(c) beginning an IV antibiotic
(d) establishing an indwelling catheter
Answer:
(b) starting a fluid bolus of normal saline
Explanation:
The child is dehydrated, is not able to retain oral fluids, and continues to have diarrhea. A normal saline bolus should be given followed by maintenance of IV fluids. Antidiarrheal medications are not recommended for children and will prolong the illness. The child has gastroenteritis caused by a viral illness. IV antibiotics are not indicated for viral illnesses. Strict I&O is important in all children with gastroenteritis.
Question 54.
Which intervention would be most appropriate for the nurse to teach the mother of a 6-month- old infant hospitalized with severe diarrhea to help her comfort her infant who is fussy?
(a) offering a pacifier
(b) placing a mobile above the crib
(c) sitting at crib side talking to the infant
(d) turning the television on to cartoons
Answer:
(a) offering a pacifier
Explanation:
Typically, an infant hospitalized with severe diarrhea receives fluid replacement intravenously rather than orally. Oral fluids and food are usually withheld. Although activities such as placing a mobile over the crib, speaking to the infant, or turning on the television may provide distraction for or help in calming the infant, a fussy
infant receiving nothing by mouth is usually best comforted by providing a pacifier to satisfy sucking needs.
Question 55.
What would the nurse identify as a priority nursing problem for an infant just admitted to the hospital with a diagnosis of gastroenteritis?
(a) pain related to repeated episodes of vomiting
(b) deficient fluid volume related to excessive losses from severe diarrhea
(c) impaired parenting related to infant’s loss of fluid
(d) impaired urinary elimination related to increased fluid intake feeding pattern
Answer:
(b) deficient fluid volume related to excessive losses from severe diarrhea
Explanation:
Given this infant’s history of gastroenteritis, the priority problem would be fluid volume deficit. With gastroenteritis, vomiting and diarrhea occur, leading to the loss of fluids. This loss of fluids is problematic in infants because a higher proportion of their body weight is water. Pain is not a priority problem, although the nurse should continue to assess the infant for pain.
There is no data to indicate impaired parenting. Impaired urinary elimination is related to the infant’s fluid volume deficit resulting from vomiting and diarrhea associated with gastroenteritis. If the infant’s fluid volume deficit is not corrected, then this nursing diagnosis may become the priority.
Question 56.
The nurse teaches the father of an infant hospitalized with gastroenteritis about the next step of the treatment plan once the infant’s condition has been controlled. The nurse determines that the father understands when he explains which intervention will occur with his infant?
(a) The infant will receive clear liquids for a period of time.
(b) Formula and juice will be offered.
(c) Blood will be drawn daily to test for anemia.
(d) The infant will be allowed to go to the playroom.
Answer:
(a) The infant will receive clear liquids for a period of time.
Explanation:
The usual way to treat an infant hospitalized with gastroenteritis is to keep the infant's nothing-by-mouth status to rest the gastrointestinal tract. The resulting fluid volume deficit is treated with intravenous fluids. When the infant’s condition is controlled (e.g., when vomiting subsides), clear liquids are then started slowly. Formula and juice will be started once the infant’s vomiting has subsided and the infant has demonstrated the ability to tolerate clear liquids for a period of time.
In this situation, there is no need to test the infant’s blood every day for anemia. Most likely, the infant’s serum electrolyte levels would be monitored closely. Typically, an infant is placed in a private room because gastroenteritis is most commonly caused by a virus that is easily transmitted to others.
Question 57.
The mother of a toddler who has just been admitted with severe dehydration secondary to gastroenteritis says that she cannot stay with her child because she has to take care of her other children at home. Which of the responses by the nurse would be most appropriate?
(a) “You really shouldn’t leave right now. Your child is very sick.’’
(b) “I understand, but feel free to visit or call anytime to see how your child is doing.”
(c) “It’s really not necessary to stay with your child. We will take very good care of him.”
(d) “Can you find someone to stay with your children? Your child needs you here.”
Answer:
(b) “I understand, but feel free to visit or call anytime to see how your child is doing.”
Explanation:
The nurse’s best course of action would be to support the mother. This is best done by conveying understanding and encouraging the mother to visit or call. Telling the mother that she should not leave and that the child is very sick is critical and insensitive. Additionally, it implies guilt should the mother leave. Commenting that the child does not need anyone is not appropriate or true.
Toddlers, in particular, need family members present because of the stresses associated with hospitalization. They experience separation anxiety, a normal aspect of development, and need constancy in their environment. Asking the mother to find someone else to stay with her children is inappropriate. The children at home also need the support of the mother and/or other family members to minimize the disruptions in family life resulting from the toddler’s hospitalization and to maintain consistency.
Question 58.
A 9-month-old is admitted because of dehy-dration. How should the nurse go about accurately monitoring fluid intake and output? Select all that apply.
(a) weighing and recording all wet diapers
(b) changing breastfeedings to bottle-feedings
(c) obtaining an accurate daily weight
(d) restricting fluids prior to weighing the child
(e) obtaining an accurate stool count
Answer:
(a) weighing and recording all wet diapers
(c) obtaining an accurate daily weight
(e) obtaining an accurate stool count
Explanation:
(a), (c), (e) Accurate intake and output recording includes noting all intake, including IV fluids; noting output, such as emesis and stool; weighing diapers; measuring weight daily; measuring urine specific gravity; monitoring serum electrolytes; and monitoring for signs of dehydration.
Children who are dehydrated must receive sufficient fluid intake, but having a breastfeeding child switch to bottle-feeding will not promote intake. Restricting fluids just prior to weighing the child will not alter the accuracy of the weight, and the nurse should continue to encourage fluids for this dehydrated child.
Question 59.
The health care provider (HCP) prescribes intravenous fluid replacement therapy with potas¬sium chloride to be added for a child with severe gastroenteritis. Before the nurse hangs the IV fluids with potassium chloride, which assessments would be most important?
(a) ability to void
(b) passage of stool today
(c) baseline electrocardiogram
(d) serum calcium level
Answer:
(a) ability to void
Explanation:
Potassium chloride is readily excreted in the urine. Before hanging IV fluids with potassium chloride, the nurse should ascertain whether the child can void; if not, potassium chloride may build up in the serum and cause hyperkalemia. An electrocardiogram could be done during intravenous potassium replacement therapy to evaluate for these changes. Having a stool daily is important, but because potassium is primarily excreted in the urine, the child’s ability to void must be verified. Serum calcium levels do not indicate the child’s ability to tolerate potassium replacement.
Question 60.
Which finding would alert the nurse to suspect that a child with severe gastroenteritis who has been receiving intravenous therapy for the past several hours may be developing circulatory overload?
(a) a drop in blood pressure
(b) change to slow, deep respirations
(c) auscultation of moist crackles
(d) marked increase in urine output
Answer:
(c) auscultation of moist crackles
Explanation:
An early sign of circulatory overload is moist rales or crackles heard when auscultating over the chest wall. Elevated blood pressure, engorged neck veins, a wide variation between fluid intake and output (with a higher intake than output), shortness of breath, increased respiratory rate, dyspnea, and cyanosis occur later.
Question 61.
The stool culture of a child with profuse diarrhea reveals Salmonella bacilli. After the nurse teaches the parent about the course of Salmonella, which statement by the parent indicates effective teaching?
(a) “Some people become carriers and stay infectious for a long time.”
(b) “After the acute stage passes, the organism is usually not present in the stool.”
(c) “Although the organism may be alive indefinitely, in time it will be of no danger to anyone.”
(d) “If my child continues to have the organism in the stool, an antitoxin can help destroy the organism.”
Answer:
(a) “Some people become carriers and stay infectious for a long time.”
Explanation:
After having S. enteritidis, some clients become chronic carriers of the causative organism and remain infectious for a long time as the organism continues to be shed from the body. During this time, the child is still considered infectious. No antitoxin is available to treat or prevent Salmonella infections.
Question 62.
A child undergoes rehydration therapy after having diarrhea and dehydration. A nurse is teaching the child’s parents about dietary management after rehydration. The nurse understands that the teaching plan has been successful when the parents tell the nurse that they will follow which type of diet?
(a) regular
(b) clear liquid
(c) full liquid
(d) soft
Answer:
(a) regular
Explanation:
Dietary management following rehydration for diarrhea and mild dehydration would include offering the child a regular diet. Following rehydration, there is no need for the child to be on a special diet, such as a clear liquid, full liquid, or soft diet.
Question 63.
When obtaining a history from the parents of a child diagnosed with diarrhea due to Salmonella, the nurse should ask the parents if the child has been exposed to which possible source of infection?
(a) nonrefrigerated custard
(b) a pet canary
(c) undercooked eggs
(d) unwashed fruit
Answer:
(c) undercooked eggs
Explanation:
Diarrhea related to Salmonella bacilli is commonly spread by raw or undercooked fowl and eggs, pet turtles, and kittens. Food poisoning caused by Staphylococcus species is commonly spread by inadequately cooked or refrigerated custards, cream fillings, or mayonnaise. Psittacosis, a respiratory illness, may be spread by canaries. Contaminated, unwashed fruit is associated with typhoid fever (caused by Salmonella typhi), a disorder rarely seen in the United States.
Question 64.
On a home visit following discharge from the hospital after treatment for severe gastroenteritis, the parent tells the nurse that a toddler answers “No!” and is difficult to manage. After discussing this further with the parent, the nurse explains that the child's behavior is most likely the result of which factor?
(a) beginning leadership skills
(b) inherited personality trait
(c) expression of individuality
(d) usual lack of interest in everything
Answer:
(c) expression of individuality
Explanation:
The “no" behavior demonstrated by a toddler is typical of this age group as the child attempts to be self-assertive as an individual. Negativism does not demonstrate an inherited personality trait or disinterest. Rather, it reflects the developmental task of establishing autonomy. The toddler is attempting to exert control over the environment. It is too early to assess leadership qualities in a toddler.
Question 65.
The parent of a toddler hospitalized for episodes of diarrhea reports that when the toddler cannot have things the way she wants, she throws her legs and arms around, screams, and cries. The mother says, “I don’t know what to do!” After the nurse teaches the parent about ways to manage this behavior, which statement by the parent indicates that the nurse’s teaching was successful?
(a) “Next time she screams and throws her legs, I’ll ignore the behavior.”
(b) “I’ll allow her to have what she wants once in a while.”
(c) “I’ll explain why she cannot have what she wants.”
(d) “When she behaves like this, I’ll tell her that she is being a bad girl.”
Answer:
(a) “Next time she screams and throws her legs, I’ll ignore the behavior.”
Explanation:
The child is demonstrating behavior associated with temper tantrums, which are relatively frequent normal occurrences during toddlerhood as the child attempts to develop a sense of autonomy. The development of autonomy requires opportunities for the child to make decisions and express individuality. Ignoring the outbursts is probably the best strategy. Doing so avoids rewarding the behavior and helps the child to learn limits, promoting the development of self-control. However, the mother should intervene in a temper tantrum if the child is likely to injure herself.
Allowing the child to have what she wants occasionally would typically add to the problems associated with temper tantrums because doing so rewards the behavior and prevents the child from developing self-control. Toddlers do not possess the capacity to understand explanations about behavior. Expressing disappointment in the child’s behavior or telling her that she is being a bad girl reinforces feelings of guilt and shame, thus interfering with the child’s ability to develop a sense of autonomy.
Question 66.
The mother of a toilet-trained toddler who was admitted to the hospital for severe gastroenteritis and subsequent dehydration and is now at home asks the nurse why the child still wets the bed.
What would be the nurse’s best response?
(a) “Hospitalization is a traumatic experience for children. Regression is common, and it takes time for them to return to their former behavior.”
(b) “The stress of hospitalization is hard for many children, but usually they have no problems when they return home.”
(c) “After returning home from being hospitalized, children still feel they should be the center of attention.”
(d) “Children do not feel comfortable in their home surroundings once they return home from being hospitalized. "
Answer:
(a) “Hospitalization is a traumatic experience for children. Regression is common, and it takes time for them to return to their former behavior.”
Explanation:
Hospitalization is a traumatic time for a child, and it takes some time to readjust to the home environment. The child may regress at home for a period until she feels comfortable. Children normally do not dislike their home environment; in fact, they usually are eager to get home to familiar surroundings where they feel safe.
Question 67.
An adolescent is being seen in the clinic for abdominal pain with a fever. In what order should the nurse assess the abdomen? All options must be used.
Answer:
Explanation:
(b), (a), (c), (d) The nurse should first inspect the abdomen for abnormalities. Auscultation should be done before percussion and palpation as vigorous touching may disturb the intestines. Percussion is next. Palpation is the last step as it is most likely to cause pain.
Question 68.
The pediatric client with suspected appendicitis presents with a fever and abdominal pain. Which area should the nurse assess to determine if the pain is localized at McBurney’s point?
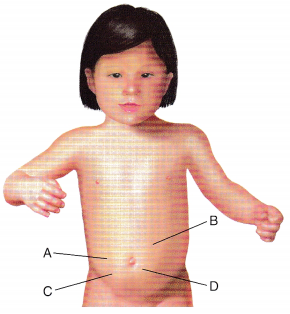
(a) A
(b) B
(c) C
(d) D
Answer:
(c) C
Explanation:
Appendicitis starts as vague abdominal pain. As the disease progresses over the course of a few hours, the pain localizes at McBurney’s point midway between the right iliac crest and the umbilicus.
Question 69.
A child is admitted with constipation and a diagnosis of possible appendicitis. The child is in acute pain. Which nursing interventions would be appropriate prior to surgery to decrease pain? Select all that apply.
(a) Offer an ice pack.
(b) Apply a heating pad.
(c) Assume a position of comfort.
(d) Limit the child’s activity.
(e) Request a prescription for a cathartic.
Answer:
(a) Offer an ice pack.
(c) Assume a position of comfort.
(d) Limit the child’s activity.
Explanation:
(a), (c), (d) Cold is a vasoconstrictor and sup-plies some degree of anesthesia. The child is usually more comfortable on his side with his legs flexed to take the strain off the inflamed appendix. Limiting the child’s activity puts less stress on the inflamed appendix and lessens the discomfort.
Heat increases circulation to an area, causing more engorgement and pain and, possibly, rupture of the appendix. Heat is contraindicated in any situation where rupture or perforation is a possibility. A cathartic is contraindicated when appendicitis is suspected. Increasing peristalsis can cause the appendix to rupture.
Question 70.
A 10-year-old male is 24 hours postappen dectomy. He is awake, alert, and oriented. He tells the nurse that he is experiencing pain. He has a prescription for morphine 1 to 2 mg PRN for pain. What is the priority nursing action in managing the child’s pain?
(a) Change the child’s position in bed.
(b) Obtain vital signs with a pain score.
(c) Administer 1 mg morphine as prescribed.
(d) Perform a head-to-toe assessment.
Answer:
(b) Obtain vital signs with a pain score.
Explanation:
The child is in pain and needs intervention, but before the nurse can determine how to proceed, it is essential to know the client’s pain score to determine the appropriate morphine dose. In addition, the nurse cannot evaluate the effectiveness of the pain medication if there is no pain score prior to administering the medication.
Changing the child’s position and administering pain medication may be helpful to relieve the child’s pain, but the nurse must first know the severity of the pain before determining the appropriate intervention. The nurse must perform a head-to-toe assessment, but it is not the priority in managing the child’s pain.
Question 71.
A typically developing preschool child is experiencing pain after an appendectomy. Which data collection tool is the most appropriate for the nurse to use to assess the pain?
(a) visual analog scale
(b) FLACC scale
(c) numerical pain scale
(d) FACES pain rating scale
Answer:
(d) FACES pain rating scale
Explanation:
The nurse should use the FACES pain rating scale for children aged 3 or older. The visual analog and numerical scales are used preferred with adults or older children who count well. The faces, legs, activity, cry, consolability (FLACC) scale is a behavioral scale that is appropriate for very small children or nonverbal children.
Question 72 .
A 7-year-old has had an appendectomy on November 12. He has had pain for the last 24 hours. There is a prescription to administer acetaminophen with codeine every 3 to 4 hours as needed. The nurse is beginning the shift, and the child is requesting pain medication. The nurse reviews the chart below for pain history. Based on the information in the medical record, what should the nurse do next?
|
Date |
Time |
Progress Notes |
|
11/12 |
1500 |
Tylenol with Codeine given PO. FACES pain scale changed from 5 to 2 within 15 minutes |
|
11/12 |
1800 |
Tylenol with Codeine given PO. FACES pain scale changed from 5 to 2 |
|
11/12 |
21300 |
Tylenol with Codeine given PO. FACES pain scale changed from 5 to 2 |
|
11/13 |
0100 |
Tylenol with Codeine given PO. FACES pain scale changed from 4 to 1 |
|
11/13 |
0700 |
Client rates pain on FACES pain scale as 4 |
(a) Administer the acetarninophen with codeine.
(b) Distract the child by giving him breakfast.
(c) Instruct the child to take deep breaths and blow his pain away.
(d) Assess the child again in 1 hour.
Answer:
(c) Instruct the child to take deep breaths and blow his pain away.
Explanation:
The nurse should administer the acetaminophen with codeine because the client indicates he is having pain. Although the child reports less severe pain, he is still experiencing pain. The nurse will also want the child to have less pain because he will need to be more active during the day. Assessing the child later will likely cause the pain to have increased and be more difficult to manage. While distraction is appropriate for short-term pain, such as from a needlestick or pain that the child might be able to manage himself, postoperative pain should be relieved with medication.
Question 73.
When the nurse is obtaining the initial health history from a 10-year-old child with abdomi¬nal pain and suspected appendicitis, which question would be most helpful in eliciting data to help support the diagnosis?
(a) “Where did the pain start?”
(b) “What did you do for the pain?”
(c) “How often do you have a bowel movement?”
(d) “Is the pain continuous, or does it let up?”
Answer:
(a) “Where did the pain start?”
Explanation:
The most helpful question would be to determine the location of the pain when it started. The pain associated with appendicitis usually begins in the periumbilical area and then progresses to the right lower quadrant. After the nurse has determined the location of the pain, asking about what was done for the pain would be appropriate. Asking about the child’s usual bowel movement pattern is a general question unrelated to child’s condition.
Children with appendicitis may have diarrhea or constipation. Additionally, knowledge about the child’s usual pattern would not be a priority because the child with appendicitis typically is not hospitalized long enough to reestablish the normal pattern. Although the characteristics of the pain are important, asking if the pain is continuous or intermittent is vague and general because the pain could be associated with numerous conditions. With appendicitis, the client’s pain may begin as intermittent, but it eventually becomes continuous.
Question 74.
When developing the plan of care for a school-age child with a suspected diagnosis of appendicitis who has severe abdominal pain, the nurse should expect to include which measure in the child’s plan of care?
(a) application of a heating pad
(b) insertion of a rectal tube
(c) application of an ice bag
(d) administration of an intravenous narcotic
Answer:
(c) application of an ice bag
Explanation:
Application of an ice bag may help to relieve pain by decreasing circulation to the area. A heating pad is contraindicated because heat may increase circulation to the appendix, possibly leading to rupture. Rectal tubes are contraindicated because they stimulate bowel motility and can exacerbate abdominal pain. Also, they would be ineffective because accumulation of gas in the lower bowel is not likely to be the cause of the child’s discomfort. Because narcotics can mask the child’s symptoms, such as pain and discomfort, and they also decrease bowel motility, they are not given until after a definitive diagnosis has been made.
Question 75.
Which assessment finding should alert the nurse to suspect appendicitis in a male adolescent with severe abdominal pain?
(a) The abdomen appears slightly rounded.
(b) Bowel sounds are heard twice in 2 minutes.
(c) All four abdominal quadrants reveal tympany.
(d) The client demonstrates a cremasteric reflex.
Answer:
(b) Bowel sounds are heard twice in 2 minutes.
Explanation:
Manifestations of appendicitis include decreased or absent bowel sounds. Normally, bowel sounds are heard every 10 to 30 seconds. Therefore, bowel sounds heard twice in 2 minutes suggests appendicitis. Normally, the contour of the male adolescent abdomen is flat to slightly rounded, and tympany is typically heard when auscultating over most of the abdomen. A cremasteric reflex is normal for male adolescents.
Question 76.
An adolescent client scheduled for an emergency appendectomy is to be transferred directly from the emergency department to the operating room. Which statement by the client should the nurse interpret as most significant?
(a) “All of a sudden, it does not hurt at all.”
(b) “The pain is centered around my navel.”
(c) “I feel like I am going to throw up.”
(d) “It hurts when you press on my stomach.”
Answer:
(a) “All of a sudden, it does not hurt at all.”
Explanation:
Sudden relief of pain in a client with appendicitis may indicate that the appendix has ruptured. Rupture relieves the pressure within the appendix but spreads the infection to the peritoneal cavity. Periumbilical pain (pain centered around the navel), vomiting, and abdominal tenderness on palpation are common findings associated with appendicitis.
Question 77.
A nurse admits a pediatric client weighing 11.6 kg at the time of surgery for appendicitis. The nurse reviews the unit’s standing prescription for IV fluids rates (see exhibit). At what hourly rate would the nurse set the IV pump? Round to whole numbers.
- Start an IV of lactated Ringers.
- Run infusion at: (loo mL for each of the first 10 kg) + (50 mL for each kg 11-20) + (20 mL for each additional kg beyond 20)124 hours.
(a) Administer the acetaminophen with codeine.
(b) Distract the child by giving him breakfast.
(c) Instruct the child to take deep breaths and blow his pain away.
(d) Assess the child again in 1 hour.
Answer:
45 mL/h.
Explanation:
The nurse must first calculate the daily fluid requirements for a client weighing 11.6 kg. The daily maintenance fluid volume is divided by 24 hours.
100 mL x 10 kg = 1,000 mL
50 mL x 1.6 kg = 80 mL
1,000 + 80 = 1,080 mL 1,080 mL/24 hours = 45 mL/h
Question 78.
What should be the priority assessment for an adolescent on return to the nursing unit after an appendectomy?
(a) the dressings on the surgical sites
(b) intravenous fluid infusion site
(c) nasogastric (NG) tube function
(d) amount of pain
Answer:
(a) the dressings on the surgical sites
Explanation:
The priority assessment after an appendectomy would be the dressing over the surgical site to determine whether there is any drainage or bleeding. If the procedure was done laparoscopically, there may be more than one incision. Any surgical dressings should be clean, dry, and intact. Once the dressing has been assessed, the nurse would assess the intravenous infusion site, assess the NG tube to be sure it is functioning, and finally, determine the degree of pain the client is experiencing.
Question 79.
An adolescent who has had an appendectomy and developed peritonitis has nausea. Which intervention should the nurse do first?
(a) Administer an antiemetic.
(b) Irrigate the nasogastric (NG) tube.
(c) Notify the surgeon.
(d) Take the blood pressure.
Answer:
(b) Irrigate the nasogastric (NG) tube.
Explanation:
After an appendectomy, the client who develops peritonitis typically has an NG tube in place. When a client has nausea, the nurse would first check to ensure that the NG tube is functioning correctly because the client’s nausea may be related to a blockage of the NG tube. If the tube is clogged, it can be irrigated with normal saline. An antiemetic may be given, but only after the nurse has determined that the NG tube is functioning properly.
Postoperative prescriptions usually include an antiemetic. Typically, the nurse would notify the surgeon if the client did not obtain relief from irrigation of the NG tube or administration of a prescribed antiemetic. Although taking the client’s blood pres¬sure is an important postoperative nursing activity, it is unrelated to relieving the client’s nausea.
Question 80.
When developing the postoperative plan of care for an adolescent who has undergone an appendectomy for a ruptured appendix, in which position should the nurse expect to place the client during the early postoperative period?
(a) semi-Fowler’s position
(b) supine
(c) lithotomy position
(d) prone
Answer:
(a) semi-Fowler’s position
Explanation:
After an appendectomy for a ruptured appendix, assuming semi-Fowler’s or a right side- lying position helps localize the infection. These positions promote drainage from the peritoneal cavity and decrease the incidence of sub diaphragmatic abscess.
Question 81.
What would the nurse expect as a normal response from an adolescent who has just returned to her room after an open appendectomy?
(a) “I will need plastic surgery for this scar.”
(b) “I am worried about the size of my scar.”
(c) “I do not want to have any pain.”
(d) “What will my boyfriend say about the scar?”
Answer:
(b) “I am worried about the size of my scar.”
Explanation:
Adolescents are concerned about the immediate state and functioning of their bodies. The adolescent needs to know whether any changes (e.g., illness, trauma, surgery) will alter her lifestyle or interfere with her quest for physical perfection. Having a scar may be devastating to the adolescent. The need for plastic surgery cannot be determined at this point. The adolescent has just returned from surgery and has yet to see the scar. Healing has yet to occur. Typically, scars become smaller and fade over time.
The desire for no pain is unrealistic. Although adolescents are worried about pain and how they will respond, they typically are discharged within 24 hours after an appendectomy with pain well controlled by oral analgesics. The immediate concern of adolescents is the state and functioning of their bodies. After concerns about themselves, adolescents are concerned about their peer group and their responses. Although the boyfriend’s response will matter, this concern will be more common later in the course of the adolescent’s recovery.
Question 82.
Which client action would the nurse judge to be a healthy coping behavior for a male adolescent after an appendectomy?
(a) insisting on wearing a T-shirt and gym shorts rather than pajamas
(b) avoiding interactions with other adolescents on the nursing unit
(c) refusing to fill out the menu and allowing the nurse to do so
(d) not taking telephone calls from friends so he can rest
Answer:
(a) insisting on wearing a T-shirt and gym shorts rather than pajamas
Explanation:
Adolescents struggle for independence and identity, needing to feel in control of situations and to conform to peers. Control and conformity are often manifested in appearance, including clothing, and this carries over into the hospital experience. The adolescent feels best when he is able to look and act as he normally does, for example, wearing a T-shirt and gym shorts.
Adolescents normally want to interact with peers and commonly seek every opportunity to do so. Avoiding other adolescents on the nursing unit or not taking phone calls from friends might suggest ineffective coping behavior. Refusing to fill out the menu and allowing the nurse to do so demonstrate dependent behavior, not a healthy coping mechanism.
Question 83.
The nurse prepares to teach an adolescent scheduled for an appendectomy about what to expect. The adolescent says, “I would rather look this up on the Internet.” What should the nurse do?
(a) Explain that completing a teaching checklist is required by the hospital.
(b) Help the client find information on the Internet.
(c) Provide the client with written information instead.
(d) Explain that information found on the Internet cannot be trusted.
Answer:
(b) Help the client find information on the Internet.
Explanation:
Part of providing client-centered care is to honor the client’s preferred method of learning. The nurse should help the adolescent find accurate information about the procedure. By assisting with the information search, the nurse can verify learning. Teaching straight from a checklist does not encourage customization.
If the client has requested to use the Internet, it is unlikely that written information will be read. While it is true that some information on the Internet is not accurate, the nurse can take this opportunity to help the client learn how to determine if a source is reliable.
Question 84.
The health care team has noticed an increase in IV infiltrations on the pediatric floor. As part of a “Plan, Do, Study, Act” quality improvement plan, the team should perform the actions in which order? All options must be used.
(a) Analyze the data.
(b) Decide to monitor IV gauges.
(c) Perform chart audits.
(d) Write a new IV insertion policy gauges.
Answer:
(b) Decide to monitor IV gauges.
(a) Analyze the data.
(c) Perform chart audits.
(d) Write a new IV insertion policy gauges.
Explanation:
(b), (a), (c), (d) Deciding what to study and how to do it is part of the planning process. Collecting data through chart audits is part of the “do” phase. Once the chart audits are complete, the data may be “studied” or analyzed. The final step of the process, or the “act” phase, is to determine what should be done, which may include writing a new policy.
Question 85.
The nurse works with the health care team to establish a policy regarding sleep positions for infants with gastroesophageal reflux. What information should the nurse search for first?
(a) policies from other hospitals
(b) data from retrospective studies
(c) published national standards
(d) expert opinions
Answer:
(c) published national standards
Explanation:
Published national standards are based on the best evidence and, when available, should serve as the foundation for nursing unit policies. Policies from other hospitals may or may not be evidence-based. Retrospective studies and expert opinions should only be used to form policy when data from experimental studies or national standards are not available.
Question 86.
The nurse is assisting another member of the health care team who is placing a peripherally inserted central catheter in a 10-year-old with peritonitis from a ruptured appendix. The family is present in the treatment room to support the child. The nurse observes that the other team member has contaminated a sterile glove. What should the nurse do next?
(a) Discuss the incident with the team member after the event.
(b) Report the incident to the nursing unit manager.
(c) Tell the team member the glove is contaminated.
(d) Ask the family to leave before confronting the team member.
Answer:
(c) Tell the team member the glove is contaminated.
Explanation:
It is the responsibility of all healthcare members to protect the client. The team member may honestly not have realized that the glove was contaminated. Therefore, the nurse needs to alert the team member to the situation. Waiting until after the procedure to address the problem puts the child at unnecessary risk for infection. Asking the parents to leave could invoke anxiety in both the child and the parents. Alerting the team member does not need to be confrontational. If done with a calm approach, the result is most likely to be gratitude instead of embarrassment.
Question 87.
The hospital is responding to a mass casualty disaster with adult and pediatric victims. What should the charge nurse on the pediatric floor do after reallocating staff?
(a) Ask parents to leave to free up areas for incoming victims.
(b) Review the census for candidates for early discharge.
(c) Initiate paper charting backup.
(d) Change taking all vital signs to every 8 hours.
Answer:
(b) Review the census for candidates for early discharge.
Explanation:
The charge nurse can anticipate needing beds for incoming victims. Any client who can go home should go home. Parents are a child’s primary caregivers and should not be asked to leave. If computers had not been affected by the disaster, charting in the electronic health record would have been safer. Some routine procedures are altered during a disaster, but clients who are unstable will still need frequent assessments; reducing vital sign frequency must be considered on a case-to-case basis.
Question 88.
Eight hours ago, an infant with Hirschsprung’s disease had surgery to create a colostomy. Which finding should alert the nurse to notify the health care provider (HCP) immediately?
(a) a 3-cm increase in abdominal circumference
(b) periods of occasional fussiness
(c) absence of bowel sounds since surgery
(d) appearance of a bright red stoma
Answer:
(a) a 3-cm increase in abdominal circumference
Explanation:
Abdominal circumference is measured to monitor for abdominal distention. An increase of 3 cm in 8 hours would require notification of the HCP; it would indicate a substantial degree of abdominal distention, possibly from fluid or gas accumulation. Normally, after surgery, an infant experiences occasional periods of fussiness.
However, as long as the infant is able to be quiet by himself or with the aid of a pacifier, the HCP does not need to be contacted. Absence of bowel sounds would be expected after surgery because of the effects of anesthesia. It takes approximately 48 hours for gastric motility to resume. New stomas are typically bright red or pink.
Read More:
Child With Cardiovascular and Haematologic Health Nclex Questions