Many nursing schools and review courses offer structured study plans that include specific sets of NCLEX PN Study Guide for each topic.
NCLEX Hematologic Health Problems Questions
Hematologic Health Problems NCLEX Practice Questions
Question 1.
The nurse is assisting with a bone marrow aspiration and biopsy. In which order, from first to last, should the nurse complete these tasks? All options must be used.
(a) Position the client in a side-lying position.
(b) Clean the skin with an antiseptic solution.
(c) Verify the client has signed an informed consent.
(d) Apply ice to the biopsy site.
Answer:
(c) Verify the client has signed an informed consent.
(a) Position the client in a side-lying position.
(b) Clean the skin with an antiseptic solution.
(d) Apply ice to the biopsy site.
Explanation:
(c), (a), (b), (d). First, the nurse must verify that the client has voluntarily signed a consent form before the procedure begins and check that the client understands the procedure. The nurse then positions the client in a side-lying, or lateral decubitus, position with the affected side up. Then, the nurse should clean the skin site and surrounding area with an antiseptic solution before the health care provider (HCP) numbs the site and collects the specimen. When the procedure is finished, the nurse must apply ice to the biopsy site to reduce pain.
Question 2.
A client with iron deficiency anemia is refusing to take the prescribed oral iron medication because the medication is causing nausea; the client is also constipated. What actions should the nurse take? Select all that apply.
(a) Suggest that the client use ginger when taking the medication.
(b) Ask the client what is causing the nausea.
(c) Tell the client to use stool softeners to minimize constipation.
(d) Offer to administer the medication by an intramuscular injection.
(e) Suggest that the client take the iron with orange juice.
Answer:
(a) Suggest that the client use ginger when taking the medication.
(b) Ask the client what is causing the nausea.
(d) Offer to administer the medication by an intramuscular injection.
Explanation:
Nausea and vomiting are common adverse effects of oral iron preparations. The nurse should first ask the client why the client does not want to take the oral medication and then suggest ways to decrease the nausea and vomiting. Ginger may help minimize the nausea, and the client can try this remedy and evaluate its effectiveness.
Iron should be taken on an empty stomach but can be taken with orange juice. The client can evaluate if this helps the nausea. Stool softeners should not be used in clients with iron deficiency anemia. Instead, constipation can be prevented by following a high- fiber diet. Administering iron intramuscularly is done only if other approaches are not effective.
Question 3.
A client had a mastectomy followed by chemotherapy 6 months ago. She reports that she is now “unable to concentrate at her card game” and “it seems harder and harder to finish my errands because I am so tired.” What should the nurse suggest that the client do to manage the exhaustion?
(a) Take frequent naps.
(b) Limit activities.
(c) Increase fluid intake.
(d) Avoid contact with others.
Answer:
(a) Take frequent naps.
Explanation:
This client is likely experiencing fatigue and should increase periods of rest. The fatigue may be caused by anemia from depletion of red blood cells due to the chemotherapy. Asking the client to limit her activities may cause the client to become withdrawn. The information given does not support limiting activity. Increasing fluid intake will not reduce the fatigue. The information does not indicate that the client is immunosuppressed and should avoid contact with others.
Question 4.
A client is to have a transfusion of packed red blood cells from a designated donor. The client asks if any diseases can be transmitted by this donor. The nurse should inform the client that which diseases can be transmitted by a designated donor? Select all that apply.
(a) Epstein-Barr virus
(b) human immunodeficiency virus (HIV)
(c) cytomegalovirus (CMV)
(d) hepatitis A
(e) malaria
Answer:
(a) Epstein-Barr virus
(b) human immunodeficiency virus (HIV)
(c) cytomegalovirus (CMV)
Explanation:
(a), (b), (c). Using designated donors does not decrease the risk of contracting infectious diseases, such as the Epstein-Barr vims, HIV, or CMV. Hepatitis A is transmitted by the oral-fecal route, not the blood route; however, hepatitis B and C can be contracted from a designated donor. Malaria is transmitted by mosquitoes.
Question 5.
The nurse is preparing to teach a client with iron deficiency anemia about the diet to follow after discharge. Which food should be included in the diet?
(a) eggs
(b) lettuce
(c) citrus fruits
(d) cheese
Answer:
(a) eggs
Explanation:
For the client with iron deficiency anemia, a rich source of iron is needed in the diet, and eggs are high in iron. Other foods high in iron include organ and muscle (dark) meats; shellfish, shrimp, and tuna; enriched, whole-grain, and fortified cereals and breads; legumes, nuts, dried fruits, and beans; oatmeal; and sweet potatoes. Dark green, leafy vegetables and citrus fruits are good sources of vitamin C. Cheese is a good source of calcium.
Question 6.
The nurse should instruct the client with vitamin B12 deficiency to eat which foods to obtain the best supply of vitamin B12?
(a) whole grains
(b) green leafy vegetables
(c) meats and dairy products
(d) broccoli and Brussels sprouts
Answer:
(c) meats and dairy products
Explanation:
Good sources of vitamin B12 include meats and dairy products. Whole grains are a good source of thiamine. Green, leafy vegetables are good sources of niacin, folate, and carotenoids (precursors of vitamin A). Broccoli and Brussels sprouts are good sources of ascorbic acid (vitamin C). adds iron to the diet. Clients are instructed to add a rich supply of vitamin C to every meal because the absorption of iron is increased when food with vitamin C or ascorbic acid is consumed.
Question 7.
Which lab values should the nurse report to the health care provider (HCP) when the client has anemia?
(a) Schilling test result, elevated
(b) intrinsic factor, absent
(c) sedimentation rate, 16 mm/h
(d) red blood cells (RBCs) within normal range
Answer:
(b) intrinsic factor, absent
Explanation:
The defining characteristic of pernicious anemia, a megaloblastic anemia, is lack of the intrinsic factor, which results from atrophy of the stomach wall. Without the intrinsic factor, vitamin B12 cannot be absorbed in the small intestine, and folic acid needs vitamin B12 for deoxyribonucleic acid synthesis of RBCs. The gastric analysis is done to determine the primary cause of the anemia.
An elevated excretion of the injected radioactive vitamin B12, which is protocol for the first and second stages of the Schilling test, indicates that the client has the intrinsic factor and can absorb vitamin B12 in the intestinal tract. A sedimentation rate of 16 mm/h is normal for both men and women and is a nonspecific test to detect the presence of inflammation; it is not specific to anemias. An RBC value within the normal range does not indicate an anemia.
Question 8.
The nurse is developing a teaching plan for the client with aplastic anemia. Which is most important to include in the plan?
(a) Eat animal protein and dark green, leafy veg etables every day.
(b) Avoid exposure to others with acute infections.
(c) Practice yoga and meditation to decrease stress and anxiety.
(d) Get 8 hours of sleep at night, and take naps during the day.
Answer:
(b) Avoid exposure to others with acute infections.
Explanation:
Clients with aplastic anemia are severely immunocompromised and at risk for infection and possible death related to bone marrow suppression and pancytopenia. Strict aseptic technique and reverse isolation are important measures to prevent infection. Although diet, reduced stress, and rest are valued in supporting health, the potentially fatal consequence of an acute infection places it as a priority for teaching the client about health mainte-nance. Animal meat and dark green leafy vegetables, good sources of vitamin B12 and folic acid, should be included in the daily diet. Yoga and meditation are good complementary therapies to reduce stress. Eight hours of rest and naps are good for spacing and pacing activity and rest.
Question 9.
A client had a resection of the terminal ileum 3 years ago. While obtaining a health history and physical assessment, the nurse finds that the client has weakness, shortness of breath, and a sore tongue. Which additional information from the client indicates a need for client teaching?
(a) “I have been drinking plenty of fluids.”
(b) “I have been gargling with warm salt water for my sore tongue.”
(c) “I have regular bowel movements on most days.”
(d) “I take a vitamin B12 tablet every day.”
Answer:
(d) “I take a vitamin B12 tablet every day.”
Explanation:
Vitamin B12 combines with intrinsic factor in the stomach and is then carried to the ileum, where it is absorbed into the bloodstream. In this situation, vitamin B12 cannot be absorbed regardless of the amount of oral intake of sources of vitamin B12, such as animal protein or vitamin B12 tablets. Vitamin B12 needs to be injected every month because the ileum has been surgically removed. Warm salt water is used to soothe sore mucous membranes. Crohn’s disease and a small-bowel resection may cause several loose stools a day, but the client does not report having this problem.
Question 10.
A client who follows a vegetarian diet was referred to a dietitian for nutritional counseling for anemia. Which client outcome indicates that the client needs further nutritional counseling?
(a) The client adds dried fruit to cereal and baked goods.
(b) The client cooks tomato-based foods in iron pots.
(c) The client drinks coffee or tea with meals.
(d) The client adds vitamin C to all meals.
Answer:
(c) The client drinks coffee or tea with meals.
Explanation:
Coffee and tea increase gastrointestinal motility and inhibit the absorption of nonheme iron. Clients are instructed to add dried fruits to dishes at every meal because dried fruits are a nonheme or nonanimal iron source. Cooking in iron cookware, especially acid-based foods such as tomatoes, adds iron to the diet. Clients are instructed to add a rich supply of vitamin C to every meal because the absorption of iron is increased when food with vitamin C or ascorbic acid is consumed.
Question 11.
A client was admitted to the hospital with iron deficiency anemia and blood-streaked emesis. Which question is most appropriate for the nurse to ask in determining the extent of the client’s activity intolerance?
(a) “What daily activities were you able to do 6 months ago compared with the present?”
(b) “How long have you had this problem?”
(c) “Have you been able to keep up with all your usual activities?”
(d) “Are you more tired now than you used to be?”
Answer:
(a) “What daily activities were you able to do 6 months ago compared with the present?”
Explanation:
It is difficult to determine activity intolerance without objectively comparing activities from one time frame to another. Because iron deficiency anemia can occur gradually and individual endurance varies, the nurse can best assess the client’s activity tolerance by asking the client to compare activities 6 months ago and at present. Asking a client how long a problem has existed is a very open- ended question that allows for too much subjectivity for any definition of the client’s activity tolerance. Also, the client may not even identify that a “problem” exists.
Asking the client whether he is staying abreast of usual activities addresses whether the tasks were completed, not the tolerance of the client while the tasks were being completed or the resulting condition of the client after the tasks were completed. Asking the client about being more tired now than usual does not address activity tolerance. Tiredness is a subjective evaluation and again can be distorted by factors such as the gradual onset of the anemia or the endurance of the individual.
Question 12.
A health care provider (HCP) prescribes vitamin B12 for a client with pernicious anemia. Which sites are appropriate for the nurse to administer vitamin B12 to an adult? Select all that apply.
(a) median cutaneous
(b) greater femur trochanter
(c) acromion muscle
(d) ventrogluteal
(e) upper back
(f) dorsogluteal
Answer:
(d) ventrogluteal
(f) dorsogluteal
Explanation:
(d), (f). A client with pernicious anemia has lost the ability to absorb vitamin B12 either because of the lack of an acidic gastric environment or the lack of the intrinsic factor. Vitamin B12 must be administered by a deep intramuscular route. The ventrogluteal and dorsogluteal locations are the most acceptable sites for a deep intramuscular injection. The other sites are not acceptable.
Question 13.
When administering an injection of Vitamin B12, in which position should the nurse place the client that will decrease discomfort when injecting the medication in the ventrogluteal site?
(a) lying on the side with legs extended
(b) lying on the abdomen with toes pointed inward
(c) leaning over the edge of a low table with hips flexed
(d) standing upright with the feet one shoulder-width apart
Answer:
(b) lying on the abdomen with toes pointed inward
Explanation:
To promote comfort when injecting at the ventrogluteal site, the position of choice is with the client lying on the abdomen with toes pointed inward. This positioning promotes muscle relaxation, which decreases the discomfort of making an injection into a tense muscle. Lying on the side with legs extended will not provide the greatest muscle relaxation. Leaning over the edge of a table with the hips flexed and standing upright with the feet apart will increase muscular tension.
Question 14.
A client is admitted from the emergency department after falling down a flight of stairs at home. The client’s vital signs are stable, and the history states that the client had a gastric stapling 2 years ago. The client jokes about being clumsy lately and tripping over things. The nurse should gather additional information by asking the client which questions? Select all that apply.
(a) “Are you experiencing numbness in your extremities?”
(b) “How much vitamin B12 are you getting?”
(c) “Are you feeling depressed?”
(d) “Do you feel safe at home?”
(e) “Are you getting sufficient iron in your diet?”
Answer:
(a) “Are you experiencing numbness in your extremities?”
(b) “How much vitamin B12 are you getting?”
(c) “Are you feeling depressed?”
(d) “Do you feel safe at home?”
Explanation:
(a), (b), (c), (d). The nurse should ask the client about symptoms related to pernicious anemia because the client had the stomach stapled 2 years ago and shows no history of supplemental vitamin B12. Numbness and tingling relate to a loss of intrin sic factor from the gastric stapling. Intrinsic factor is necessary for absorption of vitamin B12. The nurse should suspect pernicious anemia if the client is not taking supplemental vitamin B12. Other signs and symptoms of pernicious anemia include cognitive problems and depression. The nurse also should ask about the client’s support at home in case the fall was not an accident. Pernicious anemia is not related to dietary intake of iron.
Question 15.
A client has fatigue, temperature of 99.5°F (37.5°C), dark bronze skin, and dark urine. Hemoglobin is 9 g/dL (90 g/L); hematocrit is 49 (0.49). What should the nurse do first?
(a) Start an intake and output record.
(b) Place the client on bed rest.
(c) Initiate contact precautions.
(d) Keep the client out of sunlight.
Answer:
(a) Start an intake and output record.
Explanation:
The nurse should prepare to start an intake and output record because the client is exhibiting clinical manifestations of anemia with jaundice and is demonstrating a fluid imbalance. The client does not need to be on bed rest at this point. The client is not contagious and does not require contact precautions. The changes in the color of the skin and urine are related to the jaundice and will not be affected by sunlight.
Question 16.
When a client is receiving a cephalosporin, the nurse should monitor the client for which finding?
(a) drug-induced hemolytic anemia
(b) purpura
(c) infectious emboli
(d) ecchymosis
Answer:
(a) drug-induced hemolytic anemia
Explanation:
Drug -induced hemolytic anemia is acquired, antibody-mediated, red blood cell destruction precipitated by medications, such as cephalosporins, sulfa drugs, rifampin, methyldopa, procainamide, quinidine, and thiazides. Purpura is a condition with various manifestations characterized by hemorrhages into the skin, mucous membranes, internal organs, and other tissues. Infectious emboli are clumps of bacteria present in blood or lymph. Ecchymoses are skin discolorations due to extravasations of blood into the skin or mucous membranes.
Question 17.
A client is to have a Schilling’s test. How should the nurse prepare the client for this test?
(a) Administer methylcellulose.
(b) Start a 24- to 48-hour urine specimen collection.
(c) Maintain nothing-by-mouth (NPO) status.
(d) Start a 72-hour stool specimen collection.
Answer:
(b) Start a 24- to 48-hour urine specimen collection.
Explanation:
Urinary vitamin B12 levels are measured after the ingestion of radioactive vitamin B12. A 24- to 48-hour urine specimen is collected after administration of an oral dose of radioactively tagged vitamin B12 and an injection of nonradioactive vitamin B12. In a healthy state of absorption, excess vitamin B12 is excreted in the urine; in a malabsorptive state or when the intrinsic factor is missing, vitamin B12 is excreted in the feces. Methylcellulose is a bulkforming agent. Laxatives interfere with the absorption of vitamin B12. The client is NPO 8 to 12 hours before the test but is not NPO during the test. A stool collection is not a part of the Schilling test. If stool contaminates the urine collection, the results will be altered.
Question 18.
A client with pernicious anemia is receiving vitamin B12. The nurse should evaluate the client for which expected outcome of vitamin B12?
(a) increased energy
(b) healed tongue and lips
(c) absence of paresthesias
(d) improved clotting time
Answer:
(c) absence of paresthesias
Explanation:
Pernicious anemia is caused by a lack of vitamin B12. Primary symptoms include neuropathy with paresthesias of hands and feet. The nurse assesses the client to determine the effectiveness of the monthly dose of vitamin B12, which is to reverse the deficiency and the related symptoms. Improved energy is associated with treatment for iron deficiency anemia. Healing of cracked lips and tongue is an outcome of taking folic acid for folic acid deficiency. Delayed clotting time is associated with hemophilia; the clotting time is not affected by vitamin B12.
Question 19.
A client with pernicious anemia asks why it is necessary to take vitamin B12 injections forever. Which is the nurse’s best response?
(a) “The reason for your vitamin deficiency is an inability to absorb the vitamin because the stomach is not producing sufficient acid.”
(b) "The reason for your vitamin deficiency is an inability to absorb the vitamin because the stomach is not producing sufficient amounts of a factor that allows the vitamin to be absorbed.”
(c) “The reason for your vitamin deficiency is an excessive excretion of the vitamin because of kidney dysfunction.”
(d) “The reason for your vitamin deficiency is an increased requirement for the vitamin because of rapid red blood cell production.”
Answer:
(b) "The reason for your vitamin deficiency is an inability to absorb the vitamin because the stomach is not producing sufficient amounts of a factor that allows the vitamin to be absorbed.”
Explanation:
Most clients with pernicious anemia have deficient production of intrinsic factor in the stomach. Intrinsic factor attaches to the vitamin in the stomach and forms a complex that allows the vitamin to be absorbed in the small intestine. The stomach is producing enough acid, there is not an excessive excretion of the vitamin, and there is not a rapid production of red blood cells in this condition.
Question 20.
The nurse is assessing a client’s activity tolerance. Which report from a treadmill test indicates an abnormal response?
(a) pulse rate increased by 20 bpm immediately after the activity
(b) respiratory rate decreased by 5 breaths/min
(c) diastolic blood pressure increased by 7 mm Hg
(d) pulse rate within 6 bpm of resting pulse after 3 minutes of rest
Answer:
(b) respiratory rate decreased by 5 breaths/min
Explanation:
The normal physiologic response to activity is an increased metabolic rate over the resting basal rate. The decrease in respiratory rate indicates that the client is not strong enough to complete the mechanical cycle of respiration needed for gas exchange. The postactivity pulse is expected to increase immediately after activity but by no more than 50 bpm if it is strenuous activity. The diastolic blood pressure is expected to rise but by no more than 15 mm Hg. The pulse returns to within 6 bpm of the resting pulse after 3 minutes of rest.
Question 21.
In a postoperative client, the hematocrit decreased from 36% (0.36) to 34% (0.34) on the 3rd day even though the red blood cell (RBC) count and hemoglobin value remained stable at 4.5 million/pL (4.5 x 1012/L) and 11.9 g/dL (119 g/L), respectively. What should the nurse do next?
(a) Check the dressing and drains for frank bleeding.
(b) Call the health care provider (HCP).
(c) Continue to monitor vital signs.
(d) Start oxygen at 2 L/min per nasal cannula.
Answer:
(c) Continue to monitor vital signs.
Explanation:
The nurse should continue to monitor the client because this value reflects a normal physiologic response. The HCP does not need to be called, and oxygen does not need to be started based on these laboratory findings. Immediately after surgery, the client’s hematocrit reflects a falsely high value related to the body’s compensatory response to the stress of sudden loss of fluids and blood.
Activation of the intrinsic pathway and the renin- angiotensin cycle via antidiuretic hormone produces vasoconstriction and retention of fluid for the first 1 to 2 days postoperatively. By the 2nd to 3rd day, this response decreases, and the client’s hematocrit level is more reflective of the amount of RBCs in the plasma. Fresh bleeding is a less likely occurrence on the third postoperative day but is not impossible; however, the nurse should have expected to see a decrease in the RBC count and hemoglobin value accompanying the hematocrit.
Question 22.
The nurse is administering packed red blood cells (PRBCs) to a client. What should the nurse do first?
(a) Discontinue the IV catheter if a blood transfusion reaction occurs.
(b) Administer the PRBCs through a percutaneously inserted central catheter line with a 20-gauge needle.
(c) Flush PRBCs with 5% dextrose and 0.45% normal saline solution.
(d) Stay with the client during the first 15 min utes of infusion.
Answer:
(d) Stay with the client during the first 15 min utes of infusion.
Explanation:
The most likely time for a blood transfusion reaction to occur is during the first 15 minutes or first 50 mL of the infusion. If a blood transfusion reaction does occur, it is imperative to keep an established IV line so that medication can be administered to prevent or treat cardiovascular collapse in case of anaphylaxis. PRBCs should be administered through a 19-gauge or larger needle; a peripherally inserted central catheter line is not recommended in order to avoid a slow flow. RBCs will hemolyze in dextrose or lactated Ringer’s solution and should be infused with only normal saline solution.
Question 23.
The nurse is preparing a client with sickle cell anemia for discharge. What information should the nurse include in the teaching plan? Select all that apply.
(a) Drink plenty of fluids when outside in hot weather.
(b) Avoid being in high altitudes where less oxygen is available.
(c) Be aware that since she is homozygous for HbS, she carries the sickle cell trait.
(d) Know that pregnancy with sickle cell disease increases the risk of a crisis.
(e) Avoid flying on commercial airlines.
Answer:
(a) Drink plenty of fluids when outside in hot weather.
(b) Avoid being in high altitudes where less oxygen is available.
(d) Know that pregnancy with sickle cell disease increases the risk of a crisis.
Explanation:
(a), (b), (d). The nurse should teach the client to drink plenty of fluids to avoid becoming dehydrated. The client should avoid being in high altitudes, such as mountains above 5,000 feet (1,524 m), where less oxygen is available and may precipitate a sickle cell crisis. The nurse should alert young women with sickle cell anemia that pregnancy increases the risk of a crisis. People who are homozygous for HbS have sickle cell anemia; the heterozygous form is the sickle cell carrier trait.
A client with sickle cell anemia may fly on commercial airlines; the airplane is pressurized and has an adequate oxygen level.
Question 24.
The nurse is teaching a client newly diagnosed with hemochromomatosis about reducing risk of complications. Which information should the nurse include in the teaching plan? Select all that apply.
(a) “You should not take any iron supplements.”
(b) “Read labels on multivitamins and do not use if they contain iron.”
(c) “Increase the vitamin C in your diet by drinking more orange juice.”
(d) “Try to increase your fluid intake to 3,500 mL/day.”
(e) “You should not have drinks or medications containing alcohol.”
Answer:
(a) “You should not take any iron supplements.”
(b) “Read labels on multivitamins and do not use if they contain iron.”
(e) “You should not have drinks or medications containing alcohol.”
Explanation:
(a), (b), (e). Hemochromatosis is a heredity disease that causes the body to absorb increased amounts of iron from food, which can lead to liver and heart disease. The primary treatment is periodic removal of blood. To avoid complications, the nurse should instruct the client to not take iron supplements, vitamins with iron, or vitamin C. The client should not increase the amount of vitamin C in the diet because vitamin C promotes absorption of iron. The client should not drink alcoholic beverages in order to prevent liver damage. It is not necessary to increase the amount of fluids in the diet, but the client should not become dehydrated.
Question 25.
A client is having a blood transfusion reaction. What must the nurse do in order of priority from first to last? All options must be used.
(a) Notify the health care provider (HCP) and blood bank.
(b) Complete the appropriate transfusion reaction form(s).
(c) Stop the transfusion.
(d) Keep the IV open with normal saline infusion.
Answer:
(c) Stop the transfusion.
(d) Keep the IV open with normal saline infusion.
(a) Notify the health care provider (HCP) and blood bank.
(b) Complete the appropriate transfusion reaction form(s).
Explanation:
(c) , (d), (a), (b). When the client is having a blood transfusion reaction, the nurse should first stop the transfusion and then keep the IV open with normal saline infusion. Next, the nurse should notify the HCP and blood bank and then complete the required form(s) regarding the transfusion reaction.
Question 26.
Which safety measures would be most important to implement when caring for a client who is receiving 2 units of packed red blood cells (PRBCs)? Select all that apply.
(a) Verify that the ABO and Rh of the two units are the same.
(b) Infuse a unit of PRBCs in <4 hours.
(c) Stop the transfusion if a reaction occurs, but keep the line open.
(d) Take vital signs every 15 minutes while the unit is transfusing.
(e) Inspect the blood bag for leaks, abnormal color, and clots.
(f) Use a 22-gauge catheter for optimal flow of a blood transfusion.
Answer:
(b) Infuse a unit of PRBCs in <4 hours.
(c) Stop the transfusion if a reaction occurs, but keep the line open.
(e) Inspect the blood bag for leaks, abnormal color, and clots.
Explanation:
(b),(c), (e). The American Association of Blood Banks and Canadian Blood Services recommend that two qualified people, such as two registered nurses (RNs) P, compare the name and number on the identification bracelet with the tag on the blood bag. Verifying that the two units are the same is not a recommendation. Rather, the verification is always with the client, not with bags of blood.
A unit of blood should infuse in 4 hours or less to avoid the risk of septicemia since no preservatives are used. When a blood transfusion reaction occurs, the blood transfusion should be stopped immediately, but the IV line should be kept open so that emergency medications and fluids can be administered.
The unit of PRBCs should be inspected for contamination by looking for leaks, abnormal color, clots, and excessive air bubbles. When a unit of PRBCs is being transfused, vital signs are assessed before the transfusion begins, after the first 15 minutes and then every hour until 1 hour after the transfusion has been completed. When PRBCs are being administered, a 20-gauge or larger needle is needed to avoid destroying the RBCs passing through the lumen and to allow for maximal flow rate.
Question 27.
A client who had received 25 mL of packed red blood cells (PRBCs) has low back pain and pruritus. After stopping the infusion, the nurse should take what action next?
(a) Administer prescribed antihistamine and an antipyretic.
(b) Collect blood and urine samples and send to the lab.
(c) Administer prescribed diuretics.
(d) Administer prescribed vasopressors.
Answer:
(b) Collect blood and urine samples and send to the lab.
Explanation:
ABO- and Rh-incompatible blood causes an antigen-antibody reaction that produces hemolysis or agglutination of red blood cells (RBCs). At the first indication of any sign/symptom of reaction, the blood transfusion is stopped. Blood and urine samples are obtained from the client and sent to the lab along with the remaining untransfused blood. Hemoglobin in the urine and blood samples taken at the time of the reaction provides evidence of a hemolytic blood transfusion reaction. Antihistamine, aspirin, diuretics, and vasopressors may be administered with different types of transfusion reactions.
Question 28.
A client is to receive epoetin injections. What laboratory value should the nurse assess before giving the injection?
(a) hematocrit
(b) partial thromboplastin time
(c) hemoglobin concentration
(d) prothrombin time
Answer:
(a) hematocrit
Explanation:
Epoetin is a recombinant DNA form of erythropoietin, which stimulates the production of red blood cells and therefore causes the hematocrit to rise. The partial thromboplastin time, hemoglobin level, and prothrombin time are not monitored for this drug.
Question 29.
When beginning IV erythropoietin therapy, what actions should the muse take? Select all that apply.
(a) Check the hemoglobin levels before administering subsequent doses.
(b) Shake the vial thoroughly to mix the concentrated white, milky solution.
(c) Keep the multidose vial refrigerated between scheduled twice-a-day doses.
(d) Administer the medication through the IV line without other medications.
(e) Adjust the initial doses according to the client’s changes in blood pressure.
(f) Instruct the client to avoid driving and performing hazardous activity during the initial treatment.
Answer:
(d) Administer the medication through the IV line without other medications.
(e) Adjust the initial doses according to the client’s changes in blood pressure.
(f) Instruct the client to avoid driving and performing hazardous activity during the initial treatment.
Explanation:
(d), (e), (f). Erythropoietin is administered to decrease the need for blood transfusions by stimulating red blood cell (RBC) production. The medication should be administered through the IV line without other medications to avoid a reaction. The hematocrit, a simple measurement of the percentage of RBCs in the total blood volume, is used to monitor this therapy. When initiating TV erythropoietin therapy, the nurse should monitor the hematocrit level so that it rises no more than four points in any 2-week period.
In addition, the initial doses of erythropoietin are adjusted according to the client’s changes in blood pressure. The nurse should tell the client to avoid driving and performing hazardous activity during the initial treatment due to possible dizziness and headaches secondary to the adverse effect of hypertension. The hematocrit, not the hemoglobin level, is used for monitoring the effectiveness of therapy. The vial of erythropoietin should not be shaken because it may be biologically inactive. The solution should not be used if it is discolored. The nurse should not reenter the vial once it has been entered; it is a one-time use vial. All remaining erythropoietin should be discarded since it does not contain preservatives.
Question 30.
A client is afraid of receiving vitamin B12 injections because of potential toxic reactions. Which is the nurse’s best response to relieve these fears?
(a) “Vitamin B12 will cause ringing in the ears before a toxic level is reached.”
(b) “Vitamin B12 may cause a very mild rash initially.”
(c) “Vitamin B12 cause mild nausea but nothing toxic.”
(d) “Vitamin B12 is generally free of toxicity because it is water soluble.”
Answer:
(d) “Vitamin B12 is generally free of toxicity because it is water soluble.”
Explanation:
Vitamin B12 is a water-soluble vitamin. When water-soluble vitamins are taken in excess of the body’s needs, they are filtered through the kidneys and excreted. Vitamin B12 is considered to be nontoxic. Adverse reactions that have occurred are believed to be related to impurities or to the preservative in B12 preparations. Ringing in the ears, rash, and nausea are not considered to be related to vitamin B12 administration.
Question 31.
A client with iron deficiency anemia is having trouble selecting food from the hospital menu. Which foods should the nurse suggest to meet the client’s need for iron? Select all that apply.
(a) eggs
(b) brown rice
(c) dark green vegetables
(d) tea
(e) oatmeal
Answer:
(a) eggs
(b) brown rice
(c) dark green vegetables
(e) oatmeal
Explanation:
(a), (b), (c), (e). Eggs are a source of iron, but may not be well absorbed. Brown rice is a source of iron from plant sources (nonheme iron). Other sources of nonheme iron are whole-grain cereals and breads, dark green vegetables, legumes, nuts, dried fruits (apricots, raisins, dates), oatmeal, and sweet potatoes. Tea contains tannin, which combines with nonheme iron, preventing its absorption.
Question 32.
A client with macrocytic anemia has a burn on the foot and reports watching television while lying on a heating pad. Which action should be the nurse’s first response?
(a) Assess for potential abuse.
(b) Check for diminished sensations.
(c) Document the findings.
(d) Clean and dress the area.
Answer:
(b) Check for diminished sensations.
Explanation:
Macrocytic anemias can result from deficiencies in vitamin B12 or ascorbic acid. Only vitamin B12 deficiency causes diminished sensations of peripheral nerve endings. The nurse should assess for peripheral neuropathy and instruct the client in self-care activities for diminished sensation to heat and pain (e.g., using a heating pad at a lower heat setting, making frequent checks to protect against skin trauma). The burn could be related to abuse, but this conclusion would require more supporting data. The findings should be documented, but the nurse would want to address the client’s sensations first. The decision of how to treat the burn should be determined by the health care provider (HCP).
Question 33.
When a client is diagnosed with aplastic anemia, the nurse should assess the client for changes in which physiologic functions?
(a) bleeding tendencies
(b) intake and output
(c) peripheral sensation
(d) bowel function
Answer:
(a) bleeding tendencies
Explanation:
Aplastic anemia decreases the bone marrow production of red blood cells, white blood cells, and platelets. The client is at risk for bruising and bleeding tendencies. A change in the client’s intake and output is important, but assessment for the potential for bleeding takes priority. Change in the peripheral nervous system is a priority problem specific to clients with vitamin B12 deficiency. Change in bowel function is not associated with aplastic anemia.
Question 34.
A health care provider (HCP) prescribes 0.5 mg of protamine sulfate for a client who is showing signs of bleeding after receiving a 100-unit dose of heparin. The nurse should expect the effects of the protamine sulfate to be noted in how many minutes?
(a) 5 minutes
(b) 10 minutes
(c) 20 minutes
(d) 30 minutes
Answer:
(c) 20 minutes
Explanation:
A dose of 0.5 mg of protamine sulfate reverses a 100-unit dose of heparin within 20 minutes. The nurse should administer protamine sulfate by IV push slowly to avoid adverse effects, such as hypotension, dyspnea, bradycardia, and anaphylaxis.
Question 35.
The nurse is to administer subcutaneous heparin to an underweight older adult. What facts should the nurse keep in mind when administering this medication? Select all that apply.
(a) Administer in the anterior area of the iliac crest.
(b) The onset is immediate.
(c) Use a 27-G, 5/8-inch (1.6-mm) needle.
(d) Cephalosporin potentiates the effects of heparin.
(e) Verify the dose with another nurse according to agency policy.
Answer:
(a) Administer in the anterior area of the iliac crest.
(c) Use a 27-G, 5/8-inch (1.6-mm) needle.
(d) Cephalosporin potentiates the effects of heparin.
(e) Verify the dose with another nurse according to agency policy.
Explanation:
(a), (c), (d), (e)Underweight older adults may have little subcutaneous tissue, so the area around the anterior iliac crest is a suitable site for these clients. The nurse should use a 27-G, 5/8-inch (1.6-cm) needle. Cephalosporin and penicillin potentiate the effects of heparin. Some agency medication safety policies require two nurses check the dose because a dose error could cause bleeding. The onset of heparin is not immediate when given subcutaneously.
Question 36.
What should the nurse instruct the client with a platelet count of 31,000/µL (31 x 109/L) to do?
(a) Pad sharp surfaces to avoid minor trauma when walking.
(b) Assess for spontaneous petechiae in the extremities.
(c) Wear a mask when in crowds of people.
(d) Check for blood in the urine.
Answer:
(a) Pad sharp surfaces to avoid minor trauma when walking.
Explanation:
A client with a platelet count of 30,000 to 50,000/µL (30 to 50 x 109/L) is susceptible to bruising with minor trauma. Padding areas that the client might bump, scratch, or hit may help prevent minor trauma. A platelet count of 15,000 to 30,000/µL (15 to 30 x 109/L) may result in spontaneous petechiae and bruising, especially on the extremities. Padding measures would still be used, but the focus would be on assessing for new spontaneous petechiae.
Although the client should use precautions to prevent infection, the white blood count is not affected, and the client does not need to wear a mask when in areas where there are large numbers of people who are sources of potential infection. With a count below 20,000/µL (20 x 109/L), the client is at risk for spontaneous bleeding from the mucous membranes and intracranial bleeding.
Question 37.
A client with a history of systemic lupus ery-thematosus was admitted with a severe viral respiratory tract infection and diffuse petechiae. Based on these data, what recent information about the client should the nurse assess further?
(a) quality and quantity of food intake
(b) type and amount of fluid intake
(c) extent of weakness and fatigue
(d) length and amount of menstrual flow
Answer:
(d) length and amount of menstrual flow
Explanation:
A recent viral infection in a female client between the ages of 20 and 30 with a history of systemic lupus erythematosus and an insidious onset of diffuse petechiae are hallmarks of idiopathic thrombocytopenic purpura. It is important to ask whether the client’s recent menses have been lengthened or are heavier. Determining her ability to clot can help determine her risk of increased bleeding tendency until a platelet count is drawn. Petechiae are not caused by poor nutrition. Because of poor food and fluid intake or weakness and fatigue, the client may have gotten bruises from falling or bumping into things, but not petechiae.
Question 38.
When a client with thrombocytopenia has a severe headache, what does the nurse interpret that this may indicate?
(a) stress of the disease
(b) cerebral bleeding
(c) migraine headache
(d) sinus congestion
Answer:
(b) cerebral bleeding
Explanation:
When the platelet count is very low, red blood cells leak out of the blood vessels and into the tissue. If the blood pressure is elevated and the platelet count falls to <15,000/pL (15 x 109/L), internal bleeding in the brain can occur. A severe headache occurs from meningeal irritation when blood leaks out of the cerebral vasculature. When a client has thrombocytopenia, the nurse should always assess for cerebral bleeding by checking vital signs and performing neurologic checks. Headaches can be caused by stress, migraines, and sinus congestion. However, the concern here is the risk of internal bleeding into the brain.
Question 39.
The nurse is teaching the client with a platelet disorder about signs of bleeding. What statement from the client indicates the client has understood the teaching?
(a) “Petechiae are large, red skin bruises.”
(b) “Ecchymoses are large, purple skin bruises.”
(c) “Purpura is an open cut on the skin.”
(d) “Abrasions are small pinpoint red dots on the skin.”
Answer:
(b) “Ecchymoses are large, purple skin bruises.”
Explanation:
Large, purplish skin lesions caused by hemorrhage are called ecchymoses. Small, flat, red pinpoint lesions are petechiae. Numerous petechiae result in a reddish, bruised appearance called purpura. An abrasion is a wound caused by scraping.
Question 40.
The nurse should instruct the client with a platelet count of <150,000/µL (150 x 109/L) to avoid which activity?
(a) walking for more than 10 minutes
(b) straining to have a bowel movement
(c) visiting with young children
(d) sitting in semi-Fowler’s position
Answer:
(b) straining to have a bowel movement
Explanation:
When the platelet count is <150,000/µL (150 x 109/L), prolonged bleeding can occur from trauma, injury, or straining such as with Valsalva’s maneuver. Clients should avoid any activity that causes straining to evacuate the bowel. Clients can ambulate, but pointed or sharp surfaces should be padded. Clients can visit with their families but should avoid any scratches, bumps, or scrapes. Clients can sit in a semi-Fowler’s position but should change positions to promote circulation and check for petechiae.
Question 41.
A client who is taking aspirin caplets develops prolonged bleeding from a superficial skin injury on the forearm. The nurse should tell the client to do which action first?
(a) Place the forearm under a running stream of lukewarm water.
(b) Pat the injury with a dry washcloth.
(c) Wrap the entire forearm from the wrist to the elbow.
(d) Apply an ice pack for 20 minutes.
Answer:
(d) Apply an ice pack for 20 minutes.
Explanation:
Aspirin has an antiplatelet effect, and bleeding time can consequently be prolonged. Intermittent use of ice packs to the site may stop the bleeding; ice causes blood vessels to vasocon- strict. Use of lukewarm water, patting the injury, and wrapping the entire forearm do not promote vasoconstriction to stop bleeding.
Question 42.
A client with thrombocytopenia has developed a hemorrhage. The nurse should assess the client for which finding?
(a) tachycardia
(b) bradycardia
(c) decreased PaC02
(d) narrowed pulse pressure
Answer:
(a) tachycardia
Explanation:
The nurse should assess the client who is bleeding for tachycardia because the heart beats faster to compensate for decreased circulating volume and decreased numbers of oxygen-carrying red blood cells. The degree of cardiopulmonary distress and anemia will be related to the amount of hemorrhage that occurred and the period of time over which it occurred.
Bradycardia is a late symptom of hemorrhage; it occurs after the client is no longer able to compromise and is debilitating further into shock. If bradycardia is left untreated, the client will die from cardiovascular collapse. Decreased PaCCb is a late symptom of hemorrhage, after transport of oxygen to the tissue has been affected. A narrowed pulse pressure is not an early sign of hemorrhage.
Question 43.
The client with idiopathic thrombocytopenic purpura (ITP) asks the nurse why it is necessary to take steroids. The nurse should base the response on which information?
(a) Steroids destroy the antibodies and prolong the life of platelets.
(b) Steroids neutralize the antigens and prolong the life of platelets.
(c) Steroids increase phagocytosis and increase the life of platelets.
(d) Steroids alter the spleen’s recognition of platelets and increase the life of platelets.
Answer:
(d) Steroids alter the spleen’s recognition of platelets and increase the life of platelets.
Explanation:
ITP is treated with steroids to suppress the splenic macrophages from phagocytizing the antibody-coated platelets, which are recognized as foreign bodies, so that the platelets live longer. The steroids also suppress the binding of the autoimmune antibody to the platelet surface. Steroids do not destroy the antibodies on the platelets, neutralize antigens, or increase phagocytosis.

Question 44.
A client is to be discharged on prednisone. Which statement indicates that the client understands how to take the medication?
(a) “I need to take the medicine in divided doses at morning and bedtime.”
(b) “I am to take 40 mg of prednisone for 2 months and then stop.”
(c) “I need to wear or carry identification that I am taking prednisone.”
(d) “I will take the medication on an empty stomach.”
Answer:
(c) “I need to wear or carry identification that I am taking prednisone.”
Explanation:
The client needs to wear or carry information containing the name of the drug, dosage, health care provider (HCP) and contact information, and emergency instructions because additional corticosteroid drug therapy would be needed during emergency situations. Prednisone should be taken in the morning because it can cause insomnia and because exogenous corticosteroid suppression of the adrenal cortex is less when it is administered in the morning. Prednisone must never be stopped suddenly. It must be tapered off to allow for the adrenal cortex to recover from drug-induced atrophy so that it can resume its function. Prednisone should be taken with food or milk to prevent stomach irritation.
Question 45.
When teaching the client older than age 50 who is receiving long-term prednisone therapy, the nurse should make which suggestion to the client?
(a) Take the prednisone with food.
(b) Take over-the-counter antiemetics.
(c) Exercise three to four times a week.
(d) Eat foods that are low in potassium.
Answer:
(a) Take the prednisone with food.
Explanation:
Nausea, vomiting, and peptic ulcers are gastrointestinal adverse effects of prednisone, so it is recommended that clients take the prednisone with food. In some instances, the client may be advised to take a prescribed antacid prophylactically. The client should never take over-the-counter drugs without notifying the health care provider (HCP) who prescribed the prednisone. The client should ask the HCP about the amount and kind of exercise because of the need to establish baseline physical values before starting an exercise program and because of the increased potential for comorbidity with increasing age. The client should eat foods that are high in potassium to prevent hypokalemia.
Question 46.
The nurse is preparing a teaching plan about increased exercise for a female client who is receiving long-term corticosteroid therapy. What type of exercise is most appropriate for this client?
(a) floor exercises
(b) stretching
(c) running
(d) walking
Answer:
(d) walking
Explanation:
The best exercise for females who are on long-term corticosteroid therapy is a low-impact, weight-bearing exercise such as walking or weight lifting. Floor exercises do not provide for the weight bearing. Stretching is appropriate but does not offer sufficient weight bearing. Running provides for weight bearing but is hard on the joints and may cause bleeding.
Question 47.
The nurse is teaching a female client with a history of acquired thrombocytopenia about how to prevent and control hemorrhage. Which statement indicates that the client needs further instruction?
(a) “I can apply direct pressure over small cuts for at least 5 to 10 minutes to stop a venous bleed.”
(b) “I can count the number of tissues saturated to detect blood loss during a nosebleed.”
(c) “I can take hormones to decrease blood loss during menses.”
(d) “I can count the number of sanitary napkins to detect excess blood loss during menses.”
Answer:
(b) “I can count the number of tissues saturated to detect blood loss during a nosebleed.”
Explanation:
The client needs further teaching if she thinks that the number of tissues saturated represents all of the blood lost during a nosebleed. During a nosebleed, a significant amount of blood can be swallowed and go undetected. It is important that clients with severe thrombocytopenia do not take a nosebleed lightly. Clients with thrombocytopenia can apply pressure for 5 to 10 minutes over a small, superficial cut. Clients with thrombocytopenia can take hormones to suppress menses and control menstrual blood loss. Clients can also count the number of saturated sanitary napkins to approximate blood loss during menses. Some authorities estimate that a completely soaked sanitary napkin holds 50 mL.
Question 48.
A client has been on long-term prednisone therapy. What should the nurse instruct the client to include in the diet? Select all that apply.
(a) carbohydrates
(b) protein
(c) saturated fat
(d) potassium
(e) calcium
(f) vitamin D
Answer:
(b) protein
(d) potassium
(e) calcium
(f) vitamin D
Explanation:
(b), (d), (e), (f). Adverse effects of prednisone are weight gain, retention of sodium and fluids with hypertension and Cushingoid features, a low serum albumin level, suppressed inflammatory processes with masked symptoms, and osteoporosis. A diet high in protein, potassium, calcium, and vitamin D is recommended. Carbohydrates would elevate glucose and further compromise a client’s immune status. Saturated does not counteract the adverse effects of steroids such as prednisone.
Question 49.
The nurse is preparing to administer platelets to a client. When should the nurse contact the pharmacist about the bag of platelets?
(a) The platelet bag is cold.
(b) The platelet bag is 2 days old.
(c) The platelet bag is at room temperature.
(d) The platelet bag is 12 hours old.
Answer:
(a) The platelet bag is cold.
Explanation:
Platelets cannot survive cold temperatures. The platelets should be stored at room temperature and last for no more than 5 days.
Question 50.
The nurse is preparing to administer platelets. What should the nurse do first?
(a) Check the ABO compatibility.
(b) Administer the platelets slowly.
(c) Gently rotate the bag.
(d) Use a whole-blood tubing set.
Answer:
(c) Gently rotate the bag.
Explanation:
The bag containing platelets needs to be gently rotated to prevent clumping. ABO compatibility is not a necessary requirement, but human leukocyte antigen (HLA) matching of lymphocytes may be completed to avoid development of anti- HLA antibodies when multiple platelet transfusions are necessary. Platelets should be administered as fast as can be tolerated by the client to avoid aggregation. Most institutions use tubing especially for platelets instead of tubing for blood and blood products.
Question 51.
Which action by the client indicates that the client has achieved the goal of correctly demonstrating deep breathing for
an upcoming splenectomy?
(a) The client breathes in through the nose and out through the mouth.
(b) The client breathes in through the mouth and out through the nose.
(c) The client uses diaphragmatic breathing in the lying, sitting, and standing positions.
(d) The client takes a deep breath in through the nose, holds it for 5 seconds, and blows out through pursed lips.
Answer:
(d) The client takes a deep breath in through the nose, holds it for 5 seconds, and blows out through pursed lips.
Explanation:
The correct technique for deep breathing postoperatively to avoid atelectasis and pneumonia is to take in a deep breath through the nose, hold it for 5 seconds, and then blow it out through pursed lips. The goal is to fully expand and empty the lungs for pulmonary hygiene.
Question 52.
A client is scheduled for an elective splenectomy. What is the last thing the nurse should determine before the client goes to surgery?
The client has:
(a) voided completely.
(b) signed the consent.
(c) vital signs recorded.
(d) name band on wrist.
Answer:
(c) vital signs recorded.
Explanation:
An elective surgical procedure is scheduled in advance so that all preparations can be completed ahead of time. The vital signs are the final check that must be completed before the client leaves the room so that continuity of care and assessment is provided for. The first assessment that will be completed in the preoperative holding area or operating room will be the client’s vital signs.
The client should have emptied the bladder before receiving preoperative medications so that the bladder is empty when it is time for transport into the operating room. The client should have signed the consent yjj before the transport time so that if there were any questions or concerns, there was time to meet with the surgeon. Also, the consent form must be signed before any sedative medications are given. The client’s name band should be placed as soon as the client arrives in the perioperative setting, and it remains in place through discharge.
Question 53.
When receiving a client from the postanesthesia care unit after a splenectomy, the nurse should assess which information next after obtaining vital signs?
(a) nasogastric drainage
(b) urinary catheter
(c) dressing
(d) need for pain medication
Answer:
(c) dressing
Explanation:
After a splenectomy, the client is at high risk for hypovolemia and hemorrhage. The dressing should be checked often; if drainage is present, a circle should be drawn around the drainage and the time noted to help determine how fast bleeding is occurring. The nasogastric tube should be connected, hut this can wait until the dressing has been checked. A urinary catheter is not needed. The last pain medication administration and the client’s current pain level should be communicated in the exchange report. Checking for hemorrhage is a greater priority than assessing pain level.
Question 54.
A client who had a splenectomy yesterday has a nasogastric (NG) tube. What should the nurse assess to determine the effectiveness of the NG tube?
(a) depth of diaphragmatic breathing
(b) amount of blood draining from the tube
(c) absence of abdominal distention
(d) normal pH of gastric contents
Answer:
(c) absence of abdominal distention
Explanation:
A splenectomy may involve manipulation of the upper abdominal organs, such as diaphragm, stomach, liver, spleen, and small intestines. Manipulation of these organs and resulting inflammation lead to a slowed peristalsis. An NG tube is placed to decrease abdominal distention in the immediate postoperative phase. The NG tube does not affect the depth of diaphragmatic breathing.
The NG tube drains gastric contents and air in the stomach; it is not in the operative site and therefore cannot be used to irrigate it and there should not be bloody drainage. The gastric juices are not checked as an indicator that peristalsis has returned, and the pH should be normal; instead, bowel sounds are auscultated in all four quadrants to indicate the return of peristalsis.
Question 55.
A client who had a splenectomy is being discharged. What should the nurse teach the client to do?
(a) Refrain from driving a car for 6 weeks.
(b) Alternate rest and activity.
(c) Make an appointment for the staples to be removed.
(d) Report early signs of infection.
Answer:
(d) Report early signs of infection.
Explanation:
Clients who have had a splenectomy are especially prone to infection. The reduction of immunoglobulin M leaves the client especially at risk for immunologic deficiency infections. All clients who have had major abdominal surgery usually receive discharge instructions not to drive because the stomach muscles are not strong enough to brake hard or quickly after the abdominal muscles have been separated.
All clients need to pace activity and rest when going home after major surgery. Rest and sleep allow the growth hormone to repair the tissue, and activity allows the energy and strength to build endurance and muscle strength. An appointment is usually made to see the surgeon in the office 1 week after discharge for follow-up and to remove sutures or staples if this has not already been done.
Question 56.
The nurse should assess a client at risk for acute disseminated intravascular coagulation (DIC) for which early sign?
(a) severe shortness of breath
(b) bleeding without history or cause
(c) orthopnea
(d) hematuria
Answer:
(b) bleeding without history or cause
Explanation:
There is no well-defined sequence for acute DIC other than that the client starts bleeding without a history or cause and does not stop bleeding. Later signs may include severe shortness of breath, hypotension, pallor, petechiae, hematoma, orthopnea, hematuria, vision changes, and joint pain.
Question 57.
Which is contraindicated for a client diagnosed with disseminated intravascular coagulation (DIC]?
(a) treating the underlying cause
(b) administering heparin
(c) administering warfarin sodium
(d) replacing depleted blood products
Answer:
(c) administering warfarin sodium
Explanation:
DIC has not been found to respond to oral anticoagulants such as warfarin sodium. Treatments for DIC are controversial but include treating the underlying cause, administering heparin, and replacing depleted blood products.
Question 58.
A client with disseminated intravascular coagulation develops clinical manifestations of microvascular thrombosis. What signs should the nurse report to the health care provider (HCP)?
(a) hemoptysis
(b) focal ischemia
(c) petechiae
(d) hematuria
Answer:
(b) focal ischemia
Explanation:
Clinical manifestations of microvascu- lar thrombosis are those that represent a blockage of blood flow and oxygenation to the tissue that results in eventual death of the organ. Examples of microvascular thrombosis include acute respiratory distress syndrome, focal ischemia, superficial gangrene, oliguria, azotemia, cortical necrosis, acute ulceration, delirium, and coma. Hemoptysis, pete- chiae, and hematuria are signs of hemorrhage.
Question 59.
A client is diagnosed with infectious mono-nucleosis. The white blood cell count is 19,000/pL (19 x 109/L). The client has a streptococcal throat infection, enlarged spleen, and aching muscles. Which instructions should the nurse include in discharge planning with the client? Select all that apply.
(a) Stay on bed rest until the temperature is normal.
(b) Gargle with warm saline while the throat is irritated.
(c) Increase intake of fluids until the infection subsides.
(d) Wear a mask if others are present.
(e) Avoid contact sports while the spleen isenlarged.
Answer:
(a) Stay on bed rest until the temperature is normal.
(b) Gargle with warm saline while the throat is irritated.
(c) Increase intake of fluids until the infection subsides.
(e) Avoid contact sports while the spleen isenlarged.
Explanation:
(a), (b), (c), (e). The nurse should teach this client to stay on bed rest as long as there is a fever, gargle with warm saline, and increase oral fluids to prevent dehydration from the elevated temperature. The client with an enlarged spleen should avoid contact sports due to the increased risk of injury due to the enlargement. The client does not need to wear a mask but should observe handwashing procedures.
Question 60.
The daily white blood cell (WBC) count in a client with aplastic anemia drops overnight from 3,900 to 2,900/µL (3.9 to 2.9 x 109/L). Which is the appropriate nursing intervention?
(a) Continue monitoring the client.
(b) Call the laboratory to verify the report.
(c) Document the finding.
(d) Call the health care provider (HCP), and request that the client be placed in reverse isolation.
Answer:
(d) Call the health care provider (HCP), and request that the client be placed in reverse isolation.
Explanation:
The client will need a prescription from the HCP [Ij to be placed in reverse (protective) isolation because the normal defenses are ineffective and place the client at risk for infection (leukopenia, <5,000 cells/µL [5 x 109/L]). The faster the decrease in WBCs, the greater the bone marrow suppression and the more susceptible the client is to infection from not only pathogenic but also nonpathogenic organisms. The client will continue to be monitored, the laboratory may be called, and the report will be placed on the chart, but protection of the client must be instituted immediately.
Question 61.
A client who had an exploratory laparotomy 3 days ago now has a white blood cell (WBC) count of 15,000 µL (15 x 109/L). For which clinical findings of this laboratory report should the nurse assess the client? Select all that apply.
(a) swelling around the incision
(b) redness around the incision
(c) elevated temperature
(d) nonproductive cough
(e) weak pedal pulses
Answer:
(a) swelling around the incision
(b) redness around the incision
(c) elevated temperature
Explanation:
(a), (b), (c). The client has an elevated white count. Normal white count is 4,300 to 10,800 µL (4.3 to 10.8 x 109/L), The client is at risk for infection, and the nurse should assess the client for inflammation around the incision site, redness at the incision site, and elevated temperature. The client should be encouraged to cough and deep breathe, and it is unlikely that a cough is related to an incisional infection. Weak pedal pulses are not indications of an infection, but the nurse should report this finding if it persists.
Question 62.
The nurse is developing a care plan with a client who has leukemia. What instructions should the nurse include in the plan? Select all that apply.
(a) Monitor temperature and report elevation.
(b) Recognize signs and symptoms of infection.
(c) Avoid crowds.
(d) Maintain integrity of skin and mucous membranes.
(e) Take a baby aspirin each day.
Answer:
(a) Monitor temperature and report elevation.
(b) Recognize signs and symptoms of infection.
(c) Avoid crowds.
(d) Maintain integrity of skin and mucous membranes.
Explanation:
(a), (b), (c), (d). Nursing care of a client with leukemia includes managing and preventing infection, maintaining integrity of skin and mucous membranes, instituting measures to prevent bleeding, and monitoring for bleeding. Aspirin is an anticoagulant; bleeding tendencies, such as petechiae, ecchvmosis, epistaxis, gingival bleeding, and retinal hemorrhages, are likely due to thrombocvtopenia.
Question 63.
A client with neutropenia has an absolute neutrophil count (ANC) of 900 (0.9 x 109/L). The nurse teaches the client to prevent which risk of neutropenia?
(a) bleeding
(b) infection
(c) hemorrhagic stroke
(d) sickle cell crisis
Answer:
(b) infection
Explanation:
A client is at moderate risk for infection when the ANC is <1,000 (1 x 109/L). The client does not have a platelet disorder and is not at risk for bleeding or hemorrhagic stroke. The client does not have sickle cell anemia and is not at risk for a crisis.
Question 64.
The nurse is taking care of a client with neu-tropenia. Which nursing action is most important in preventing cross-contamination?
(a) changing gloves immediately after use
(b) standing 2 feet (61 cm) from the client
(c) speaking minimally when in the room
(d) wearing protective coverings
Answer:
(a) changing gloves immediately after use
Explanation:
Bedside rails, call bells, drug administration controls operated by the client, and other surface areas are frequently touched by caregivers with used gloves. Changing gloves immediately after use protects the client from contamination by organisms. Cross-contamination is a break in technique of serious consequence to the severely compromised client. Standing 2 feet (61 cm) from the client, speaking minimally, and wearing protective covering shirts are not required in standard interventions for risk of infection.
Question 65.
What should the nurse teach the client with neutropenia to avoid?
(a) using suppositories or enemas
(b) using a high-efficiency particulate air (HEPA) filter mask
(c) performing perianal care after every bowel movement
(d) performing oral care after every meal
Answer:
(a) using suppositories or enemas
Explanation:
The neutropenic client is at risk for infection, especially bacterial infection of the respiratory and gastrointestinal tracts. Breaks in the mucous membranes, such as those that could be caused by the insertion of a suppository or enema tube, would be a break in the first line of the body’s defense and a direct port of entry for infection. The client with neutropenia is encouraged to wear an HEPA filter mask and to use an incentive spirometer for pulmonary hygiene.
The client needs to know the importance of completing meticulous total body hygiene daily, including perianal care after every bowel movement, to decrease the flora at normal body orifices. The client also needs to know the importance of performing oral care after every meal and every 4 hours while the client is awake to decrease the bacterial buildup in the oropharynx.
Question 66.
A client with granulocytopenia has many visitors. To prevent infection what is the most important thing the nurse should tell the visitors to do?
(a) Visit only if they do not have a cold.
(b) Wash their hands.
(c) Leave the children at home.
(d) Avoid kissing the client.
Answer:
(b) Wash their hands.
Explanation:
Washing hands before, during, and after care has a significant effect in reducing infections. It is advisable to avoid introducing a cold or children’s germs and to avoid kissing the client, but the primary prevention technique is handwashing.
Question 67.
A nurse is obtaining consent for a bone marrow aspiration. Which actions should the nurse take? Select all that apply.
(a) Witness the client signing the consent form.
(b) Evaluate that the client understands the procedure.
(c) Explain the risks of the procedure to the client.
(d) Verify that the client is signing the consent form of his or her own free will.
(e) Determine that the client understands postprocedure care.
Answer:
(a) Witness the client signing the consent form.
(b) Evaluate that the client understands the procedure.
(d) Verify that the client is signing the consent form of his or her own free will.
(e) Determine that the client understands postprocedure care.
Explanation:
(a), (b), (d), (e). The nurse can serve as a witness for consent for procedures. The nurse also ascertains whether the client has an understanding that is consistent with the procedure listed on the form, determines that the client is signing the consent of his or her own free will, and determines that the client understands postprocedure care. The nurse’s role does not include explaining the risks of the procedure; that responsibility belongs to the person who is to perform the procedure, such as the health care provider (HCP).
Question 68.
A client is about to undergo bone marrow aspiration of the sternum. What should the nurse tell the client?
(a) “You may feel a solution being wiped over your entire front from your neck down to your navel and out to your shoulders.”
(b) “You will not feel the local anesthetic being applied because it will be sprayed on.”
(c) “You will feel a pulling type of discomfort for a few seconds.”
(d) “After the needle is removed, you will feel a bandage being applied around your chest.”
Answer:
(c) “You will feel a pulling type of discomfort for a few seconds.”
Explanation:
As the bone marrow is being aspirated, the client will feel a suction or pulling type of sensation or discomfort that lasts a few seconds. A systemic premedication may be given to decrease this discomfort. A small area over the sternum is cleaned with an antiseptic. It is unnecessary to paint the entire anterior chest. The local anesthetic is injected through the subcutaneous tissue to numb the tissue for the larger-bore needle that is used for aspiration and biopsy.
After the needle is removed, pressure is held over the aspiration site for 5 to 10 minutes to achieve hemostasis. A small dressing is applied; a large pressure dressing, such as an Ace bandage, would restrict the expansion of the lungs and is not used.
Question 69.
Twenty-four hours after a bone marrow aspiration, the nurse is evaluating the client’s postprocedure status. Which outcome is expected?
(a) The client maintains bed rest.
(b) There is redness and swelling at the aspira tion site.
(c) The client requests a strong analgesic for pain.
(d) There is no bleeding at the aspiration site.
Answer:
(d) There is no bleeding at the aspiration site.
Explanation:
After a bone marrow aspiration, the puncture site should be checked every 10 to 15 minutes for bleeding. For a short period after the procedure, bed rest may be prescribed. Signs of infection, such as redness and swelling, are not anticipated at the aspiration site. A mild analgesic may be prescribed for pain, but if the client has pain longer than 24 hours, the nurse should assess the client for internal bleeding or increased pressure at the puncture site, which may be the cause of the pain, and should consult the health care provider (HCP).
Question 70.
A client states, “I don’t want any more tests. Who cares what kind of leukemia I have? I just want to be treated now.” Which is the nurse’s best response?
(a) “I am sure you are frustrated and want to be well now.”
(b) “Your treatment can be more effective if it is based on more specific information about your disease.”
(c) “Now, you know the tests are necessary and that you are just upset right now.”
(d) “I understand how you feel.”
Answer:
(b) “Your treatment can be more effective if it is based on more specific information about your disease.”
Explanation:
The nurse is an advocate for the client with leukemia who can be empowered with knowledge of the treatment. Immunologic, cytogenic, morphologic, histochemical, and other means are used to identify cell subtypes and stages of leukemia cell development for very specific and optimal treatment.
The nurse should not label the client’s feeling, such as frustration or emotional; only the client can identify his or her own feelings. Chastising the client is not helpful. It disavows the client’s emotional state and responses to the diagnosis and involved treatment. Unless nurses have had leukemia, they cannot possibly know how the client feels even though they may be trying to offer empathy.
Question 71.
During the induction stage for treatment of leukemia, the nurse should remove which items that the family has brought into the room?
(a) a prayer book
(b) a picture
(c) a bouquet of flowers
(d) a hairbrush
Answer:
(c) a bouquet of flowers
Explanation:
The induction phase of chemotherapy is an aggressive treatment to kill leukemia cells. The client is severely immunocompromised and severely at risk for infection. Flowers, herbs, and plants should be avoided during this time. The client’s prayer book, pictures, and other personal belongings can be cleaned before being brought into the room to prevent client contact with pathogenic and nonpathogenic organisms.
Question 72.
The nurse understands that the client who is undergoing induction therapy for leukemia needs additional instruction when the client makes which statement?
(a) “I will pace my activities with rest periods.”
(b) “I cannot wait to get home to my cat!”
(c) “I will use warm saline gargle instead of brushing my teeth.”
(d) “I must report a temperature of 100°F (37.7°C).”
Answer:
(b) “I cannot wait to get home to my cat!”
Explanation:
The nurse identifies that the client does not understand that contact with animals must be avoided because they carry infection and the induction therapy will destroy the client’s white blood cells (WBCs). The induction therapy will cause anemia, and the client will experience fatigue and will have to pace activities with rest periods.
Platelet production will be decreased, and the client will be at risk for bleeding tendencies; oral hygiene will have to be provided by using a warm saline gargle instead of brushing the teeth and gums. The client will be at risk for infection owing to the decrease in WBC production and should report a temperature of 100°F (37.8°C) or higher.
Question 73.
A client with chronic myelogenous leukemia is taking Imatinib. The nurse should instruct the client to report which adverse effect of this drug?
(a) edema
(b) numbness and tingling in extremities
(c) bloody stools
(d) persistent cough
Answer:
(a) edema
Explanation:
Imatinib works by inhibiting the proliferation of abnormal cells. Adverse effects include edema and GI irritation. Typical effects of this drug do not include numbness and tingling, bloody stools, or persistent cough. If the client has these symptoms, they may relate to disease occurrence or recurrence.
Question 74.
A client with acute lymphocytic leukemia is receiving vincristine. Prior to infusing the drug, the nurse administers diphenhydramine. What should the nurse tell the client about the purpose of taking diphenhydramine?
(a) Diphenhydramine promotes sleep, while the vincristine is infusing.
(b) Diphenhydramine decreases incidence of a reaction to the vincristine.
(c) Diphenhydramine potentiates the action of the vincristine.
(d) Diphenhydramine reduces anxiety associated with the vincristine infusion.
Answer:
(b) Diphenhydramine decreases incidence of a reaction to the vincristine.
Explanation:
Diphenhydramine is an antihistamine. This drug helps reduce the incidence of an allergic response by blocking the release of histamine. Diphenhydramine also possesses anticholinergic effects and can reduce the incidence of nausea and vomiting for clients receiving chemotherapy. Although diphenhydramine may promote sleep, it is not the primary reason for its administration in this instance. Diphenhydramine will not reduce anxiety or potentiate the action of the vincristine.
Question 75.
A nurse is administering an IV antineoplastic agent when the client says, “My arm is burning by the IV site.” What should the nurse do first?
(a) Slow the infusion rate and check the IV site.
(b) Double check that the dose is correct.
(c) Stop infusing the medication.
(d) Place a warm, moist pack on the IV site area.
Answer:
(c) Stop infusing the medication.
Explanation:
Antineoplastic agents can cause severe tissue damage if they extravasate; therefore, the nurse should immediately stop the infusion. The correct dose should be verified before starting the infusion. After stopping the infusion, the nurse should notify the health care provider. If extravasation has occurred, it may be appropriate to apply ice packs to the site.
Ice packs cause desired vaso-constriction; warm, moist packs cause vasodilation. Ice packs should not remain in place for more than 15 to 20 minutes because rebound vasodilation can occur; the ice packs are removed for a short time and then reapplied as needed.
Question 76.
A client who is receiving a blood transfusion suddenly experiences chills and a temperature of 101°F (38°C). The client also has a headache and appears flushed. In what order, from first to last, should the nurse perform the actions? All options must be used.
(a) Obtain a blood culture from the client.
(b) Send the blood bag and administration set to the blood bank.
(c) Stop the blood infusion.
(d) Infuse normal saline to keep the vein open.
Answer:
(c) Stop the blood infusion.
(d) Infuse normal saline to keep the vein open.
(a) Obtain a blood culture from the client.
(b) Send the blood bag and administration set to the blood bank.
Explanation:
(c), (d), (a), (b). The client is experiencing a septic reaction to the blood transfusion. The nurse first stops the infusion and notifies the health care provider (HCP) and blood bank; then, the nurse uses an infusion of normal saline to keep the vein open and follows by obtaining a sample of the client’s blood for a blood culture. Lastly, the nurse sends the blood bag and the administration set to the blood bank for culture.
Question 77.
A client undergoing antineoplastic therapy is prescribed subcutaneous epoetin. What indicates to the nurse that the drug has been effective?
(a) Biopsies no longer show malignancy.
(b) Hemoglobin levels rise.
(c) Nausea and vomiting stop.
(d) A scan shows tumor shrinkage.
Answer:
(b) Hemoglobin levels rise.
Explanation:
Epoetin stimulates erythropoiesis and the production of RBCs. This is important for clients taking antineoplastics because they often suffer bone marrow depression as a side effect of antineoplastic therapy. Epoetin does not affect tissue malignancy or tumor size. Nausea and vomiting are commonly associated with antineoplastics, but these are treated with antiemetics.
Question 78.
The nurse is planning care for a client with acute myeloid leukemia (AML). What is an appropriate goal for this client?
(a) Prevent cardiac arrhythmias.
(b) Prevent liver failure.
(c) Prevent renal failure.
(d) Prevent hemorrhage.
Answer:
(d) Prevent hemorrhage.
Explanation:
Bleeding and infection are the major complications and causes of death for clients with AML. Bleeding is related to the degree of thrombocytopenia, and infection is related to the degree of neutropenia. Cardiac arrhythmias rarely occur as a result of AML. Liver or renal failure may occur, but neither is a major cause of death in AML.
Question 79.
The client with acute lymphocytic leukemia (ALL) is at risk for infection. What action should the nurse take?
(a) Place the client in a private room.
(b) Have the client wear a mask.
(c) Have staff wear gowns and gloves.
(d) Restrict visitors.
Answer:
(a) Place the client in a private room.
Explanation:
Clients with ALL are at risk for infection due to granulocytopenia. The nurse should place the client in a private room. Strict handwashing procedures should be enforced and will be the most effective way to prevent infection. It is not necessary to have the client wear a mask. The client is not contagious, and the staff does not need to wear gloves. The client can have visitors; however, they should be screened for infection and use handwashing procedures.
Question 80.
The nurse is planning care with a client with acute leukemia who has mucositis. What should the nurse advise the client to use for mouth care?
(a) lemon-glycerin swabs
(b) a commercial mouthwash
(c) normal saline
(d) a commercial toothpaste and brush
Answer:
(c) normal saline
Explanation:
Simple rinses with saline or a baking soda and water solution are effective and moisten the oral mucosa. Commercial mouthwashes and lemon glycerin swabs contain glycerin and alcohol, which are drying to the mucosa and should be avoided. Brushing after each meal is recommended, but every 4 hours may be too traumatic. During acute leukemia, the neutrophil and platelet counts are often low, and a soft-bristle toothbrush, instead of the client’s usual brush, should be used to prevent bleeding gums.
Question 81.
An adult client with acute leukemia and the health care team establish goals of improved tidal volume and activity tolerance. Which activities would be most helpful to attaining these goals? Select all that apply.
(a) increasing fluids to 3,000 mL/24 hours
(b) walking to increase the number of steps each day
(c) sitting in a chair to read or watch television
(d) taking deep breaths while sitting or lying in bed
(e) using a stationary bicycle to increase elevation and time
Answer:
(b) walking to increase the number of steps each day
(d) taking deep breaths while sitting or lying in bed
(e) using a stationary bicycle to increase elevation and time
Explanation:
(b), (d), (e). The client with acute leukemia experiences fatigue and deconditioning. To improve tidal volume, the nurse can encourage the client to take deep breaths while sitting or lying with the goal of increasing the depth and duration of the breath each time. The client should also increase activity tolerance. The client can do this by walking or using a stationary bike with the goal of increasing the activity. These exercises also help the client increase tidal volume. While drinking fluids and sitting rather than lying down are helpful, it is not necessary to increase the fluid intake to 3,000 mL/day or to spend much time sitting.
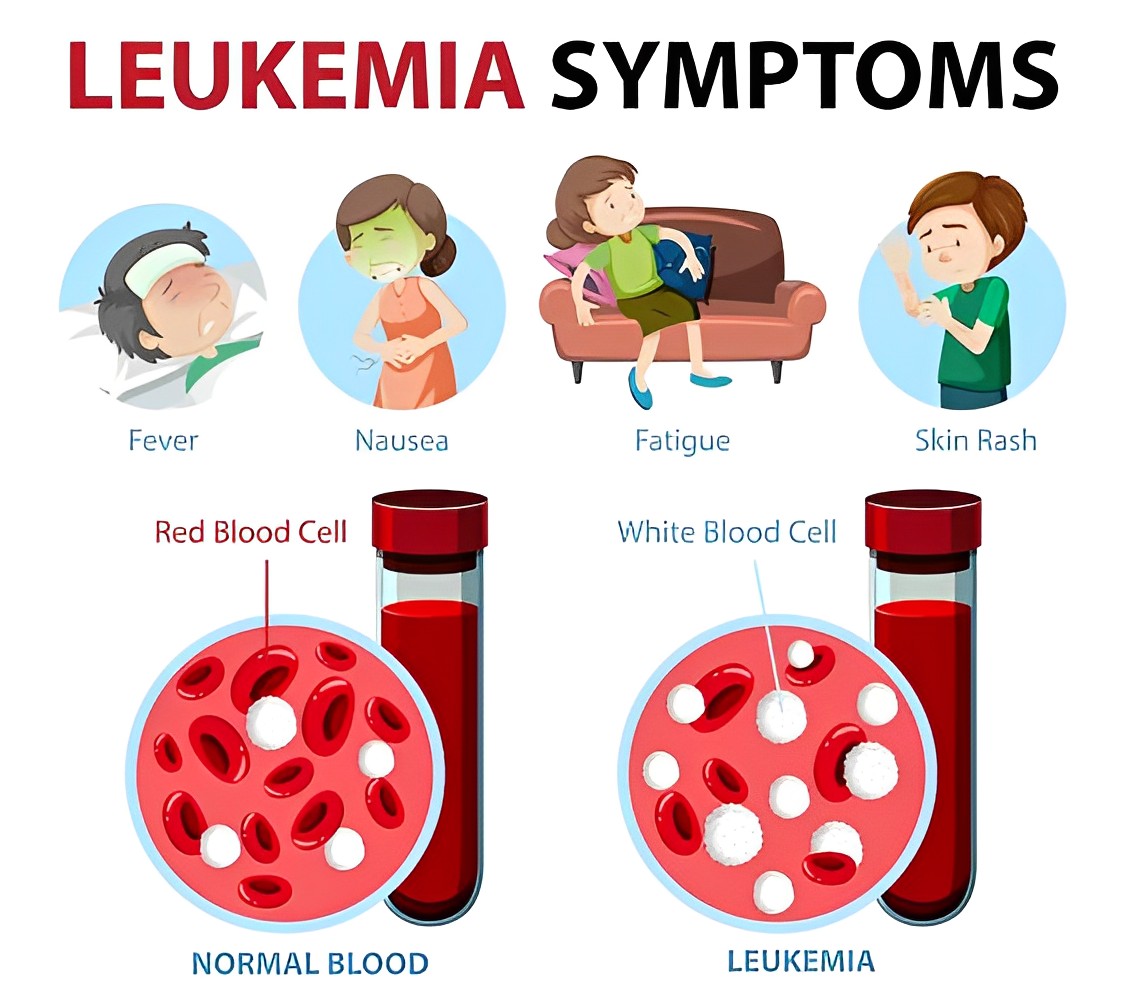
Question 82.
The nurse is evaluating the client’s understanding about combination chemotherapy. Which statement by the client about reasons for using combination chemotherapy indicates the need for further explanation?
(a) “Combination chemotherapy is used to inter rupt cell growth cycle at different points.”
(b) “Combination chemotherapy is used to destroy cancer cells and treat side effects simultaneously. ”
(c) “Combination chemotherapy is used to decrease resistance.”
(d) “Combination chemotherapy is used to minimize the toxicity from using high doses of a single agent.”
Answer:
(b) “Combination chemotherapy is used to destroy cancer cells and treat side effects simultaneously. ”
Explanation:
Combination chemotherapy does not mean two groups of drugs, one to kill the cancer cells and one to treat the adverse effects of the chemotherapy. Combination chemotherapy means that multiple drugs are given to interrupt the cell growth cycle at different points, decrease resistance to a chemotherapy agent, and minimize the toxicity associated with use of a high dose of a single agent (i.e., by using multiple agents with different toxicities).
Question 83.
In providing care to the client with leukemia who has developed thrombocytopenia, the nurse assesses the most common sites for bleeding. Which is not a common site?
(a) biliary system
(b) gastrointestinal tract
(c) brain and meninges
(d) pulmonary system
Answer:
(a) biliary system
Explanation:
The biliary system is not especially prone to hemorrhage. Thrombocytopenia (a low platelet count) leaves the client at risk for a potentially life- threatening spontaneous hemorrhage in the gastrointestinal, respiratory, and intracranial cavities.
Question 84.
The nurse is placing a client with severe neutropenia in reverse isolation. What should the nurse tell the client why this is necessary?
Reverse isolation helps prevent the spread of organisms:
(a) to the client from sources outside the client’s environment.
(b) from the client to health care personnel, visitors, and other clients.
(c) by using special techniques to dispose of contaminated materials.
(d) by using special techniques to handle the client’s linens and personal items.
Answer:
(a) to the client from sources outside the client’s environment.
Explanation:
The primary purpose of reverse isolation is to reduce transmission of organisms to the client from sources outside the client’s environment.
Question 85.
The nurse is developing a care plan for a client who has had radiation therapy for Hodgkin’s lymphoma. What is the primary goal of care for this client?
(a) Maintain fluid balance.
(b) Obtain sufficient exercise.
(c) Prevent infection.
(d) Avoid depression.
Answer:
(c) Prevent infection.
Explanation:
The client with Hodgkin’s lymphoma who has had radiation therapy is prone to infection; therefore, the primary goal is to prevent infection. The nurse instructs the client to perform frequent hand hygiene, avoid crowded areas, and report a temperature over 100°F (37.7°C). Maintaining fluid balance, exercising, and maintaining mental health are also important, but these are not primary goals at this time.
Question 86.
A client with a suspected diagnosis of Hodgkin’s disease is to have a lymph node biopsy. What should the nurse make sure that personnel involved with the procedure do?
(a) Maintain sterile technique.
(b) Use a mask, gloves, and a gown when assisting with the procedure.
(c) Send the specimen to the laboratory when someone is available to take it.
(d) Ensure that all instruments used are placed in a sealed and labeled container.
Answer:
(a) Maintain sterile technique.
Explanation:
The nurse must ensure that sterile technique is used when a biopsy is obtained because the client is at high risk for infection. In most cases, a lymph node biopsy is sent immediately to the laboratory once it is placed in a specific solution in a closed container. It is not necessary to wear a gown and mask when obtaining the specimen. It is not necessary to use special handling procedures for the instruments used.
Question 87.
The client with Hodgkin’s disease undergoes an excisional cervical lymph node biopsy under local anesthesia. After the procedure, what does the nurse assess first?
(a) vital signs
(b) the incision
(c) the airway
(d) neurologic signs
Answer:
(c) the airway
Explanation:
Assessing for an open airway is always first. The procedure involves the neck; the anesthesia may have affected the swallowing reflex, or the inflammation may have closed in on the airway, leading to ineffective air exchange. Once a patent airway is confirmed and an effective breathing pat-tern established, the circulation is checked. Vital signs and the incision are assessed as soon as possible, but only after it is established that the airway is patent and the client is breathing normally. A neurologic assessment is completed as soon as possible after other important assessments.
Question 88.
When assessing the client with Hodgkin’s disease, the nurse should observe the client for which finding?
(a) herpes zoster infections
(b) discolored teeth
(c) hemorrhage
(d) hypercellular immunity
Answer:
(a) herpes zoster infections
Explanation:
Herpes zoster infections are common in clients with Hodgkin’s disease. Discoloring of the teeth is not related to Hodgkin’s disease but rather to the ingestion of iron supplements or some antibiotics such as tetracycline. Mild anemia is common in Hodgkin’s disease, but the platelet count is not affected until the tumor has invaded the bone marrow. A cellular immunity defect occurs in Hodgkin’s disease in which there is little or no reaction to skin sensitivity tests. This is called anergy.
Question 89.
The client with Hodgkin’s disease develops B symptoms. Which symptom is a manifestation of B symptoms?
(a) a low-grade fever (temperature lower than 100°F [37.8°C])
(b) a weight loss of 5% or less of body weight
(c) night sweats
(d) not progressing to an advanced stage
Answer:
(c) night sweats
Explanation:
A temperature higher than 100.4°F (38°C), profuse night sweats, and an unintentional weight loss of 10% of body weight represent the cluster of clinical manifestations known as the B symptoms. Forty percent of clients with Hodgkin’s disease have B symptoms, and B symptoms are more common in advanced stages of the disease.
Question 90.
The nurse is developing a discharge plan with a client who is receiving chemotherapy to treat lymphoma. What should the nurse include in the plan?
(a) Wear a mask if leaving the house.
(b) Rest as needed.
(c) Avoid people with colds or flu.
(d) Decrease the protein in your diet.
(e) Contact the health care provider (HCP) if a fever develops.
Answer:
(b) Rest as needed.
(c) Avoid people with colds or flu.
(e) Contact the health care provider (HCP) if a fever develops.
Explanation:
(b), (c), (e). The nurse should teach the client to obtain as much rest as need, to avoid people who have a cold or the flu, and to report a fever to the HCP. It is not necessary for the client to wear a mask when going out of the house, but the client should avoid large crowds where there may be people with contagious diseases. It is not necessary to decrease the protein in the diet, but rather, the client should eat a well-balanced diet. The client may need to change some foods if the client has side effects of the chemotherapy and may need to obtain more calories.
Question 91.
The client asks the nurse to explain what it means that Hodgkin’s disease is diagnosed at stage 1A. What should the nurse explain about the involvement of the disease?
(a) involvement of a single lymph node
(b) involvement of two or more lymph nodes on the same side of the diaphragm
(c) involvement of lymph node regions on both sides of the diaphragm
(d) diffuse disease of one or more extralymphatic organs
Answer:
(a) involvement of a single lymph node
Explanation:
In the staging process, the designations A and B signify that symptoms were or were not present when Hodgkin’s disease was found, respectively. The Roman numerals I through IV indicate the extent and location of involvement of the disease. Stage I indicates involvement of a single lymph node; stage II, two or more lymph nodes on the same side of the diaphragm; stage III, lymph node regions on both sides of the diaphragm; and stage IV, diffuse disease of one or more extralymphatic organs.
Question 92.
A client is undergoing a bone marrow aspiration and biopsy. The client is very worried about the procedure. What should the nurse do to prepare the client for the procedure?
(a) Allow the client’s family to stay as long as possible.
(b) Listen as the client expresses concerns.
(c) Encourage the client to take slow, deep breaths to relax.
(d) Suggest the client request the health care provider prescribe a sedative.
Answer:
(d) Suggest the client request the health care provider prescribe a sedative.
Explanation:
Administering a sedative prior to a bone marrow aspiration and biopsy is a common preparation for the procedure, and the nurse can suggest that the client request a sedative if it has not been prescribed. Encouraging the client to take slow, deep breaths may be helpful, but a sedative may be more helpful during the uncomfortable parts of procedure to decrease the stress response of tightening and tensing the muscles.
Allowing the client’s family to stay may be appropriate if the family has a calming effect on the client prior to the procedure, but they will not be able to be present during the procedure. The nurse should listen while the client expresses concerns, but this may not be sufficient for calming the client during the procedure.
Question 93.
The nurse explains to the client with Hodgkin’s disease that a bone marrow biopsy will be taken after the aspiration. What should the nurse explain about the biopsy?
(a) “Your biopsy will be performed before the aspiration because enough tissue may be obtained so that you will not have to go through the aspiration.’’
(b) “You will feel a pressure sensation when the biopsy is taken but should not feel actual pain; if you do, tell the health care provider so that you can be given extra numbing medicine.”
(c) “You may hear a crunch as the needle passes through the bone, but when the biopsy is taken, you will feel a suction-type pain that will last for just a moment.”
(d) “You will be shaved and cleaned with an antiseptic agent, after which the health care provider will inject a needle without making an incision to aspirate out the bone marrow. ”
Answer:
(b) “You will feel a pressure sensation when the biopsy is taken but should not feel actual pain; if you do, tell the health care provider so that you can be given extra numbing medicine.”
Explanation:
A biopsy needle is inserted through a separate incision in the anesthetized area. The client will feel a pressure sensation when the biopsy is taken but should not feel actual pain. The client should be instructed to inform the health care provider (HCP). if pain is felt so that more anesthetic agent can be administered to keep the client comfortable.
The biopsy is performed after the aspiration and from a slightly different site so that the tissue is not disturbed by either test. The client will feel a suction-type pain for a moment when the aspiration is being performed, not the biopsy. A small incision is made for the biopsy to accommodate the larger- bore needle. This may require a stitch.
Question 94.
A client with advanced Hodgkin’s disease is admitted to hospice because death is imminent. What is the most important nursing goal at this time?
(a) Reduce the client’s fear of pain.
(b) Support the client’s wish to discontinue further therapy.
(c) Prevent feelings of isolation.
(d) Help the client overcome feelings of social inadequacy.
Answer:
(c) Prevent feelings of isolation.
Explanation:
Terminally ill clients most often describe feelings of isolation because they tend to be ignored, they are often left out of conversations (especially those dealing with the future), and they sense the attitudes of discomfort that many people feel in their presence. Helpful nursing measures include taking the time to be with the client, offering oppor-tunities to talk about feelings, and answering questions honestly.
Question 95.
The client is a survivor of non-Hodgkin’s lymphoma. Which statement indicates the client needs additional information?
(a) “Regular screening is very important for me.”
(b) “The survivor rate is directly proportional to the incidence of second malignancy.”
(c) “The survivor rate is indirectly proportional to the incidence of second malignancy.”
(d) “It is important for survivors to know the stage of the disease and their current treatment plan.”
Answer:
(b) “The survivor rate is directly proportional to the incidence of second malignancy.”
Explanation:
It is incorrect that the survivor rate is directly proportional to the incidence of second malignancy. The survivor rate is indirectly proportional to the incidence of second malignancy, and regular screening is very important to detect a second malignancy, especially acute myeloid leukemia or myelodysplastic syndrome. Survivors should know the stage of the disease and their current treatment plan so that they can remain active participants in their health care.
Question 96.
What is the most important goal of nursing care for a client who is in shock?
(a) Manage fluid overload.
(b) Manage increased cardiac output.
(c) Manage inadequate tissue perfusion.
(d) Manage vasoconstriction of vascular beds.
Answer:
(c) Manage inadequate tissue perfusion.
Explanation:
Nursing interventions and collaborative management are focused on correcting and maintaining adequate tissue perfusion. Inadequate tissue perfusion may be caused by hemorrhage, as in hypovolemic shock; by decreased cardiac output, as in cardiogenic shock; or by massive vasodilation of the vascular bed, as in neurogenic, anaphylactic, and septic shock. Fluid deficit, not fluid overload, occurs in shock.
Question 97.
Which finding indicates hypovolemic shock in an adult who has had a 15% blood loss?
(a) pulse rate <60 bpm
(b) respiratory rate of 4 breaths/min
(c) pupils unequally dilated
(d) systolic blood pressure <90 mm Hg
Answer:
(d) systolic blood pressure <90 mm Hg
Explanation:
Typical signs and symptoms of hypovolemic shock include systolic blood pressure <90 mm Hg, narrowing pulse pressure, tachycardia, tachypnea, cool and clammy skin, decreased urine output, and mental status changes, such as irritability or anxiety. Unequal dilation of the pupils is related to central nervous system injury or possibly to a previous history of eye injury.
Question 98.
Which finding is the best indication that fluid replacement for the client in hypovolemic shock is adequate?
(a) urine output >30 mL/h
(b) systolic blood pressure >110 mm Hg
(c) diastolic blood pressure >90 mm Hg
(d) respiratory rate of 20 breaths/min
Answer:
(a) urine output >30 mL/h
Explanation:
Urine output provides the most sensitive indication of the client’s response to therapy for hypovolemic shock. Urine output should be consistently >35 mL/h. Blood pressure is a more accurate reflection of the adequacy of vasoconstric-tion than of tissue perfusion. Respiratory rate is not a sensitive indicator of fluid balance in the client recovering from hypovolemic shock.
Question 99.
Which finding is a risk factor for hypovolemic shock?
(a) hemorrhage
(b) antigen-antibody reaction
(c) gram-negative bacteria
(d) vasodilation
Answer:
(a) hemorrhage
Explanation:
Causes of hypovolemic shock include external fluid loss, such as hemorrhage; internal fluid shifting, such as ascites and severe edema; and dehydration. Massive vasodilation is the initial phase of vasogenic or distributive shock, which can be further subdivided into three types of shock: septic, neurogenic, and anaphylactic. A severe antigen- antibody reaction occurs in anaphylactic shock. Gram-negative bacterial infection is the most common cause of septic shock. Loss of sympathetic tone (vasodilation) occurs in neurogenic shock.
Question 100.
Which is a priority assessment for the client in shock who is receiving an IV infusion of packed red blood cells and normal saline solution?
(a) fluid balance
(b) anaphylactic reaction
(c) pain
(d) altered level of consciousness
Answer:
(b) anaphylactic reaction
Explanation:
The client who is receiving a blood product requires astute assessment for signs and symptoms of allergic reaction and anaphylaxis, including pruritus (itching), urticaria (hives), facial or glottal edema, and shortness of breath. If such a reaction occurs, the nurse should stop the transfusion immediately, but leave the IV line intact, and notify the health care provider (HCP) p^. Usually, an antihistamine (such as diphenhydramine hydrochloride) is administered.
Epinephrine and corticosteroids may be administered in severe reactions. Fluid balance is not an immediate concern during the blood administration. The administration should not cause pain unless it is extravasating out of the vein, in which case the IV administration should be stopped. Administration of a unit of blood should not affect the level of consciousness.
Question 101.
The client who does not respond adequately to fluid replacement has a prescription for an IV infusion of dopamine hydrochloride at 5 meg/ kg/min. To determine that the drug is having the desired effect, what should the nurse assess?
(a) increased renal and mesenteric blood flow
(b) increased cardiac output
(c) vasoconstriction
(d) reduced preload and afterload
Answer:
(b) increased cardiac output
Explanation:
At medium doses (4 to 8 mcg/kg/min), dopamine hydrochloride slightly increases the heart rate and improves contractility to increase cardiac output and improve tissue perfusion. When given at low doses (0.5 to 3.0 mcg/kg/min), dopamine increases renal and mesenteric blood flow. At high doses (8 to 10 mcg/kg/min), dopamine produces vasoconstriction, which is an undesirable effect. Dopamine is not given to affect preload and afterload.
Question 102.
A client is receiving dopamine hydrochloride for treatment of shock. What action should the nurse take?
(a) Administer pain medication concurrently.
(b) Monitor blood pressure continuously.
(c) Evaluate arterial blood gases at least every 2 hours.
(d) Monitor for signs of infection.
Answer:
(b) Monitor blood pressure continuously.
Explanation:
The client who is receiving dopamine hydrochloride requires continuous blood pressure monitoring with an invasive or noninvasive device. The nurse may titrate the IV infusion to maintain a systolic blood pressure of 90 mm Hg. Administration of a pain medication concurrently with dopamine hydrochloride, which is a potent sympathomimetic with dose-related alpha-adrenergic agonist, beta 1-selective adrenergic agonist, and dopaminergic blocking effects, is not an essential nursing action for a client who is in shock with already low hemodynamic values.
Arterial blood gas concentrations should be monitored according to the client’s respiratory status and acid-base balance status and are not directly related to the dopamine hydrochloride dosage. Monitoring for signs of infection is not related to the nursing action for the client receiving dopamine hydrochloride.
Question 103.
A client who has been taking warfarin has been admitted with severe acute rectal bleeding and the following laboratory results: international normalized ratio (INR), 8; hemoglobin, 11 g/dL (110 g/L); and hematocrit, 33% (0.33). In which order, from first to last, should the nurse implement the health care provider’s prescriptions? All options must be used.
(a) Give 1 unit fresh frozen plasma (FFP).
(b) Administer vitamin K 2.5 mg by mouth.
(c) Schedule the client for sigmoidoscopy.
(d) Administer IV dextrose 5% in 0.45% normal saline.
Answer:
(d) Administer IV dextrose 5% in 0.45% normal saline.
(a) Give 1 unit fresh frozen plasma (FFP).
(b) Administer vitamin K 2.5 mg by mouth.
(c) Schedule the client for sigmoidoscopy.
Explanation:
(d), (a), (b), (c). Analysis of the client’s laboratory results indicates that an INR of 8 is increased beyond therapeutic ranges. The client is also experiencing severe acute rectal bleeding and has a hemoglobin level in the low range of normal and a hematocrit reflecting fluid volume loss. The nurse should first establish an IV line and administer the dextrose in saline. Next, the nurse should administer the FFP.
FFP contains concentrated clotting factors and provides an immediate reversal of the prolonged INR. Vitamin K 2.5 mg PO should be given next because it reverses the warfarin by returning the PT to normal values. However, the reversal process occurs over 1 to 2 hours. Lastly, the nurse can schedule the client for the sigmoidoscopy.
Question 104.
When assessing a client for early septic shock, the nurse should assess the client for which finding?
(a) cool, clammy skin
(b) warm, flushed skin
(c) increased blood pressure
(d) hemorrhage
Answer:
(b) warm, flushed skin
Explanation:
Warm, flushed skin from a high cardiac output with vasodilation occurs in warm shock or the hyperdynamic phase (first phase) of septic shock. Other signs and symptoms of early septic shock include fever with restlessness and confusion; normal or decreased blood pressure with tachypnea and tachycardia; increased or normal urine output; and nausea and vomiting or diarrhea. Cool, clammy skin occurs in the hypodynamic or cold phase (later phase). Hemorrhage is not a factor in septic shock.
Question 105.
A client with toxic shock has been receiving ceftriaxone sodium, 1 g every 12 hours. In addition to culture and sensitivity studies, what other laboratory finding should the nurse monitor?
(a) serum creatinine
(b) spinal fluid analysis
(c) arterial blood gases
(d) serum osmolality
Answer:
(a) serum creatinine
Explanation:
The nurse monitors the blood levels of antibiotics, white blood cells, serum creatinine, and blood urea nitrogen because of the decreased perfusion to the kidneys, which are responsible for filtering out the ceftriaxone sodium. It is possible that the clearance of the antibiotic has been decreased enough to cause toxicity. Increased levels of these laboratory values should be reported to the health care provider (HCP) immediately.
A spinal fluid analysis is done to examine cerebral spinal fluid, but there is no indication of central nervous system involvement in this case. Arterial blood gases are used to determine actual blood gas levels and assess acid-base balance. Serum osmolality is used to monitor fluid and electrolyte balance.
Question 106.
Which nursing intervention is most important in preventing septic shock?
(a) administering IV fluid replacement therapy as prescribed
(b) obtaining vital signs every 4 hours for all clients
(c) monitoring red blood cell counts for elevation
(d) maintaining asepsis of indwelling urinary catheters
Answer:
(d) maintaining asepsis of indwelling urinary catheters
Explanation:
Maintaining asepsis of indwelling urinary catheters is essential to prevent infection. Preventing septic shock is a major focus of nursing care because the mortality rate for septic shock is as high as 90% in some populations. Very young and elderly clients (those younger than age 2 or older than age 65) are at increased risk for septic shock. Administering IV fluid replacement therapy, obtaining vital signs every 4 hours on all clients, and monitoring red blood cell counts for elevation do not pertain to septic shock prevention.
Question 107.
Which finding is an indication of a complication of septic shock?
(a) anaphylaxis
(b) acute respiratory distress syndrome (ARDS)
(c) chronic obstructive pulmonary disease (COPD)
(d) mitral valve prolapse
Answer:
(b) acute respiratory distress syndrome (ARDS)
Explanation:
ARDS is a complication associated with septic shock. ARDS causes respiratory failure and may lead to death, even after the client has recovered from shock. Anaphylaxis is a type of distributive or vasogenic shock. COPD is a functional category of pulmonary disease that consists of persistent obstruction of bronchial airflow and involves chronic bronchitis and chronic emphysema. Mitral valve prolapse is a condition in which the mitral valve is pushed back too far during ventricular contraction.
Question 108.
A nurse is taking care of two clients who have a prescription to receive a blood transfusion of packed red blood cells at the same time. The first client’s blood pressure dropped from the preoperative value of 120/80 mm Hg to a postoperative value of 100/50 mm Hg. The second client is hospitalized because he developed dehydration and anemia following pneumonia. After checking the patency of their IV lines and vital signs, what should the nurse do next?
(a) Call for both clients’ blood transfusions at the same time.
(b) Ask another nurse to verify the compatibility of both units at the same time.
(c) Call for and hang the first client’s blood transfusion.
(d) Ask another nurse to call for and hang the blood for the second client.
Answer:
(c) Call for and hang the first client’s blood transfusion.
Explanation:
When two clients are to receive blood at the same time, the nurse should call for and hang the clients’ transfusions separately to avoid error. The nurse should call for and hang the first client’s blood first because this client has experienced a change in blood pressure over a short period of time. The nurse should next call and hang the second cli-ent’s blood transfusion as there is no indication that this client is unstable at this time.
The nurse should not call for both units of transfusions at the same time due to the increased risk of misidentification. The nurse should not verify compatibility of both units at the same time due to the increased risk of misidentification. It is not necessary to involve two nurses because the second client can wait until the nurse has time to hang the blood.
Question 109.
When a blood transfusion is terminated following a reaction, what actions must the nurse take? Select all that apply.
(a) Send freshly collected urine samples to the laboratory.
(b) Return the remainder of the blood component unit to the blood bank.
(c) Return the intravenous administration set to the blood bank.
(d) Alert Risk Management about the incident.
(e) Report the incident to the Infection Control Manager.
Answer:
(a) Send freshly collected urine samples to the laboratory.
(b) Return the remainder of the blood component unit to the blood bank.
(c) Return the intravenous administration set to the blood bank.
(d) Alert Risk Management about the incident.
Explanation:
(a), (b), (c), (d). If a blood transfusion is terminated, the nurse must send a freshly collected blood sample to the blood bank and a urine sample to the laboratory; the nurse must send the blood component unit with the attached administration set and completed Transfusion Reaction Form to the blood bank. It is not necessary to inform Infection Control, but the Risk Management department should be notified, since a transfusion reaction may be a significant liability issue.
Question 110.
The nurse is administering a medication to a client with myeloid leukemia and does not know the use, dose, or side effects. To obtain the most up-to-date information about this drug, what should the nurse do?
(a) Check a commercially published drug guide.
(b) Read a pharmacology textbook.
(c) Consult the drug guide provided by the clinical agency.
(d) Review information at the drug manufacturer’s website.
Answer:
(c) Consult the drug guide provided by the clinical agency.
Explanation:
The most current pharmacology information is found in the clinical agency’s drug guide, which may be available on electronic sources that are frequently updated and can be transmitted to
a handheld device or by logging into the Internet or hospital’s intranet, if available. A commercially published drug guide and pharmacology textbooks are outdated once published and, therefore, may not have current information. The manufacturer’s website has the potential for bias.
Question 111.
The charge nurse on a hematology/oncology unit is reviewing the policy for using abbreviations with the staff. The charge nurse should emphasize which information about why dangerous abbreviations need to be eliminated? Select all that apply.
(a) to ensure efficient and accurate communication
(b) to prevent medication errors
(c) to ensure client safety
(d) to make it easier for clients to understand the medication prescriptions
(e) to make data entry into a computerized health record easier
Answer:
(a) to ensure efficient and accurate communication
(b) to prevent medication errors
(c) to ensure client safety
Explanation:
(a), (b), (c). Abbreviations can be misinterpreted, and all health care professionals should avoid the use of easily misunderstood abbreviations. The purpose of avoiding abbreviations is not to make it easier for clients to understand the medication prescriptions or to make data entry easier.
Question 112.
The nurse is delegating care of client with neutropenia who is in isolation to an unlicensed assistive personnel (UAP). What information should the nurse give the UAP about the care of this client?
(a) listening and responding to the client’s feelings of concern
(b) completing the client’s care in a calm, unhurried manner
(c) completing all of the client’s care for the shift at one time
(d) instructing the client to dispose of the tissue used after blowing the nose
Answer:
(d) instructing the client to dispose of the tissue used after blowing the nose
Explanation:
The most common source of infection and microbial colonization in neutropenic clients is their own nonpathogenic normal flora. Attention to personal hygiene, such as oral, pulmonary, urinary, and rectal care, is essential. It is important to acknowledge the client’s concerns and fears and to provide organized, calm, compassionate care, but it is more important to teach the client how to prevent an infection that could be life-threatening.
Read More: