By reviewing NCLEX Exam Questions, students can identify common themes and patterns in exam content, improving their chances of success.
NCLEX Child with Respiratory Health Problems Questions
Child with Respiratory Health Problems NCLEX Practice Questions
Question 1.
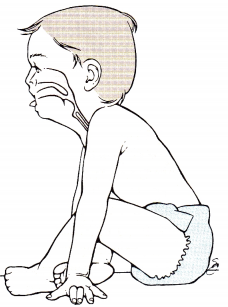
The nurse is inspecting the child’s throat (see figure). How should the nurse proceed with the throat exam?
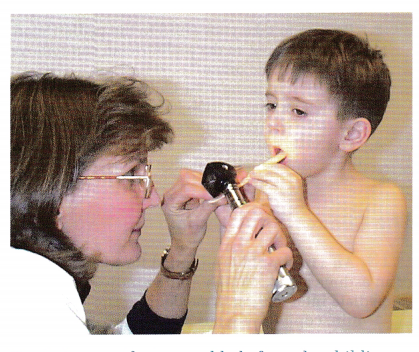
(a) Remove the tongue blade from the chi1ds hands after he has experienced what it feels like in his mouth.
(b) Ask the child to hold the tongue blade with both hands in his lap while the nurse uses another tongue blade.
(c) Have the parent hold the child with arms restrained.
(d) Guide the tongue blade while the child is holding it to depress the tongue to visualize the throat.
Answer:
(d) Guide the tongue blade while the child is holding it to depress the tongue to visualize the throat.
Explanation:
If the child does not stick out his tongue so the nurse can visualize the throat, it is appropriate to use a tongue blade. Having the child participate by holding the tongue blade while the nurse guides it to facilitate visualization of the throat is appropriate technique. It is not useful to remove the tongue blade or have the child hold it because the nurse will need to use the tongue blade to depress the tongue. It is preferable to engage the child’s cooperation before asking the parent to restrain the child.
Question 2.
The nurse has identified a problem of anxiety for a 4-year-old preparing for a tonsillectomy. What should the nurse tell the child?
(a) “You will not have so many sore throats after your tonsils are removed.”
(b) “The doctor will put you to sleep so you do not feel anything.”
(c) “Show me how to give the doll an IV.”
(d) “Tfl it is done, you will get to see your mommy and get a Popsicle.”
Answer:
(d) “Tfl it is done, you will get to see your mommy and get a Popsicle.”
Explanation:
When preparing a child for a procedure the nurse should use neutral words, focus on sensory experiences, and emphasize the positive aspects at the end. Being reunited with parents and having a popsicle would be considered pleasurable events. Children this age fear bodily harm. To reduce anxi-ety, the nurse should use the word “fixed” instead of “removed” to describe what is being done to the tonsils. Using the terms “put to sleep” and “IV” may be threatening. Additionally, directing a play experience to focus on IV insertion may be counterproductive as the child may have little recollection of this aspect of the procedure.
Question 3.
After a tonsillectomy and adenoidectomy, which finding should alert the nurse to suspect early hemorrhage in a 5-year-old child?
(a) drooling of bright red secretions
(b) pulse rate of 95 bpm
(c) vomiting of 25 mL of dark brown ernesis
(d) blood pressure of 95/56 mnì Hg
Answer:
(a) drooling of bright red secretions
Explanation:
After a tonsillectomy and adenoidectomy, drooling bright red blood is considered an early sign of hemorrhage. Often, because of discomfort in the throat, children tend to avoid swallowing; instead, they drool. Frequent swallowing would also be an indication of hemorrhage because the child attempts to clear the airway of blood by swallowing. Secretions may be slightly blood-tinged because of a small amount of oozing after surgery.
However, bright red secretions indicate bleeding. A pulse rate of 95 bpm is within the normal range for a 5-year- old child, as is a blood pressure of 95/56 mm Hg. A small amount of blood that is partially digested, and therefore dark brown, is often present in postoperative emesis.
Question 4.
The nurse is offering nutritional instruction to the parents of a preschooler who has undergone a tonsillectomy and adenoidectomy. What food choice by the parents would indicate successful teaching?
(a) meat loaf and uncooked carrots
(b) pork and noodle casserole
(c) cream of chicken soup and orange sherbet
(d) hot dog and potato chips
Answer:
(c) cream of chicken soup and orange sherbet
Explanation:
For the first few days after a tonsillectomy and adenoidectomy, liquids and soft foods are best tolerated by the child while the throat is sore. Children typically do not chew their food thoroughly, and solid foods are to be avoided because they are difficult to swallow. Although meat loaf would be considered a soft food, uncooked carrots would not be. Pork is frequently difficult to chew. Foods that have sharp edges, such as potato chips, are contraindicated because they are hard to chew and may cause more throat discomfort.
Question 5.
A nurse is teaching the parents of a preschooler about the possibility of postoperative hemorrhage after a tonsillectomy and adenoidectomy. When should the nurse explain that the risk of bleeding is the greatest?
(a) 1 to 3 days after surgery
(b) 4 to 6 days after surgery
(c) 7 to 10 days after surgery
(d) 11 to 14 days after surgery
Answer:
(c) 7 to 10 days after surgery
Explanation:
The risk of hemorrhage from a tonsillectomy is greatest when the tissue begins sloughing and the scabs fall off. This typically happens 7 to 10 days after a tonsillectomy.
Question 6.
A toddler is scheduled to have tympanostomy tubes inserted. When approaching thu toddler for the first time, which should the nurse do?
(a) Talk to the mother first so that the toddler can get used to the now person.
(b) Hold the toddler so thai the toddler becomes more comfortable.
(c) Walk over and pick the toddler up right away so that the mimother can relax.
(d) Pick up the toddler and take the child to the play area so that the mother can rest.
Answer:
(a) Talk to the mother first so that the toddler can get used to the now person.
Explanation:
Toddlers should be approached slowly because they are wary of strangers and need time to get used to someone they do not know. The best approach is to ignore them initially and to focus on talking to the parents. The child will likely resist being held by a stranger, so the nurse should not pick up or hold the child until the child indicates a readiness to be approached or the mother indicates that it is okay.
Question 7.
After insertion of bilateral tympanostomy tubes in a toddler, which instructions should the nurse include in the child’s discharge plan for the parents?
(a) Insert ear plugs into the canals when the child bathes.
(b) Gently clean the ear canal with cotton swabs.
(c) Administer antibiotics daily while the tubos are in place.
(d) Disregard any drainage from the ear after 1 week.
Answer:
(a) Insert ear plugs into the canals when the child bathes.
Explanation:
Placing ear plugs in the ears will prevent contaminated bathwater from entering the middle ear through the tympanostomy tube and causing an infection. Inserting cotton swabs into the ear canal is not recommended. Antibiotics may be given for a short period after insert and are appropriate only when an ear infection is present. Tympanostomy tubes may remain in place for several years. It is not necessary to administer antibiotics continuously to a child with a tympanostomy tube. Drainage from the ear may be a sign of middle ear infection and should be reported to the health care provider (HCP) .
Question 8.
The nurse caring for mi 3-year-old with otitis media notes thai the client has an allergy to amoxicillin that causes wheezing. Which prescription should the nurse question?
(a) azithromvcin
(b) cephalexin
(c) trimethoprim-sulfamethoxazole
(d) cefdinir
Answer:
(b) cephalexin
Explanation:
Cephalexin is a first-generation cephalosporin. Because clients with a history of anaphylaxis to penicillin, or related antibiotics, have an increased risk of having a cross-reaction to first- generation cephalosporin, the nurse should question a prescription for cephalexin. Azithromycin is not usually considered to be a first-line antibiotic for ear infections in pediatric clients but is effective in pediatric clients with an allergy to amoxicillin.
Trimethoprim-sulfamethoxazole is effective against middle ear infections and can be used effectively in pediatric clients with an allergy to amoxicillin. Second- and third-generation cephalosporins, like cefdinir, do not have the same rates of cross-sensitivities to penicillins as first-generation cephalosporin and may be prescribed for pediatric clients with an allergy to amoxicillin.
Question 9.
After teaching the parents of a toddler about commonly aspirated foods, which food, if identified by the parents as easily aspirated. would indicate the need for additional teaching?
(a) popcorn
(b) raw vegetables
(c) round candy
(d) crackers
Answer:
(d) crackers
Explanation:
Crackers, because they crumble and easily dissolve, are not commonly aspirated. Because children commonly eat popcorn hulls or pieces that have not popped, popcorn can be easily aspirated. Toddlers frequently do not chew their food well, making raw vegetables a commonly aspirated food. Round candy is often difficult to chew and comes in large pieces, making it easily aspirated.
Question 10.
A toddler who has been treated for a foreign body aspiration begins to fuss and cry when the parents attempt to leave the hospital for an hour. As the nurse tries to take the child oui of the crib, the child pushes the nurse away. The nurse interprets this behavior as indicating which stage of separation anxiety?
(a) protest
(b) despair
(c) regression
(d) detachment
Answer:
(a) protest
Explanation:
Young children have specific reactions to separation and hospitalization. In the protest stage, the toddler physically and verbally attacks anyone who attempts to provide care. Here, the child is fussing and crying and visibly pushes the nurse away. In the despair stage, the toddler becomes withdrawn and obviously depressed (e.g., not engaging in play activities and sleeping more than usual).
Regression is a return to a developmentally earlier phase because of stress or crisis (e.g., a toddler who could feed himself before this event is not doing so now). Denial or detachment occurs if the toddler’s stay in the hospital without the parent is prolonged because the toddler settles in to the hospital life and denies the parents’ existence (e.g., not reacting when the parents come to visit).
Question 11.
The nurse teaches the three cardinal signs of choking and total airway blockage to the parents of a toddler who was treated for a foreign body obstruction. When asked to repeat the signs. the parents identify “turn blue” and “cannot speak.” what( third sign would the parents identify if teaching was successful?
(a) vomits
(b) gasps
(c) gags
(d) collapses
Answer:
(d) collapses
Answer:
The three cardinal signs indicating that a child is truly choking and requires immediate life saving interventions include inability to speak, blue color (cyanosis), and collapse. Vomiting does not occur while a child is unable to breathe. Once the object is dislodged, however, vomiting may occur. Gasping, a sudden intake of air, indicates that the child is still able to inhale. When a child is choking, air is not being exchanged, so gagging will not occur.
Question 12.
The father of a 2-year•old phones the emergency department on a Sunday evening and informs the nurse that his son put a bead in his nose. What is the most appropriate recomjnondation made by the nurse?
(a) “Try to remove the beed at home as soon as possible: you might try using a pair of tweezers.”
(b) “Be sure to take your child to the pediatrician in the morning so tue pediatrician can remove the bead In the office.”
(c) “You should bring your child to the emergency department tonight so the bead can be removed as soon as possible.”
(d) “Ask your child to blow his nose several times; this should dislodge the bead.”
Answer:
(d) “Ask your child to blow his nose several times; this should dislodge the bead.”
Explanation:
The bead should be removed by a health care professional as soon as possible to prevent the risk of aspiration and tissue necrosis. Unskilled individuals should not attempt to remove an object from the nose as they may push the object further increasing the risk for aspiration. Two-year-old children are not skilled at blowing their nose and may breathe in, further increasing the risk of aspiration.
Question 13.
An 11-veer-old is admitted for treatment of an asthma attack. Which finding indicates immediate intervention is needed?
(a) thin, copious mucous secretions
(b) productive cough
(c) intercostal retractions
(d) respiratory rate of 20 breaths/mm
Answer:
(c) intercostal retractions
Explanation:
Intercostal retractions indicate an increase in respiratory effort, which is a sign of respiratory distress. During an asthma attack, secretions are thick, the cough is tight, and respiration is difficult (and shortness of breath may occur). If mucous secretions are copious but thin, the client can expectorate them, which indicates an improvement in the condition. If the cough is productive, it means the bronchospasms and the inflammation have been resolved to the extent that the mucus can be expectorated. A respiratory rate of 20 breaths/ min would be considered normal and no intervention would be needed.
Question 14.
A 12-year-old with asthma wants to exercise. Which activity should the nurse suggest to improve breathing?
(a) soccer
(b) swimming
(c) track
(d) gymnastics
Answer:
(b) swimming
Explanation:
Swimming is appropriate for this child because it requires controlled breathing, assists in maintaining cardiac health, enhances skeletal muscle strength, and promotes ventilation and perfusion. Stop-and-start activities, such as soccer, track, and gymnastics, commonly trigger symptoms in asthmatic clients.
Question 15.
When preparing the teaching plan for the mother of a child with asthma, what information should the nurse include as a sign to alert the mother that her child is having an asthma attack?
(a) secretion of thin, copious mucus
(b) tight, productive cough
(c) wheezing on expiration
(d) temperature of 99.4°F (37.4°C)
Answer:
(c) wheezing on expiration
Explanation:
The child who is experiencing an asthma attack typically demonstrates wheezing on expiration initially. This results from air moving through narrowed airways secondary to bronchoconstriction. The child’s expiratory phase is normally longer than the inspiratory phase.
Expiration is passive as the diaphragm relaxes. During an asthma attack, secretions are thick and are not usually expelled until the bronchioles are more relaxed. At the beginning of an asthma attack, the cough will be tight but not productive. Fever is not always present unless there is an infection that may have triggered the attack.
Question 16.
Which assessment findings should lead the nurse to suspect that a toddler is experiencing respiratory distress? Select all that apply.
(a) coughing
(b) respiratory rate of 35 breaths/min
(c) heart rate of 95 beats/min
(d) restlessness
(e) malaise
(f) diaphoresis
Answer:
(a) coughing
(b) respiratory rate of 35 breaths/min
(d) restlessness
(e) malaise
Explanation:
(a), (b), (d), (e) Coughing, especially at night and in the absence of an infection, is a common symptom of asthma. Early signs of respiratory distress include restlessness, tachypnea, tachycardia, and diaphoresis. Other signs also include hypertension, nasal flaring, grunting, wheezing, and intercostal retractions. A heart rate of 95 bpm is normal for a toddler. Malaise typically does not indicate respiratory distress.

Question 17.
A child, who uses an inhaled bronchodilator only when needed for asthma, has a best peak expiratory flow rate of 270 L/min. The child’s current peak flow reading is 180 L/min. How does the nurse interpret this reading?
(a) The child’s asthma is under good control, so the routine treatment plan should continue.
(b) The child needs to use short-acting, inhaled beta2-agonist medication.
(c) To the emergency department for treatment.
(d) The child needs to use inhaled cromolyn sodium.
Answer:
(b) The child needs to use short-acting, inhaled beta2-agonist medication.
Explanation:
The peak flow of 180 L/min is in the yellow zone, or 50% to 80% of the child’s personal best. This means that the child’s asthma is not well controlled, thereby necessitating the use of a short-acting beta2-agonist medication to relieve the bronchospasm. A peak flow reading > 80% of the child’s personal best (in this case, 220 L/min or better) would indicate that the child’s asthma is in the green zone or under good control.
A peak flow reading in the red zone, or < 50% of the child’s personal best (135 L/min or less), would require notification of the health care provider (HCP) or a trip to the emergency department. Cromolyn sodium is not used for short-term treatment of acute broncho¬spasm. It is used as part of a long-term therapy regimen to help desensitize mast cells and thereby help to prevent symptoms.
Question 18.
An adolescent with chest pain goes to the nurse. The nurse determines that the teenager has a history of asthma but has had no problems for years. What should the nurse do next?
(a) Call the adolescent’s parent.
(b) Have the adolescent lie down for 30 minutes.
(c) Obtain a peak flow reading.
(d) Have the teen take two puffs of a short-acting bronchodilator.
Answer:
(c) Obtain a peak flow reading.
Explanation:
Problems of chest pain in children and adolescents are rarely cardiac. With a history of asthma, the most likely cause of the chest pain is related to the asthma. Therefore, the nurse should check the adolescent’s peak flow reading to evaluate the status of the airflow. Calling the adolescent’s parent would be appropriate, but this would be done after the nurse obtains the peak flow reading and additional assessment data.
Having the adolescent lie down may be an option, but more data need to be collected to help establish a possible cause. Because the adolescent has not experienced any asthma problems for a long time, it would be inappropriate for the nurse to administer a short-acting bronchodi-lator at this time.
Question 19.
A 7-year-old child with a history of asthma controlled without medications is referred to the school nurse by the teacher because of persistent coughing. What should the nurse do first?
(a) Obtain the child’s heart rate.
(b) Give the child a PRN nebulizer treatment.
(c) Call a parent to obtain more information.
(d) Have a parent come and pick up the child.
Answer:
(c) Call a parent to obtain more information.
Explanation:
Because persistent coughing may indicate an asthma attack and a 7-year-old child would be able to provide only minimal history information, it would be important to obtain information from the parent. Although determining the child’s heart rate is an important part of the assessment, it would be done after the history is obtained. More informa-tion needs to be obtained before giving the child a nebulizer treatment. Although it may be necessary for the parent to come and pick up the child, a thorough assessment including history information should be obtained first.
Question 20.
When developing a teaching plan for the parent of an asthmatic child concerning measures to reduce allergic triggers, which suggestion should the nurse include?
(a) Have the child bring his or her own pillow when sleeping away from home.
(b) If using bunk beds, have the child sleep on the bottom.
(c) Use a scented room deodorizer to keep the room fresh.
(d) Vacuum the carpet once or twice a week.
Answer:
(a) Have the child bring his or her own pillow when sleeping away from home.
Explanation:
Down pillows and exposure to dust mites are common allergic triggers. The family can reduce exposure to bedding related allergens during travel or sleepovers by having the child bringing a pillow from home. Typically, the child with asthma should sleep in the top bunk bed to minimize the risk of exposure to dust mites. The risk of exposure to dust mites increases when the child sleeps in the bottom bunk bed because dust mites fall from the top bed, settling in the bottom bed.
Scented sprays should be avoided because they may trigger an asthmatic episode. Ideally, carpeting should be avoided in the home if the child has asthma. However, if it is present, carpeting in the child’s room should be vacuumed often, possibly daily, to remove dust mites and dust particles.
Question 21.
After discussing asthma as a chronic condition, which statement by the parent of a child with asthma best reflects the family’s positive adjustment to this aspect of the child’s disease?
(a) “We try to keep him happy at all costs; otherwise, he has an asthma attack.”
(b) “We keep our child away from other children to help cut down on infections.”
(c) “Although our child’s disease is serious, we try not to let it be the focus of our family.”
(d) “I’m afraid that when my child gets older, he will not be able to care for himself like I do.”
Answer:
(c) “Although our child’s disease is serious, we try not to let it be the focus of our family.”
Explanation:
Positive adjustment to a chronic condition requires placing the child’s illness in its proper perspective. Children with asthma need to be treated as normally as possible within the scope of the limitations imposed by the illness. They also need to learn how to manage exacerbations and then resume as normal a life as possible. Trying to keep the child happy at all costs is inappropriate and can lead to the child’s never learning how to accept responsibility for behavior and get along with others.
Although minimizing the child’s risk for exposure to infections is important, the child needs to be with his or her peers to ensure appropriate growth and development. Children with a chronic illness need to be involved in their care so that they can learn to manage it. Some parents tend to overprotect their child with a chronic illness. This overprotectiveness may cause a child to have an exaggerated feeling of importance or later, as an adolescent, to rebel against the overprotectiveness and the parents.
Question 22.
A child with asthma states, “I want to play some sports like my friends. What can I do?” The nurse responds to the child based on the understanding of which information?
(a) Physical activities are inappropriate for children with asthma.
(b) Children with asthma must be excluded from team sports.
(c) Vigorous physical exercise frequently precipitates an asthmatic episode.
(d) Most children with asthma can participate in sports if the asthma is controlled.
Answer:
(d) Most children with asthma can participate in sports if the asthma is controlled.
Explanation:
Physical activities are beneficial to asthmatic children, physically and psychosocially. Most children with asthma can engage in school and sports activities that are geared to the child’s condition and within the limits imposed by the disease. The coach and other team members need to be aware of the child’s condition and know what to do in case an attack occurs. Those children who have exercise-induced asthma usually use a short-acting bronchodilator before exercising.
Question 23.
A child with cystic fibrosis does not like taking a pancreatic enzyme supplement with meals and snacks. The parent does not like to force the child
to take the supplement. What is the most important reason for the child to take the pancreatic enzyme supplement with meals and snacks?
(a) The child will become dehydrated if the supplement is not taken with meals and snacks.
(b) The child needs these pancreatic enzymes to help the digestive system absorb fats, carbohydrates, and proteins.
(c) The child needs the pancreatic enzymes to aid in liquefying mucus to keep the lungs clear.
(d) The child will experience severe diarrhea if the supplement is not taken as prescribed.
Answer:
(b) The child needs these pancreatic enzymes to help the digestive system absorb fats, carbohydrates, and proteins.
Explanation:
The child must take the pancreatic enzyme supplement with meals and snacks to help absorb nutrients so he can grow and develop normally. In cystic fibrosis, the normally liquid mucus is tenacious and blocks three digestive enzymes from entering the duodenum and digesting essential nutrients.
Without the supplemental pancreatic enzyme, the child will have voluminous, foul, fatty stools due to the undigested nutrients and may experience developmental delays due to malnutrition. Dehydration is not a problem related to cystic fibrosis. The pancreatic enzymes have no effect on the viscosity of the tenacious mucus. Diarrhea is not caused by failing to take the pancreatic enzyme supplement.
Question 24.
An adolescent with cystic fibrosis has been hospitalized several times. On the latest admission, the client has labored respirations, fatigue, malnu¬trition, and failure to thrive. Which initial nursing actions are most important?
(a) placing the client on bed rest and obtaining a prescription for a blood gas analysis
(b) implementing a high-calorie, high-protein, low-fat, vitamin-enriched diet and pancreatic granules
(c) applying an oximeter and initiating respiratory therapy
(d) inserting an IV line and initiating antibiotic therapy
Answer:
(c) applying an oximeter and initiating respiratory therapy
Explanation:
Clients with cystic fibrosis commonly die from respiratory problems. The mucus in the lungs is tenacious and difficult to expel, leading to lung infections and interference with oxygen and carbon dioxide exchange. The client will likely need supplemental oxygen and respiratory treatments to maintain adequate gas exchange, as identified by the oximeter reading. The child will be on bed rest due to respiratory distress. However, although blood gases will probably be prescribed, the oximeter readings will be used to determine oxygen deficit and are, therefore, more of a priority.
A diet high in calories, proteins, and vitamins with pancreatic granules added to all foods ingested will increase nutrient absorption and help the malnutrition; however, this intervention is not the priority at this time. Inserting an IV to administer antibiotics is important and can be done after ensuring adequate respiratory function.
Question 25.
A child with cystic fibrosis is receiving gentamicin. Which nursing action is most important?
(a) monitoring intake and output
(b) obtaining daily weights
(c) monitoring the client for indications of constipation
(d) obtaining stool samples to test for occult blood
Answer:
(a) monitoring intake and output
Explanation:
Monitoring intake and output is the most important nursing action when administering an aminoglycoside, such as gentamicin, because a decrease in output is an early sign of renal damage. Daily weight monitoring is not indicated when the client is receiving an aminoglycoside. Constipation and bleeding are not adverse effects of aminoglycosides.
Question 26.
When developing the plan of care for a child with cystic fibrosis (CF) who is scheduled to receive postural drainage, the nurse should anticipate performing postural drainage at which times?
(a) after meals
(b) before meals
(c) after rest periods
(d) before inhalation treatments
Answer:
(b) before meals
Explanation:
Postural drainage, which aids in mobilizing the thick, tenacious secretions commonly associated with CF, is usually performed before meals to avoid the possibility of vomiting or regurgitating food. Although the child with CF needs frequent rest periods, this is not an important factor in scheduling postural drainage. However, the nurse would not want to interrupt the child’s rest period to perform the treatment. Inhalation treatments are usually given before postural drainage to help loosen secretions.
Question 27.
The nurse assesses the results of a gentamicin trough blood level for an adolescent with cystic fibrosis who has had been treated with gentamicin several times over the last year. The drug level is high. What is the nurse’s primary concern?
(a) The child may develop liver dysfunction.
(b) The child may suffer hearing loss.
(c) The medication may have been administered incorrectly.
(d) The child may need to have a different antibiotic.
Answer:
(b) The child may suffer hearing loss.
Explanation:
When given for an extended period of time, aminoglycoside antibiotics can cause permanent hearing loss. The high trough level may indicate that the child has decreased kidney function and is not clearing the drug out of their system efficiently. While hepatotoxicity has been shown in isolated reports, changes in liver function resolve rapidly once gentamicin is stopped.
While errors in medication administration can cause abnormal lab results, the child’s clinical history and frequency of gentamicin use support an elevated blood level. The lab result indicates that the dose of gentamicin may need to be decreased.
Question 28.
What toy should the nurse include as part of a recreational therapy plan of care for a 3-year- old child hospitalized with pneumonia and cystic fibrosis?
(a) 100-piece jigsaw puzzle
(b) child’s favorite doll
(c) fuzzy stuffed animal
(d) scissors, paper, and paste
Answer:
(b) child’s favorite doll
Explanation:
The child’s favorite doll would be a good choice of toys. The doll provides support and is familiar to the child. Although a 3-year-old may enjoy puzzles, a 100-piece jigsaw puzzle is too complicated for an ill 3-year-old child. In view of the child’s lung pathology, a fuzzy stuffed animal would not be advised because of its potential as a reservoir for dust and bacteria, possibly predisposing the child to additional respiratory problems. Scissors, paper, and paste are not appropriate for a 3-year-old unless the child is supervised closely.
Question 29.
Which factor, if described by the parents of a child with cystic fibrosis (CF), indicates understanding the underlying problem of the disease?
(a) an abnormality in the body’s mucus-secreting glands
(b) formation of fibrous cysts in various body organs
(c) failure of the pancreatic ducts to develop properly
(d) reaction to the formation of antibodies against streptococcus
Answer:
(a) an abnormality in the body’s mucus-secreting glands
Explanation:
CF is characterized by a dysfunction in the body’s mucus-producing exocrine glands. The mucus secretions are thick and sticky rather than thin and slippery. The mucus obstructs the bronchi, bronchioles, and pancreatic ducts. Mucus plugs in the pancreatic ducts can prevent pancreatic digestive enzymes from reaching the small intestine, resulting in poor digestion and poor absorption of various food nutrients.
Fibrous cysts do not form in various organs. Cystic fibrosis is an autosomal recessive inherited disorder and does not involve any reaction to the formation of antibodies against streptococcus.
Question 30.
Which outcome criterion would the nurse develop for a child with cystic fibrosis who has ineffective airway clearance related to increased pulmonary secretions and inability to expectorate?
(a) respiratory rate and rhythm within expected range
(b) absence of chills and fever
(c) ability to engage in age-related activities
(d) ability to tolerate usual diet without vomiting
Answer:
(a) respiratory rate and rhythm within expected range
Explanation:
After treatment, the client outcome would be that respiratory status would be within normal limits, as evidenced by a respiratory rate and rhythm within expected range. Absence of chills and fever, although related to an underlying problem causing the respiratory problem (e.g., the infection], does not specifically relate to the respiratory problem of ineffective airway clearance.
The child’s ability to engage in age-related activities may provide some evidence of improved respiratory status. However, this outcome criterion is more directly related to activity intolerance. Although the child’s ability to tolerate his or her usual diet may indirectly relate to respiratory function, this outcome is more specifically related to an imbalanced nutrition that may or may not be related to the child’s respiratory status.
Question 31.
A school-age client with cystic fibrosis asks the nurse what sports she can become involved in as she becomes older. What is the best information for the nurse to provide about sports and cystic fibrosis?
(a) “The best sport is one that you will enjoy and do regularly.”
(b) “Swimming is the best exercise for anyone with cystic fibrosis.”
(c) “You should avoid contact sports where you might experience a blow to the chest.”
(d) “Indoor sports have lower risks of infection than outdoor sports.”
Answer:
(a) “The best sport is one that you will enjoy and do regularly.”
Explanation:
Responses to physical activity among children with cystic fibrosis vary greatly; therefore, plans of care must be individualized. Selecting a sport that the child likes and will do regularly is most important because children with CF who exercise regularly have better health and quality of life. Many children with CF tolerate and enjoy swimming, but some children do not. There are no universal recommendations that children with CF should not engage in contact sports. There is evidence to suggest that clients who exercise outdoors are at greater risk of infection compared to those who exercise indoors.
Question 32.
When explaining to parents how to reduce the risk of sudden infant death syndrome (SIDS), the nurse should teach about which measures? Select all that apply.
(a) Maintain a smoke-free environment.
(b) Use a wedge for side-lying positions.
(c) Breastfeed the baby.
(d) Place the baby on his or her back to sleep.
(e) Use bumper pads over the bed rails.
(f) Have the baby sleep in the parent’s bed.
Answer:
(a) Maintain a smoke-free environment.
(c) Breastfeed the baby.
(d) Place the baby on his or her back to sleep.
Explanation:
(a), (c), (d) Exposure to environmental tobacco increases the risk for SIDS. Sleeping on the back and breastfeeding both decrease the risk of SIDS. The side-lying position is not recommended for sleep. It is recommended that babies be dressed in sleepers and that cribs are free of blankets, pillows, bumper pads, and stuffed animals. Cobedding with parents is not recommended as parents may roll on the child.
Question 33.
Which child is most at risk for sudden infant death syndrome (SIDS)?
(a) infant who is 3 months old
(b) 2-year-old who has apnea lasting up to 5 seconds
(c) firstborn child whose parents are in their early 40s
(d) 6-month-old who has had two bouts of pneumonia
Answer:
(a) infant who is 3 months old
Explanation:
The highest incidence of SIDS occurs in infants between ages 2 and 4 months. About 90% of SIDS occurs before the age of 6 months. Apnea lasting longer than 20 seconds has also been associated with a higher incidence of SIDS. SIDS occurs with higher frequency in families where a child in the family has already died of SIDS, but the age of the parents has not been shown to contribute to SIDS. A respiratory infection such as pneumonia has not been shown to cause a higher incidence of SIDS.
Question 34.
Parents bring their infant to the emergency department because the child has stopped breathing. A nurse obtains a brief history of events occurring before and after the parents found the infant not breathing. Which question should the nurse ask the parents first?
(a) “Was the infant sleeping while wrapped in a blanket?”
(b) “Was the infant lying on his stomach?”
(c) “What did the infant look like when you found him?”
(d) “When had you last checked on the infant?”
Answer:
(c) “What did the infant look like when you found him?”
Explanation:
Because this is an especially disturbing and upsetting time for the parents, they must be approached in a sensitive manner. Asking what the infant looked like when found allows the parents to verbalize what they saw and felt, thereby helping to minimize their feelings of guilt without implying any blame, neglect, wrongdoing, or abuse. Asking if the child was wrapped in a blanket or lying on his stomach, or when the parents last checked on the infant, implies that the parents did something wrong or failed in their care of the infant, thus blaming them for the event.
Question 35.
When planning a visit to the parents of an infant who died of sudden infant death syndrome (SIDS) at home, the nurse should visit the parents at which time?
(a) a few days after the funeral
(b) 2 weeks after the funeral
(c) as soon as the parents are ready to talk
(d) as soon after the infant’s death as possible
Answer:
(d) as soon after the infant’s death as possible
Explanation:
The community health nurse should visit as soon after the death as possible because the parents may need help to deal with the sudden, unexpected death of their infant. Parents often have a great deal of guilt in these situations and need to express their feelings to someone who can provide counseling.
Question 36.
A child has just ingested about 10 adult- strength acetaminophen tablets an hour ago. The mother brings the child to the emergency department. What should the nurse do? Place the interventions in the order of priority from first to last. All options must be used.
(a) Administer activated charcoal.
(b) Assess the airway.
(c) Check serum acetaminophen levels.
(d) Administer acetylcysteine.
Answer:
(b) Assess the airway.
(c) Check serum acetaminophen levels.
(a) Administer activated charcoal.
(d) Administer acetylcysteine.
Explanation:
(b), (c), (a), (d) Care of children with an acetaminophen overdose is based on time of ingestion. Immediate care of the child is to ensure airway, breathing, and circulation. If it has been < 4 hours since ingestion, activated charcoal should be given. Acetaminophen levels should be drawn at 4 hours post ingestion. Depending on the findings, acetylcysteine may also be used as an antidote.
Question 37.
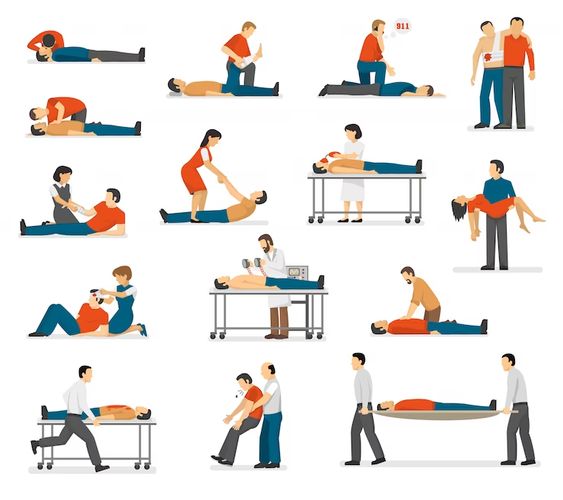
On finding a child who is not breathing, the nurse has someone activate the emergency medical system and then does what first?
(a) Clear the airway.
(b) Begin mouth-to-mouth resuscitation.
(c) Initiate oxygen therapy.
(d) Start chest compressions.
Answer:
(d) Start chest compressions.
Explanation:
The current CPR guidelines call for a CAB approach. When breathlessness is determined, the priority nursing action is checking a pulse and beginning compressions. After 30 compressions, the nurse opens the airway and gives 2 breaths. Oxygen therapy would not be initiated at this time because the child is not breathing. Also, administering oxy-gen therapy would interfere with providing mouth- to-mouth resuscitation.
Question 38.
Which breathing rates should the nurse use when performing rescue breathing during cardiopulmonary resuscitation for a 5-year-old?
(a) 10 breaths/min
(b) 12 breaths/min
(c) 15 breaths/min
(d) 20 breaths/min
Answer:
(a) 10 breaths/min
Explanation:
Rescue breaths should be delivered slowly at a volume that makes the chest rise and fall. For a 5-year-old child, the rate is 10 breaths/ min. If the nurse is also administering chest compressions, the rate is 2 breaths for every 30 compressions.
Question 39.
The nurse begins CPR on a 5-year-old unre-sponsive client. When the emergency response team arrives, the child continues to have no respiratory effort but has a heart rate of 50 with cyanotic legs. What should the team do next?
(a) Continue administering breaths with a bag-mask device without compressions.
(b) Suspend CPR briefly to apply defibrillation patches.
(c) Begin 2-person CPR at a ratio of 2 breaths to 15 compressions.
(d) Begin 2-person CPR at a ratio of 2 breaths to 30 compressions.
Answer:
(c) Begin 2-person CPR at a ratio of 2 breaths to 15 compressions.
Explanation:
CPR is done on children for heart rate of <60 with signs of poor perfusion. Rescuers should use a 15:2 compression to ventilation ratio for 2-rescuer CPR for a child. Breaths without compressions are indicated only for respiratory arrests where the heart rate remains above 60. The AED/defibrillator should be used as soon as it is ready, but rescuers should not discontinue compressions until the device is ready for use. The ratio for 2-person CPR in adults is 30 : 2.
Question 40.
As part of a health education program, the nurse teaches a group of parents CPR. The nurse determines that the teaching had been effective when a parent makes which statement about providing CPR to a child?
(a) “If I am by myself, I should call for help before starting CPR.”
(b) “I should compress a child’s chest using 2 to 3 fingers.”
(c) “I should deliver chest compression at a rate of 100 per minute.”
(d) “If I cannot get the breaths to make the chest rise, I should administer abdominal thrusts.”
Answer:
(c) “I should deliver chest compression at a rate of 100 per minute.”
Explanation:
To maintain the best perfusion, it is recommended that compressions be given at a rate of 100 per minute in a ratio of 30 compressions to 2 breaths for 1-rescuer CPR. Children still are more likely to have had a respiratory arrest than a cardiac arrest and are more likely to respond to opening the airway and rescue breaths.
Therefore, it is recommended that unless the collapse was witnessed, a sole rescuer should attempt 5 cycles of CPR before leaving to call for help. Using 2 to 3 fingers for chest compressions is recommended for infant CPR only. Abdominal thrusts are no longer recommended for unconscious victims.
Question 41.
When performing cardiopulmonary resuscitation (CPR), which finding indicates that external chest compressions are effective?
(a) mottling of the skin
(b) pupillary dilation
(c) palpable pulse
(d) cool, dry skin
Answer:
(c) palpable pulse
Explanation:
With CPR, effectiveness of external chest compressions is indicated by palpable peripheral pulses, the disappearance of mottling and cyanosis, the return of pupils to normal size, and warm, dry skin. To determine whether the victim of cardiopulmonary arrest has resumed spontaneous breathing and circulation, chest compressions must be stopped for 5 seconds at the end of the first minute and every few minutes thereafter.
Question 42.
A nurse walks into the room just as a 10-month-old infant places an object in his mouth and starts to choke. After opening the infant’s mouth, which should the nurse do next to clear the airway?
(a) Use blind finger sweeps.
(b) Deliver back slaps and chest thrusts.
(c) Apply four subdiaphragmatic abdominal thrusts.
(d) Attempt to visualize the object.
Answer:
(b) Deliver back slaps and chest thrusts.
Explanation:
The nurse should use mechanical force back slaps and chest thrusts in an attempt to dislodge the object. Blind finger sweeps are not appropriate in infants and children because the foreign body may be pushed back into the airway. Sub diaphragmatic abdominal thrusts are not used for infants aged 1 year or younger because of the risk of injury to abdominal organs. If the object is not visible when opening the mouth, time is wasted in looking for it. Action is required to dislodge the object as quickly as possible.
Question 43.
A young child has had a cardiac arrest, and the rapid response team has been activated. The nurse arrives in the client’s room and observes a licensed practical/vocational nurse (LPN/VN) administering CPR to an infant (see figure). What should the nurse do to assist the LPN/VN with CPR?
(a) Take over rescue breaths with a rate of 1 breath per 5 compressions using a bag-mask device while the LPN/VN continues compressions.
(b) Take over compressions using one hand while the LPN/VN uses a mask device to administer rescue breaths.
(c) Take over rescue breaths using a rate of 2 breaths per 15 compressions using a bag-mask device while the LPN/VN delivers compressions.
(d) Take over compressions at 80 compressions a minute while the LPN/VN uses a bag-mask device to administer rescue breaths.
Answer:
(c) Take over rescue breaths using a rate of 2 breaths per 15 compressions using a bag-mask device while the LPN/VN delivers compressions.
Explanation:
The nurse should first obtain a bag-mask device and assist with CPR by giving breaths at 2 breaths/15 compressions. The LPN/VN Q is using correct technique by using one hand on the chest to administer chest compressions. The heel of both hands is used for older children and adolescents. The compression rate is at least 100 per minute
Question 44.
When teaching the parents of an infant how to perform back slaps to dislodge a foreign body, what should the nurse tell the parents to use to deliver the blows?
(a) palm of the hand
(b) heel of the hand
(c) fingertips
(d) entire hand
Answer:
(b) heel of the hand
Explanation:
Back slaps are delivered rapidly and forcefully with the heel of the hand between the infant’s shoulder blades. Slowly delivered back slaps are less likely to dislodge the object. Using the heel of the hand allows more force to be applied than when using the palm or the whole hand, increasing the likelihood of loosening the object. The fingertips would be used to deliver chest com¬pressions to an infant younger than 1 year of age.
Question 45.
While the nurse is delivering abdominal thrusts to a 6-year-old who is choking on a foreign body, the child begins to cry. What should the nurse do next?
(a) Tap or gently shake the shoulders.
(b) Deliver back slaps.
(c) Perform a blind finger sweep of the mouth.
(d) Observe the child closely.
Answer:
(d) Observe the child closely.
Explanation:
Crying indicates that the airway obstruction has been relieved. No additional thrusts are needed. However, the child needs to be observed closely for complications, including respiratory distress. Tapping or shaking the shoulders is used initially to determine unresponsiveness in someone who appears unconscious. Delivering chest
or back slaps could jeopardize the child’s now- patent airway. Because the obstruction has been relieved, there is no need to sweep the child’s mouth. Additionally, blind finger sweeps are contraindicated because the object may be pushed further back, possibly causing a complete airway obstruction.
Question 46.
The parent of a 16-month-old child calls the clinic because the child has a low-grade fever, cold symptoms, and a hoarse cough. What should the nurse suggest that the parent do?
(a) Offer extra fluids frequently.
(b) Bring the child to the clinic immediately.
(c) Count the child's respiratory rate.
(d) Use a hot air vaporizer.
Answer:
(a) Offer extra fluids frequently.
Explanation:
The toddler is exhibiting cold symptoms. A hoarse cough may be part of the upper respiratory tract infection. The best suggestion is to have the father offer the child additional fluids at frequent intervals to help keep secretions loose and membranes moist. There is no evidence presented to suggest that the child needs to be brought to the clinic immediately.
Although having the father count the child’s respiratory rate may provide some additional information, it may lead the father to suspect that something is seriously wrong, possibly leading to undue anxiety. A hot air vaporizer is not recom-mended. However, a cool mist vaporizer would cause vasoconstriction of the respiratory passages, making it easier for the child to breathe and loosening secretions.
Question 47.
A 21-month-old child admitted with the diagnosis of croup now has a respiratory rate of 48 breaths/min, a heart rate of 120 bpm, and a tem-perature of 100.8°F (38.2°C) rectally. The nurse is having difficulty calming the child. What should the nurse do next?
(a) Administer acetaminophen.
(b) Notify the health care provider (HCP) immediately.
(c) Allow the toddler to continue to cry.
(d) Offer clear fluids every few minutes.
Answer:
(b) Notify the health care provider (HCP) immediately.
Explanation:
The nurse may be having difficulty calming the child because the child is experiencing increasing respiratory distress. The normal respiratory rate for a 21-month-old is 25 to 30 breaths/ min. The child’s respiratory rate is 48 breaths/min. Therefore, the HCP Qj] needs to be notified immediately. Typically, acetaminophen is not given to a child unless the temperature is 101°F (38.6°C) or higher.
Letting the toddler cry is inappropriate with croup because crying increases respiratory distress. Offering fluids every few minutes to a toddler experiencing increasing respiratory distress would do little, if anything, to calm the child. Also, the child would have difficulty coordinating breathing and swallowing, possibly increasing the risk of aspiration.
Question 48.
A child has viral pharyngitis. What should the nurse advise the parents to do? Select all that apply.
(a) Use a cool mist vaporizer.
(b) Offer a soft-to-liquid diet.
(c) Administer amoxicillin.
(d) Administer acetaminophen.
(e) Place the child on secretion precautions.
Answer:
(a) Use a cool mist vaporizer.
(b) Offer a soft-to-liquid diet.
(d) Administer acetaminophen.
Explanation:
(a), (b), (d) Viral pharyngitis is treated with symptomatic, supportive therapy. Treatment includes use of a cool mist vaporizer, feeding a soft or liquid diet, and administration of acetaminophen for comfort. Viral infections do not respond to antibiotic administration. The child does not need to be on secretion precautions because viral pharyngitis is not contagious.
Question 49.
A parent brings a 3-month-old infant to the clinic, reporting that the infant has a cold, is having trouble breathing, and “just does not seem to be acting right.” Which action should the nurse take first?
(a) Check the infant’s heart rate.
(b) Weigh the infant.
(c) Assess the infant’s oxygen saturation.
(d) Obtain more information from the parent.
Answer:
(c) Assess the infant’s oxygen saturation.
Explanation:
In an infant with these symptoms, the first action by the nurse would be to obtain an oxygen saturation reading to determine how well the infant is oxygenating. Because the parent probably can provide no other information, checking the heart rate would be the second action done by the nurse. Then the nurse would obtain the infant’s weight.
Question 50.
The nurse assessment of a 6-month-old infant brought to the outpatient clinic reveals a respiratory rate of 52 breaths/min, retractions, and wheezing. The mother states that her infant was doing fine until yesterday. Which action would be most appropriate?
(a) Administer a nebulizer treatment.
(b) Send the infant for a chest radiograph.
(c) Refer the infant to the emergency department.
(d) Provide teaching about cold care to the mother.
Answer:
(c) Refer the infant to the emergency department.
Explanation:
Based on the assessment findings of increased respiratory rate, retractions, and wheezing, this infant needs further evaluation, which could be obtained in an emergency department. Without a definitive diagnosis, administering a nebulizer treatment would be outside the nurse’s scope of practice unless there was a prescription for such a treatment.
Sending the infant for a radiograph may not be in the nurse’s scope of practice. The findings need to be reported to an HCP who can then determine whether or not a chest radiograph is warranted. The infant is exhibiting signs and symptoms of respiratory distress and is too ill to send out with just instructions on cold care for the mother.
Question 51.
An infant is being treated at home for bronchiolitis. What should the nurse teach the parent about home care? Select all that apply.
(a) offering small amounts of fluids frequently
(b) allowing the infant to sleep prone
(c) calling the clinic if the infant vomits
(d) writing down how much the infant drinks
(e) performing chest physiotherapy every 4 hours
(f) watching for difficulty breathing
Answer:
(a) offering small amounts of fluids frequently
(e) performing chest physiotherapy every 4 hours
Explanation:
(a), (e) An infant with bronchiolitis will have increased respirations and will tire more quickly, so it is best and easiest for the infant to take fluids more often in smaller amounts. The parents also would be instructed to watch for signs of increased difficulty breathing, which signal possible complications. Healthy infants and even those with bronchi-olitis should sleep in the supine position. Calling the clinic for an episode of vomiting would not be necessary.
However, the parents would be instructed to call if the infant cannot keep down any fluids for a period of more than 4 hours. Parents would not need to record how much the infant drinks. Chest physiotherapy is not indicated because it does not help and further irritates the infant.
Question 52.
In preparation for discharge, the nurse teaches the mother of an infant diagnosed with bronchiolitis about the condition and its treatment. Which statement by the mother indicates successful teaching?
(a) ‘‘I need to be sure to take my child’s temperature every day.”
(b) “I hope I do not get a cold from my child.”
(c) “Next time my child gets a cold I need to listen to the chest.”
(d) “I need to wash my hands more often.”
Answer:
(d) “I need to wash my hands more often.”
Explanation:
Handwashing is the best way to prevent respiratory illnesses and the spread of disease. Bronchiolitis, a viral infection primarily affecting the bronchioles, causes swelling and mucus accumulation of the lumina and subsequent hyperinflation of the lung with air trapping. It is transmitted primarily by direct contact with respiratory secretions as a result of eye-to-hand or nose-to-hand contact or from contaminated fomites. Therefore, handwashing minimizes the risk for transmission. Taking the child’s temperature is not appropriate in most cases.
As long as the child is getting better, taking the temperature will not be helpful. The mother’s statement that she hopes she does not get a cold from her child does not indicate understanding of what to do after discharge. For most parents, listening to the child’s chest would not be helpful because the parents would not know what they were listening for. Rather, watching for an increased respiratory rate, fever, or evidence of poor eating or drinking would be more helpful in alerting the parent to potential illness.
Question 53.
The nurse observes an 18-month-old who has been admitted with a respiratory tract infection who is drooling (see figure). What should the nurse do first?
(a) Position the child supine.
(b) Call the rapid response team.
(c) Suction the airway.
(d) Administer oxygen.
Answer:
(b) Call the rapid response team.
Explanation:
The nurse should suspect epiglottitis in any young child with a respiratory infection who sits leaning forward with an open mouth and protruding tongue and is drooling. Epiglottitis is a medical emergency. The rapid response team fU should be notified to secure the airway. While waiting for the team, the child should remain sitting upright to facilitate breathing; complete obstruction may occur if the child is placed prone or becomes agitated. Therefore, it is important to avoid any procedures that upset the child such as suctioning or applying oxygen.
Question 54.
A teaching care plan to prevent the transmission of respiratory syncytial vims (RSV) should include what information? Select all that apply.
(a) The virus can be spread by direct contact.
(b) The virus can be spread by indirect contact.
(c) Palivizumab is recommended to prevent RSV for all toddlers in day care.
(d) The virus is typically contagious for 3 weeks.
(e) Older children seldom spread RSV.
(f) Frequent handwashing helps reduce the spread of RSV.
Answer:
(a) The virus can be spread by direct contact.
(b) The virus can be spread by indirect contact.
(e) Older children seldom spread RSV.
Explanation:
(a), (b) (e) RSV can be spread through direct contact such as kissing the face of an infected person, and it can be spread through indirect contact by touching surfaces covered with infected secretions. Handwashing is one of the best ways to reduce the risk of disease transmission. Palivizumab can prevent severe RSV infections but is only recommended for the most at-risk infants and children. RSV is typically contagious for 3 to 8 days. RSV frequently manifests in older children as cold-like symptoms. Infected school-age children frequently spread the virus to other family members.
Question 55.
A charge nurse is making assignments for a group of children on a pediatric unit. Which client should the nurse most avoid assigning the same nurse caring for a 2-year-old with respiratory syncytial virus (RSV)?
(a) an 18-month-old with RSV
(b) a 9-year-old 8 hours post appendectomy
(c) a 1-year-old with a heart defect
(d) a 6-year-old with sickle cell crisis
Answer:
(c) a 1-year-old with a heart defect
Explanation:
RSV may be spread through both direct and indirect contact. While contact and standard precautions should be employed, a measure to further decrease the risk of nosocomial infections is to avoid assigning the same nurse caring for an RSV client to a client at risk for infection. A private room is preferred, but if this is not an option, the nurse should understand that children 2 years of age and younger are most at risk for RSV, especially if they have other chronic problems such as a heart defect. From an infection control perspective, pairing two clients with RSV is ideal. RSV infections are less likely to pose a serious problem in older children.
Question 56.
The nurse is preparing to administer the last dose of ceftriaxone before discharge to a 1-year- old but finds the IV has occluded. What should the nurse do?
(a) Restart the IV.
(b) Administer the medication intramuscularly.
(c) Document that the last dose was withheld.
(d) Contact the prescriber to request a prescription change.
Answer:
(d) Contact the prescriber to request a prescription change.
Explanation:
Restarting an IV for one dose of a medication may not be in the infant’s best interest when the medication can be given in an alternate form. The prescriber should be contacted to determine IM or PO options. Ceftriaxone may be given IM, but changing the route of a medication administration requires a prescription. While reasons for giving a medication late would be indicated, the failing to complete an entire course of antibiotics contributes to the emergence of antibiotic resistance, and withholding the medicine would rarely be the best option.
Question 57.
A nurse administers cefazolin instead of cef-triaxone to an 8-year-old with pneumonia. The client has suffered no adverse effects. The nurse tells the charge nurse of the incident but fears disciplinary action from reporting the error. What should the charge nurse tell the nurse?
(a) “If you do not report the error, I will have to.”
(b) “Reporting the error helps to identify system problems to improve client safety.”
(c) “Notify the client’s health care provider to see if she wants this reported. "
(d) “This is not a serious mistake, so reporting it will not affect your position.”
Answer:
(b) “Reporting the error helps to identify system problems to improve client safety.”
Explanation:
Client safety is enhanced when the emphasis on medication errors is to determine the root cause. All errors should be reported so systems can identify patterns that contribute to errors. Here, the similar names probably contributed to the error. The nurse who commits the error knows all the relevant information and is in the best position to report it. While the health care provider (HCP) m should be notified, it is a nursing responsibility to report errors, not an HCP’s choice. Relating mistakes to a nurse’s position focuses on personal blame.
Question 58.
A 12-year-old with cystic fibrosis is being treated in the hospital for pneumonia. The health care provider (HCP) is calling in a telephone prescription for ampicillin. The nurse should take which actions? Select all that apply.
(a) Ask the unit clerk to listen on the speaker phone with the nurse and write down the prescription.
(b) Ask the HCP to come to the hospital and write the prescription on the medical record.
(c) Repeat the prescription to the HCP.
(d) Ask the HCP to confirm that the prescription is correct as understood by the nurse.
(e) Ask the nursing supervisor to cosign the telephone prescription as transcribed by the nurse.
Answer:
(c) Repeat the prescription to the HCP.
(d) Ask the HCP to confirm that the prescription is correct as understood by the nurse.
Explanation:
(c), (d) To ensure client safety in obtaining telephone prescriptions, the prescription must be received by a registered nurse fRNI LD. The nurse should write the prescription, read the prescription back to the HCP (LCj, and receive confirmation from the HCP that the prescription is correct. It is not necessary to ask the unit clerk to listen to the prescription, to require the HCP to come to the hospital to write the prescription on the medical record ITl. or to have the nursing supervisor cosign the telephone prescription.
Question 59.
The triage nurse in the emergency department must prioritize the children waiting to be seen. Which child is in the greatest need of emergency medical treatment?
(a) a 6-year-old with a fever of 104°F (40°C), a muffled voice, no spontaneous cough, and drooling
(b) a 3-year-old with a fever of 100°F (37.8°C), a barky cough, and mild intercostal retractions
(c) a 4-year-old with a fever of 101°F (38.3°C), a hoarse cough, inspiratory stridor, and restlessness
(d) a 13-year-old with a fever of 104°F (40°C), chills, and a cough with thick yellow secretions
Answer:
(a) a 6-year-old with a fever of 104°F (40°C), a muffled voice, no spontaneous cough, and drooling
Explanation:
This child is exhibiting signs and symptoms of epiglottitis, which is a medical emergency due to the risk of complete airway obstruction. The 3- and 4-year-olds are exhibiting signs and symptoms of croup. Symptoms often diminish after the child has been taken out in the cool night air. If symptoms do not improve, the child may need a single dose of dexamethasone. Fever should also be treated with antipyretics. The 13-year-old is exhibiting signs and symptoms of bronchitis. Treatment includes rest, antipyretics, and hydration.
Question 60.
A 6-month-old on the pediatric floor has a respiratory rate of 68, mild intercostal retractions, and oxygen saturation of 89%. The infant has not been feeding well for the last 24 hours and is restless. Using the situation, background, assessment, and recommendation (SBAR) technique for communication, the nurse calls the health care provider (HCP) with the recommendation for which treatment?
(a) starting oxygen
(b) providing sedation
(c) transferring to pediatric intensive care
(d) prescribing a chest CT scan
Answer:
(a) starting oxygen
Explanation:
The infant is experiencing signs and symptoms of respiratory distress indicating the need for oxygen therapy. Sedation will not improve the infant’s respiratory distress and would likely cause further respiratory depression. If the infant's respira-tory status continues to decline, she may need to be transferred to the pediatric intensive care. Oxygen should be the priority as it may improve the infant’s respiratory status. A chest CT is not indicated. However, a CXR would be another appropriate recommendation for this infant.
Question 61.
A child with cystic fibrosis has been admitted to the pediatric unit. What type of diet should the nurse request for the client?
(a) high-fat, high-carbohydrate
(b) high-calorie, high-protein
(c) high-calorie, high-carbohydrate
(d) high-carbohydrate, high-protein
Answer:
(b) high-calorie, high-protein
Explanation:
A high-calorie, high-protein diet is necessary to ensure adequate growth. Some children require up to two times the recommended daily allowance of calories (an increased calorie diet includes foods high in fat and balanced carbohydrates). Pancreatic enzyme activity is lost, and malabsorption of fats, proteins, and carbohydrates occurs.
Also Read: