Working through NCLEX PN Study Guide can boost confidence and reduce test anxiety by building familiarity and competence.
NCLEX Health Promotion Questions - NCLEX Questions on Health Promotion
Health Promotion NCLEX Practice Questions
Question 1.
After reading the vaccine information sheets, the parent of a 2-month-old infant is hesitant to consent to the recommended vaccinations. What should the nurse ask the parent first?
(a) “Did you know that vaccinations are required by law for school entry?”
(b) “What concerns do you have about vaccinations?”
(c) “Would you prefer that fewer vaccines are given at a time?”
(d) “Can you please sign this vaccine waiver form?”
Answer:
(b) “What concerns do you have about vaccinations?”
Explanation:
By trying to determine the source of parents’ concerns, the nurse is able to acknowledge their feelings and provide the most appropriate informa¬tion. This approach increases the likelihood parents will listen to the health care provider’s (HCP’s) views.
Exemptions for vaccines vary by state, prov¬ince, or territory, and many parents feel legal require-ments for vaccinations take away parental rights. The number of vaccinations given at one time may not be the issue. Waivers are used only if clients refuse vaccination after a discussion of risks and benefits.
Question 2.
The nurse assesses an 8-month-old’s language development. Which finding would the nurse consider to be typical language development?
(a) saying “dada” to father and “mama” to mother
(b) saying three other words besides “mama” and “dada”
(c) saying “dada” and “mama” nonspecifically
(d) saying “mama” and “dada” while pointing to the parent
Answer:
(c) saying “dada” and “mama” nonspecifically
Explanation:
It is important for the nurse to assist parents in assessing speech development in their child so that developmental delays can be identified early. At 8 months of age, the child should say “mama” and “dada” nonspecifically and imitate speech sounds. Children cannot say “dada” or “mama” specifically or use more than three words until they are about 12 months of age. A child cannot respond to specific commands or point to objects when requested until about 17 months of age.
Question 3.
The nurse should refer the parents of an 8-month-old child to a health care provider (HCP) if the child is unable to demonstrate which gross motor ability?
(a) stand momentarily without holding onto furniture
(b) stand unsupported well for long periods of time
(c) stoop to recover an object on the ground
(d) sit without support for long periods of time
Answer:
(d) sit without support for long periods of time
Explanation:
According to the Denver Developmental Screening Examination, a child of 8 months should sit without support for long periods of time. An 8-month-old child does not have the ability to stand without hanging onto a stationary object for support. His or her muscles are not developed enough to support all his weight without assistance. His or her balance has not developed to the point that he or she can stand and stoop over to reach an object.
Question 4.
The nurse is teaching the parents of an 8-month-old about what the child should eat. The nurse should include which information points in the teaching plan?
(a) Vegetables should be introduced before fruits when the infant is 6 months old.
(b) Solid foods should not be introduced until the infant is 10 months old.
(c) Iron-fortified cereals should not be introduced until the infant is 8 months old.
(d) Formula can be changed to whole milk when the infant is 12 months old.
Answer:
(c) Iron-fortified cereals should not be introduced until the infant is 8 months old.
Explanation:
Infants should be kept on formula or breast milk until 1 year of age. The protein in cow’s milk is harder to digest than the protein found in formula. It does not matter in what order fruits and vegetables are introduced as long as the foods are introduced slowly. Solids are introduced into the infant’s diet around 4 to 6 months, after the extrusion reflex has diminished and when the child will accept new textures.
Iron deficiency develops in term infants between 4 to 6 months when the prenatal iron stores are depleted. Fortified cereals can be added to the infant’s diet at 4 to 6 months to prevent iron deficiency anemia.
Question 5.
A 10-month-old looks for objects that have been removed from his view. How does the nurse explain the finding to the parents?
(a) The child is showing typical neuromuscular development.
(b) The child’s curiosity has increased.
(c) The child understands objects are there even though the child cannot see them.
(d) The child is now able to transfer objects from hand to hand.
Answer:
(c) The child understands objects are there even though the child cannot see them.
Explanation:
Understanding object permanence means that the child is aware of the existence of objects that are covered or displaced. Neuromuscular development, curiosity, and the ability to transfer objects are not associated with the principle of object permanence. Although, at 10 months, neuromuscular development is sufficient to grasp objects and a child’s curiosity has increased, neither are related to the thought process involved in object permanence.
Question 6.
Which structure should be closed by the time the child is 2 months old?
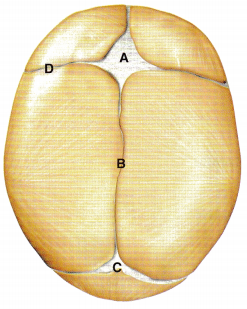
(a) A
(b) B
(c) C
(d) D
Answer:
(c) C
Explanation:
The posterior fontanelle should be closed by age 2 months. The anterior fontanelle and sagittal and frontal sutures should be closed by age 18 months.
Question 7.
Which statement by a parent reflects the need for further teaching regarding car seat safety?
(a) “My baby should stay in a rear-facing car seat until he is 1 year old.”
(b) “I should check my old car seat’s expiration date before using it for this baby.”
(c) “My older child will need to stay in a booster seat until he is 4 feet 9 inches (144.8 cm).”
(d) “My children should ride in the back seat until they are 13 years old.”
Answer:
(a) “My baby should stay in a rear-facing car seat until he is 1 year old.”
Explanation:
New guidelines recommend that parents keep their toddlers in a rear-facing car seat until 2 years of age or they reach maximum height and weight for the seat. Car seats are marked with an expiration date because the integrity of the plastic may deteriorate with age. Booster seats are recom-mended for older children until they are 4 feet 9 inches (144.8 cm). This typically occurs between the ages 8 and 12 years. Children should ride in the back seat until they are 13 years of age to minimize injury should airbags be deployed.
Question 8.
The parents of a 3-week-old healthy newborn ask the nurse why their child is intermittently crosseyed. What is the nurse’s best response?
(a) “An eye patch may be necessary for to correct your child’s vision.”
(b) “Your child will likely need an ophthalmology consult.”
(c) “It is normal to have eye-crossing in the new born period.”
(d) “Surgery may be necessary to correct your child’s vision.”
Answer:
(c) “It is normal to have eye-crossing in the new born period.”
Explanation:
During the first few months of life, an infant’s eyes may wander and appear to be crossing. As the eye muscles mature, between 2 and 3 months of age, both eyes will focus on the same thing. No intervention is necessary, as crossing of the eyes is normal in the first few months of life.
Question 9.
A parent brings a 4-month-old to the clinic for a regular well visit and expresses concern that the infant is not developing appropriately. Which finding in the infant would indicate the need for further developmental screening?
(a) has no interest in peekaboo games
(b) does not turn front to back
(c) does not babble
(d) does not without support
Answer:
(c) does not babble
Explanation:
By the end of 3 months, infants should babble. Lack of babbling suggests a language delay and warrants further investigation. Infants typically would begin playing peekaboo around 7 months. The ability to roll front to back typically occurs at 5 months. Sitting unsupported is expected at 6 months.
Question 10.
The nurse assesses a 6-month-old for vaccination readiness. Which finding would most likely indicate the need to delay administering the diphtheria, tetanus, and acellular pertussis (DTaP) vaccine?
(a) a family history of sudden infant death syndrome (SIDS)
(b) a fever of 38.5°C (101.3°F) following the 4-month vaccinations C
(c) an acute bilateral ear infection
(d) living with a family member who is immunosuppressed
Answer:
(c) an acute bilateral ear infection
Explanation:
Vaccination in the presence of a mod- erate-to-severe infection, with or without fever, increases the risk of injury and decreases the chance of mounting good immunity. An acute bilateral ear infection would constitute a moderate infection/ illness.
There is currently no evidence to suggest vaccines raise the risk of SIDS. A mild temperature may be expected with the DTaP. A fever of > 40.5°C (105°F) within 48 hours of vaccination would warrant caution. The DTaP is not a live vaccine. No special precautions are needed regarding immuno-suppressed family members.
Question 11.
The parents of a 9-month-old bring the infant to the clinic for a regular checkup. The infant has received no immunizations. Which vaccine if prescribed would the nurse question?
(a) diphtheria, tetanus, and acellular pertussis (DTaP)
(b) Haemophilus influenzae type B (HIb)
(c) measles, mumps, and rubella (MMR)
(d) inactivated influenza (Flu)
Answer:
(c) measles, mumps, and rubella (MMR)
Explanation:
The MMR is a live vaccine. Neither the American Academy of Pediatrics nor the Public Health Agency of Canada recommends routine vaccination with the MMR (either alone or combined with the varicella vaccine) to children younger than 12 months. The DTaP, Hib, and influenza are all indicated.
Question 12.
To assess the development of a 1-month-old, the nurse asks the parent if the infant is able to demonstrate which skill?
(a) smile and laugh out loud
(b) roll from back to side
(c) hold a rattle briefly
(d) lift head from prone position
Answer:
(d) lift head from prone position
Explanation:
A 1-month-old infant is usually able to lift the head from a prone position. The full-term infant with no complications has probably been able to do this since birth. Smiling and laughing is expected behavior at 2 to 3 months. Rolling from back to side and holding a rattle are characteristics of a 4-month-old.
Question 13.
The parent of a 6-month-old reports starting 2% milk. What should the nurse ask the parent first?
(a) “Do you think your baby will be fine with this milk?”
(b) “Is it possible for you to switch your baby to whole milk?”
(c) “Can you tell me more about the reason you switched your baby to 2% milk?”
(d) “You cannot switch to 2% milk right now. Did your pediatrician tell you to do this?”
Answer:
(c) “Can you tell me more about the reason you switched your baby to 2% milk?”
Explanation:
The American Academy of Pediatrics and Canadian Pediatric Society recommend that infants remain on iron-fortified formula or breast milk until 1 year of age. The nurse needs to first assess if the parent switched the baby prematurely to due to lack of information or lack of resources.
Then appropriate teaching or referrals may be determined. At 1 year of age, the infant may be switched to whole milk, which has a higher fat content than 2%. The higher fat content is needed for brain growth. Demanding clients change behaviors without addressing the cause is unlikely to produce desired results.
Question 14.
The nurse notes that an infant stares at an object placed in his hand and takes it to his mouth, coos and gurgles when talked to, and sustains part of his own weight when held in a standing position. The nurse correctly interprets these findings as characteristic of an infant at which age?
(a) 2 months
(b) 4 months
(c) 7 months
(d) 9 months
Answer:
(b) 4 months
Explanation:
Holding the head erect when sitting, staring at an object placed in the hand, taking the object to the mouth, cooing and gurgling, and sustaining part of his body weight when in a standing position are behaviors characteristic of a 4-month-old infant.
A 2-month-old typically vocalizes, follows objects to the midline, and smiles. A 7-month-old typically is able to sit without support, turns toward the voice, and transfers objects from hand to hand. Usually, a 9-month-old can crawl, stand while holding on, and initiate speech sounds.
Question 15.
An 8-month-old infant is seen in the well- child clinic for a routine checkup. The nurse should expect the infant to be able to do which tasks? Select all that apply.
(a) saying “mama” and “dada” with specific meaning
(b) feeding self with a spoon
(c) playing peekaboo
(d) walking independently
(e) stacking two blocks
(f) transferring an object from hand to hand
Answer:
(c) playing peekaboo
(e) stacking two blocks
Explanation:
(c) (e) Typical abilities demonstrated by 8-month-old infants include playing peekaboo and transferring objects from one hand to another. The ability to say “dada” and “mama” is more typical of 10-month-old infants. Infants usually are at least 12 months old when they achieve the ability to walk independently. Infants who are 15 months old commonly can feed themselves with a spoon and stack two blocks.
Question 16.
The parent of a 9-month-old infant is concerned that the infant’s front soft spot is still open. What should the nurse tell the parent?
(a) “I will measure your baby’s head to see if it is a normal size.”
(b) “Your infant will need to be referred for more testing.”
(c) “You should contact your health care provider immediately.”
(d) “This is normal because this soft spot usually closes between 12 and 18 months.”
Answer:
(d) “This is normal because this soft spot usually closes between 12 and 18 months.”
Explanation:
The anterior fontanelle, commonly known as the soft spot, closes between 12 to 18 months in most infants. The nurse normally measures an infant’s occipital frontal circumference at each well-child visit. This action alone does not relieve the parent’s concerns. Referrals would be indicated for premature or delayed closures of the
fontanelle especially if there were other abnormal findings. Closure of the anterior fontanelle by 12 months can only be expected to occur in approximately a third of all infants.
Question 17.
The parent of a 9-month-old expressed concern that the baby “is developing slowly.” The nurse is concerned about a developmental delay when finding the baby is unable to accomplish which skill?
(a) vocalizing single syllables
(b) standing alone
(c) building a tower of two cubes
(d) drinking from a cup with little spilling
Answer:
(a) vocalizing single syllables
Explanation:
Typically, a 9-month-old infant should have been voicing single syllables since 6 months of age. Absence of this finding would be a cause for concern. An infant usually is able to stand alone at about 10 months of age. An infant usually is able to build a tower of two cubes at about 15 months of age. An infant usually is able to drink from a cup with little spilling at about 15 months of age.
Question 18.
Which infant most needs a developmental referral for a gross motor delay?
(a) the 2-month-old who does not roll over
(b) the 4-month-old who does not sit without support
(c) the 6-month-old who does not crawl
(d) the 9-month-old who does not stand holding on
Answer:
(d) the 9-month-old who does not stand holding on
Explanation:
More than 90% of 9-month-olds are able to stand holding onto objects. Rolling over is expected at 4 to 6 months, and sitting without sup¬port is expected at 6 months. Crawling is expected at 9 months.
Question 19.
Which intervention should the nurse employ to reduce trauma caused by vaccine administration to an infant?
(a) Use a 5/8-inch (1.6-cm) needle.
(b) Simultaneously administer vaccines at separate sites with a second nurse.
(c) Aspirate to verify needle placement.
(d) Breastfeed right before administering the vaccines.
Answer:
(b) Simultaneously administer vaccines at separate sites with a second nurse.
Explanation:
Simultaneous injection reduces the anxiety from anticipation of the next injection. Needle length must be long enough to deposit the vaccine into the muscle. A 5/8-inch (1.6-cm) needle is appropriate for newborns but is not long enough for infants older than 1 month or other children. Aspirating for blood return does not confirm needle placement. Breastfeeding during vaccinations, not before, has been found to reduce pain.
Question 20.
An uncle is shopping for a toy to give his niece. He has no children of his own and asks his neighbor, a nurse, what would be the most appropriate toy to give a 15-month-old child. Which toy should the nurse recommend to facilitate learning and development?
(a) a stuffed animal
(b) a music box
(c) a push-pull toy
(d) a nursery mobile
Answer:
(c) a push-pull toy
Explanation:
A push-pull toy will aid in development of gross motor skills and muscle development. A stuffed animal is age appropriate for a toddler but is not the toy to promote development. A music box and nursery mobile are most appropriate to stimulate development for an infant.
Question 21.
A 2-year-old tells his parent he is afraid to go to sleep because “the monsters will get him.” What should the nurse tell the parent to do?
(a) Allow him to sleep with his parents in their bed whenever he is afraid.
(b) Increase his activity before he goes to bed so he eventually falls asleep from being tired.
(c) Read a story to him before bedtime, and allow him to have a cuddly animal or a blanket.
(d) Allow him to stay up an hour later with the family until he falls asleep.
Answer:
(c) Read a story to him before bedtime, and allow him to have a cuddly animal or a blanket.
Explanation:
Behavior problems related to sleep and rest are common in young children. Consistent rituals around bedtime help to create an easier transition from waking to sleep. Allowing a child to sleep with his parents commonly creates more problems for the family and child and does not alleviate the problem or foster autonomy.
Increasing activity before bed-time does not alleviate the separation anxiety in the toddler and causes further anxiety. Allowing him to stay up later than his normal time for bed will increase his anxiety, make it more difficult for him to fall asleep, and do nothing to lessen his fear.
Question 22.
A 2-year-old always puts his teddy bear at the head of his bed before he goes to sleep. The parents ask the nurse if this behavior is normal. The nurse should explain to the parents that toddlers use ritualistic patterns to establish which factor?
(a) a sense of identity
(b) control over adults in their environment
(c) sequenced patterns of learning behavior
(d) a sense of security
Answer:
(d) a sense of security
Explanation:
Toddlers establish ritualistic patterns to feel secure, despite inconsistencies in their environment. Establishing a sense of identity is the developmental task of the adolescent. The toddler’s developmental task is to use rituals and routines to help in making autonomy easier to accomplish. Ritualistic patterns do involve patterns of behavior, but they are not utilized to develop learning behaviors.
Question 23.
Which development is necessary for toilet training readiness for a 2-year-old? Select all that apply.
(a) adequate neuromuscular development for sphincter control
(b) appropriate chronological age
(c) ability to communicate the need to use the toilet
(d) desire to please the parents
(e) ability to play with other 2-year-olds
Answer:
(a) adequate neuromuscular development for sphincter control
(c) ability to communicate the need to use the toilet
(d) desire to please the parents
Explanation:
(a), (c), (d) Readiness for toilet training is based on neurological, psychological, and physical developmental readiness. The nurse can introduce concepts of readiness for toilet training and encourage parents to look for adaptive and psychomotor signs such as the ability to walk well, balance, climb, sit in a chair, dress oneself, please the parent, and communicate awareness of the need to urinate or defecate. Chronological age is not an indicator for toilet training. Two-year-olds engage in parallel play, which is not an indicator of readiness for toilet training.
Question 24.
A parent of a toilet-trained 3-year-old expresses concern over her child’s bed-wetting while hospitalized. What should the nurse tell the parent?
(a) “Your child was too immature to be toilet trained. In a few months your child should be old enough.”
(b) “Children are afraid in the hospital and frequently wet their bed.”
(c) “It is very common for children to regress when they are in the hospital.”
(d) “This is normal. Your child probably received too much fluid the night before.”
Answer:
(c) “It is very common for children to regress when they are in the hospital.”
Explanation:
A child will regress to a behavior used in an earlier stage of development in order to cope with a perceived threatening situation. Readiness for toilet training should be based on neurological, physical, and psychological development, not the age of the child.
Children are afraid of hospitalization, but the bed-wetting is a compensatory mechanism done to regress to a previous stage of development that is more comfortable and secure for the child. Telling the mother that bed-wetting is related to fluid intake does not provide an adequate explanation for the underlying regression to an earlier stage of development.
Question 25.
The nurse is to obtain a urine specimen from a toddler hospitalized with a urinary tract infection. In what order should the nurse perform the following steps? Place in order from first to last. All options must be used.
(a) Cleanse the gential area.
(b) Apply gloves
(c) Offer fluids
(d) Apply collection bag.
Answer:
(c) Offer fluids
(b) Apply gloves
(a) Cleanse the gential area.
(d) Apply collection bag.
Explanation:
(c), (b), (a), (d) When obtaining a urine specimen from an infant, the nurse assists the client to drink fluids 30 to 60 minutes prior to specimen collection so the client voids as soon as possible after the col¬lection bag is applied. Next, the nurse applies gloves and then cleanses the genital area with sterile water to prevent contamination of the urine. Finally, the nurse applies the collection bag and then removes the bag when the specimen is obtained.
Question 26.
A parent brings in an 18-month-old to the clinic because the child “eats ashes, crayons, and paper.” Which information about the toddler should the nurse assess first?
(a) evidence of eruption of large teeth
(b) amount of attention from the parent
(c) any changes in the home environment
(d) intake of a soft, low-roughage diet
Answer:
(c) any changes in the home environment
Explanation:
A craving to eat nonfood substances is known as pica. Toddlers use oral gratification as a means to cope with anxiety. Therefore, the nurse should first assess whether the child is experiencing any change in the home environment that could cause anxiety.
Teething or the eruption of large teeth and the amount of attention from the mother are unlikely causes of pica. Nutritional deficiencies, especially iron deficiency, were once thought to cause pica, but research has not substantiated this theory. A soft, low-roughage diet is an unlikely cause.
Question 27.
When assessing a 2-year-old child at the clinic for a routine checkup, which skill should the nurse expect the child to be able to perform?
(a) riding a tricycle
(b) tying his or her shoelaces
(c) kicking a ball forward
(d) using blunt scissors
Answer:
(c) kicking a ball forward
Explanation:
A 2-year-old child usually can kick a ball forward. Riding a tricycle is characteristic of a 3-year-old child. Tying shoelaces is a behavior to be expected of a 5-year-old child. Using blunt scissors is characteristic of a 3-year-old child.
Question 28.
A 2-year-old child brought to the clinic by her parents is uncooperative when the nurse tries to look in her ears. What should the nurse try first?
(a) Ask another nurse to assist.
(b) Allow a parent to assist.
(c) Wait until the child calms down.
(d) Restrain the child’s arms.
Answer:
(b) Allow a parent to assist.
Explanation:
Parents can be asked to assist when their child becomes uncooperative during a procedure. Most commonly, the child’s difficulty in cooperating is caused by fear. In most situations, the child will feel more secure with a parent present.
Other methods, such as asking another nurse to assist or waiting until the child calms down, may be necessary, but obtaining a parent’s assistance is the recom-mended first action. Restraints should be used only as a last resort, after all other attempts have been made to encourage cooperation.
Question 29.
When observing the parent instilling prescribed ear drops prescribed twice a day for a 2-year-old, the nurse decides that the teaching about positioning of the pinna for instillation of the drops is effective when the parent pulls the toddler’s pinna in which direction?
(a) up and forward
(b) up and backward
(c) down and forward
(d) down and backward
Answer:
(d) down and backward
Explanation:
In a child younger than 3 years of age, the pinna is pulled back and down because the auditory canals are almost straight in children. In children over 3 through adulthood, the pinna is pulled up and backward because the auditory canals are directed inward, forward, and down.
Question 30.
The mother asks the nurse for advice about discipline for her 18-month-old. Which discipline strategy should the nurse suggest that the mother use?
(a) reprimand
(b) spanking
(c) reasoning
(d) time-out
Answer:
(d) time-out
Explanation:
Time-out is the most appropriate discipline for toddlers. It helps to remove them from the situation and allows them to regain control. Structuring interactions with 3-year-olds helps minimize unacceptable behavior. This approach involves setting clear and reasonable rules and calling attention to unacceptable behavior as soon as it occurs.
Reprimanding a young child can reinforce undesirable behavior over time because it provides attention. Physical punishment, such as spanking, has limited effectiveness and serious negative effects. Reasoning is more appropriate for older children, such as preschoolers and those older, especially when moral issues are involved. Unfortunately, reasoning combined with scolding often takes the form of shame or criticism, and children take such remarks seriously, believing that they are “bad.”
Question 31.
When assessing for pain in a toddler, which method would be the most appropriate?
(a) Ask the child about the pain.
(b) Observe the child for restlessness.
(c) Use a numeric rating pain scale.
(d) Assess for changes in vital signs.
Answer:
(b) Observe the child for restlessness.
Explanation:
Toddlers usually express pain through such behaviors as restlessness, facial grimaces, irritability, and crying. It is not particularly helpful to ask toddlers about pain. In most instances, they would be unable to understand or describe the nature and location of their pain because of their lack of verbal and cognitive skills. However, preschool and older children have the verbal and cognitive skills to be able to respond appropriately.
While the FACES pain scale can be used in young children, numeric rating pain scales are more appropriate for children who are of school age or older. Changes in vital signs do occur as a result of pain, but behavioral changes usually are noticed first.
Question 32.
Which amount of daily milk intake should the nurse include in the plan of care for a 15-month-old?
(a) 1/2 to 1 cup (125 to 250 mL)
(b) 2 to 3 cups (500 to 750 mL)
(c) 3 to 4 cups (750 to 1,000 mL)
(d) 4 to 5 cups (1,000 to 1,250 mL)
Answer:
(b) 2 to 3 cups (500 to 750 mL)
Explanation:
Toddlers around the age of 15 months need 2 to 3 cups (500 to 750 mL) of milk per day to supply necessary nutrients such as calcium. A daily intake of more than 3 cups (750 mL) of milk may interfere with the ingestion of other necessary nutrients.
Question 33.
The nurse teaches the parents of a 4-year-old diagnosed with iron deficiency anemia about potential side effects of taking an iron supplement. The nurse knows more teaching is required when the parents state a side effect of taking an iron supplement is which factor?
(a) teeth staining
(b) black stools
(c) metallic taste
(d) dark urine
Answer:
(d) dark urine
Explanation:
Dark urine is not a potential side effect of taking an iron supplement. Families need education about the possible side effects, including placing liquid iron behind the teeth to avoid teeth staining. Stools may become dark in color, even turn black, and some clients may notice a metallic taste. Nausea and vomiting are also common side effects of iron supplements.
Question 34.
The parent of a 4-year-old expresses concern that the child may be hyperactive. The parent describes the child as always in motion, constantly dropping and spilling things. Which action would be appropriate at this time?
(a) Determine whether there have been any changes at home.
(b) Explain that this is not unusual behavior.
(c) Explore the possibility that the child is being abused.
(d) Suggest that the child be seen by a pediatric neurologist.
Answer:
(b) Explain that this is not unusual behavior.
Explanation:
Preschool-age children have been described as powerhouses of gross motor activity who seem to have endless energy. A limitation of their motor ability is that in moving as quickly as they do, they are not always able to judge distances, nor are they able to estimate the amount of strength and balance needed for activities. As a result, they have frequent mishaps.
This level of activity typically is not associated with changes at home. However, if the behavior intensifies, a referral to a pediatric neurologist would be appropriate. Children who have been abused usually demonstrate withdrawn behaviors, not endless energy.
Question 35.
The parent of a preschooler reports that the child creates a scene every night at bedtime. What is the best course of action?
(a) Allow the child to stay up later one or two nights a week.
(b) Establish a set bedtime and follow a routine.
(c) Encourage active play before bedtime.
(d) Give the child a cookie if bedtime is pleasant.
Answer:
(b) Establish a set bedtime and follow a routine.
Explanation:
Bedtime is often a problem with preschoolers. Recommendations for reducing conflicts at bedtime include establishing a set bedtime, having a dependable routine, such as story reading, and conveying the expectation that the child will comply. Allowing the child to stay up late one or two nights interferes with establishing the needed bedtime rituals.
Excitement, such as active play, just before bedtime should be avoided because it stimulates the child, making it difficult for the child to calm down and prepare for sleep. Using food such as a cookie as a reward if bedtime is pleasant should be avoided because it places too much importance on food. Other rewards, such as stickers, could be used as an alternative.
Question 36.
The parents of a preschooler ask the nurse how to handle their child’s temper tantrums. Which technique should the nurse include in the teaching plan? Select all that apply.
(a) putting the child in “time-out”
(b) ignoring the child
(c) putting the child to bed
(d) spanking the child
(d) trying to reason with the child
Answer:
(b) ignoring the child
Explanation:
Some parents find that putting the child in time-out until control is regained is very effective. Others find that ignoring the behaviors works just as well with their child. Both suggestions are appropriate to include in the teaching plan.
Spanking the child is never an option. Attempting to reason with a child having a temper tantrum does not work because the child is out of control. A more appropriate time to discuss it with the child is when the child regains control.

Question 37.
After teaching a group of parents of preschoolers attending a well-child clinic about oral hygiene and tooth brushing, the nurse determines that the teaching has been successful when the parents state that children can begin to brush their teeth without help at which age?
(a) 3 years
(b) 5 years
(c) 7 years
(d) 9 years
Answer:
(c) 7 years
Explanation:
Children younger than 7 years of age do not have the manual dexterity needed for tooth brushing. Therefore, parents need to help with this task until that time.
Question 38.
After having a blood sample drawn, a 5-year- old child insists that the site be covered with a bandage. When the parent tries to remove the bandage before leaving the office, the child screams that all the blood will come out. The nurse encourages the parent to leave the bandage in place and tells the parent that the child’s reaction is based on which factor?
(a) fearing another procedure
(b) lacking understanding of body integrity
(c) expressing severe pain
(d) attempting to regain control
Answer:
(b) lacking understanding of body integrity
Explanation:
The preschool-age child does not have an accurate concept of skin integrity and can view medical and surgical treatments as hostile invasions that can destroy or damage the body. The child does not understand that exsanguinations will not occur from the injection site. Here, the child is verbalizing a fear consistent with the developmental age.
The child would most likely verbalize concerns of not wanting another procedure or exhibit other symptoms associated with pain if those were the underlying issues. If control was the main issue, the child would try to control more than just the bandage removal.
Question 39.
When developing the teaching plan about illness for the parent of a preschooler, which information should the nurse include about how a preschooler perceives illness?
(a) a necessary part of life
(b) a test of self-worth
(c) a punishment for wrongdoing
(d) the will of God
Answer:
(c) a punishment for wrongdoing
Explanation:
Preschool-age children may view illness as punishment for their fantasies. At this age, children do not have the cognitive ability to separate fantasies from reality and may expect to be punished for their “evil thoughts.” Viewing illness as a necessary part of life requires a higher level of cognition than preschoolers possess. This view is seen in children of middle-school age and older. Perceiving illness as a test of self-worth or as the will of God is more characteristic of adults.
Question 40.
The nurse takes the blood pressure of a preschool child. To determine if the blood pressure is normal, the nurse compares the results to percentiles for systolic and diastolic blood pressure. What other information does the nurse need to interpret the blood pressure? Select all that apply.
(a) age
(b) body mass index (BMI)
(c) gender
(d) height
(e) occipital frontal circumference (OFC)
(f) weight
Answer:
(a) age
(c) gender
(d) height
Explanation:
(a), (c), (d) Blood pressures percentiles for children are referenced by the age, sex, and height. Measurements at or above the 95th percentile are considered indicative of hypertension. Weight and elevated BMI contribute to hypertension but are not used to define it. The OFC is not routinely measured in children over 2 years of age and is not used to reference blood pressure readings.
Question 41.
A nurse is assessing the growth and development of a 10-year-old. What is the expected behavior of this child?
(a) enjoys physical demonstrations of affection
(b) is selfish and insensitive to the welfare of others
(c) is uncooperative in play and school
(d) has a strong sense of justice and fair play
Answer:
(d) has a strong sense of justice and fair play
Explanation:
School-age children are concerned about justice and fair play. They become upset when they think someone is not playing fair. Physical affection makes them embarrassed and uncomfortable. They are concerned about others and are cooperative in play and school.
Question 42.
The nurse conducts a wellness screening on a 9-year-old client Which finding most suggests that that the client has typical social development?
(a) thinks independently
(b) is able to organize and plan
(c) has a best friend
(d) enjoys active play
Answer:
(c) has a best friend
Explanation:
During the school-age years, children learn to socialize with children of the same age. The “best friend” stage, which occurs around 9 or 10 years of age, is important in providing a foundation for self-esteem and later relationships. Thinking independently, organizing, and planning are cogni-tive skills. Active play relates to motor skills.
Question 43.
A 10-year-old child proudly tells the nurse that brushing and flossing her teeth is her responsibility. How does the nurse interpret the statement?
(a) She is too young to be given this responsibility.
(b) She is most likely capable of this responsibility.
(c) She should have assumed this responsibility much sooner.
(d) She is probably just exaggerating the responsibility.
Answer:
(b) She is most likely capable of this responsibility.
Explanation:
Children are capable of mastering the skills required for flossing when they reach 9 years of age. At this age, many children are able to assume responsibility for personal hygiene. She is not too young to assume this responsibility, and she should not have been expected to assume this responsibility much earlier. It is not likely that she is exaggerating; this is an expected behavior at this age.
Question 44.
The parent tells the nurse that an 8-year-old child is continually telling jokes and riddles to the point of driving the other family members crazy.
The nurse should explain this behavior is a sign of which factor?
(a) inadequate parental attention
(b) mastery of language ambiguities
(c) inappropriate peer influence
(d) excessive television watching
Answer:
(b) mastery of language ambiguities
Explanation:
School-age children delight in riddles and jokes. Mastery of the ambiguities of language and of sentence structure allows the school-age child to manipulate words, and telling riddles and jokes is a way of practicing this skill. Children who suffer from inadequate attention from parents tend to demonstrate abnormal behavior. Peer influence is less important to school-age children, and while the child may learn the joke from a friend, he or she is telling the joke to master language. Watching television does not influence the extent of joke telling.
Question 45.
The parent asks the nurse about a 9-year- old child’s apparent need for between-meal snacks, especially after school. What information should the nurse include in the teaching plan?
(a) The child does not need to eat between-meal snacks.
(b) The child should eat the snacks the mother thinks are appropriate.
(c) The child should help with preparing his or her own snacks.
(d) The child will instinctively select nutritional snacks.
Answer:
(c) The child should help with preparing his or her own snacks.
Explanation:
Snacks are necessary for school-age children because of their high energy level. School- age children are in a stage of cognitive development in which they can learn to categorize or classify and can also learn cause and effect. By preparing their own snacks, children can learn the basics of nutrition (such as what carbohydrates are and what happens when they are eaten).
The mother and child should make the decision about appropriate foods together. School-age children learn to make decisions based on information, not instinct. Some knowledge of nutrition is needed to make appropriate choices.
Question 46.
A nurse compares a child’s height and weight with standard growth charts and finds the child to be in the 50th percentile for height and in the 25th percentile for weight. How does the nurse interpret the child’s growth pattern?
(a) typical height and weight D
(b) overweight for height
(c) underweight for height
(d) abnormal in height
Answer:
(a) typical height and weight D
Explanation:
The values of height and weight percentiles are usually similar for an individual child. Measurements between the 5th and 95th percentiles are considered normal. Marked discrepancies identify overweight or underweight children.
Question 47.
The nurse is assessing an 11-year-old female, using the Tanner staging of puberty. Which finding indicates preadolescent development of the breasts?
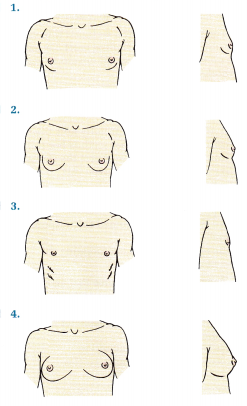
Answer:
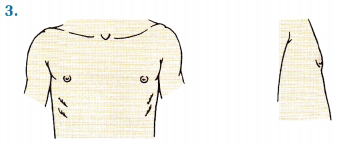
Explanation:
This figure indicates elevation of the papilla, without breast buds, considered stage 1 and typical of a preadolescent. Figure 1 shows stage 2, breast bud enlargement; there is elevation of the breast and the diameter of the areola has increased. Figure 2 shows stage 3, enlargement of the breast and areola. Figure 4 shows stage 4, in which there is projection of areola and papilla to form a secondary mound above the level of the breast.
Question 48.
The parents of a 12-year-old girl ask why their daughter, who is not sexually active, should receive the human papillomavirus (HPV) vaccine. What should the nurse should tell the parents?
(a) “The vaccine is most effective against cervical cancer if given before becoming sexually active.”
(b) “Parents are never sure when their child might become sexually active.”
(c) “HPV is most common is teens and women in their late 20s.”
(d) “If your daughter is sexually assaulted, she may be exposed to HPV.”
Answer:
(a) “The vaccine is most effective against cervical cancer if given before becoming sexually active.”
Explanation:
Vaccines are preventative in nature and ideally given before exposure. Focusing on the benefits of cancer prevention is most appropriate, as opposed to discussing with parents the potential that their child may become sexually active without their knowledge. It is true HPV is most common in adolescents and women in their late 20s, but parents still may not perceive that their child is at risk. Discussing the possibility of exposure through assault raises fears and does not focus on prevention.
Question 49.
A 16-year-old client who has been confined to a wheelchair since early childhood has lately been acting rebellious and rude. Her parents ask the nurse, “Are all adolescents like this?” The nurse should respond with which statement?
(a) “Yes, although your daughter’s behaviors are more like those of an adolescent boy.”
(b) “No. Your daughter must need some help in dealing with her feelings.”
(c) “Your daughter’s behavior seems to be typical adolescent behavior. Let us talk more about it.”
(d) “Your daughter’s behavior results from feelings about her disability: ignore it.”
Answer:
(c) “Your daughter’s behavior seems to be typical adolescent behavior. Let us talk more about it.”
Explanation:
It is normal behavior for adolescents to assert independence and begin to separate from their parents; the behavior is not changed by their daughter’s disability, nor is it unique to a girl. The nurse offers reassurance to the parents and then opens the conversation for additional discussion.
Question 50.
The parents of an adolescent boy are concerned their son seems to need 9 hours of sleep a night. What should the nurse should tell the parents?
(a) “As long as he seems otherwise well, this sounds like a typical teenager.”
(b) “Adolescents need only 8 hours of sleep a night; anything over this is excessive.”
(c) “Your son is probably engaged in too many activities and is wearing himself out.”
(d) “The side effect of many drugs is sleepiness.”
Answer:
(a) “As long as he seems otherwise well, this sounds like a typical teenager.”
Explanation:
Many teenagers feel fatigued from a com¬bination of fast-food diets, many activities, and a rapid growth spurt; this is normal behavior, and the nurse should explain possible reasons for the sleep pattern. Adolescents typically need 8.5 to 9.5 hours of sleep. There are no data to suggest that activities are tiring this teenager. It is not appropriate to sug-gest the child is taking drugs based on the question the parents are asking the nurse.
Question 51.
An adolescent tells the nurse that she would like to use tampons during her period. What should the nurse do first?
(a) Assess her usual menstrual flow pattern.
(b) Determine whether she is sexually active.
(c) Provide information about preventing toxic shock syndrome.
(d) Refer her to a specialist in adolescent gynecology.
Answer:
(c) Provide information about preventing toxic shock syndrome.
Explanation:
The nurse should provide the adolescent with information about toxic shock syndrome because of the identified relationship between tampon use and the syndrome’s development. Additionally, about 95% of cases of toxic shock syndrome occur during menses. Most adolescent females can use tampons safely if they change them frequently. Using tampons is not related to menstrual flow or sexual activity. There is no need to refer the girl to a gynecologist; a nurse can provide health teaching about tampon use.
Question 52.
Several high-school seniors are referred to the nurse because of suspected alcohol misuse. When the nurse assesses the situation, what would be most important to determine?
(a) what they know about the legal implications of drinking
(b) the type of alcohol they usually drink
(c) the reasons they choose to use alcohol
(d) when and with whom they use alcohol
Answer:
(c) the reasons they choose to use alcohol
Explanation:
Information about why adolescents choose to use alcohol or other drugs can be used to determine whether they are becoming responsible users or problem users. The senior students likely know the legal implications of drinking, and the nurse will establish a more effective relationship with the students by understanding motivations for use. The type of alcohol and when and with whom they are using it are not the first data to obtain when assessing the situation.
Question 53.
Which action initiated by the parents of an 8-month-old indicates they need further teaching about preventing childhood accidents?
(a) placing a fire screen in front of the fireplace
(b) placing a car seat in a front-seat, front-facing position
(c) inspecting toys for loose parts
(d) placing toxic substances out of reach or in a locked cabinet
Answer:
(b) placing a car seat in a front-seat, front-facing position
Explanation:
It is recommended that children up to 2 years of age ride in a rear-facing car seat. The middle of the back seat is considered the safest area of the car. Burns are a major cause of childhood accidents, and using fire screens in front of fireplaces can help prevent children from getting too close to a fire in a fireplace. Toys that contain loose parts or plastic eyes that can be swallowed or aspirated by small children should be avoided.
Parents should inspect all toys for these parts before giving one to a child. Poisonings are most commonly caused by improper storage of a toxic substance. Keeping toxic substances in a childproof container in a locked cabinet and continually observing the child’s activities can prevent most poisonings.
Question 54.
A nurse is assessing the growth and development of a 14-year-old boy. He reports that his 13-year-old sister is 2 inches (5 cm) taller than he is. What information should the nurse provide about growth spurts in adolescent boys compared to growth spurts in adolescent girls?
(a) They occur about at the same time.
(b) They occur about 2 years earlier.
(c) They occur about 2 years later.
(d) They occur about 1 year earlier.
Answer:
(c) They occur about 2 years later.
Explanation:
Adolescent boys lag about 2 years behind adolescent girls in growth. Most girls are 1 to 2 inches (3 to 5 cm) taller than boys at the beginning of adolescence but tend to stop growing approximately 2 to 3 years after menarche with the closure of the epiphyseal lines of the long bones.
Question 55.
Parents of a 15-year-old state that their child is moody and rude. What should the nurse should advise the parents to do?
(a) Restrict their child’s activities.
(b) Discuss their feelings with their child.
(c) Obtain family counseling.
(d) Talk to other parents of adolescents.
Answer:
(b) Discuss their feelings with their child.
Explanation:
Parents need to discuss with their adolescent how they perceive his or her behavior and how they feel about it. Moodiness is characteristic of adolescents. The adolescent may have a reason for or not be aware of his behavior. Restricting the adolescent’s activities will not change his or her mood or the way he or she responds to others.
It may increase his or her unacceptable responses. Counseling may not be needed at this time if the parents are open to communicating and listening to the adolescent. Talking to other parents may be of some help, but what is helpful to others may not be helpful to their child.
Question 56.
Which statement by a parent whose child was just diagnosed with pediculosis capitis (head lice) demonstrates an understanding of the safety and efficacy of the common medications used to treat the infection?
(a) “I am going to request a prescription for lindane since it works the best.”
(b) “After I shampoo, I will use the special comb to get the nits out.”
(c) “Most over the counter lice treatments are 100% effective at killing all the eggs.”
(d) “I can give a second treatment the next day if any lice remain.”
Answer:
(b) “After I shampoo, I will use the special comb to get the nits out.”
Explanation:
The makers of many of the pediculicides recommend manual removal of the nits following treatment with an extra-fine-tooth comb. None of the pediculicides are 100% effective in killing all the eggs. The FDA has issued a warning regarding the use of lindane because of the potential for neurotoxicity. Clients are treated with lindane only when the benefits outweigh the risks. Lice treat¬ments may be repeated in 7 to 10 days; the next day is too soon.
Question 57.
A parent asks, “Can I get head lice too?” The nurse indicates that adults can also be infested with head lice but that pediculosis is more com¬mon among school-age children, primarily for what reason?
(a) An immunity to pediculosis usually is established by adulthood.
(b) School-age children tend to be more neglect ful of frequent handwashing.
(c) Pediculosis usually is spread by close contact with infested children.
(d) The skin of adults is more capable of resisting the invasion of lice.
Answer:
(c) Pediculosis usually is spread by close contact with infested children.
Explanation:
Lice are spread by close personal contact and by contact with infested clothing, bed and bathroom linens, and combs and brushes. Lice are more common in school-age children than in adults because of the close contact in school or at sleepovers and the common practice of sharing possessions. Lice are not commonly spread by hand contact. There is no immunity conferred by having head lice. Adults can have head lice, particularly if they come in close contact with their children’s infested clothing or linens.
Question 58.
After teaching the parents about the cause of ringworm of the scalp (tinea capitis), which state¬ment by the parent indicates successful teaching?
(a) “It results from overexposure to the sun.”
(b) “It is caused by infestation with a mite.”
(c) “It is a fungal infection of the scalp.”
(d) “It is an allergic reaction.”
Answer:
(c) “It is a fungal infection of the scalp.”
Explanation:
Ringworm of the scalp is caused by a fungus of the dermatophyte group of the species. Overexposure to the sun would result in sunburn. Mites, such as chiggers or ticks, produce bites on the skin, resulting in inflammation. An allergic reaction commonly is manifested by hives, rash, or anaphylaxis.
Question 59.
Griseofulvin was prescribed to treat a child’s ringworm of the scalp. The nurse instructs the parents to use the medication for several weeks for which reason?
(a) A sensitivity to the drug is less likely if it is used over a period of time.
(b) Fewer side effects occur as the body slowly adjusts to a new substance over time.
(c) Fewer allergic reactions occur if the drug is maintained at the same level long-term.
(d) The growth of the causative organism into new cells is prevented with long-term use.
Answer:
(d) The growth of the causative organism into new cells is prevented with long-term use.
Explanation:
Griseofulvin is an antifungal agent that acts by binding to the keratin that is deposited in the skin, hair, and nails as they grow. This keratin is then resistant to the fungus. But as the keratin is normally shed, the fungus enters new, uninfected cells unless drug therapy continues. Long-term administration of griseofulvin does not prevent sensitivity or allergic reactions. As the body adjusts to a new substance over time, side effects are variable and do not necessarily decrease.
Question 60.
A parent asks the nurse, “How did my children get pinworms?” The nurse explains that pin-worms are most commonly spread by which route?
(a) food
(b) hands
(c) animals
(d) toilet seats
Answer:
(b) hands
Explanation:
The adult pinworm emerges from the rectum and colon at night onto the perianal area to lay its eggs. Itching and scratching introduces the eggs to the hands, from where they can easily reinfect the child or infect others. Nightclothes and bed linens can be sources of infection. The eggs can also be transmitted by dust in the home. Although transmis-sion through contaminated food and water supplies is possible, it is rare. Contaminated animals can spread histoplasmosis and salmonella. The spread of infections by toilet seats has not been supported by research.
Question 61.
A parent asks the nurse how to care for a child with chickenpox. What should the nurse include in the plan of care? Select all that apply.
(a) Use over-the-counter aspirin for fever.
(b) Encourage oatmeal baths.
(c) Keep fingernails short.
(d) Avoid overheating.
Answer:
(b) Encourage oatmeal baths.
(c) Keep fingernails short.
(d) Avoid overheating.
Explanation:
(b), (c), (d), The care of a child with chick- enpox focuses keeping the child comfortable and preventing infection in the lesions. Oatmeal baths may ease severe itching. Keeping fingernails short reduces trauma from scratching and helps prevent skin infections. Overheating can make itching worse. Children may return to school once all lesions have crusted over. The use of aspirin in children with chickenpox is contraindicated because it has been linked to Reye syndrome.
Question 62.
A mother states that a health care provider (HCP) described her daughter as having 20/60 vision, and she asks the nurse what this means. The nurse responds based on the interpretation that the child is experiencing which condition?
(a) a loss of approximately one-third of her visual acuity
(b) ability to see at 60 feet what she should see at 20 feet
(c) ability to see at 20 feet what she should see at 60 feet
(d) visual acuity three times better than average
Answer:
(c) ability to see at 20 feet what she should see at 60 feet
Explanation:
A child with 20/60 vision sees at 20 feet what those with 20/20 vision see at 60 feet. A visual acuity of 20/200 is considered to be the boundary of legal blindness.
Question 63.
The nurse discusses the eating habits of school-age children with their parents, explaining that these habits are most influenced by which factor?
(a) food preferences of their peers
(b) smell and appearance of foods offered
(c) examples provided by parents at mealtimes
(d) parental encouragement to eat nutritious foods
Answer:
(c) examples provided by parents at mealtimes
Explanation:
Although children may be influenced by their peers and smell and appearance of foods may be important, children are most likely to be influenced by the example and atmosphere provided by their parents. Coaxing and badgering a child to eat most likely will aggravate poor eating habits.
Question 64.
When discussing the onset of adolescence with parents, the nurse explains that it occurs at what time?
(a) same age for both boys and girls
(b) 1 to 2 years earlier in boys than in girls
(c) 1 to 2 years earlier in girls than in boys
(d) 3 to 4 years later in boys than in girls
Answer:
(c) 1 to 2 years earlier in girls than in boys
Explanation:
Girls experience the onset of adolescence about 1 to 2 years earlier than do boys. The reason for this is not understood.
Question 65.
A parent has heard that several adolescents have been diagnosed with mononucleosis. The par¬ent asks the nurse what precautions should be taken to prevent this from occurring in her teen. What instructions should the nurse give the parent?
(a) Tell the teen to avoid sharing food and drinks.
(b) Sterilize the teen’s eating utensils before they are reused.
(c) Wash the teen’s linens separately in hot, soapy water.
(d) Have the teen vaccinated for mononucleosis.
Answer:
(a) Tell the teen to avoid sharing food and drinks.
Explanation:
The cause of infectious mononucleosis is thought to be the Epstein-Barr virus. The virus is believed to be spread only by direct intimate contact. No precautionary measures for the general public are recommended to prevent mononucleosis. However, it is recommended that sharing food items and kissing be avoided with persons known to have mononucleosis. There currently is no vaccine for the disease.
Question 66.
A parent asks the nurse how he would know if his child had developed mononucleosis. The nurse explains that in addition to fatigue, which symptom would be most common?
(a) liver tenderness
(b) enlarged lymph glands
(c) persistent nonproductive cough
(d) a blush-like generalized skin rash
Answer:
(b) enlarged lymph glands
Explanation:
Mononucleosis usually has an insidious onset, with fatigue and the inability to maintain usual activity levels as the most common symptoms. The lymph nodes are typically enlarged, and the spleen also may be enlarged. Fever and a sore throat often accompany mononucleosis. A persistent non¬productive cough can follow an upper respiratory tract infection. A blush-like generalized skin rash is more characteristic of rubella.
Question 67.
A 17-year-old high school senior calls the clinic because she thinks she might have gonorrhea. She wants to be seen but wants assurances that no one will know. Which is the most appropriate response by the nurse?
(a) “Because you are underage, we will need your parent’s consent to treat you.”
(b) “We can treat you without your parents’ consent, but they have the right to review your medical record.”
(c) “We can see you without your parents’ consent but have to report any positive results to the public health department.”
(d) “We can see you, treat any infections, and will not share your results with anyone.”
Answer:
(c) “We can see you without your parents’ consent but have to report any positive results to the public health department.”
Explanation:
While some areas may specify a minimum age for treatment (usually 12 to 14 years), generally adolescents have the right to seek treatment for sexually transmitted infections without their parents’ permission. These medical records 03 are not shared with parents without the client’s permission. However, adolescents must be made aware that certain infections, including gonorrhea, must be reported by law to public health agencies. Partner notification will also take place, but methods vary.
Question 68.
A parent brings a 5-year-old child to a weekend vaccination clinic to prepare for school entry. The nurse notes that the child has not had any vaccinations since 4 months of age. What is the best way for the nurse to determine how to catch up the child’s vaccinations?
(a) Contact the child’s health care provider (HCP) during office hours.
(b) Review nationally published immunization guidelines.
(c) Read each vaccine’s manufacturer’s insert.
(d) Ask a local pharmacist on duty.
Answer:
(b) Review nationally published immunization guidelines.
Explanation:
National advisory committees on immunization practices review vaccination evidence and update recommendations yearly. Current vaccination catch-up schedules are readily available on their websites. The lack of vaccinations is a strong indicator that the child probably does not have an HCP OJ. Even if the client had a provider, however, that person might be difficult to reach on a weekend during the time frame of a vaccination clinic.
If consulted, the pharmacist would most likely have to review the latest guidelines that are equally available to the nurse. Reading each of manufacturer’s inserts for multiple vaccines would be time consuming, and synthesis of the information could possibly lead to errors.
Question 69.
A 13-month-old has a febrile seizure 3 weeks after the administration of the chickenpox vaccine. What is the best action for the nurse to take?
(a) Recognize that the events are unrelated.
(b) Report the event through an immunization surveillance system.
(c) Explain to the parents that this is a rare but acceptable risk.
(d) Refer the child to a neurologist.
Answer:
(b) Report the event through an immunization surveillance system.
Explanation:
Any unusual event that occurs after the administration of a vaccination should be reported through an immunization surveillance system, especially if it happens with 1 month of the vaccine administration. In the United States, it is the Vaccine Adverse Event Reporting System (VAERS). In Canada, it is Canadian Adverse Events Following Immunization Surveillance System (CAEFISS).
A high fever, with or without a seizure, that occurs within 6 weeks of vaccination may have been caused by the vaccine. A febrile seizure is considered a moderate reaction that warrants caution with future chickenpox vaccination. A single febrile seizure does not require referral to a neurologist.
Question 70.
The nurse is invited to attend a meeting with several parents who express frustration with the amount of time their adolescents spend in front of the mirror and the length of time it takes them to get dressed. What does the nurse explain that this behavior indicates?
(a) an abnormal narcissism
(b) a method of procrastination
(c) a way of testing the parents’ limit-setting
(d) a result of developing self-concept
Answer:
(d) a result of developing self-concept
Explanation:
An adolescent’s body is undergoing rapid changes. Adolescence is a time of integrating these rapidly occurring physical changes into the self-concept to achieve the developmental task of a positive self-identity. Thus, most adolescents spend much time worrying about their personal appearance. This behavior is not abnormal narcissism, a method of procrastination, or a way of testing the parents’ limits.
Question 71.
A child who is 18 months of age is brought to the emergency department by her babysitter. The babysitter states, “She fell from the sofa an hour ago and has not been herself since.” On questioning, the babysitter appears to be unsure of time and other facts about the incident. Which question below would be most effective in obtaining more information about the child’s injuries?
(a) “Why did you leave the child alone on the couch?”
(b) “Have you taken a course in safe babysitting?”
(c) “Tell me what was happening before she fell.”
(d) “Where are her parents? Do they know this happened?”
Answer:
(c) “Tell me what was happening before she fell.”
Explanation:
An open-ended question is apt to supply more information when a person is under stress and easily susceptible to being influenced by the question. The other questions are direct and only require an answer with limited information.
Also Read: