NCLEX RN Practice Questions provide an opportunity to reinforce knowledge of nursing fundamentals, including anatomy and physiology.
NCLEX Child with Neurologic Health Problems Questions
Child with Neurologic Health Problems NCLEX Practice Questions
Question 1.
Parents bring a 10-month-old boy with myelo-meningocele and hydrocephalus with a ventriculo-peritoneal shunt to the emergency department. His symptoms include vomiting, poor feeding, lethargy, and irritability. What interventions by the nurse are most appropriate? Select all that apply.
(a) Weigh the child.
(b) Listen to bowel sounds.
(c) Palpate the posterior fontanelle.
(d) Obtain vital signs.
(e) Assess pitch and quality of the child’s cry.
Answer:
(a) Weigh the child.
(b) Listen to bowel sounds.
(d) Obtain vital signs.
(e) Assess pitch and quality of the child’s cry.
Explanation:
(a), (b), (d), (e) Common shunt complications are obstruction, infection, and disconnection of the tubing. The signs presented by the child indicate increased intracranial pressure from a shunt malfunction, which could be caused by an infection, such as peritonitis or meningitis. By listening to bowel sounds, the nurse will note if peritonitis might be a possibility. Intracranial pressure manifests as a bulging or taut anterior fontanel, but the posterior fontanel is typically closed.
Obtaining vital signs would assess for signs of infection, such as elevated temperature or, possibly, Cushing’s triad (elevated blood pressure, slow pulse, and depressed respirations). A high-pitched cry is a sign of increased intracranial pressure. Weighing the child, while it would not help identify the cause of the problem, would help determine the severity of the dehydration from vomiting.
Question 2.
When positioning a neonate with an unrepaired myelomeningocele, which position is most appropriate?
(a) supine with the hips at 90-degree flexion
(b) right side-lying position with the knees flexed
(c) prone with hips in abduction
(d) supine in semi-Fowler’s position with chest and abdomen elevated
Answer:
(c) prone with hips in abduction
Explanation:
Before surgery, the infant is kept flat in the prone position to decrease tension on the sac. This allows for optimal positioning of the hips, knees, and feet because orthopedic problems are common. The supine position is unacceptable because it causes pressure on the defect. Flexing the knees when side-lying will increase tension on the sac, as will placing the infant in semi-Fowler’s position, even though the chest and abdomen are elevated.
Question 3.
The nurse is teaching the parents of a child with myelomeningocele how to prevent urinary tract infections. What information should be included in the care plan for this child? Select all that apply.
(a) Provide meticulous skin care.
(b) Use Crede’s maneuver to empty the bladder.
(c) Encourage frequent emptying of the bladder.
(d) Assure adequate fluid intake.
(e) Use tight-fitting diapers around the meatus.
Answer:
(b) Use Crede’s maneuver to empty the bladder.
(c) Encourage frequent emptying of the bladder.
(d) Assure adequate fluid intake.
Explanation:
(b), (c), (d) Prevention of urinary tract infections includes adequate fluid intake, urine acidification, and frequent emptying of the bladder, with the use of Crede’s maneuver if needed. While the nurse should keep the skin clean and dry, this will not prevent urinary tract infections. Keeping urine close to the meatus with a tight-fitting diaper would increase the risk for infection.
Question 4.
Which finding in an infant with a myelomeningocele should be reported to the health care provider (HCP) as a sign of increased intracranial pressure?
(a) minimal lower extremity movement
(b) a high-pitched cry
(c) overflow voiding only
(d) a fontanelle that bulges with crying
Answer:
(b) a high-pitched cry
Explanation:
A Chiari malformation obstructs the flow of cerebral spinal fluid resulting in hydrocephalus. This is a common problem in infants with myelomeningocele and will require surgical intervention with a shunt. A high-pitched cry is one sign of increased intracranial pressure that may indicate the presence of a Chiari malformation and requires further evaluation.
Minimal movement of the lower extremities is an expected finding associated with spinal cord damage. Overflow voiding comes from a neurogenic bladder, not increased intracranial pressure. It is normal for the fontanelle to bulge with crying.
Question 5.
When developing the plan of care for an infant diagnosed with myelomeningocele and the parents who have just been informed of the infant’s diagnosis, the nurse should include which action as the priority when the parents visit the infant for the first time?
(a) Emphasize the infant’s normal and positive features.
(b) Encourage the parents to discuss their fears and concerns.
(c) Reinforce the health care provider’s (HCP’s) explanation of the defect.
(d) Have the parents feed their infant.
Answer:
(a) Emphasize the infant’s normal and positive features.
Explanation:
The parents should see the neonate as soon as possible because the longer they must wait to see the neonate, the more anxiety they will feel. Because the parents are acutely aware of the deficit, the nurse should emphasize the neonate’s normal and positive features during the visit. All parents, but especially those with a child who has a disability or defect, need to hear positive comments and comments that reflect how the infant is normal. Although the parents need to discuss their fears and concerns, the priority on the first visit is to emphasize the neonate’s normal and positive features.
Reinforcing the HCP’s Q explanation of the defect may be necessary later. Reinforcing the explanation at this initial visit emphasizes the defect, not the child. The parents should spend time with or care for the neonate after birth because parent-infant contact is necessary for attachment. The parents cannot feed the neonate before the defect is repaired because the repair typically occurs within 24 hours. The infant will be prone in an Isolette or warmed and watched closely. However, the parents can fondle and stroke the neonate.
Question 6.
The mother of an infant with myelomeningocele asks if her baby is likely to have any other defects. The nurse responds based on the understanding that myelomeningocele is commonly associated with which disorder?
(a) excessive cerebrospinal fluid within the cranial cavity
(b) abnormally small head
(c) congenital absence of the cranial vault
(d) overriding of the cranial sutures
Answer:
(a) excessive cerebrospinal fluid within the cranial cavity
Explanation:
Excessive cerebrospinal fluid in the cranial cavity, called hydrocephalus, is the most common anomaly associated with myelomeningocele. Microcephaly, an abnormally small head, is associated with maternal exposure to rubella or cyto-megalovirus. Anencephaly, a congenital absence of the cranial vault, is a different type of neural tube defect. Overriding of the sutures, possibly a normal finding after a vaginal birth, is not associated with myelomeningocele.
Question 7.
The parents of an infant with myelomeningocele ask the nurse about their child’s future mental ability. What is the nurse’s best response?
(a) “About one-third have an intellectual disability, but it is too early to tell about your child.”
(b) “Intellectual disabilities occur in about two-thirds of these children, and you will know soon if this will occur.”
(c) “Your child will probably be of normal intelligence since he demonstrates signs of it now.”
(d) “You will need to talk with the health care provider (HCP) about that, but you can ask later.”
Answer:
(a) “About one-third have an intellectual disability, but it is too early to tell about your child.”
Explanation:
Approximately one-third of infants diagnosed with myelomeningocele have an intellectual disability, but the degree of disability is variable, and it is difficult to predict intellectual functioning in neonates. The parents are asking for an answer now and should not be told to talk with the HCP ZJ later.
Question 8.
After placing an infant with myelomeningocele in an Isolette shortly after birth, the nurse should use which indicator as the best way to determine the effectiveness of this intervention?
(a) The partial pressure of arterial oxygen remains between 94 and 100 mm Hg.
(b) The axillary temperature remains between 97°F and 98°F (36.1°C and 36.7°C).
(c) The bilirubin level remains stable.
(d) Weight increases by about 1 oz (30 g) per day.
Answer:
(b) The axillary temperature remains between 97°F and 98°F (36.1°C and 36.7°C).
Explanation:
The nurse places the neonate with myelomeningocele in an Isolette shortly after birth to help to maintain the infant’s temperature. Because of the defect, the neonate cannot be bundled in blankets. Therefore, it may be difficult to prevent cold stress.
The Isolette can be maintained at higher than room temperature, helping to maintain the temperature of a neonate who cannot be dressed or bundled. Body temperature readings, not arterial oxygen levels, are the best indicator. Typically, an infant loses 5% to 10% of body weight before beginning to regain the weight.
Question 9.
After surgical repair of a myelomeningocele, which position should the nurse use to prevent musculoskeletal deformity in the infant?
(a) Place the feet in flexion.
(b) Allow the hips to be abducted.
(c) Maintain knees in the neutral position.
(d) Place the legs in adduction.
Answer:
(b) Allow the hips to be abducted.
Explanation:
Because of the potential for hip dislocation, the neonate’s legs should be slightly abducted, hips maintained in slight to moderate abduction, and feet maintained in a neutral position. The infant’s knees are flexed to help maintain the hips in abduction.
Question 10.
When developing the discharge plan for the parents of an infant who has undergone a myelomeningocele repair, what information is most important for the nurse to include?
(a) a list of available hospital services
(b) schedule for daily home health care
(c) chaplain referral for psychological support
(d) daily care required by the infant
Answer:
(d) daily care required by the infant
Explanation:
The most important aspect of the discharge plan is to ensure that the parents understand what the daily care of their infant involves and to provide teaching related to carrying out this daily care. In addition to the routine care required by the infant, care also may include physical therapy to the lower extremities.
Providing a list of available hospital services may be helpful to the parents, but it is not the most important aspect to include in the discharge plan. Usually, home health care is not needed because the parents are able to care for their child. A referral for counseling is initiated whenever the need arises, not just at discharge.
Question 11.
Which statement by the parent of an infant with a repaired upper lumbar myelomeningocele indicates that the parent understands the nurse’s teaching at the time of discharge?
(a) "I can apply a heating pad to his lower back. ”
(b) “I will be sure to keep him away from other children.”
(c) “I will call the health care provider (HCP) if his urine has a funny smell.”
(d) “I will prop him on pillows to keep him from rolling over.”
Answer:
(c) “I will call the health care provider (HCP) if his urine has a funny smell.”
Explanation:
Children with a myelomeningocele are prone to urinary tract infections (UTIs), and foulsmelling urine is one symptom of a UTI. Because of the level of defect, the child may be insensitive to pressure or heat. Using a heating pad may lead to thermal injury because the child may not be able to sense if the pad is too hot. Keeping the child away from other children is unnecessary and can retard social development. Using pillows as props increases the risk of sudden infant death syndrome.
Question 12.
A preschooler with a history of repaired lumbar myelomeningocele is in the emergency department with wheezing and skin rash. Which questions should the nurse ask the parent first?
(a) “Is your child taking any medications?”
(b) “Who brought your child to the emergency department?”
(c) “Is your child allergic to bananas or any other food?”
(d) “What are you doing to treat your child’s skin rash?”
Answer:
(c) “Is your child allergic to bananas or any other food?”
Explanation:
Children with myelomeningocele are at high risk for development of latex allergy because of repeated exposure to latex products during surgery and bladder catheterizations. Cross-reactions to food items such as bananas, kiwi, chestnuts, and avocados also occur. These allergic reactions vary in severity ranging from mild (such as sneezing) to severe anaphylaxis.
While the child could have allergies to medications that caused the wheezing, latex and food allergies are more common. Asking about the skin rash is not a priority when a child is wheezing. Who brought the child to the emergency department is irrelevant at this time.
Question 13.
Before placement of a ventriculoperitoneal shunt for hydrocephalus, an infant is irritable, lethargic, and difficult to feed. To maintain the infant’s nutritional status, which action would be most appropriate?
(a) Feed the infant just before doing any procedures.
(b) Give the infant small, frequent feedings.
(c) Feed the infant in a horizontal position.
(d) Give large, less frequent feedings.
Answer:
(b) Give the infant small, frequent feedings.
Explanation:
An infant with hydrocephalus is difficult to feed because of poor sucking, lethargy, and vomiting, which are associated with increased intracranial pressure. Small, frequent feedings given at times when the infant is relaxed and calm are tolerated best. Feeding an infant before any procedure is inappropriate because the stress of the procedure may lead to vomiting.
Ideally, the infant should be held in a slightly vertical position when feeding to prevent backflow of formula into the eustachian tubes and subsequent development of ear infections. Giving large, less frequent feedings allows for rest but typically results in more vomiting.
Question 14.
Which clinical manifestation would lead the nurse to suspect an infant has hydrocephaly? Select all that apply.
(a) depressed fontanelle
(b) headache
(c) vomiting
(d) low-pitched cry
(e) irritability
(f) pupillary changes
Answer:
(c) vomiting
(d) low-pitched cry
(e) irritability
Explanation:
(c), (d), (e) Hydrocephaly is a block in the flow of cerebral spinal fluid. Hydrocephaly results in increased intracranial pressure (ICP). Vomiting, irritability, bulging fontanelle, and pupillary changes are all signs of increased intracranial pressure in an infant. A depressed fontanelle could be an indication of dehydration, not increased intracranial pressure.
A headache may be present in an infant with increased ICP; however, the infant has no way of communicating this to the nurse or parent. A headache is an indication of increased ICP in I a verbal child. A high-pitched cry is indicative of I infants with increased intracranial pressure.
Question 15.
The nurse assesses a 2-month old infant with hydrocephalus with a ventriculoperitoneal shunt. The nurse obtains the infant’s vital signs. In order to obtain the most significant information about the child’s status, which assessment should the nurse make next?
(a) status of posterior fontanelle
(b) pupillary reaction to light
(c) occipital frontal head circumference
(d) presence of the primitive reflex
Answer:
(c) occipital frontal head circumference
Explanation:
Measuring the occipital frontal head circumference over time is the most obvious way to monitor if hydrocephalus is worsening or improving 1 in an infant. The infant exhibits sunsetting of the eyes, which is a sign of hydrocephalus. Pupillary reactions may be decreased or unequal, but these measurements do not give as much information about changes in the infant’s status.
The posterior I fontanelle usually closes by 2 months in a typically developing infant. Finding the posterior fontanelle 1 still open in an infant with hydrocephalus would not be unexpected and would not necessarily be an indicator of the severity of the disorder. A finding of primitive reflexes in a 3-month-old infant would be an expected finding.
Question 16.
The nurse is providing postoperative care for an infant who had a ventriculoperitoneal shunt placed to correct hydrocephalus. Which clinical finding warrants immediate intervention?
(a) abdominal distention
(b) lethargy
(c) facial edema
(d) headache
Answer:
(a) abdominal distention
Explanation:
Abdominal distension in a pediatric client with a ventriculoperitoneal shunt can be an I indication of peritonitis and requires intervention. Lethargy may be present for several days following surgery for a ventriculoperitoneal shunt. Facial and eye edema is common during the postoperative period and can be reduced by utilizing a cold compress to the eyes. Infants commonly have pain in the postoperative period that should be treated with analgesics; however, infants cannot convey that they specifically have a headache.
Question 17.
Which action should the nurse take when providing postoperative nursing care to a child after insertion of a ventriculoperitoneal shunt?
(a) Administer narcotics for pain control.
(b) Check the urine for glucose and protein.
(c) Monitor for increased temperature.
(d) Test cerebrospinal fluid leakage for protein.
Answer:
(c) Monitor for increased temperature.
Explanation:
Monitoring the temperature allows the nurse to assess for infection, the most common and the most hazardous postoperative complication after ventriculoperitoneal shunt placement. Typically, pain after insertion of a ventriculoperitoneal shunt is mild, requiring the use of mild analgesics.
Usually, narcotics are not administered because they alter the level of consciousness, making assessment of cerebral function difficult. Neither proteinuria i nor glycosuria is associated with shunt placement. Cerebrospinal fluid leakage commonly occurs with head injury. It is not usually associated with shunt placement.
Question 18.
A nurse evaluates discharge teaching as successful when the parents of a school-age child with a ventriculoperitoneal shunt insertion identify which sign as signaling a blocked shunt?
(a) decreased urine output with stable intake
(b) tense fontanelle and increased head circumference
(c) elevated temperature and reddened incisional site
(d) irritability and increasing difficulty with eating
Answer:
(d) irritability and increasing difficulty with eating
Explanation:
In a school-age child, irritability, lethargy, vomiting, difficulty with eating, and decreased level of consciousness are signs of increased intracranial pressure caused by a blocked shunt. Decreased urine output with stable fluid intake indicates fluid loss from a source other than the kidneys. A tense fontanelle and increased head circumference would be signs of a blocked shunt in an infant. Elevated temperature and redness around incisions might suggest an infection.
Question 19.
The parent of an adolescent girl with Down syndrome tells the nurse that her daughter recently stated that she has a boyfriend. The parent is concerned that her daughter might become pregnant. Which is the most appropriate suggestion made by the nurse?
(a) “I understand your concern; you may want to start your daughter on long-acting contraception.”
(b) “Women with Down syndrome are infertile, so you do not need to worry about her getting pregnant.”
(c) “I understand your concern; you may want to enroll your daughter in an abstinence program. ”
(d) “I know it may be difficult, but you may want to suggest that your daughter break off the relationship.”
Answer:
(a) “I understand your concern; you may want to start your daughter on long-acting contraception.”
Explanation:
Children with Down syndrome range from having severe intellectual disability to having low- average intelligence. Thus, the adolescent’s ability to make informed choices regarding sexual activity is limited. Long-acting contraception, such as an intrauterine device or a progestin implant, greatly reduces the risk of unwanted pregnancy.
Most women with Down syndrome are fertile; however, children born to women with Down syndrome often have congenital defects. An abstinence program may not be effective due to the intellectual level of children with Down syndrome. Suggesting that the adolescent break off the relationship does not ensure that she will.
Question 20.
A nurse is assessing a child who has a mild intellectual disability. The best indication of how this child is progressing can be obtained by observing in which social setting?
(a) at school with his teacher
(b) at home with his family
(c) in the clinic with his mother
(d) playing soccer with his friends
Answer:
(a) at school with his teacher
Explanation:
Watching the child relate to his teacher and schoolwork is the best indication of how he is progressing. School involves interacting with persons who are not relatives and places the child in a situation that is not totally familiar. Observing the client in situations with family and friends shows social relationships but does not indicate how the child is learning new intellectual skills.
Question 21.
After talking with the parents of a child with Down syndrome, the nurse should help the parents establish which goal?
(a) Encourage self-care skills in the child.
(b) Teach the child something new each day.
(c) Encourage more lenient behavior limits for the child.
(d) Achieve age-appropriate social skills.
Answer:
(a) Encourage self-care skills in the child.
Explanation:
The goal in working with children with intellectual disabilities is to train them to be as independent as possible, focusing on developmental skills. The child may not be capable of learning something new every day, but he or she does need to repeat what has been taught previously.
Rather than encouraging more lenient behavior limits, the parents need to be strict and consistent when setting limits for the child. Most children with Down syndrome are unable to achieve age-appropriate social skills due to their disability. Rather, they are taught socially appropriate behaviors.
Question 22.
The nurse discusses with the parents how best to raise the IQ of their child with Down syndrome. Which intervention would be most appropriate?
(a) Serve hearty, nutritious meals.
(b) Give vasodilator medications as prescribed.
(c) Let the child play with more able children.
(d) Provide stimulating, nonthreatening life experiences.
Answer:
(d) Provide stimulating, nonthreatening life experiences.
Explanation:
Nonthreatening experiences that are stimulating and interesting to the child have been observed to help raise IQ. Practices such as serving nutritious meals or letting the child play with more able children have not been supported by research as beneficial in increasing intelligence. Vasodilator medications act to increase oxygenation to the tissues, including the brain. However, these medications do not increase the child’s IQ.
Question 23.
When developing a teaching plan for the parents of a child with Down syndrome, the nurse focuses on activities to increase which factor for the parents?
(a) affection for their child
(b) responsibility for their child’s welfare
(c) understanding of their child’s disability
(d) confidence in their ability to care for their child
Answer:
(d) confidence in their ability to care for their child
Explanation:
When teaching the parents of a child with Down syndrome, activities should focus on increasing the parents’ confidence in their ability to care for the child. The parents must continue to work daily with their child. Most parents feel affection and a sense of responsibility for their child regardless of the child’s limitations. Parents usually understand the child’s disability on the cognitive level but have difficulty accepting it on the emotional level. As the parents’ confidence in their caring abilities increases, their understanding of the child’s disability also increases on all levels.
Question 24.
After the nurse instructs a group of schoolteachers about seizures, the teachers role-play a scenario involving a child experiencing a generalized tonic-clonic seizure. Which action, when performed first, indicates that the nurse’s teaching has been successful?
(a) Ask the other children what happened before the seizure.
(b) Move the child to the nurse’s office for privacy.
(c) Remove any nearby objects that could harm the child.
(d) Place a padded tongue blade between the child’s teeth.
Answer:
(c) Remove any nearby objects that could harm the child.
Explanation:
During a generalized tonic-clonic seizure, the first priority is to keep the child safe and protect the child by removing any nearby objects that could cause injury. Although obtaining information about events surrounding the seizure is important, this information can be obtained later, once the child’s safety is ensured. During a seizure, the child should not be moved. Although providing privacy is important, the child’s safety is the priority. During a seizure, nothing should be forced into the client’s mouth because this can cause severe damage to the teeth and mouth.
Question 25.
A nurse is developing a plan of care with the parents of a school-age client diagnosed with a seizure disorder. What instructions should the nurse give the parents to promote the client’s growth and development?
(a) The child will need activity limitation and will be unable to perform as well as her peers.
(b) There is potential for a learning disability, and the child may need tutoring to reach her grade level.
(c) The child will likely have normal intelligence and be able to attend regular school.
(d) There will be problems associated with social stigma, and parents should consider home-schooling.
Answer:
(c) The child will likely have normal intelligence and be able to attend regular school.
Explanation:
Most children who develop seizures after infancy are intellectually normal. A child with a seizure disorder needs the same experiences and opportunities to develop intellectual, emotional, and social abilities as any other child. Activity limi-tation is not needed. Learning disabilities are not associated with seizures. The child is able to attend public school, and social stigma is a rarity.
Question 26.
The parents of a child with occasional generalized seizures want to send the child to summer camp. The parents contact the nurse for advice on planning for the camping experience. Which type of activity should the nurse and family decide the child should most avoid?
(a) rock climbing
(b) hiking
(c) swimming
(d) tennis
Answer:
(a) rock climbing
Explanation:
A child who has generalized seizures should not participate in activities that are potentially hazardous. Even if accompanied by a responsible adult, the child could be seriously injured if a seizure were to occur during rock climbing. Someone also should accompany the child during activities in the water. At summer camps, hiking and swimming would occur most commonly as group activities, so someone should be with the child. Tennis would be considered an appropriate, nonhazardous activity for a child with generalized seizures.
Question 27.
Which statement obtained from the nursing history of a toddler should alert the nurse to suspect that the child has had a febrile seizure?
(a) The child has had a low-grade fever for several weeks.
(b) The family history is negative for convulsions.
(c) The seizure resulted in respiratory arrest.
(d) The seizure occurred when the child had a respiratory infection.
Answer:
(d) The seizure occurred when the child had a respiratory infection.
Explanation:
Most febrile seizures occur in the presence of an upper respiratory infection, otitis media, or tonsillitis. Febrile seizures typically occur during a temperature rise rather than after prolonged fever. There appears to be increased susceptibility to febrile seizures within families. Infrequently, febrile seizures may lead to respiratory arrest.
Question 28.
After the nurse teaches the parents of a child with febrile seizures about methods to lower temperature other than using medication, which statement by the parents indicates successful teaching?
(a) “We will add extra blankets when he says he is cold.”
(b) “We will wrap him in a blanket if he starts shivering.”
(c) “We will make the bath water cold enough to make him shiver.”
(d) “We will use a solution of half alcohol and half water when sponging him.”
Answer:
(b) “We will wrap him in a blanket if he starts shivering.”
Explanation:
Shivering, the body’s defense against rapid temperature decrease, results in an increase in body temperature. Therefore, the parents need to take measures to stop the shivering (and the resulting increase in body temperature) by increasing the room temperature or the temperature of the child’s immediate environment (such as with blankets) until the shivering stops.
Then, attempts are made to lower the temperature more slowly. Shivering does not necessarily correlate with being cold. Alcohol, a toxic substance, can be absorbed through the skin. Its use is to be avoided.
Question 29.
An adolescent girl with a seizure disorder controlled with phenytoin and carbamazepine asks the nurse about getting married and having children. Which response by the nurse would be most appropriate?
(a) “You probably should not consider having children until your seizures are cured.”
(b) “Your children will not necessarily have an increased risk of seizure disorder.”
(c) “When you decide to have children, talk to the health care provider (HCP) about changing your medication.”
(d) “Women who have seizure disorders commonly have a difficult time conceiving.”
Answer:
(c) “When you decide to have children, talk to the health care provider (HCP) about changing your medication.”
Explanation:
Phenytoin sodium is a known teratogenic agent, causing numerous fetal problems. Therefore, the adolescent should be advised to talk to the HCP HI to see if changing the medication is possible. Additionally, anticonvulsant requirements usually increase during pregnancy. Seizures can be controlled but cannot be cured. There is a familial tendency for seizure disorders. Seizure disorders and infertility are not related.
Question 30.
When teaching an adolescent with a seizure disorder who is receiving valproic acid, the nurse should instruct the client to immediately report which sign or symptom to the health care provider (HCP)?
(a) diarrhea
(b) loss of appetite
(c) jaundice
(d) sore throat
Answer:
(c) jaundice
Explanation:
A toxic effect of valproic acid is liver toxicity, which may manifest with jaundice and abdominal pain. If jaundice occurs, the client needs to notify the HCP [QI] as soon as possible. Diarrhea and sore throat are not common side effects of this drug. Increased appetite is common with this drug.
Question 31.
A 3-month-old infant with meningococcal meningitis has just been admitted to the pediatric unit. Which nursing intervention has the highest priority?
(a) instituting droplet precautions
(b) administering acetaminophen
(c) obtaining history information from the parents
(d) orienting the parents to the pediatric unit
Answer:
(a) instituting droplet precautions
Explanation:
Instituting droplet precautions is the priority for a newly admitted infant with meningococcal meningitis. Acetaminophen may be prescribed, but administering it does not take priority over instituting droplet precautions. Obtaining history information and orienting the parents to the unit do not take priority
Question 32.
During the acute stage of meningitis, a 3-year- old child is restless and irritable. Which intervention would be most appropriate to institute?
(a) limiting conversation with the child
(b) keeping extraneous noise to a minimum
(c) allowing the child to play in the bathtub
(d) performing treatments quickly
Answer:
(b) keeping extraneous noise to a minimum
Explanation:
A child in the acute stage of meningitis is irritable and hypersensitive to loud noise and light. Therefore, extraneous noise should be minimized and bright lights avoided as much as possible. There is no need to limit conversations with the child. However, the nurse should speak in a calm, gentle, reassuring voice. The child needs gentle and calm bathing.
Because of the acuteness of the infection, sponge baths would be more appropriate than tub baths. Although treatments need to be completed as quickly as possible to prevent overstressing the child, they should be performed carefully and at a pace that avoids sudden movements to prevent startling the child and subsequently increasing intracranial pressure.
Question 33.
Which sign should lead the nurse to suspect that a child with meningitis has developed disseminated intravascular coagulation?
(a) hemorrhagic skin rash
(b) edema
(c) cyanosis
(d) dyspnea on exertion
Answer:
(a) hemorrhagic skin rash
Explanation:
Disseminated intravascular coagulation is characterized by skin petechiae and a purpuric skin rash caused by spontaneous bleeding into the tissues. An abnormal coagulation phenomenon causes the condition. Heparin therapy is often used to interrupt the clotting process. Edema would suggest a fluid volume excess. Cyanosis would indicate decreased tissue oxygenation. Dyspnea on exertion would suggest respiratory problems, such as pulmonary edema.
Question 34.
When interviewing the parents of a toddler, the nurse should suspect pneumococcal meningitis if there is a history of which illness?
(a) bladder infection
(b) middle ear infection
(c) fractured clavicle
(d) septic arthritis
Answer:
(b) middle ear infection
Explanation:
Organisms that cause bacterial meningitis, such as pneumococci or meningococci, are commonly spread in the body by vascular dissemination from a middle ear infection. The meningitis may also be a direct extension from the paranasal and mastoid sinuses. The causative organism is a pneumococcus. A chronically draining ear is also frequently found.
Bladder infections commonly are caused by Escherichia coli, unrelated to the development of pneumococcal meningitis. Pneumococcal meningitis is unrelated to a fractured clavicle or to septic arthritis, which is commonly caused by Staphylococcus aureus, group A streptococci, or Haemophilus influenzae.
Question 35.
A preschooler with pneumococcal meningitis is receiving intravenous antibiotic therapy. When dis-continuing the intravenous therapy, the nurse allows the child to apply a dressing to the area where the catheter is removed. The nurse’s rationale for doing so is based on the interpretation that a child in this age group has a need to accomplish which goal?
(a) Trust those caring for her.
(b) Find diversional activities.
(c) Protect the image of an intact body.
(d) Relieve the anxiety of separation from home.
Answer:
(c) Protect the image of an intact body.
Explanation:
Preschool-age children worry about having an intact body and become fearful of any threat to body integrity. Allowing the child to participate in required care helps protect her image of an intact body. Development of trust is the task typically associated with infancy.
Additionally, allowing the child to apply a dressing over the intravenous insertion site is unrelated to the development of trust. Finding diversional activities is not a priority need for a child in this age group. Separation anxiety is more common in toddlers than in preschoolers.
Question 36.
A child with meningitis is to receive 1,0 mL of dextrose 5% in normal saline over 12 hours. At what rate in milliliters per hour should the nurse set the pump? Round your answer to the nearest whole number .................. mL/h.
Answer:
83 mL/h
Explanation:
1,000 mL ÷ 12 h = 83 mL/h
Question 37.
Nursing care management of the child with bacterial meningitis includes which interventions? Select all that apply.
(a) administration of IV antibiotics
(b) IV fluids at IV 2 times maintenance
(c) decreasing environmental stimuli
(d) neurologic checks every 4 hours
(e) administration of IV anticonvulsants
Answer:
(a) administration of IV antibiotics
(c) decreasing environmental stimuli
(d) neurologic checks every 4 hours
Explanation:
(a), (c), (d) Antibiotics are indicated for the treat¬ment of bacterial meningitis. Clients with bacterial meningitis often have increased ICP, It is necessary to maintain adequate hydration. However, infusing fluids at IV2 maintenance can increase ICP, further risking neurologic damage due to cerebral edema. Most children with meningitis are sensitive to sound, light, and stimulation.
Decreasing environmental stimuli and keeping the room dim and quiet are essential. Frequent neurologic checks are necessary to monitor any changes in the child’s level of consciousness. Anticonvulsants are not indicated unless the child experiences seizures as a result of the meningitis.
Question 38.
The nurse is monitoring an infant with meningitis for signs of increased intracranial pressure (ICP). The nurse should assess the infant for which signs or symptoms? Select all that apply.
(a) irritability
(b) headache
(c) mood swings
(d) bulging fontanelle
(e) emesis
Answer:
(a) irritability
(d) bulging fontanelle
(e) emesis
Explanation:
(a), (d), (e) Irritability, bulging fontanelle, and emesis are all signs of increased ICP in an infant. A headache may be present in an infant with increased ICP; however, the infant has no way of communicating this to the parent. A headache is an indication of increased ICP in a verbal child. An infant cannot exhibit mood swings; this is indicative of increased ICP in a child or adolescent
Question 39.
A hospitalized preschooler with meningitis who is to be discharged becomes angry when the discharge is delayed. Which play activity would be most appropriate at this time?
(a) reading the child a story
(b) painting with watercolors
(c) pounding on a pegboard
(d) stacking a tower of blocks
Answer:
(a) reading the child a story
Explanation:
The child is angry and needs a positive outlet for expression of feelings. An emotionally tense child with pent-up hostilities needs a physical activity that will release energy and frustration. Pounding on a pegboard offers this opportunity. Listening to a story does not allow the child to express emotions.
It also places the child in a passive role and does not allow the child to deal with feelings in a healthy and positive way. Activities such as painting and stacking a tower of blocks require concentration and fine movements, which could add to frustration. However, if the child then knocks the tower over, doing so may help to dispel some of the anger.
Question 40.
The nurse is admitting a toddler with the diagnosis of near-drowning in a neighbor’s heated swimming pool to the emergency department. The nurse should assess the child for which complication?
(a) hypothermia
(b) hypoxia
(c) fluid aspiration
(d) cutaneous capillary paralysis
Answer:
(b) hypoxia
Explanation:
Hypoxia is the primary problem because it results in brain cell damage. Irreversible brain damage occurs after 4 to 6 minutes of submersion. Hypothermia occurs rapidly in infants and children because of their large body surface area. Hypothermia is more of a problem when the child is in cold water. Although fluid aspiration occurs in most drownings and results in atelectasis and pulmonary edema, further aggravating hypoxia, hypoxia is the primary problem. Cutaneous capillary paralysis is not a problem.
Question 41.
The nurse is caring for a lethargic but arous-able preschooler who is a victim of a near-drowning accident. What should the nurse do first?
(a) Administer oxygen.
(b) Institute rewarming.
(c) Prepare for intubation.
(d) Start an IV infusion.
Answer:
(a) Administer oxygen.
Explanation:
Near-drowning victims typically suffer hypoxia and mixed acidosis. The priority is to restore oxygenation and prevent further hypoxia. Here, the client has blunted sensorium but is not unconscious; therefore, delivery of supplemental oxygen with a mask is appropriate.
Warming protocols and fluid resuscitation will most likely be needed to help correct acidosis, but these interventions are secondary to oxygen administration. Intubation is required if the child is comatose, shows signs of airway compromise, or does not respond adequately to more conservative therapies.
Question 42.
The parents of a child tell the nurse that they feel guilty because their child almost drowned. Which remark by the nurse would be most appropriate?
(a) “I can understand why you feel guilty, but these things happen.”
(b) “Tell me a little bit more about your feelings of guilt.”
(c) “You should not have taken your eyes off of your child.”
(d) “You should focus on the fact that your child will be all right.”
Answer:
(b) “Tell me a little bit more about your feelings of guilt.”
Explanation:
Guilt is a common parental response. The parents need to be allowed to express their feelings openly in a nonthreatening, nonjudgmental atmosphere. Telling the parents that these things happen does not allow them to verbalize their feelings. Telling the parents that they should not have taken their eyes off the child blames them, possibly further contributing to their guilt.
Telling the parents that they should not feel guilty denies the parents’ feelings of guilt and is inappropriate. Telling the parents that they are lucky that the child will be okay does not remove the feelings of guilt.
Question 43.
Which assessment would be most important for the nurse to make initially in a school-age child being seen in the clinic who has a sore throat, muscle tenderness, arms feeling weak, and generally is not feeling well?
(a) difficulty swallowing
(b) diet intake for the last 24 hours
(c) exposure to illnesses
(d) difficulty urinating
Answer:
(a) difficulty swallowing
Explanation:
The child is exhibiting symptoms associated with Guiliain-Barre syndrome (infectious polyneuritis). Most children with sore throat have some difficulty swallowing, so it is important for the nurse to determine the extent of difficulty to aid in determining what action is necessary. Typically, a sore throat precedes the paralysis in clients with Guiliain-Barre syndrome.
Muscle tenderness is an initial symptom. Distal muscle weakness follows proximal muscle weakness, ultimately progressing to paralysis. Diet history and difficulty urinating will not contribute to assessment of the cause of a sore throat or difficulty swallowing. After determining the extent of difficulty swallowing, the nurse can obtain information about exposure to illness.

Question 44.
Which action should be the priority when caring for a school-age child admitted to the pediatric unit with the diagnosis of Guillain-Barre syndrome?
(a) Assess the child’s ability to follow simple commands.
(b) Evaluate the child’s bilateral muscle strength.
(c) Make a game of the range-of-motion exercises.
(d) Provide the child with a diversional activity.
Answer:
(b) Evaluate the child’s bilateral muscle strength.
Explanation:
With Guiliain-Barre syndrome, progressive ascending paralysis occurs. Therefore, the nurse should assess the child’s muscle strength bilaterally to determine the extent of involvement and progression of the illness. Assessing the child’s ability to follow simple commands evaluates brain function. Range-of-motion exercises are an important part of treatment, but they are not a priority initially. Although the child may need diversional activities later, they also are not an initial priority.
Question 45.
The nurse asks a school-age child with Guillain-Barre syndrome to cough and also assesses the child’s speech for decreased volume and clarity. The underlying rationale for these assessments is to determine which finding?
(a) inflammation of the larynx and epiglottis
(b) increased intracranial pressure
(c) involvement of facial and cranial nerves
(d) regression to an earlier developmental phase
Answer:
(c) involvement of facial and cranial nerves
Explanation:
In a child with Guiliain-Barre syndrome, decreased volume and clarity of speech and decreased ability to cough voluntarily indicate ascending progression of neural inflammation, specifically affecting the cranial nerves. Inflammation of the larynx and epiglottis is manifested by hoarseness, stridor, and dyspnea.
A child with laryngeal inflammation still retains the ability to cough. Irritability, behavior changes, headache, and vomiting are common signs of increased intracranial pressure in a school-age child. Regression would be manifested by being more dependent and less able to care for self.
Question 46.
Assessment of a school-age child with Guillain-Barre syndrome reveals absent gag and cough reflexes. Which problem should receive the highest priority during the acute phase?
(a) impaired physical mobility related to paralysis
(b) ineffective breathing pattern related to neuro muscular impairment
(c) impaired swallowing related to neuromuscu lar impairment
(d) fluid volume deficits related to total urinary incontinence
Answer:
(b) ineffective breathing pattern related to neuro muscular impairment
Explanation:
An ineffective breathing pattern caused by the ascending paralysis of the disorder interferes with the child’s ability to maintain an adequate oxygen supply. Therefore, this nursing diagnosis takes precedence. Additionally, as the neurologic impairment progresses, it will probably have an effect on the child’s ability to maintain respirations. Although impaired swallowing, impaired physical mobility, and incontinence may occur with the ascending paralysis of this disorder, oxygenation is the priority.
Question 47.
A 9-year-old child with Guillain-Barre syndrome requires mechanical ventilation. Which action should the nurse take?
(a) Maintain the child in a supine position to prevent unnecessary nerve stimulation.
(b) Transfer the child to a bedside chair three times a day to prevent postural hypotension.
(c) Engage the child in vigorous passive range- of-motion exercises to prevent loss of muscle function.
(d) Turn the child slowly and gently from side to side to prevent respiratory complications.
Answer:
(d) Turn the child slowly and gently from side to side to prevent respiratory complications.
Explanation:
Even in the absence of respiratory problems or distress, the child must be turned frequently to help prevent the cardiopulmonary complications associated with immobility, such as atelectasis and pneumonia. Maintaining the child in a supine position is unnecessary. Doing so does not prevent unnecessary nerve stimulation. In addition, maintaining a supine position may lead to stasis of secretions, placing the child at risk for pneumonia.
Transferring the child to a chair will not prevent postural hypotension. However, doing so will increase vascular tone and help prevent respiratory and skin complications. During the acute disease phase, vigorous physiotherapy is contraindicated because the child may experience muscle pain and be hypersensitive to touch. Careful and gentle han-dling is essential.
Question 48.
The parent brings a child to the clinic after discharge from the hospital for Guillain-Barre syndrome. Which statement by the parent indicates that the discharge plan is being followed?
(a) “She and her sister argue all day.”
(b) “I have to bribe her to get her to do her exercises.”
(c) “I take her to the pool where she can exercise with other children.”
(d) “She has missed a few of her therapy sessions because she often sleeps.”
Answer:
(c) “I take her to the pool where she can exercise with other children.”
Explanation:
Developmentally appropriate activities and therapeutic play should be used as rehabilitation modalities. Taking the child to the pool to exercise with other children indicates that the child is participating in exercise as well as engaging with other children, thus fostering development. Arguing with the sister does not address the discharge plan.
Inappropriate rewards or threats should not be used to coerce a child into compliance. Although the mother is attempting to comply with the discharge plan, bribery is an inappropriate technique to foster compliance. Missing therapy sessions delays recovery. The parents need to help set the child’s schedule to ensure that she gets adequate rest to be able to follow her treatment plan.
Question 49.
A 12-year-old child has had a traumatic head injury from playing in a football game. He is admitted to the emergency department and transferred to the pediatric intensive care unit. He has an IV of dextrose 5% in water at 21 mL/h and nasal oxygen at 2 L/min. The nurse is assessing the child at the beginning of the shift (2300 hours) and reviews the Glasgow Coma Scale flow sheet below. The nurse notes that the child responds to pain, is making incomprehensible sounds, and has abnormal flexion of the limbs. What should the nurse do first?
|
Test |
Score |
Client response |
|
Eye Opening |
||
|
Spontaneously |
4 |
Opens eyes spontaneously |
|
To speech |
3 |
Open eyes to verbal command |
|
To pain |
2 |
Open eyes to painful stimulus |
|
None |
1 |
Doesn’t open eyes in response to stimulus |
|
Motor Response |
||
|
Obeys |
6 |
Reacts to verbal command |
|
Localize |
5 |
Identifiers localized pain |
|
Withdraws |
4 |
Flexes and withdraws from painful stimulus |
|
Abnormal Flexion |
3 |
Assumes a decerebrate position |
|
Abnormal |
2 |
Assumes a decerebrate position |
|
Extension |
|
|
|
None |
1 |
No response; lies flacid |
|
Verbal Response |
||
|
Oriented |
5 |
Is oriented and converse |
|
Confused |
4 |
Is disoriented and confused |
|
Inappropriate Words |
3 |
Replies randomly with incorrect words |
|
Incomprehensible |
2 |
Moans or screams |
|
None |
1 |
No responses |
|
Date |
Time |
Progress Notes |
|
11/13 |
1700 |
Gcs = 13 |
|
11/13 |
1800 |
Gcs = 12 |
|
11/13 |
1900 |
Gcs = 13 |
|
11/13 |
2000 |
Gcs = 11 |
|
11/13 |
2100 |
Gcs = 10 |
|
11/13 |
2200 |
Gcs = 9 |
(a) Notify the health care provider (HCP).
(b) Lower the head of the bed.
(c) Increase the rate of nasal oxygen.
(d) Increase the rate of the IV infusion.
Answer:
(a) Notify the health care provider (HCP).
Explanation:
This client is experiencing neurologic changes consistent with increasing intracranial pressure (ICP). The nurse should first notify the HCP 01. The HCP may intubate the child to ensure a patent airway. The nurse should not lower the head of the bed as this will cause increased ICP. The nurse should ensure an adequate fluid balance. The HCP will likely prescribe hypertonic saline to draw fluid from the brain.
Question 50.
A school-age child with a severe head injury is unconscious and has coarse breath sounds, a temperature of 39°C (102.2°F), a heart rate of 70 bpm,
a blood pressure of 130/60 mm Hg, and an intracranial pressure (ICP) of 36 mm Hg. Which action should the nurse perform first?
(a) Administer prescribed IV mannitol.
(b) Suction the child.
(c) Encourage the parent to talk to the child.
(d) Administer prescribed rectal acetaminophen.
Answer:
(a) Administer prescribed IV mannitol.
Explanation:
An ICP level >15 mm Hg is abnormal. This child’s vital signs indicate increased ICP. Mannitol is an osmotic diuretic and will decrease the child’s ICP. Suctioning the child will increase the ICP. Encouraging the parent to talk to the child may be comforting but will not decrease the ICP.
The priority for this child is decreasing the ICP to avoid further brain injury. The fever is likely due to the head injury and will not decrease with acetaminophen. A cooling blanket is the most effective means of reducing a fever in a client with a head injury.
Question 51.
The nurse is inserting a nasogastric (NG) tube in a child admitted with head trauma. The nurse should explain to the parents that the NG tube will be used for what purpose?
(a) Administer medications.
(b) Decompress the stomach.
(c) Obtain gastric specimens for analysis.
(d) Provide adequate nutrition.
Answer:
(b) Decompress the stomach.
Explanation:
For the child with serious head trauma, a nasogastric tube is inserted initially to decompress the stomach and to prevent vomiting and aspiration. Medications would be administered intravenously in the initial period. The tube will not be used to obtain gastric specimens. Nutrition is not a priority initially. Later on, the tube may be used to administer feedings.
Question 52.
A nasogastric tube is prescribed to be inserted for a child with severe head trauma. Diagnostic testing reveals that the child has a basilar skull fracture. What should the nurse do next?
(a) Ask for the prescription to be changed to an oral gastric tube.
(b) Attempt to place the tube into the duodenum.
(c) Test the gastric aspirate for blood.
(d) Use extra lubrication when inserting the naso gastric tube.
Answer:
(a) Ask for the prescription to be changed to an oral gastric tube.
Explanation:
Because a basilar skull fracture can involve the frontal and ethmoid bones, inserting a nasogastric tube carries the risk of introducing the tube into the cranial cavity through the fracture. An oral gastric tube is preferred for a client with a basilar skull fracture. The tube would not be placed into the duodenum. Gastric aspirate is not routinely tested for blood unless there is an indication to suggest bleeding, such as a falling hemoglobin or visible blood in the drainage.
Question 53.
The parents of a child in a coma with a serious head injury ask the nurse if the child is going to be all right. Which response by the nurse would be most appropriate?
(a) “Children usually do not do very well after head injuries like this.”
(b) “Children usually recover rapidly from head injuries.”
(c) “It is hard to tell this early, but we will keep you informed of the progress.”
(d) “That is something you will have to talk to the health care provider (HCP) about.”
Answer:
(c) “It is hard to tell this early, but we will keep you informed of the progress.”
Explanation:
As a rule, children demonstrate more rapid and more complete recovery from coma than do adults. However, it is extremely difficult to predict a specific outcome. Reassuring the parents that they will be kept informed helps open lines of communication and establish trust.
Telling the parents that children do not do well would be extremely negative, destroying any hope that the parents might have. Telling the parents that children recover rapidly may give the parents false hopes. Telling the parents to talk to the HCP Q3 ignores the parents’ concerns and interferes with trust building.
Question 54.
A parent of a child with a moderate head injury asks the nurse, “How will you know if my child is getting worse?” The nurse should tell the parents that best indicator of the child’s brain function is which factor?
(a) the vital signs
(b) level of consciousness
(c) reactions of the pupils
(d) motor strength
Answer:
(b) level of consciousness
Explanation:
The level of consciousness (LOC) is the best indicator of brain function. If the child’s condition deteriorates, the nurse would notice changes in LOC before any other changes and should notify the health care provider (HCP) that these changes are occurring. Changes in vital signs and pupils typically follow changes in LOC. Motor strength is primarily assessed as a voluntary function. With changes in levels of consciousness, there may be motor changes.
Question 55.
When developing the plan of care for a child who is unconscious after a serious head injury, the nurse would expect to place the child in which position?
(a) prone with hips and knees slightly elevated
(b) lying on the side, with the head of the bed elevated
(c) lying on the back, in the Trendelenburg position
(d) in the semi-Fowler’s position, with arms at the side
Answer:
(b) lying on the side, with the head of the bed elevated
Explanation:
The unconscious child is positioned to prevent aspiration of saliva and minimize intracranial pressure. The head of the bed should be elevated, and the child should be in either the semiprone or the side-lying position. Lying prone with hips and knees slightly elevated increases intracranial pressure, as does lying on the back in the Trendelenburg position. The semi-Fowler’s position with arms at the side is not the best choice.
Question 56.
The health care provider (HCPj has prescribed intravenous mannitol for a child with a head injury. The best indicator that the drug has been effective is which assessment finding?
(a) increased urine output
(b) improved level of consciousness
(c) decreased intracranial pressure
(d) decreased edema
Answer:
(c) decreased intracranial pressure
Explanation:
Mannitol is an osmotic diuretic used to reduce intracranial pressure. The use of the drug is controversial and should be reserved to cases that do not respond to other treatments or when brain herniation is likely. Children this sick should be on intracranial pressure (ICP) monitoring. The best indicator that the drug has produced the desired results is a reduction in the ICP.
Improved levels of consciousness should follow reduced ICP. While the drug will cause increased urine output, that measurement in and of itself does not indicate successful treatment. Because the drug is being used for head injuries, not to improve urine output in acute renal failure, the child may not have visible edema.
Question 57.
The nurse assigned to telephone triage returns the call of a parent whose teenager experienced a hard tackle last night. The parent reports, “He seemed dazed after it happened, and the coach had him sit out the rest of the game, but he’s fine now.” What is the most appropriate instruction for the nurse to give?
(a) “Take him immediately to the emergency department.”
(b) “He can’t return to play until he has been evaluated by a health care provider (HCP).”
(c) “If he seems fine now and has had no other symptoms, it probably was not a concussion.”
(d) “Watch him closely, and call us back if you see any changes.”
Answer:
(b) “He can’t return to play until he has been evaluated by a health care provider (HCP).”
Explanation:
Appearing dazed or stunned after a head injury is a symptom of a concussion. Concussion care includes removing the athlete from play and having the injury evaluated. Athletes should not return to play until they have been cleared by an HCP. Concussions require ongoing monitoring. Since the client has no signs of deterioration in neurologic function, it may best be provided by an HCP, who will follow him over time, rather than through an emergency department.
Question 58.
A history of which factors will complicate the recovery from a concussion? Select all that apply.
(a) asthma
(b) attention deficit hyperactivity disorder (ADHD)
(c) depression
(d) migraines
(e) obesity
(f) previous concussion
Answer:
(b) attention deficit hyperactivity disorder (ADHD)
(c) depression
(d) migraines
(f) previous concussion
Explanation:
(b), (c), (d), (f) Concussion recovery can be complicated by any previous brain injury, such as a previous concussion. Recovery can also be complicated by the presence of other neurologic problem, such as migraines, ADHD, and depression. Asthma and obesity have not been linked to concussion recovery.
Question 59.
A 3-year-old is recovering from a concussion. The persistence of which finding would the nurse consider as being a normal finding for a 3-year-old?
(a) lack interest in favorite toys
(b) change in eating habits
(c) inability to hop
(d) increased temper tantrums
Answer:
(c) inability to hop
Explanation:
The inability to hop is not concerning because it is a milestone for a 4-year-old, not a 3-year-old. Lack of interest in toys, changes in eating habits, and increased temper tantrums that persist several weeks all require an evaluation by a neurologist or other specialist.
Question 60.
The nurse teaches an adolescent about returning to school after a concussion. Which statement by the client reflects the need for more teaching?
(a) “I should limit my activities that require concentration.”
(b) “I must slowly return to my previous activity level as my symptoms improve.”
(c) “My symptoms may reemerge with exertion.”
(d) “Time is the most important factor in my recovery.”
Answer:
(d) “Time is the most important factor in my recovery.”
Explanation:
While recovery from a concussion takes time, adequate rest and limiting exertion facilitate recovery. Both physical and cognitive exertion can cause the reemergence of symptoms and delay recovery. As symptoms resolve, clients may slowly return to previous levels of activity.
Question 61.
A child with a brain tumor has a decreased respiratory rate and is less responsive to verbal commands than he was when the nurse assessed the client the previous hour. What should the nurse do next?
(a) Raise the head of the bed.
(b) Notify the health care provider (HCP).
(c) Implement seizure precaution
(d) Obtain an oximeter reading.
Answer:
(b) Notify the health care provider (HCP).
Explanation:
A decreasing level of consciousness, decerebrate positioning, or Cushing’s triad (elevated systolic blood pressure, decreased pulse, and decreased respiratory rate) indicates that there is pressure on the brain stem and the client could require intuba-tion and cardiac resuscitation unless the health care provider (HCP) can prescribe a medication or surgical procedure to reduce the intracranial pressure.
Raising the head of the bed could offer some reduction in the intracranial pressure by increasing venous blood return from the head, but it is not the priority at this time. While brain tumors can cause seizures in children, they often manifest early in the disease process. The impending risk of seizure is not as great as the potential for respiratory arrest. An oximeter would measure the oxygen level in the blood but not necessarily in the brain.
Question 62.
The nurse is caring for a preschool-age client with a neuroblastoma who has been receiving chemotherapy for the last 4 weeks. His lab results indicate an Hgb of 12.5 g/dL (125 g/L), an HCT of 36.8% (0.37), a WBC of 2,000 mm3 (2 x 109/L), and a platelet count of 150,000 pL (150 x 109/L). Based on the child’s lab values, what is the highest priority nursing intervention?
(a) Encourage meticulous handwashing by the client and visitors.
(b) Prepare to give the child a transfusion of platelets.
(c) Encourage mouth care with a soft toothbrush.
(d) Prepare to give the child a transfusion of packed red blood cells.
Answer:
(b) Prepare to give the child a transfusion of platelets.
Explanation:
A WBC of 2,000 mm3 (2 x 109/L) is low and increases risk for infection. Meticulous handwashing is a universal precaution and the first line of defense in combating infection. A platelet count of 150,0 pL (150 x 109/L) is normal, so there is no need for a platelet transfusion. Mouth care will help decrease the risk of infection. However, handwashing is the priority as it will have the greatest impact on diminishing the risk of infection. An Hgb of 12.5 g/dL (125 g/L) and an HCT of 36.8% (0.37) are within normal range, so there is no need to transfuse packed red blood cells.
Question 63.
An adolescent client has seen the school nurse several times with headache, vomiting, and difficulty walking. When calling the adolescent’s mother about these symptoms, the nurse should suggest the mother do what first?
(a) Schedule an appointment with the eye health care provider (HCP).
(b) Begin psychological counseling for her adolescent.
(c) Make an appointment with the adolescent's health care provider (HCP).
(d) Meet with the adolescent’s teachers to determine academic progress.
Answer:
(c) Make an appointment with the adolescent's health care provider (HCP).
Explanation:
A child who has symptoms of vomiting, headaches, and problems walking needs to be evaluated by a health care provider (HCP) to determine the cause. Unexplained headaches and vomiting along with difficulty walking (e.g., ataxia) may suggest a brain tumor.
Evaluation by an eye HCP would bo appropriate once a complete medical evaluation has been accomplished. Psychological counseling may he indicated for this adolescent, but only after medical evaluation to determine that she is physically healthy. Meeting with the child’s teachers would be appropriate after medical evaluation.
Question 64.
A school-age child is admitted to the hospital with the diagnosis of probable infratentorial brain tumor. During the child's admission to the pediatric unit, which action should the nurse anticipate taking first?
(a) Eliminate the child’s anxiety.
(b) Implement seizure precautions.
(c) Introduce the child to other clients of the same age.
(d) Prepare the child and parents for diagnostic procedures.
Answer:
(d) Prepare the child and parents for diagnostic procedures.
Explanation:
When a brain tumor is suspected, the child and parents are likely to be very apprehensive and anxious. It is unrealistic to expect to eliminate their fears; rather, the nurse’s goal is to decrease them. Preparing both the child and family during hospitalization can help them cope with some of their fears. Although the nurse may be able to decrease some of the child’s anxiety, it would be impossible to eliminate it.
Children with infratentorial tumors seldom have seizures, so seizure precautions are not indicated. Although introducing the child to other children is a positive action, this action would be more appropriate once the nurse has decreased some of the child’s and parents’ anxiety by preparing them.
Question 65.
The nurse is giving care to an infant with a brain tumor. The nurse observes the infant arches the back (see figure). What action should the nurse take first?
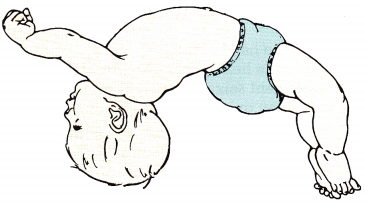
(a) Notify the health care provider (HCP).
(b) Stroke the back to release the arching.
(c) Pad the side rails of the crib.
(d) Place the child prone.
Answer:
(a) Notify the health care provider (HCP).
Explanation:
The infant has opisthotonos, an indication of brain stem herniation; the nurse should notify the HCP Q immediately and have resuscitation equipment ready. Stroking the back will not relieve the herniation or release the arching. Although the infant may also have a seizure, and padded side rails will prevent injury, the first action is to notify the HCP. Placing the child in a prone position will not relieve the herniation or release the arching.
Question 66.
The nurse is assessing a child diagnosed with a brain tumor. Which signs and symptoms should the nurse expect the child to demonstrate? Select all that apply.
(a) head tilt
(b) vomiting
(c) polydipsia
(d) lethargy
(e) increased appetite
(f) increased pulse
Answer:
(a) head tilt
(b) vomiting
(d) lethargy
Explanation:
(a), (b), (d) Head tilt, vomiting, and lethargy are HB classic signs assessed in a child with a brain tumor. Clinical manifestations are the result of location and size of the tumor. Polydipsia is rare with a brain tumor. It is more often a sign of diabetes insipidus following a closed head injury.
Increased appetite occurs during a growth spurt and is not necessarily HB a sign of a brain tumor. Increased pulse is a nonspe- & cific sign and can occur with many illnesses, cardiac anomalies, fever, or exercise. Slow heart rate is more associated with increased intracranial pressure seen BBH with brain tumors
Question 67.
After a child undergoes a craniotomy for an infratentorial brain tumor, the nurse should place the child in which position to prevent undue strain on the sutures?
(a) prone
(b) semi-Fowler’s
(c) side-lying
(d) Trendelenburg
Answer:
(c) side-lying
Explanation:
After surgery for an infratentorial tumor, the child is usually positioned flat on either side, with the head and neck in midline and the body slightly extended. Pillows against the back, not the head, help maintain position. Such a position helps avoid pressure on the operative site. Placing the hemorrhage.
Question 68.
A child who was intubated after a craniotomy now shows signs of decreased level of consciousness. The health care provider (HCP) prescribes manual hyperventilation to keep the PaCO2 between 25 and 29 mm Hg and the PaO2 between 80 and 100 mm Hg. The nurse interprets this prescription based on the understanding that this action will accomplish which goal?
(a) decrease intracranial pressure
(b) ensure a patent airway
(c) lower the arousal level
(d) produce hypoxia
Answer:
(a) decrease intracranial pressure
Explanation:
Hypercapnia, hypoxia, and acidosis are potent cerebral vasodilating mechanisms that can cause increased intracranial pressure. Lowering the carbon dioxide level and increasing the oxygen level through hyperventilation is the most effective short-term method of reducing intracranial pressure.
Although ensuring a patent airway is important, this is not accomplished by manual hyperventilation. Manual hyperventilation does not lower the arousal level; in fact, the arousal level may increase. Manual hyperventilation is used to reduce hypoxia, not produce it.
Question 69.
Which action should the nurse do first when noting clear drainage on the child’s dressing and bed linen after a craniotomy for a brain tumor?
(a) Change the dressing.
(b) Elevate the head of the bed.
(c) Test the fluid for glucose.
(d) Notify the health care provider (HCP).
Answer:
(c) Test the fluid for glucose.
Explanation:
Glucose in this clear, colorless fluid indicates the presence of cerebrospinal fluid. Excessive fluid leakage should be reported to the HCP FT The nurse should not change the dressing of a postoperative craniotomy client unless instructed to do so by the surgeon. Ordinarily, the head of the bed would not be elevated because this would put pressure on the sutures. The nurse should notify the HCP after testing the fluid for glucose.
Question 70.
An 8-year-old child does well after infratentorial tumor removal and is transferred back to the pediatric unit. Although she had been told about having her head shaved for surgery, she is very upset. After exploring the child’s feelings, the nurse should take which action?
(a) Ask the child if she would like to wear a hat.
(b) Reassure the child that her hair will grow back.
(c) Explain to the child’s parents that her reaction is normal.
(d) Suggest that the parents buy the child a wig as a surprise.
Answer:
(a) Ask the child if she would like to wear a hat.
Explanation:
It is not uncommon for a child to be concerned about a change in appearance when the entire head or only part of the head has been shaved. The child should be encouraged to par-ticipate in decisions about her care when possible. Asking her if she would like to wear a hat is one way to encourage this participation. Reassuring the child that her hair will grow back does not address the immediate change in appearance, and it ignores the child’s current feelings. Explaining that this type of reaction is normal does not address the child’s feelings.
The child needs to be able to express feelings and be involved in care as much as possible. Buying the child a wig as a surprise does not address the child’s feelings and does not allow her to participate in decision-making. Rather, the parents should ask the child if she would like a wig and then work with the child to determine what kind of wig she would like.
Question 71.
Which statement made by the parent of a school-age child who has had a craniotomy for a brain tumor would warrant further exploration by the nurse?
(a) “After this, I will never let her out of my sight again.”
(b) “I hope that she’ll be able to go back to school soon.”
(c) “I wonder how long it will be before she can ride her bike.”
(d) “Her best friend is eager to see her; I hope she won’t be upset.”
Answer:
(a) “After this, I will never let her out of my sight again.”
Explanation:
Parents of a child who has undergone neurosurgery can easily become overprotective. Yet, the parents must foster independence in the convalescing child. It is important for the child to resume age-appropriate activities, and parents play an important role in encouraging this. Statements about going back to school would be expected. Parents want the child to return to normal activities after a serious illness or injury as a sign that the child is doing well.
Question 72.
A nurse, who witnesses an accident involving an adolescent being thrown from a motorcycle, stops to help. The adolescent reports that he is now unable to move his legs. While waiting for the emergency medical service to arrive, what should the nurse do?
(a) Flex the adolescent’s knees to relieve stress on his back.
(b) Leave the adolescent as he is, staying close by.
(c) Remove the adolescent’s helmet as soon as possible.
(d) Assess the adolescent for abdominal trauma.
Answer:
(b) Leave the adolescent as he is, staying close by.
Explanation:
The adolescent’s signs and symptoms sug¬gest a spinal cord injury. A client with suspected spinal cord injury should not be moved until the spine has been immobilized. Removing the helmet could further aggravate a spinal cord injury. The nurse could assess for abdominal trauma, but only if it can be done without moving the adolescent.
Question 73.
An adolescent sustains a T3 spinal cord injury. After insertion of an intravenous line, a nasogastric tube, and an indwelling urinary catheter, the adolescent is admitted to the intensive care unit. What should the nurse do next when assessment reveals that the adolescent’s feet and legs are cool to the touch?
(a) Cover the adolescent’s legs with blankets.
(b) Report this finding to the health care provider (HCP) immediately.
(c) Reposition the adolescent’s legs.
(d) Lay the adolescent flat to aid circulation.
Answer:
(a) Cover the adolescent’s legs with blankets.
Explanation:
In spinal cord injury, temperature regulation is lost below T3. Body temperature must be maintained by adjusting room temperature or bed linens, such as covering the client’s legs with blankets. Coolness of the extremities is an expected find-ing. Therefore, it is not necessary to notify the HCP a immediately.
Repositioning the client’s legs does not alleviate the temperature regulation problem and could be harmful, considering the client’s diagnosis. Moving the legs before the spine is stabilized could lead to further cord damage. Laying the client flat will not increase the warmth to the legs and feet
Question 74.
During assessment of an adolescent who has sustained a recent thoracic spinal injury, the nurse auscultates the adolescent’s abdomen. The nurse explains to the parents that this is necessary because clients with spinal cord injury often develop which problem?
(a) abdominal cramping
(b) hyperactive bowel sounds
(c) paralytic ileus
(d) profuse diarrhea
Answer:
(c) paralytic ileus
Explanation:
A thoracic spinal cord injury involves the muscles of the lower extremities, bladder, and rectum. Paralytic ileus often occurs as a result of decreased gastrointestinal muscle innervation. The nurse evaluates this by auscultating the abdomen. Because the client has a thoracic spinal cord injury, the client may not feel abdominal cramping. Additionally, auscultation would provide no evidence of cramping.
Hyperactive bowel sounds would be evidenced with increased peristalsis; peristalsis would probably be diminished with this injury. Profuse diarrhea, resulting from increased peristalsis, would not be an expected finding. Diarrhea would be more commonly associated with a gastrointestinal infection.
Question 75.
Which finding should lead the nurse to decide that spinal shock was resolving in the adolescent with a spinal cord injury?
(a) atonic urinary bladder
(b) flaccid paralysis
(c) hyperactive reflexes
(d) widened pulse pressure
Answer:
(c) hyperactive reflexes
Explanation:
Spinal shock causes a loss of reflex activity below the level of the injury, resulting in bladder atony and flaccid paralysis. When the reflex arc returns, it tends to be overactive, resulting in spasticity. The reflexes and bladder become hypertonic during this phase of spinal shock resolution; sensation does not return. A widened pulse pressure is not associated with resolution of spinal shock.
Question 76.
A school-age boy with a spinal cord injury is moved to the rehabilitation unit. The nurse notes that the child tends to refuse to cooperate in care and to be hostile. The nurse interprets this behavior as indicative of which response?
(a) a stage of grief reaction
(b) a phase of rebellion
(c) a reaction to sensory overload
(d) a response to too much attention
Answer:
(a) a stage of grief reaction
Explanation:
After a catastrophic injury, individuals commonly experience grief. Initially, the person experiences denial, the most common response. With gradual awareness of the situation, anger commonly occurs. The child is demonstrating anger, not rebellion, as he gradually becomes aware of his situation. Rebellion is the child’s way to maintain autonomy and individuality.
It is a reaction to rigid rules. Examples include refusing to follow a treatment protocol when the child had no input and running away. Sensory overload would cause the child to be irritable and tired and to have difficulty sleeping. Too much attention usually would lead to irritability, difficulty sleeping, and mood swings.
Question 77.
Two months after an adolescent’s thoracic spinal cord injury, he has a pounding headache. The nurse notes that the client’s arms and face are flushed and he is diaphoretic. What should the nurse do next?
(a) Check the patency of the urinary catheter.
(b) Lower the adolescent’s head below his knees.
(c) Place the adolescent flat on his back.
(d) Prepare to administer epinephrine subcutaneously.
Answer:
(a) Check the patency of the urinary catheter.
Explanation:
The adolescent is exhibiting signs of autonomic dysreflexia, a generalized sympathetic response usually caused by bladder or bowel distention. Immediate treatment involves eliminating the cause. Because bladder distention is a common cause of this problem, the nurse should immediately determine the patency of the indwelling (Foley) catheter.
Lowering the head below the knees would increase the blood pressure and is contraindicated because of the spinal cord injury. Lying flat will not decrease blood pressure. Epinephrine is contraindi-cated because it elevates blood pressure and therefore can exacerbate the problem.
Question 78.
The nurse is admitting a child who has been diagnosed with bacterial meningitis to the pediatric unit. The nurse should implement which type of isolation?
(a) standard or routine precautions
(b) contact precautions
(c) airborne precautions
(d) droplet precautions
Answer:
(d) droplet precautions
Explanation:
Bacterial meningitis is caused by one of three organisms, Haemophilus influenzae type b, Neisseria meningitidis, or Streptococcus pneumoniae. All three organisms may be transmitted through contact with respiratory droplets. These droplets are heavy and typically fall within 3 feet (91.4 cm) of the client. Droplet precautions require, in addition to standard (routine) precautions, that HCPs m wear masks when coming into close contact with the client.
Standard or routine precautions, previously referred to as universal precautions, are general measures used for all clients. Contact precautions are used when direct or indirect contact with the client causes disease transmission. Gowns and gloves are needed but not masks. Airborne precautions differ from droplet in that the particles are smaller and may stay suspended in the air for longer periods of time. These clients require nega- ' tive pressure rooms, and all health care workers must wear respirators.
Question 79.
A multidisciplinary team is updating rec-ommendations to reduce medication errors on the pediatric unit. Which strategy, if suggested by the team to reduce medication errors, would the nurse question?
(a) Increase the number of steps in the medication administration procedure.
(b) Avoid using parenteral syringes when administering liquid oral medications.
(c) Limit the size of IV fluid bags that can be hung on small children.
(d) Reduce the available concentrations or dose strengths of high-alert medications to the minimum.
Answer:
(a) Increase the number of steps in the medication administration procedure.
Explanation:
Any time steps are added to the medication administration process, there is one more place where an error might occur. Using only oral syringes to administer oral medications reduces the chance that the medication will be given intravenously. The use of smart pumps alone is not enough to prevent IV fluid administration.
An additional measure that pediatric floors can institute to prevent accidental fluid overload is to use smaller IV fluid bags, such as 250 mL. Whenever a medication comes in multiple concentrations and doses, there is risk of administering the wrong dose.
Question 80.
The health care provider (HCP) prescribes carbamazepine extended release for a client with a cerebral palsy who also has a seizure disorder. The client has a gastrostomy feeding tube, and carbamazepine is on the hospital’s “no crush” list. What should the nurse do in order to administer the medication?
(a) Cut the medication into four pieces.
(b) Dissolve the medication in 30 mL of juice.
(c) Ask the pharmacist for an oral suspension.
(d) Contact the HCP to change the prescription.
Answer:
(d) Contact the HCP to change the prescription.
Explanation:
The coating on an extended-release medication helps assure slow absorption of the medication. If the nurse crushes the medication, the medication may enter the client’s system too quickly and result in toxic levels. The only appropriate action is to contact the prescriber and ask that the prescription be changed.
Cutting the medication or trying to dissolve a whole tablet would have similar results as crushing it. Carbamazepine comes as an oral suspension, but it is not extended release. Therefore, a prescription would be needed to address dosing if switching to this form.
Question 81.
When making rounds on the pediatric neurology unit, the nurse manager notes that when giving IV medications many of the staff nurses are disconnecting the flush syringe first and then clamping the intermittent infusion device. The nurse is concerned that the nurses do not understand the benefits of positive pressure technique and turbulence flow flush in preventing clots. After the nurse manager discusses the problem with the staff educator, which intervention would be the most effective way to improve the nursing practice?
(a) Create a poster presentation on the topic with a required posttest.
(b) Send a group email discussing the importance of clamping the device first.
(c) Ask each nurse if he or she is aware that his or her practice is not current.
(d) Post an evidence-based article on the unit.
Answer:
(a) Create a poster presentation on the topic with a required posttest.
Explanation:
A poster presentation is an eye-catching way to disseminate information that can be used to educate nurses on all shifts. The addition of the posttest will verify that the poster information has been received. Because of the large volume of emails the typical employee receives, information sent this way might be overlooked. If several nurses are observed not using the most current practice, it is quite possible many more do not understand it. Thus, a larger-scale plan is needed. Posting an article will not assure that the information is read.
Question 82.
The emergency department nurse has admitted an infant with bulging fontanelles, setting sun eyes, and lethargy. Which diagnostic procedure would be contraindicated in this infant?
(a) lumbar puncture
(b) magnetic resonance imaging
(c) arterial blood draw
(d) computerized tomography scan
Answer:
(a) lumbar puncture
Explanation:
The child is exhibiting signs and symptoms of increased intracranial pressure (ICP). A lumbar puncture is contraindicated in children with increased ICP due to the risk of herniation. Magnetic resonance imaging and a computerized tomography scan are indicated in children with suspected increased ICP.
Radiology studies will allow visu-alization of the cause of the increased ICP, such as inflammation, a tumor, or hemorrhage. An arterial blood draw is not indicated in this client. However, there is no contraindication for performing an arterial blood draw on a child with increased ICP.
Question 83.
A 7-year-old with a history of tonic-clonic seizures has been actively seizing for 10 minutes. The child weighs 22 kg and currently has an IV of D5 NS + 20 mEq KC1/L running at 60 mL/h. The vital signs are temperature 100.4°F (38°C), heart rate 120 bpm, respiratory rate 28 breaths/min, and oxygen saturation 92%. Using the SBAR (situation- background-assessment-recommendation) technique for communication, the nurse calls the health care provider (HCP) with the recommendation for which medication?
(a) rectal diazepam
(b) IV lorazepam
(c) rectal acetaminophen
(d) IV fosphenytoin
Answer:
(d) IV fosphenytoin
Explanation:
IV lorazepam is the benzodiazepine of choice for treating prolonged seizure activity. IV benzodiazepines act to potentiate the action of the gamma-aminobutyric acid (GABA) neurotransmitter, stopping seizure activity. If an IV is not available, rectal diazepam is the benzodiazepine of choice.
The child has a low-grade fever, which is likely caused by excessive motor activity. The primary goal for the child is to stop the seizure to reduce neurologic damage. Benzodiazepines are used for the initial treatment of prolonged seizures. Once the seizure has ended, a loading dose of fosphenytoin is given.
Read More: