Some NCLEX PN Practice Questions involve analyzing data from laboratory reports, diagnostic tests, and client assessments.
NCLEX Gastrointestinal Disorders Questions - NCLEX Questions on Gastrointestinal Disorders
Gastrointestinal Disorders NCLEX Practice Questions
Question 1.
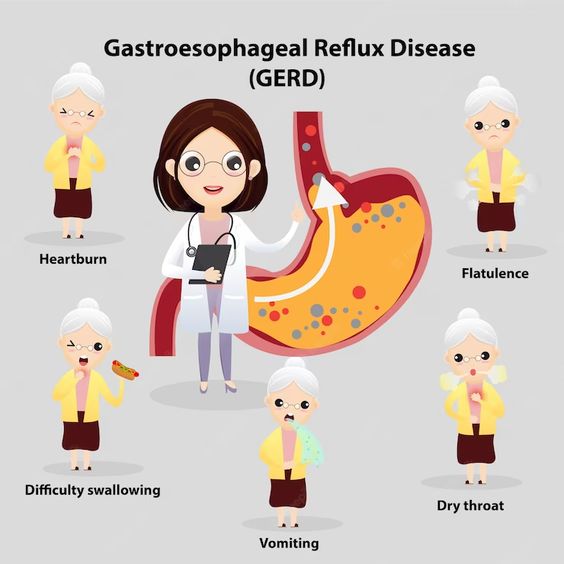
Ms. Alvin, a 60-year-old female with a history of hypertension, presents to the clinic with complaints of heartburn and acid reflux. Upon examination, the provider prescribes an antacid for her symptoms.
Aluminum compounds can cause while reducing the
effects of tetracyclines, warfarin sodium, and digoxin.
(a) Hypertension
(b) Hypophosphatemia
(c) Hypernatremia
(d) Constipation
(e) Acid rebound
(f) Diarrhea
Answer:
(b) Hypophosphatemia
Explanation:
Aluminum hydroxide is used to treat hyperphosphatemia, but it can also cause hypophosphatemia by reducing phosphate absorption. This medication should be used with caution in patients with renal impairment. Options (a) and (c) are incorrect because aluminum compounds do not contain significant amounts of sodium nor do they cause hypertension. Option (d) is a common side effect of aluminum compounds. Option (e) is a side effect of calcium compounds, not aluminum compounds. Option (f) is a side effect of magnesium compounds.
Question 2.
Mrs. Garcia has been diagnosed with hepatitis B. As her nurse, you are providing home care instructions. Which of the following statements by Mrs. Garcia indicate that she understands the instructions?
(a) "I can prepare food for my family as long as I wash my hands frequently."
(b) "I can drink alcohol in moderation and take Tylenol for my headache."
(c) "I should avoid close personal contact until my surface antigen test results are negative."
(d) "I don't need to inform my dentist about my hepatitis B diagnosis."
Answer:
(c) "I should avoid close personal contact until my surface antigen test results are negative."
Explanation:
Option (a) is incorrect because Mrs. Garcia should not prepare food for her family to prevent transmission of the virus. This is emphasized in the home care instructions that individual utensils, towels, toothbrushes, and razors must be labeled and used only by the client.
Option (b) is incorrect because Mrs. Garcia should avoid alcohol and over-the-counter medications, particularly acetaminophen and sedatives, because these medications are hepatotoxic.
Option (c) is correct because the client should avoid close personal contact such as kissing and sexual activity until her surface antigen test results are negative. This is also emphasized in the home care instructions.
Option (d) is incorrect because the client needs to inform other health professionals, such as medical or dental personnel, of the onset of hepatitis. This is also emphasized in the home care instructions. The client should carry a MedicAlert card noting the date of hepatitis onset and keep follow-up appointments with the health care provider.
Therefore, option (c) is the correct answer as it reflects the understanding of the home care instructions given to the client with hepatitis B.
Question 3.
Fill in the blanks:
Magnesium hydroxide is a ............... and its most prominent side effect is ..................
(a) Diuretic, diarrhea
(b) Antacid, constipation
(c) Laxative, diarrhea
(d) Antihistamine, dizziness
(e) Analgesic, headache
(f) Hypnotic, drowsiness
Answer:
(c) Laxative, diarrhea
Explanation:
Magnesium hydroxide is a saline laxative commonly used to relieve constipation. Its most prominent side effect is diarrhea. It is often administered in combination with aluminum hydroxide, an antacid that assists in preventing diarrhea. Options A, B, D, E, and F are incorrect because they do not describe the classification and side effect of magnesium compounds.
Question 4.
A 35-year-old female patient presents to the healthcare facility with complaints of abdominal pain and diarrhea. She was diagnosed with Crohn's disease in the past. On assessment, she reports fever, crampy and colicky pain after meals, diarrhea (semisolid) with mucus and pus, abdominal distention, anorexia, nausea, vomiting, weight loss, anemia, dehydration, electrolyte imbalances, and malnutrition. Which of the following interventions should the nurse prioritize for this patient?
Which of the following interventions should the nurse prioritize for the patient with Crohn's disease?
(a) Encourage a low-fiber diet
(b) Administer high-dose corticosteroids
(c) Provide parenteral nutrition
(d) Administer antidiarrheal medication
(e) Avoid surgery as long as possible
(f) Administer antibiotics
Answer:
(c) Provide parenteral nutrition
(e) Avoid surgery as long as possible
Explanation:
The nurse should prioritize providing parenteral nutrition (Option c) and avoiding surgery as long as possible (Option e) for the patient with Crohn's disease. This disease can lead to malnutrition due to malabsorption of nutrients, and it is important to provide adequate nutrition to the patient. Surgery is avoided for as long as possible because recurrence of the disease process in the same region is likely to occur.
Low-fiber diet (Option a) is not recommended for Crohn's disease as it can aggravate the condition. High-dose corticosteroids (Option b) may be used for acute exacerbations, but it is not the priority intervention in this case. Antidiarrheal medication (Option d) is not recommended for Crohn's disease as it can worsen the condition. Antibiotics (Option f) may be used to treat bacterial infections in patients with Crohn's disease but it is not the priority intervention in this case.
Note: It is important to provide education to the patient about their condition and how to manage it. The nurse should encourage the patient to follow a high-protein, high-calorie diet and drink plenty of fluids. The nurse should also monitor the patient's electrolyte levels and administer electrolyte replacement therapy as necessary.
Question 5.
A 35-year-old female patient presents to the healthcare facility with complaints of abdominal pain and diarrhea. She was diagnosed with Crohn's disease in the past. On assessment, she reports vomiting, fever, crampy and colicky pain after meals, diarrhea (semisolid) with mucus and pus and abdominal distention. Which of the following interventions should the nurse prioritize for this patient?
Which of the following interventions should the nurse prioritize for the patient with Crohn's disease?
(a) Encourage a low-fiber diet
(b) Administer high-dose corticosteroids
(c) Provide parenteral nutrition
(d) Administer antidiarrheal medication
(e) Avoid surgery as long as possible
(f) Administer antibiotics
Answer:
(c) Provide parenteral nutrition
(e) Avoid surgery as long as possible
Explanation:
The nurse should prioritize providing parenteral nutrition (Option c) and avoiding surgery as long as possible (Option e) for the patient with Crohn's disease. This disease can lead to malnutrition due to malabsorption of nutrients, and it is important to provide adequate nutrition to the patient. Surgery is avoided for as long as possible because recurrence of the disease process in the same region is likely to occur. Low-fiber diet (Option a) is not recommended for Crohn's disease as it can aggravate the condition.
High-dose corticosteroids (Option b) may be used for acute exacerbations, but it is not the priority intervention in this case. Antidiarrheal medication (Option D) is not recommended for Crohn's disease as it can worsen the condition. Antibiotics (Option f) may be used to treat bacterial infections in patients with Crohn's disease but it is not the priority intervention in this case.
It is important to provide education to the patient about their condition and how to manage it. The nurse should encourage the patient to follow a high-protein, high-calorie diet and drink plenty of fluids. The nurse should also monitor the patient's electrolyte levels and administer electrolyte replacement therapy as necessary.
Question 6.
A 45-year-old man presents to the emergency department with complaints of severe abdominal cramping and bloody diarrhea for the past 2 days. He also reports a low-grade fever and chills. He has a history of ulcerative colitis and has been experiencing frequent flare-ups in the past year. On examination, his abdomen is tender and there are hyperactive bowel sounds. His laboratory test results show anemia and leukocytosis.
What is the most likely diagnosis for this patient?
(a) Diverticulitis
(b) Irritable bowel syndrome
(c) Ulcerative colitis exacerbation
(d) Crohn's disease
Answer:
(c) Ulcerative colitis exacerbation
Explanation:
The patient's history of ulcerative colitis, along with his symptoms of bloody diarrhea, fever, and abdominal tenderness, are indicative of an exacerbation of his condition. Anemia and leukocytosis are common laboratory findings in ulcerative colitis.
Diverticulitis presents with left lower quadrant pain and fever, while irritable bowel syndrome is a functional disorder without inflammation. Crohn's disease typically presents with transmural inflammation that can involve any part of the digestive tract, while ulcerative colitis involves only the colon and rectum.
Question 7.
Saigrace is a 34-year-old man who is admitted to the hospital with a diagnosis of ulcerative colitis. His medical history includes asthma and seasonal allergies. He has a history of smoking, but has quit for the past year.
Which of the following is a characteristic of ulcerative colitis?
(a) It results in excessive absorption of nutrients
(b) It begins in the cecum and spreads downwards
(c) It causes loss of elasticity and inability to absorb nutrients
(d) It is not characterized by periods of remissions and exacerbations
Answer:
(c) It causes loss of elasticity and inability to absorb nutrients
Explanation:
Ulcerative colitis is an inflammatory disease that affects the colon and rectum. It causes inflammation, ulcers, and bleeding in the colon, leading to the development of scar tissue, which can result in a loss of elasticity and the ability to absorb nutrients. Option (a) is incorrect because ulcerative colitis results in poor absorption of nutrients, not excessive absoiption.
Option (b) is incorrect because ulcerative colitis commonly begins in the rectum and spreads upward toward the cecum, not the other way around. Option (d) is incorrect because ulcerative colitis is characterized by various periods of remissions and exacerbations.
Question 8.
A 52-year-old male patient presented to the clinic with complaints of severe diarrhea containing blood and mucus, malaise, abdominal tenderness, and cramping. He also reported significant weight loss and anorexia. The patient was diagnosed with ulcerative colitis, and the healthcare provider prescribed a combination of medications that included corticosteroids, salicylate compounds, and antidiarrheals.
Which of the following statements is true about ulcerative colitis?
(a) It is a disease that results in poor absorption of nutrients.
(b) It commonly begins in the cecum and spreads downward towards the rectum.
(c) It causes muscular hypertrophy, fat deposits, and fibrous tissue, with bowel thickening, shortening, and narrowing.
(d) It is characterized by various periods of remissions and exacerbations.
Answer:
(d) It is characterized by various periods of remissions and exacerbations.
Explanation:
Option (a) is incorrect because ulcerative colitis is not a disease that results in poor absoiption of nutrients. Rather, the colon becomes edematous and may develop bleeding lesions and ulcers, which may lead to perforation.
Option (b) is incorrect because ulcerative colitis commonly begins in the rectum and spreads upward towards the cecum, not the other way around.
Option (c) is incorrect because chronic ulcerative colitis causes muscular hypertrophy, fat deposits, and fibrous tissue, with bowel thickening, shortening, and narrowing, but not scar tissue development that causes loss of elasticity and loss of the ability to absorb nutrients.
Option (d) is the correct answer because ulcerative colitis is characterized by various periods of remissions and exacerbations. During remission, the patient may have few or no symptoms, while during an exacerbation, the patient may experience severe diarrhea containing blood and mucus, malaise, abdominal tenderness, and cramping, as well as significant weight loss and anorexia.
Question 9.
Ms. Alvin is a 26-year-old female who was admitted to the hospital with complaints of severe abdominal pain that began in the periumbilical area and has now localized to the right lower quadrant. She reports feeling nauseous and has vomited several times in the last 24 hours. The client has a low-grade fever and elevated white blood cell count. The healthcare provider suspects appendicitis.
Which of the following is the most common presenting symptom of appendicitis?
(a) Pain in the left lower quadrant
(b) Pain in the periumbilical area that descends to the right lower quadrant
(c) Abdominal pain that is most intense at the left lower quadrant
(d) Abdominal pain that is most intense at the right upper quadrant
Answer:
(b) Pain in the periumbilical area that descends to the right lower quadrant
Explanation:
The appendix is located in the lower right quadrant of the abdomen, and pain associated with appendicitis often begins in the periumbilical area and then localizes to the right lower quadrant. Pain in the left lower quadrant or the right upper quadrant is not associated with appendicitis.
Question 10.
Which of the following is a preoperative intervention for a client with appendicitis?
(a) Encouraging the client to eat a regular diet
(b) Applying heat to the abdomen
(c) Administering laxatives or enemas
(d) Administering antibiotics as prescribed
Answer:
(d) Administering antibiotics as prescribed is a preoperative intervention for a client with appendicitis.
Explanation:
Preoperative interventions for a client with appendicitis include maintaining NPO status, administering fluids intravenously to prevent dehydration, monitoring for signs of ruptured appendix and peritonitis, positioning the client in a right side-lying or low to semi-Fowler’s position to promote comfort, monitoring bowel sounds, applying ice packs to the abdomen if prescribed, and administering antibiotics as prescribed. Encouraging the client to eat a regular diet, applying heat to the abdomen, and administering laxatives or enemas are contraindicated in a client with appendicitis as they can cause the appendix to rupture, leading to peritonitis.
Question 11.
A 35-year-old female patient presents to the healthcare facility with complaints of abdominal pain and diarrhea. She was diagnosed with Crohn's disease in the past. On assessment, she reports . diarrhea (semisolid) with mucus and pus. fever, crampy and colicky pain after meals, abdominal distention, anorexia, nausea and vomiting. Which of the following interventions should the nurse prioritize for this patient?
Which of the following interventions should the nurse prioritize for the patient with Crohn's disease?
(a) Encourage a low-fiber diet
(b) Administer high-dose corticosteroids
(c) Provide parenteral nutrition
(d) Administer antidiarrheal medication
(e) Avoid surgery as long as possible
(f) Administer antibiotics
Answer:
(c) Provide parenteral nutrition
(e) Avoid surgery as long as possible
Explanation:
The nurse should prioritize providing parenteral nutrition (Option c) and avoiding surgery as long as possible (Option e) for the patient with Crohn's disease. Crohn's disease can cause malnutrition due to malabsorption of nutrients, and parenteral nutrition can help provide the patient with the necessary nutrients to support their recovery. Surgery is avoided for as long as possible because recurrence of the disease process in the same region is likely to occur. Research has shown that early initiation of parenteral nutrition can improve clinical outcomes in patients with Crohn's disease.
A low-fiber diet (Option a) is not recommended for Crohn's disease as it can aggravate the condition. A high-fiber diet may be beneficial for some patients with Crohn's disease, but it is not appropriate for all patients. Therefore, it is important to individualize dietary recommendations based on the patient's specific needs and symptoms.
High-dose corticosteroids (Option b) may be used for acute exacerbations of Crohn's disease, but it is not the priority intervention in this case. Corticosteroids have numerous side effects, including increased risk of infection, osteoporosis, and hypertension, and therefore should only be used when necessary and under close supervision.
Antidiarrheal medication (Option d) is not recommended for Crohn's disease as it can worsen the condition. These medications can cause toxic megacolon and bowel perforation, particularly in patients with active inflammation or strictures.
Antibiotics (Option f) may be used to treat bacterial infections in patients with Crohn's disease but it is not the priority intervention in this case. Antibiotics should be used judiciously and only when necessary to avoid the development of antibiotic resistance.
It is important to provide education to the patient about their condition and how to manage it. The nurse should encourage the patient to follow a high-protein, high-calorie diet and drink plenty of fluids. The nurse should also monitor the patient's electrolyte levels and administer electrolyte replacement therapy as necessary, as electrolyte imbalances can occur in patients with Crohn's disease due to diarrhea and malabsorption.
Question 12.
Traditional gastrostomy has been scheduled for a patient, and preoperative teaching has been completed. The patient and family verbalize understanding. What is the best action by the nurse?
(a) Arrange a tour of the ICU
(b) Assess patient’s psychosocial status
(c) Document the patient teaching and response
(d) Have the patient begin nutritional supplements
Answer:
(b) Assess patient’s psychosocial status
Explanation:
A percutaneous endoscopic gastrostomy (PEG) is a safe and effective way to provide food, liquids, and medications (when appropriate) directly into the stomach. The gastrostomy procedure is performed to create a new opening to the stomach through the abdominal wall, for a feeding tube. It is a long and difficult procedure, and afterwards, the patient’s normal nutritional and eating habits will be changed.
The pre-operative teaching can cause the patient to be anxious. Psychosocial status should be assessed by the nurse to help further prepare the patient and family for the procedure. Worries about feeding supplies, home setup, and care of the gastrostomy tube should be addressed pre-op, if possible. The nurse can consult with home care services or a nutritionist to help alleviate anxiety about the upcoming change in daily life.
Rationale:
(a) is incorrect because the patient should be offered a tour after psychosocial needs have been addressed. A tour may actually increase anxiety about the procedure, so the nurse should not offer this until after anxiety level has been determined.
(c) is incorrect because documentation should be performed after psychosocial issues have been assessed and addressed. Documentation never takes priority over patient care.
(d) is incorrect because nutritional supplements may be started before the procedure, but the nurse must first determine when the patient is going to the OR. The patient must be NPO prior to the start of the procedure.
Question 13.
A patient is admitted to the surgical unit following open Nissen fundoplication. An indwelling urinary catheter, two peripheral IVs, and nasogastric (NG) tube are in place. The nurse connects the NG tube to low intermittent wall suction. The nurse notes bright red blood in the suction canister from the NG tube. What is the first action the nurse should take?
(a) Document in the patient’s chart
(b) Immediately notify the surgeon
(c) Measure the drainage, empty the canister, and reassess the drainage in one hour
(d) Obtain vital signs
Answer:
(d) Obtain vital signs
Explanation:
A Nissen fundoplication is a laparoscopic procedure performed to treat hiatal hernia and gastroesophageal reflux disease (GERD). Drainage from the NG tube following the procedure should be brown, indicating normal GI contents or old blood.
Bright red blood in the suction canister and NG tube indicates active bleeding, which is an abnormal finding. The nurse should obtain a full set of vital signs to identify signs of shock. Hypotension and tachycardia are indications of shock. Vitals should be reassessed frequently to determine if BP is dropping. The nurse should be prepared to increase the IV fluid rate.
Rationale:
(a) is incorrect because documentation should be completed after patient care has been completed. It is negligent to document before assessing and treating the symptom, which indicate a GI bleed.
(b) is incorrect because the surgeon should be notified immediately after vital signs are obtained. Vital signs are pieces of data that the nurse can collect quickly at the bedside, and this is information which the surgeon will want to know.
(c) is incorrect because obtaining vital signs should be the first action. Waiting an hour to re¬assess is doing nothing for the current problem and could delay emergency treatment.
Question 14.
The nurse is caring for a patient on the medical-surgical unit who had a Zenker’s diverticulum removed yesterday. The patient’s NG tube, which is set to low intermittent suction, has had no drainage for the past four hours. The surgeon did not leave specific orders for the NG tube. What is the most appropriate action by the nurse?
(a) Reposition the patient for comfort and document the findings
(b) Irrigate NG tube with 20 mL normal saline
(c) Notify the surgeon
(d) Remove the NG tube and insert a new one
Answer:
(c) Notify the surgeon
Explanation:
Zenker’s diverticula (also known as “false diverticula”) occur in the hypopharynx, usually in elderly patients, as the result of esophageal mucosa herniation. The result is an outpouching of the posterior pharyngeal wall, just above the esophagus, and can lead to dysphagia, regurgitation, and aspiration. The patient will be NPO postoperatively for several days, or until swallowing has been re-established.
The surgically placed NG tube should be draining small amounts of gastric juice, green-to-brown in color with a low pH. The nurse should not advance, withdraw or manipulate the tube in any way. Irrigation should not be performed without specific direction from the healthcare provider. The surgeon needs to be notified about the absence of drainage.
Rationale:
(a) is incorrect because the absence of drainage is an abnormal finding which must be addressed ahead of documentation. Repositioning the patient may help facilitate drainage, but notifying the surgeon is the priority'. The question does not state that the patient is in discomfort.
(b) is incorrect because surgically placed NG tubes should not be irrigated without an order from the surgeon.
(d) is incorrect because the patient needs temporary gastric decompression while healing from the surgery and removing the NG tube will require a new one to be placed, which can be traumatic to the patient. Surgically-placed NG tubes should not be removed without an order from the surgeon.
Question 15.
A patient in the emergency department has esophageal trauma. Subcutaneous emphysema with crepitus in the mediastinal area up to the lower part of the neck is palpated by the nurse. What is the priority action the nurse should take?
(a) Assess oxygenation status
(b) Order a STAT chest X-ray
(c) Prepare patient for surgery immediately
(d) Start a large-bore peripheral IV
Answer:
(a) Assess oxygenation status
Explanation:
Subcutaneous emphysema indicates air has leaked under the skin. This can occur from a ruptured esophagus. Airway is priority in this patient. Oxygenation status needs to be assessed by the nurse before any diagnostic procedure. Vomiting, chest pain, and subcutaneous emphysema are the “Macklers’s triad” of symptoms that indicate esophageal perforation.
Rationale:
(b) is incorrect because before ordering a chest X-ray (and while awaiting the X-ray), the nurse is responsible for assessing the respiratory system and intervening if the patient is not oxygenating well.
(c) is incorrect because oxygenation status must be assessed first. If the patient’s airway is not patent with equal breath sounds bilaterally, the nurse will perform emergency interventions before preparing for surgery.
(d) is incorrect because the patient needs IV access, but respiratory concerns take priority over fluid replacement in this patient who is demonstrating an airway issue.
Question 16.
When caring for a patient with a nasogastric (NG) tube, what action by the nursing student requires intervention by the registered nurse?
(a) Checking NG tube placement every four hours
(b) Monitoring NG tube drainage and documenting
(c) Pinning the tube snug to the patient gown, with the head in the midline position
(d) Providing oral care every four hours
Answer:
(c) Pinning the tube snug to the patient gown, with the head in the midline position
Explanation:
The NG tube should be pinned to the patient gown, but the patient should be able to turn their head without pulling on the NG tube. Pinning the tube without enough slack will risk withdrawal of the tube when the patient changes position or turns their head from side-to- side.
Rationale:
(a) is incorrect because checking NG tube placement every four hours is appropriate. Checking placement can be done by measuring the tube and comparing to the previously documented measurement or by checking pH of NG tube contents.
(b) is incorrect because monitoring and documenting NG tube drainage is appropriate and these actions are within the scope of practice of a nursing student.
(d) is incorrect because providing oral care every four hours is appropriate for a patient with a NG tube in place.
Question 17.
A Nissen fundoplication with nasogastric (NG) tube placement was performed on a patient the previous day. During rounds, the nurse finds the patient vomiting bright red blood, and the NG tube is on the bed. What is the first action the nurse should take?
(a) Notify the surgeon
(b) Don gloves
(c) Reinsert NG tube
(d) Obtain vital signs
Answer:
(b) Don gloves
Explanation:
A Nissen fundoplication is a laparoscopic procedure performed to treat hiatal hernia and gastroesophageal reflux disease (GERD). The nurse must put on a pair of clean gloves first, to prevent exposure to the blood. The nurse should remain at the bedside, facilitate proper positioning to prevent aspiration of the vomit, and suction as necessary. Vital signs should be obtained and oxygen applied if necessary.
Rationale:
(a) is incorrect because notifying the surgeon is appropriate but not the first action. The nurse must stay with the patient and delegate to another member of the nursing team to notify the surgeon.
(c) is incorrect because a NG tube that was placed in surgery should not be replaced at the bedside by the nurse. Furthermore, the nurse does not insert an NG tube into a patient who is actively vomiting. The insertion could cause aspiration of the vomit, leading to further complications. The vomiting must be controlled before a new tube is inserted.
(d) is incorrect because obtaining vital signs is priority, but the nurse must be protected by wearing gloves before coming into contact with blood or any other bodily fluid.
Question 18.
A patient is admitted to the medical-surgical unit for peptic ulcer disease. The patient calls the nurse to report sharp abdominal pain that started suddenly. When the nurse palpates the abdomen, it is rigid and tense. What is the priority action by the nurse?
(a) Administer pain medication
(b) Notify the healthcare provider
(c) Percuss the abdominal quadrants
(d) Obtain vital signs
Answer:
(b) Notify the healthcare provider
Explanation:
Peptic ulcer disease is manifested by erosion of the lining of the stomach and duodenum due to overproduction of hydrochloric acid. Other causes include excessive alcohol consumption, severe stress, NSAID and corticosteroid use, and H. pylori infection. This patient has several signs and symptoms of a perforated ulcer, which include severe epigastric pain spreading across the abdomen, with abdominal rigidity, hyperactive-diminished bowel sounds, and rebound tenderness. The healthcare provider must be notified immediately for medical attention.
Rationale:
(a) is incorrect because treatment of pain does not take priority over other actual physical problems. Oral medications, especially, should not be administered in case NPO status is required for surgery. Opiates should be withheld until the nurse determines if a surgical consent needs to be signed.
(c) is incorrect because further assessing the abdomen (percussion) is not priority at this time. The nurse has enough assessment to call the healthcare provider.
(d) is incorrect because vital signs will not initially give vital information about a perforated ulcer.
Question 19.
A patient is in the emergency department reporting pain from peptic ulcer disease that has worsened over the last few days. Blood pressure when supine was 122/80 mmHg and 98/52 mm Hg upon standing. What is the most appropriate action by the nurse?
(a) Administration of ibuprofen
(b) Notify the rapid response team
(c) Start an IV and administer normal saline
(d) Keep the patient on bedrest
Answer:
(c) Start an IV and administer normal saline
Explanation:
The patient is displaying signs of dehydration or fluid volume loss with the orthostatic changes in blood pressure. The patient needs an IV and isotonic solution, or normal saline, to replace the fluid lost.
Rationale:
(a) is incorrect because NSAID medications, such as ibuprofen, should be avoided in a patient with peptic ulcer disease. Generally, H2-receptor antagonists and proton pump inhibitors can be administered to alleviate the pain associated with peptic ulcer disease.
(b) is incorrect because the rapid response team is not necessary for orthostatic hypotension. The nurse should first administer fluids and reassess to determine if the BP stabilizes in response to fluid replacement.
(d) is incorrect because the patient should be put on bedrest, but this nursing action does not address the fluid deficit or the blood pressure.
Question 20.
A patient is being taught by the nurse about medications for Helicobacter pylori infection. What is the most question for the nurse to ask?
(a) “How much alcohol do you consume each week?”
(b) “Do you have a family history of H. pylori infection?”
(c) “Do you use nicotine patches?”
(d) “Do you think you will be able to take several medications daily?”
Answer:
(d) “Do you think you will be able to take several medications daily?”
Explanation:
H. pylori infection is treated with a combination of several drugs, so it can be difficult to adhere to the drug therapy. The nurse needs to assess the patient’s ability and willingness to adhere to the treatment program. Drugs to treat H. pylori include metronidazole (usually used along with another antibiotic), an H2-receptor antagonist such as cimetidine (blocks acid production), and bismuth subsalicylate, which coats the ulcer and protects from stomach acid.
Rationale:
(a) is incorrect because although alcohol can worsen peptic ulcer disease, alcohol consumption is not directly related to teaching the patient about medications.
(b) is incorrect because personal or family history of H. pylori infection history is not more important than determining compliance with treatment regimen. This information is also unrelated to teaching about medications.
(c) is incorrect because although nicotine and tobacco smoke can increase gastric acid production, this is not the most important thing to address.
Question 21.
Esomeprazole has been prescribed for chronic gastric ulcers in a 55-year-old female patient. What is particularly important for the nurse to teach this patient?
(a) Ask the pharmacist about taking other medications
(b) Increase calcium and vitamin D intake
(c) Notify healthcare provider of worsening symptoms
(d) Medication must be taken each morning
Answer:
(b) Increase calcium and vitamin D intake
Explanation:
Chronic gastric ulcers are commonly caused by overproduction of gastric acid, which is improved with the use of a proton-pump inhibitor (PPI) such as esomeprazole. Long term use of this medication has been shown to lead to osteoporosis and fractures, so the patient should be taught to increase calcium and vitamin D intake at the start of the medication therapy.
Rationale:
(a) is incorrect because esomeprazole does not commonly interact with other medications.
(c) is incorrect because notifying the healthcare provider of worsening symptoms is generally appropriate but not specific to esomeprazole.
(d) is incorrect because esomeprazole is taken at night to prevent nocturnal acid production.
Question 22.
The nurse responds to a patient’s call light and finds them in the bathroom. The patient has vomited a large amount of bright red blood. After applying gloves, what is the first action the nurse should take?
(a) Assist patient back to the bed
(b) Immediately notify the healthcare provider
(c) Measure the bloody vomit
(d) Obtain vital signs
Answer:
(a) Assist patient back to the bed
Explanation:
After donning gloves to protect the nurse from exposure to the blood, the priority action is to safely assist the patient back to bed, where the nurse can further assess them.
Rationale:
(b) is incorrect because notifying the healthcare provider is appropriate, but this can be delegated to another member of the nursing team. The patient who has vomited blood is unstable, and the nurse should stay with the patient.
(c) is incorrect because assisting the patient to bed is a safety measure that takes priority. After the patient has been assessed and appropriate nursing interventions have been performed, the vomit can be measured, documented, and cleaned up. Furthermore, this action can be delegated to a UAP.
(d) is incorrect because if the patient is internally bleeding, he may be hypotensive and light¬headed and at risk for a fall. Obtaining vital signs is appropriate after the patient is safely back in bed.
Question 23.
The nurse cares for a patient with upper gastrointestinal hemorrhage and a nasogastric (NG) tube in place. The blood pressure has been dropping, and a l liter bolus of 0.9% NS requires comfort measures. Which comfort measure may be delegated to the unlicensed assistive personnel (UAP) by the nurse?
(a) Lavage NG tube with cold water
(b) Frequent oral care
(c) Reposition NG tube every four hours
(d) Obtaining frequent vital signs
Answer:
(b) Frequent oral care
Explanation:
Oral care is important to perform for the patient with an NG tube for comfort and infection prevention. This is a standard task that can be delegated to the UAP. In order for a task to be delegated to the UAP, it must frequently recur in the daily care of patients, be performed according to an established sequence of steps, and involve little or no modification from one patient situation to another. Tasks that are performed with a predictable outcome and do not inherently involve ongoing assessment, interpretation, or decision-making, and do not endanger a patient’s life or well-being, are able to be delegated to the UAP.
Rationale:
(a) is incorrect because lavage of the NG tube is not within the scope of practice of a UAP. Lavage is performed by the nurse because it requires judgment about type and amount of fluid used, amount of force to use when injecting the fluid, and evaluating for patient response.
(c) is incorrect because repositioning of the NG tube is not typically required and is not within the scope of practice of a UAP. If needed, repositioning requires consultation with the healthcare provider and will be performed by the nurse.
(d) is incorrect because vital signs can be delegated to the UAP, but this is not a comfort measure.
Question 24.
The nurse is caring for a female patient diagnosed with gastric cancer. Before sending the patient to the preoperative area for a total gastrectomy procedure, which of the following lab values would the nurse report to the surgeon immediately?
(a) Albumin 2.3 g/dL
(b) Hematocrit 31%
(c) Hemoglobin 9.2 mg/dL
(d) International normalized ratio (INR) 4.3
Answer:
(d) International normalized ratio (INR) 4.3
Explanation:
INR is a measure of bleeding time and is routinely checked for patients taking warfarin. Normal INR is 1.0. This patient’s level is elevated, which indicates bleeding risk. The surgeon should be notified of this result immediately because of the increased risk for bleeding during the procedure. The patient may need vitamin K supplementation or the procedure postponed until the INR is normalized.
Rationale:
(a) is incorrect because a decreased albumin level is expected with gastric cancer. Protein digestion begins in the stomach and continues in the small intestine, so in patients with gastric cancer it is common to have decreased protein levels. Normal serum albumin is 3.5-5-5 g/dL.
(b) and (c) are incorrect because these are expected findings in a patient with stomach cancer. Ulcers and cancers of the esophagus, stomach or intestines are some of the most serious causes of chronic gastrointestinal blood loss, leading to decreased hemoglobin and hematocrit. Normal hemoglobin for a male is 13-18 g/dl, normal for a female is 12-16 g/dl, normal for a child aged 3-12 is 11-12.5 g/dl. Hematocrit measures percentage of red blood cells per fluid volume of blood. Normal hematocrit is 42-52% for men, 35-47% for women, and 35-45% for children.
Question 25.
The clinic nurse cares for a male, 63-year-old patient with a history of type II diabetes, stomach cancer, and hypercholesterolemia. He has just been informed that his stomach cancer has returned and he is very upset. Vitals are BP 125/74, pulse 88, RR 14, and Sp02 97%. What is the most appropriate response by the nurse?
(a) “Who do you have for support?”
(b) “Tell me what you’re feeling.”
(c) “We knew this might happen.”
(d) “Would you like a referral to hospice?”
Answer:
(b) “Tell me what you’re feeling.”
Explanation:
The patient’s vital signs are normal, so the nurse should focus on how upset the patient is. Asking the patient about his feelings is therapeutic and demonstrates willingness to listen to concerns. This is an open-ended question which will facilitate the nurse-patient relationship and help determine the patient’s emotional state. Once rapport is established, the nurse can then help the patient to understand treatment options and offer reassurance, as appropriate. (The history of diabetes and hypercholesterolemia are unrelated to the current situation.)
Rationale:
(a) is incorrect because the nurse should first help the patient identify his feelings related to his diagnosis. Open-ended communication about how the patient is currently feeling focuses on the patient and will help the nurse help the patient. Asking about others who can support the patient can be done after establishing rapport.
(c) is incorrect because this nursing response dismisses the patient’s feelings.
(d) is incorrect because it is a yes/no question, which is non-therapeutic. The patient may not need hospice care yet.
Question 26.
The nurse is caring for a 71-year-old female patient who is recovering from a partial gastrectomy due to stomach cancer. The patient has had six loose stools in the past 12 hours. Which action by the nurse is best, initially, for this patient?
(a) Dietary consult arrangement
(b) Encourage the patient to drink 8 oz of fluid with three meals daily
(c) Offer tea and coffee between meals to replenish fluid lost from diarrhea
(d) Encourage the patient to lie down after meals
Answer:
(d) Encourage the patient to lie down after meals
Explanation:
Dumping syndrome commonly occurs after surgery to the stomach that causes foods to move from the stomach, through the small intestine, and through the colon rapidly, causing frequent diarrhea. Nutrients are not properly absorbed, as the contents of the GI tract are moved through too quickly. This can lead to malnutrition and dehydration. Other symptoms such as fatigue, sweating, fainting, mental confusion, and tachycardia may be present. Gravity facilitates movement through the GI system, so lying down after meals can slow this process and promote more absorption. Other instructions include avoiding sugary foods and limiting fiber.
Rationale:
(a) is incorrect because the nurse should implement specific nursing interventions ahead of consulting another service.
(b) is incorrect because the patient experiencing dumping syndrome should be encouraged to eat six small meals daily. PO fluids should not be consumed with meals because fluids increase speed of movement through the GI system. The patient should consume fluids between meals to meet daily fluid needs to prevent dehydration.
(c) is incorrect because caffeine is a stimulant which speeds movement through the GI tract. Caffeine should be avoided in a patient with dumping syndrome.
Question 27.
A 78-year-old female client is scheduled for partial gastrectomy for cancer. The family requests the patient not be informed of the diagnosis. What is the best action by the nurse?
(a) Ask family why they feel the patient shouldn’t be informed
(b) Assess the family’s concerns and fears
(c) Refuse to follow family’s wishes
(d) Inform the family the patient must be notified of her diagnosis.
Answer:
(b) Assess the family’s concerns and fears
Explanation:
The nurse must assess the family’s concerns and fears using open-ended questions for therapeutic communication. The Self-determination Act is a federal law requiring health care facilities to provide written information to adult patients about their rights to make health care decisions. Generally, the patient has a right to know their diagnosis and the plan of treatment.
Rationale:
(a) is incorrect because “why” questions are not therapeutic. Asking “why?” leads people to feel they need to defend themselves. The nurse should ask open-ended questions that encourage discussion, without the use of the word “why?”
(c) is incorrect because refusing to follow family’s wishes does not help foster the nurse’s relationship with the family and does not promote trust.
(d) is incorrect because telling the patient against their wishes will not help the nurse’s relationship with the family. If the patient is alert and oriented, and able to understand spoken language, she will have the legal right to know her diagnosis, but it is better, first, to further address the family’s concerns in a therapeutic way. The nurse must determine if the family feels the patient is psychologically unstable or at risk of harming herself. It is also important for the nurse to determine of the family has durable power of attorney or guardianship if the patient is mentally incapacitated.
Question 28.
The nurse is teaching a patient with a new diagnosis of irritable bowel syndrome (IBS) about dietary choices. Which of the following menu selections demonstrates the patient understands the instructions?
(a) Ham on white bread, applesauce, diet ginger ale
(b) Baked chicken, brown rice, steamed cauliflower, apple juice
(c) Grilled cheese, banana, hot tea
(d) Baked tilapia, green beans, coffee with milk
Answer:
(b) Baked chicken, brown rice, steamed cauliflower, apple juice
Explanation:
Irritable bowel syndrome (IBS) is a gastrointestinal (GI) disorder that causes a cluster of symptoms in adults and children including abdominal pain, bloating, cramping, diarrhea, gas, and altered bowel habits (constipation, diarrhea, or both). This is a functional disorder; the problem is related to motility, not damage to the actual organs of the GI system.
Patients with this diagnosis should consume high levels of fiber (30-40 g per day) and plenty of fluids. Soda should be avoided, and the patient should consume smaller meals. The menu choice with the highest amount of fiber is baked chicken, brown rice, cauliflower, and apple juice (brown rice and cauliflower contain high amounts of fiber).
Rationale:
(a) is incorrect because only the applesauce is high fiber. Ham on white bread does not have a high amount of fiber, and soda should be avoided with IBS. Artificial sweeteners, as contained in diet soda, and high-fructose corn syrup, which is often found in regular soda, can both irritate the bowel of a patient with IBS.
(c) is incorrect because only the banana has high fiber. The grilled cheese sandwich menu selection should specify “on whole wheat bread” for added fiber.
(d) is incorrect because tilapia and green beans do not have a high amount of fiber. Caffeinated beverages, such as coffee, and milk products can cause worsened symptom in IBS.
Question 29.
A female patient with a history of severe irritable bowel syndrome (IBS) comes to the clinic. She has been taking alosetron, as prescribed, since her last visit, six weeks ago. She reports feeling depressed and anxious about her bowel habits. What is an important question the nurse should ask the patient?
(a) “Have you had any constipation?”
(b) “Have you been getting enough fiber and fluids?”
(c) “Would you like to talk to the healthcare provider about an order for fluvoxamine?”
(d) “Have you experienced hypertension?”
Answer:
(a) “Have you had any constipation?”
Explanation:
Alosetron is indicated only for women with severe diarrhea-predominant irritable bowel syndrome (IBS) who have not responded to conventional treatment. A side effect is constipation, which can lead to complications such as ischemic colitis and mesenteric ischemia (both are life-threatening). The patient should be assessed for any constipation and if present, the health care provider should be notified, and the medication should be withheld.
Rationale:
(b) is incorrect because fiber and fluid intake are beneficial for someone with severe IBS, but determining if the patient has experienced any constipation is most important with alosetron.
(c) is incorrect because fluvoxamine (SSRI) is contraindicated with alosetron and this medication should not be ordered for the patient.
(d) is incorrect because alosetron does not cause or treat hypertension, so this is an irrelevant assessment.
Question 30.
The nurse is caring for a male, 49-year-old patient with a femoral hernia and a history of type II diabetes. The patient is not a candidate for hernia repair surgery. The nurse teaches the patient about the use of a truss pad. Which patient statement demonstrates more teaching is needed?
(a) “I will put the truss on when I go to bed every night.”
(b) “I will put on powder under the truss to prevent skin irritation.”
(c) “Because I am unable to have surgical repair, the truss will help the hernia.”
(d) “I will notify the healthcare provider of abdominal pain.”
Answer:
(a) “I will put the truss on when I go to bed every night.”
Explanation:
A truss is a support garment that holds the intestine in place to lessen protrusion of a hernia. The truss should be put on before getting out of bed in the morning and worn throughout the day. The patient’s statement indicated poor understanding of the need to wear the truss during the day.
Rationale:
(b) is incorrect because powder can be used under the truss, indicating correct understanding.
(c) is incorrect because the truss is used in place of surgery, indicating correct understanding.
(d) is incorrect because the healthcare provider should be notified of abdominal pain, indicating correct understanding.
Question 31.
The nurse cares for a male 68-year-old patient who is post op day l from hemorrhoidectomy. The nurse assesses the patient at shift change and notes lower abdominal distension that is dull to percussion. Which action should be taken by the nurse?
(a) Assess vital signs
(b) Determine last urinary void by the patient
(c) Ask if the patient has passed gas since the surgery
(d) Auscultate the abdomen
Answer:
(b) Determine last urinary void by the patient
Explanation:
Lower abdominal distension that is dull to percussion is indicative of a full bladder. Urinary retention is common postoperatively, so the nurse must determine the last time the patient avoided. The patient should be encouraged to void, and if unable, straight catheterization may be needed.
Rationale:
(a) is incorrect because vital signs will not give significant information related to bladder fullness or urinary retention.
(c) is incorrect because presence of flatus is not related to bladder function. Assessment of flatus (and bowel sounds) is necessary to determine of the patient is ready to have his diet advanced.
(d) is incorrect because auscultation of the abdomen is not the most important action. The correct sequence for abdominal assessment is inspection and auscultation, followed by palpation and then percussion (IAPP). The auscultation should have been completed before the nurse percussed the abdomen.
Question 32.
A nurse at the community health center is assessing clients. Which client is at highest risk for developing colorectal cancer?
(a) 35-year-old female who drink five cups of coffee per day, exercises six times per week, and has a history of melanoma
(b) 45-year-old male with irritable bowel syndrome, eats five servings of vegetables daily, consumes one glass of red wine daily
(c) 64-year-old Asian American male who works 60 hours/week
(d) 64-year-old Native American female who frequently eats fast food
Answer:
(d) 64-year-old Native American female who frequently eats fast food
Explanation:
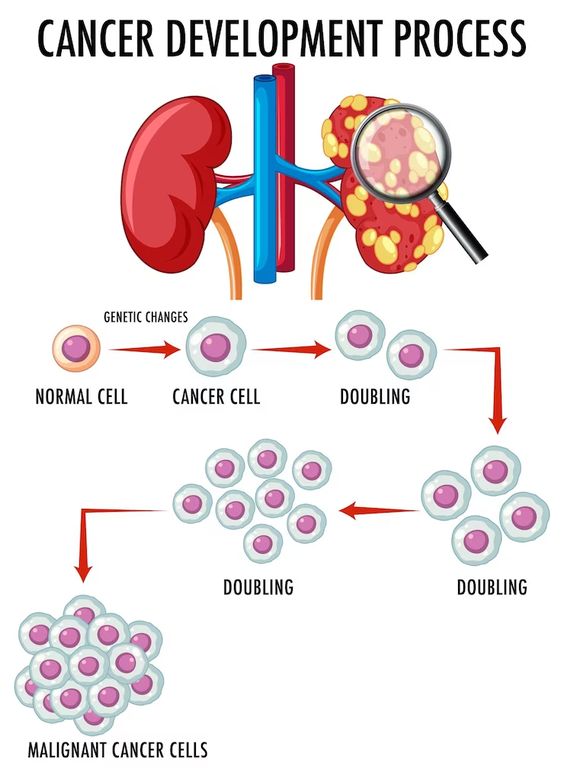
This patient has two risk factors: age over 50 and diet. Modifiable risk factors for colorectal (colon) cancer include being overweight (or obese), smoking, physical inactivity, diet high in red meat or processed meats, low-fiber/high-fat diet, and heavy alcohol use. Non-modifiable risk factors include personal history of type II diabetes, colorectal polyps, colorectal cancer, or inflammatory bowel disease (Crohn’s disease or ulcerative colitis).
Age over 50 and family history of colorectal cancer are also risk factors. Racial and ethnic background also affects one’s risk: African Americans have the highest colorectal cancer incidence and mortality rates of all racial groups in the United States. Jews of Eastern European descent (Ashkenazi Jews) have one of the highest colorectal cancer risks of any ethnic group in the world.
Rationale:
(a) is incorrect because this patient has no risk factors. Neither coffee intake nor caffeine increases colorectal cancer risk. Regular physical exercise actually reduces the risk for colon cancer. Melanoma does not increase one’s risk for colorectal cancer.
(b) is incorrect because this patient has no significant risk factors for colorectal cancer.
(c) is incorrect because this patient has one risk factor: age over 50. Working overtime does not increase colorectal cancer risk. Asian Americans are not at higher risk than other ethnic groups.
Question 33.
The nurse is assessing a 59-year-old male patient admitted to the surgical unit with colorectal cancer. The patient has a history of urinary tract infections. The nurse notes high- pitched bowel sounds and visible peristaltic waves when inspecting the patient’s abdomen. Which of the following actions should be taken by the nurse?
(a) Ask the patient if he is experiencing any right shoulder pain
(b) Assess the patient’s rectum for polyps
(c) Contact the healthcare provider and request a computed tomography scan
(d) Administer a laxative to increase movement of the bowel
Answer:
(c) Contact the healthcare provider and request a computed tomography scan
Explanation:
High-pitched bowel sounds and visible peristaltic waves indicate partial obstruction of the bowel which can be a result of colorectal cancer. The healthcare provider should be contacted so computed tomography can be performed to diagnose the obstruction.
Rationale:
(a) is incorrect because right shoulder pain (referred pain) is associated with peritonitis and cholecystitis. Referred pain in the upper thorax muscles is seen in patients with inflammation of organs in the abdominal cavity.
(b) is incorrect because an internal rectal examination to assess for polyps is not within the scope of practice of the registered nurse.
(d) is incorrect because laxatives are not indicated until after the obstruction has been verified and the healthcare provider determines whether or not surgery is needed.
Question 34.
The nurse cares for patients on the medical unit. The 6i-year-old, male patient, who has just been informed of his diagnosis of colon cancer, says to the nurse, “Please tell my visitors that I don’t want any company today.” Which action should the nurse take?
(a) Contact the healthcare provider and request a psychiatric consult
(b) Ask the patient about feelings related to the new colon cancer diagnosis
(c) Provide education regarding treatment options
(d) Encourage friends and family to visit and provide support
Answer:
(b) Ask the patient about feelings related to the new colon cancer diagnosis
Explanation:
A new diagnosis of cancer of any type can be detrimental to a patient. Initially, the patient may experience denial and depression related to the diagnosis. The patient should be encouraged to verbalize these feelings so the nurse can assist with moving through the grief stages. Note: Kubler-Ross’s stages of grief are as follows: denial, anger, bargaining, depression, and acceptance. However, not all patients experience these stages in this particular order.
Rationale:
(a) is incorrect because psychiatric consult may be needed, but the nurse should focus on the patient in the here and now, first. The nurse should always attempt to do something for the patient, ahead of “passing-the-buck” to another member of the professional team.
(c) is incorrect because discussion of the patient’s feelings should occur before treatment options are presented. The healthcare provider (not the nurse) is responsible for offering treatment options. Furthermore, providing education before the patient is ready avoids discussing the patient’s feelings.
(d) is incorrect because the nurse should focus on the patient’s concerns. Inviting visitors to see the patient, against the patient’s wishes, may cause the patient to lose trust in the nurse. The patient has already stated that no visitors are wanted. It is more important to focus on the nurse-patient communication at this time.
Question 35.
A patient with colon cancer has recently had a colostomy placed. The patient says, "I would like to speak with someone with a similar experience. I think it would help me." What is the best response by the nurse?
(a) “My neighbor has a colostomy and would probably be willing.”
(b) “The enterostomal therapist should be able to answer your questions.”
(c) “I can refer you to the United Ostomy Associations of America.”
(d) “Most people who have colostomies don’t talk about them because it is such a private matter.”
Answer:
(c) “I can refer you to the United Ostomy Associations of America.”
Explanation:
Nurses can better help patients if they knowr about community-based resources. The United Ostomy Associations of America (ostomy.org) has local chapters with resources. Arrangements can be made to have visitors who have experienced similar surgical procedures for ostomy placement talk to the patient.
Rationale:
(a) is incorrect because the nurse should not use a personal contact to speak with a patient. It is important for the nurse to keep professional and personal life separate.
(b) is incorrect because the enterostomal therapist may be an expert in stoma care, but the patient is asking to speak to someone with a colostomy. The nurse should meet the patient’s needs by connecting the patient with someone who has had a similar medical experience.
(d) is incorrect because the statement dismisses the patient’s concern.
Question 36.
The nurse is caring for a patient in the emergency room after a motor vehicle accident. When performing the initial physical assessment, the nurse notes bruising across the lower abdomen. Which is the first action the nurse should take?
(a) Measure abdominal girth
(b) Assess abdomen for guarding or rigidity
(c) Check the most recent lab results for hemoglobin and hematocrit
(d) Assess complete health history
Answer:
(b) Assess abdomen for guarding or rigidity
Explanation:
After a traumatic injury, bruising on the abdomen accompanied by guarding or rigidity may indicate major internal organ injury and the patient may be bleeding internally. Determining whether the patient has these additional symptoms is imperative.
Rationale:
(a) is incorrect because measuring abdominal girth is not necessary at this time. Internal hemorrhage may be present before the nurse notes increase in abdominal girth measurement.
(c) is incorrect because assessing lab results is not the first action. Initial labs drawn upon arrival to the emergency department may not indicate slow bleeding from trauma to visceral organs. Immediate physical assessment of the patient takes priority.
(d) is incorrect because taking a complete health history is a general assessment which should be completed but is not the first action the nurse should take. The nurse should remain focused on the here-and-now situation.
Question 37.
A nurse is caring for a 38-year-old female patient who had a colostomy placed three months ago. The client says her husband refuses to be intimate with her because of the colostomy. What is the best response by the nurse?
(a) “Shall we talk, together, with your husband about his concerns related to intimacy and your colostomy?”
(b) “Longer lingerie can be worn to hide the appliance.”
(c) “You can empty the pouch more frequently, so your husband won’t notice it as much.”
(d) “Sexual activity can cause stoma harm, if you’re not careful.”
Answer:
(a) “Shall we talk, together, with your husband about his concerns related to intimacy and your colostomy?”
Explanation:
A colostomy is a new opening made in the large intestine through the abdominal wall where stool will pass into a pouch or appliance. The nurse should try to facilitate open communication between the patient and the spouse about sexual concerns with the colostomy. Collaboration with the ostomy nurse can also help the patient and spouse work through issues related to intimacy after colostomy.
Rationale:
(b) is incorrect because suggesting longer lingerie is dismissive of the patient’s concerns. (The nurse should not assume that the patient wears lingerie.)
(c) is incorrect because although more frequent emptying of the pouch can help eliminate odor, this doesn’t enable open communication about the colostomy’s effect on sexual behavior.
(d) is incorrect because sexual activity does not cause stoma harm. Many colostomy patients are able to return to normal sexual activity with the collection bag in place.
Question 38.
The patient recovering from hemorrhoidectomy tells the nurse he feels the need to have a bowel movement. Which of the following actions should be taken by the nurse?
(a) Assign a UAP to place a bedside commode in the room
(b) Provide for privacy, but stay with the patient
(c) Place the call light in reach, so the patient can call when finished
(d) Obtain a specimen container for stool sample
Answer:
(b) Provide for privacy, but stay with the patient
Explanation:
Hemorrhoidectomy is a surgical removal of hemorrhoids, internal or external. After the surgical procedure, the first bowel movement can be extremely painful and can even cause syncope. The nurse should assist the patient to the bedside commode or bathroom and stay with the patient for the bowel movement.
Rationale:
(a) is incorrect because a bedside commode may be necessary, but it is more important that the patient not be left alone.
(c) is incorrect because the call light should be within reach, but this does not meet safety needs.
(d) is incorrect because a stool sample is not necessary. Stool sample is indicated for a patient who needs laboratory testing to assess for bacterial infection, such as difficile, or parasites. The patient after a hemorrhoidectomy is not necessarily at risk for these complications unless other symptoms are present.
Question 39.
The nurse in the emergency department cares for a patient who experienced a gunshot to the abdomen. The patient’s BP is 88/62, pulse is 126 bpm, and RR is 26. Which action should the emergency room nurse take first?
(a) Send blood for type and cross-matching
(b) Start a large IV for fluid replacement
(c) Obtain vital signs
(d) Assess and maintain airway
Answer:
(d) Assess and maintain airway
Explanation:
The vital signs (low BP, high pulse, high RR) suggest hemorrhage. Airway is the nurse’s priority, especially in a patient who has sustained trauma.
Rationale:
(a) is incorrect because type and cross-matching blood is an appropriate nursing action, but the airway needs to be assessed first. Intubation will take place before supplemental blood products are hung.
(b) is incorrect because IV and fluids are appropriate, but not the first action that should be taken. Establishing an airway is the nurse’s primary concern.
(c) is incorrect because vital signs is an appropriate nursing assessment but not the first needed action.
Question 40.
A male patient in the emergency room, with a diagnosis of mechanical bowel obstruction, is experiencing intermittent abdominal pain. Later, the patient reports constant abdominal pain. What is the next action the nurse should take?
(a) Administer opioid medications, as ordered, intravenously
(b) Position the patient’s knees to his chest
(c) Insert NG tube attached to low-wall suction for gastric decompression
(d) Assess bowel sounds
Answer:
(d) Assess bowel sounds
Explanation:
Due to the change in abdominal pain the patient is experiencing, the nurse must assess bowel sounds and check for rebound tenderness, which can be due to peritonitis or bowel perforation.
Rationale:
(a) is incorrect because pain medications should not be administered until the nurse further assesses the change.
(b) is incorrect because repositioning the patient may lessen or alleviate the abdominal pain, but determining the cause of the pain is the greater priority.
(c) is incorrect because an NG tube is invasive and may not be needed. The nurse should implement least-invasive measures first.
Question 41.
A client is receiving intravenous 5-fluorouracil chemotherapy for colon cancer. Which finding would cause the nurse to contact the healthcare provider?
(a) WBCi400/mm3
(b) Fatigue
(c) Nausea and diarrhea
(d) Oral ulcers and mucositis
Answer:
(a) WBCi400/mm3
Explanation:
5-fluorouracil is an antineoplastic medication used for chemotherapy. Side effects include fatigue, nausea, diarrhea, oral ulcers, bone marrow depression, liver dysfunction, and mucositis. This patient’s WBC count is extremely low, placing the patient at high risk for infection, so the healthcare provider should be notified.
Rationale:
(b) is incorrect because fatigue is a common side effect of fluorouracil.
(c) is incorrect because nausea and diarrhea are common side effects of fluorouracil.
(d) is incorrect because oral ulcers and mucositis are common side effects of fluorouracil.
Question 42.
The nurse cares for a 46-year-old male patient who had an ascending colon colostomy placed two weeks ago. The client states the stool in the pouch is still liquid. What is the best response by the nurse?
(a) “This type of colostomy will always have liquid stool.”
(b) “If you eat more fiber, this will bulk up the stool.”
(c) “The stool will be firmer over time.”
(d) “I will contact the healthcare provider because this is not normal.”
Answer:
(a) “This type of colostomy will always have liquid stool.”
Explanation:
A colostomy placed in the ascending colon will always have liquid stool output because fluid is reabsorbed in the distal portions of the large intestine. The patient’s statement indicates the need for further instruction about expected outcomes after an ascending colon colostomy placement.
Rationale:
(b) is incorrect because fiber will not bulk up the stool at this location.
(c) is incorrect because the stool will not firm up over time.
(d) is incorrect because this is a normal finding for a patient with an ascending colostomy placement.
Question 43.
A 50-year-old male client with irritable bowel syndrome (IBS) has made changes to his diet and taken bulk-forming laxatives but states his symptoms have not improved. He asks the nurse if lubiprostone treatment might help his symptoms. What is the best response by the nurse?
(a) “The drug is still being researched and is not available yet.”
(b) “Lubiprostone is only approved for female patients, but we can talk about other treatment options.”
(c) “Lubiprostone is an effective drug; I will recommend it to the healthcare provider.”
(d) “Bulk-forming laxatives should not be used with lubiprostone.”
Answer:
(b) “Lubiprostone is only approved for female patients, but we can talk about other treatment options.”
Explanation:
Lubiprostone is a drug given for chronic constipation associated with irritable bowel syndrome (IBS). It works by stimulating intestinal receptors for increased fluid absorption and increased bowel transit time. It is only approved for use in women. The nurse should respond therapeutically, by giving factual information and suggesting other options for this patient.
Rationale:
(a) is incorrect because lubiprostone was approved by the FDA in 2006 and has since been used in female patients.
(c) is incorrect because lubiprostone is not yet approved for use in male patients.
(d) is incorrect because lubiprostone can be used safely with bulk-forming laxatives in women.
Question 44.
The nurse is providing education for a male patient who is recovering from colon resection. Which of the following statements does the nurse include in the plan of care?
(a) “Nausea and vomiting may be experienced for a few weeks.”
(b) “Acid reflux can be decreased with moderate consumption of carbonated beverages.”
(c) “Stool softeners will make it easier to have a bowel movement.”
(d) “Your normal workout routine may be resumed, as long as you take it easy.”
Answer:
(c) “Stool softeners will make it easier to have a bowel movement.”
Explanation:
Colon resection is performed to remove part of the large intestine to prevent or remove diseases and conditions affecting the colon. Stool softeners can be taken to make bowel movements easier after colon resection surgery.
Rationale:
(a) is incorrect because nausea and vomiting should not be expected. These symptoms could indicate obstruction or perforation of the intestines and must be reported to the healthcare provider immediately.
(b) is incorrect because carbonated beverages should be avoided after colon resection surgery because they can be irritating to the GI system.
(d) is incorrect because exercise and weight lifting should be completely avoided after colon resection surgery. The patient may be instructed to resume normal physical activities after the first post-op clinic visit.
Question 45.
The nurse is caring for a patient who is at risk for colon cancer. Which dietary recommendation should the nurse include when teaching the patient?
(a) “Consume low-fiber, low-residual foods.”
(b) “It’s easier to digest white bread and rice.”
(c) “Cauliflower and broccoli should be added to your diet.”
(d) “Animal fat foods will protect the mucosa of the intestines.”
Answer:
(c) “Cauliflower and broccoli should be added to your diet.”
Explanation:
A patient who is at risk for colon cancer should increase intake of high-fiber foods, including cauliflower and broccoli, while decreasing animal fats and refined carbohydrates. Other sources of fiber may include whole grain products, beans, peas, and nuts.
Rationale:
(a) is incorrect because a low-fiber diet increases the risk for colon cancer. A high fiber-diet will help prevent colon cancer.
(b) is incorrect because foods rich in simple carbohydrates, such as rice and white bread, are not high in fiber. A high-fiber diet will help prevent colon cancer.
(d) is incorrect because animal fat foods do not protect the mucosa of the intestines.
Question 46.
A patient with a new colostomy is being cared for by the nurse. Which of the following actions should be taken by the nurse?
(a) Empty the colostomy pouch frequently to remove collections of excess gas
(b) Change the pouch and wafer of the ostomy every morning
(c) Allow complete filling of the pouch before emptying
(d) Apply surgical tape to secure pouch and prevent any leakage
Answer:
(a) Empty the colostomy pouch frequently to remove collections of excess gas
Explanation:
A new ostomy pouch should be emptied frequently (when the pouch is 1/3 to 1/2 full), due to excess gas production after placement.
Rationale:
(b) is incorrect because the pouch and wafer do not necessarily need to be changed daily.
(c) is incorrect because the pouch should be emptied when 1/3 to 1/2 full.
(d) is incorrect because surgical tape should not be used on ostomies because of the risk for skin breakdown.
Question 47.
A 35-year-old male patient arrives at the clinic. He has a family history of colon cancer. His father and brother had cancer, and he wants to know what the chances are that he will be diagnosed with colon cancer. What is the best response by the nurse?
(a) “Eating a low-fat, low-fiber diet will decrease your chances significantly.”
(b) “Colon cancer is autosomal dominant and skips generations, so you will be safe.”
(c) “Preventive surgery plus chemotherapy can remove the cancer cells and prevent the disease.”
(d) “You should have colonoscopies more often for early identification of abnormal polyps.”
Answer:
(d) “You should have colonoscopies more often for early identification of abnormal polyps.”
Explanation:
Modifiable risk factors for colorectal (colon) cancer include low-fiber/high-fat diet. Frequent colonoscopies should be encouraged for early identification of abnormal/cancerous cells.
Rationale:
(a) is incorrect because a low-fat, high-fiber diet decreases chances of developing colon cancer.
(b) is incorrect because colon cancer does not skip generations. Family history of colon cancer increases this patient’s risk.
(c) is incorrect because preventive surgery and chemotherapy can decrease risk but do not prevent cancer, ultimately.
Question 48.
A 64-year-old patient in the emergency room has been admitted for Salmonella poisoning. The patient’s heart rate is 104 bpm, blood pressure 96/56 mmHg, respirations 24 bpm, and oxygen saturation 97%. What is the first action the nurse should complete?
(a) Apply oxygen
(b) Administer IV fluids
(c) Provide perineal care
(d) Teach proper food preparation
Answer:
(b) Administer IV fluids
Explanation:
Older patients who experience Salmonella poisoning can develop dehydration from vomiting and diarrhea quickly. This patient’s vital signs suggest the patient is hypotensive and tachycardic, with elevated respirations, in response to dehydration. Restoring fluid balance is important in this population. Prompt administration of IV fluids is the priority nursing action.
Rationale:
(a) is incorrect because additional oxygen is not necessary for a patient with an oxygen saturation of 97%.
(c) is incorrect because caring for the perineum is a standard component of care but does not directly address the dehydration.
(d) is incorrect because teaching proper food preparation is appropriate before the patient is discharged home but not the first action.
Question 49.
A client with viral gastroenteritis is receiving dietary instruction from the nurse. Which instruction should be included in the client's teaching?
(a) “Drink extra fluids for prevention of dehydration.”
(b) “Limit your fluids to l liter per day.”
(c) “Drink milk to increase protein intake.”
(d) “Nausea can be relieved with small sips of tea or cola.”
Answer:
(a) “Drink extra fluids for prevention of dehydration.”
Explanation:
In viral gastroenteritis (more commonly referred to as the stomach flu), the lining of the stomach, small intestine, and large intestine become inflamed, causing vomiting and/or diarrhea. This can be caused by several different viruses and is highly contagious and extremely common. The most common complication is dehydration. Fluids should be encouraged to replace water lost in the vomit and diarrhea.
Rationale:
(b) is incorrect because fluids should not be limited in viral gastroenteritis. A normal adult needs at least 2 liters of fluid daily, so suggesting the patient limit fluids to 1 liter is not appropriate to meet hydration needs.
(c) is incorrect because milk products are not recommended with viral gastroenteritis as they can further irritate the GI tract and worsen diarrhea.
(d) is incorrect because caffeine increases motility of the intestinal tract and can worsen diarrhea. Carbonated beverages, such as ginger ale or lemon-lime soda, may be tolerated with viral gastroenteritis; however, the high fructose corn syrup used to sweeten most sodas can also be irritating.
Question 50.
A 55-year-old male patient hospitalized with Salmonella food poisoning has been educated by the nurse. Which statement made by the patient indicates additional teaching is needed?
(a) “I will have my wife do all the cooking.”
(b) “The ciprofloxacin should be taken until diarrhea resolves.”
(c) “I will wash my hands with antibacterial soap before eating.”
(d) “Dishes should be placed in the dishwasher after eating.”
Answer:
(b) “The ciprofloxacin should be taken until diarrhea resolves.”
Explanation:
Salmonella gastroenteritis infection is generally not treated with antibiotics unless the infection becomes systemic. In that case, ciprofloxacin (a fluoroquinolone antibiotic) is the drug of choice. This medication is taken for 10 days to two weeks. The medication should be taken until completed, even after the diarrhea or other symptoms subside.
Rationale:
(a) is incorrect because people who have Salmonella should not prepare foods because this is highly contagious and can be transferred person-to-person. The patient’s statement indicates correct understanding.
(c) is incorrect because hands should be washed with antibacterial soap before eating, indicating correct understanding. The nurse should also teach the patient about the importance of proper handwashing after using the bathroom, because Salmonella can be transferred via the fecal-oral route.
(d) is incorrect because the statement indicates the patient understands that the dishwasher is the preferred method of cleaning dishes to eradicate Salmonella bacteria. (Handwashing dishes is not recommended when a member of the household has Salmonella poisoning.) Dishes, silverware, and cups should not be shared.
Question 51.
Which clinical symptoms should the nurse expect to find in a patient experiencing exacerbation of Crohn's disease?
(a) Positive Murphy’s sign, rebound tenderness
(b) Dull, hypoactive bowel sounds heard in bilateral lower abdominal quadrants
(c) High-pitched rushing sounds in the right lower quadrant
(d) Abdominal cramping that worsens at night
Answer:
(c) High-pitched rushing sounds in the right lower quadrant
Explanation:
Crohn’s disease is inflammatory bowel disease that causes abdominal pain, fatigue, severe diarrhea, malnutrition, and weight loss. Crohn’s disease causes narrowing of the bowel lumen, (often in the ileum and the ascending colon, in the right lower abdominal quadrant) and thus would cause the nurse to hear high-pitched rushing sounds.
Rationale:
(a) is incorrect because Murphy’s sign is not used with Crohn’s disease. Murphy’s sign refers pain during inspiration while the examiner’s fingers are pressing on the location of the gallbladder. A positive Murphy’s sign indicates cholecystitis; a negative Murphy’s sign is seen with choledocholithiasis (bile duct stones), pyelonephritis (kidney infection), and cholangitis (bile duct infection). Rebound tenderness is used to determine peritonitis.
(b) is incorrect because Crohn’s disease is not characterized by dullness or hypoactive bowel sounds.
(d) is incorrect because Crohn’s disease is not characterized by worsening abdominal cramping at night. Abdominal pain in patients with Crohn’s disease is usually worse after meals.
Read More: