The variety of NCLEX Questions available allows students to cover a wide range of topics and increase their knowledge base.
NCLEX Complications of Pregnancy Questions
Complications of Pregnancy NCLEX Practice Questions
Question 1.
A laboring client with preeclampsia is prescribed magnesium sulfate 2 g/h IV piggyback. The pharmacy sends the IV to the unit labeled magnesium sulfate 20 g/500 mL normal saline. To deliver the correct dose, the nurse should set the pump to deliver how many milliliters per hour? Record your answer using one decimal place.
.................mL.
Answer:
50 ml
Explanation:
\(\frac{500 \mathrm{~mL}}{20 \mathrm{~g}} \times \frac{2 \mathrm{~g}}{\mathrm{~h}}\) = \(\frac{1,000 \mathrm{~g} / \mathrm{mL}}{2_1^{50} \mathrm{~g} / \mathrm{h}}\) = \(\frac{50 \mathrm{~mL}}{1 \mathrm{~h}}\)
Question 2.
A 3 2-year-old multigravida returns to the clinic for a routine prenatal visit at 36 weeks’ gestation. The assessments during this visit include blood pressure, 140/90 mm Hg; pulse, 80 beats/min; respiratory rate, 16 breaths/min. What further information should the nurse obtain to determine if this client is becoming preeclamptic?
(a) headaches
(b) blood glucose level
(c) proteinuria
(d) peripheral edema
Answer:
(c) proteinuria
Explanation:
The two major defining characteristics of preeclampsia are blood pressure elevation of 140/90 mm Hg or greater and proteinuria. Because the client’s blood pressure meets the gestational hypertension criteria, the next nursing responsibility is to determine if she has protein in her urine. If she does not, then she may be having transient hypertension. The peripheral edema is within normal limits for someone at this gestational age, particularly because it is in the lower extremities.
While the preeclamptic client may have significant edema in the face and hands, edema can be caused by other factors and is not part of the diagnostic criteria. Headaches are significant in pregnancy-induced hypertension but may have other etiologies. The client’s blood glucose level has no bearing on a preeclampsia diagnosis.
Question 3.
The nurse instructs a preeclamptic client about monitoring the movements of her fetus to determine fetal well-being. Which statement by the client indicates that she needs further instruction about when to call the health care provider (HCP) concerning fetal movement?
(a) “if the fetus is becoming less active than before”
(b) “if it takes longer each day for the fetus to move 10 times”
(c) “if the fetus stops moving for 12 hours”
(d) “if the fetus moves more often than three times an hour”
Answer:
(d) “if the fetus moves more often than three times an hour”
Explanation:
The fetus is considered well if it moves more often than three times in 1 hour. Daily fetal movement counting is part of all high-risk assessments and is a noninvasive, inexpensive method of monitoring fetal well-being. The HCP Q should be notified if there is a gradual slowing over time of fetal activity, if each day it takes longer for the fetus to move a minimum of 10 times, or if the fetus stops moving for 12 hours or longer.
Question 4.
A 29-year-old multigravida at 37 weeks’ gestation is being treated for severe preeclampsia and has magnesium sulfate infusing at 3 g/h. What is the priority intervention to maintain safety for this client?
(a) Maintain continuous fetal monitoring.
(b) Encourage family members to remain at bedside.
(c) Assess reflexes, clonus, visual disturbances, and headache.
(d) Monitor maternal liver studies every 4 hours.
Answer:
(c) Assess reflexes, clonus, visual disturbances, and headache.
Explanation:
The central nervous system (CNS) functioning and freedom from injury is a priority in maintaining well-being of the maternal-fetal unit. If the mother suffers CNS damage related to hypertension or stroke, oxygenation status is compromised, and the well-being of both mother and infant are at risk. Continuous fetal monitoring is an assessment strategy for the infant only and would be of secondary importance to maternal CNS assessment because maternal oxygenation will dictate fetal oxygenation and well-being.
In preeclampsia, frequent assessment of maternal reflexes, clonus, visual disturbances, and headache give clear evidence of the condition of the maternal CNS system. Monitoring the liver studies does give an indication of the status of the maternal system, but the less invasive and highly correlated condition of the maternal CNS system in assessing reflexes, maternal headache, visual disturbances, and clonus is the highest priority. Psychosocial care is a priority and can be accomplished in ways other than having the family remain at the bedside.
Question 5.
At 32 weeks’ gestation, a 15-year-old primi- a gravid client who is 5 feet, 2 inches (151.7 cm) has gained a total of 20 lb (9.1 kg), with a 1-lb (0.45-kg) gain in the last 2 weeks. Urinalysis reveals negative glucose and a trace of protein. The nurse should advise the client on which factor increases her risk for preeclampsia?
(a) total weight gain
(b) short stature
(c) adolescent age group
(d) trace proteinuria
Answer:
(c) adolescent age group
Explanation:
Clients with increased risk for preeclampsia include primigravid clients younger than 20 years or older than 40 years, clients with 5 or more pregnancies, women of color, women with multifetal pregnancies, women with diabetes or heart disease, and women with hydramnios. A total weight gain of 20 lb (9.1 kg) at 32 weeks’ gestation with a 1-lb (0.45 kg) weight gain in the last 2 weeks is within normal limits. Short stature is not associated with the development of preeclampsia. A trace amount of protein in the urine is common during pregnancy. However, protein amounts of 1 + or more may be a symptom of pregnancy-induced hypertension.
Also Check: Side Effects Of Eating Too Many Walnuts
Question 6.
After instructing a primigravid client at 38 weeks' gestation about how preeclampsia can affect the client and the growing fetus, the nurse realizes that the client needs additional instruction when she says that preeclampsia can lead to which problem?
(a) hydrocephalic infant
(b) abruptio placentae
(c) intrauterine growth restriction
(d) poor placental perfusion
Answer:
(a) hydrocephalic infant
Explanation:
Congenital anomalies such as hydrocephalus are not associated with preeclampsia. Conditions such as stillbirth, prematurity, abruptio placentae, intrauterine growth restriction, and poor placental perfusion are associated with preeclampsia. Abruptio placentae occurs because of severe vasoconstriction. Intrauterine growth restriction is possible owing to poor placental perfusion. Poor placental perfusion results from increased vasoconstriction.
Question 7.
A nurse is completing a prenatal assessment on a woman who is 28 weeks’ pregnant with gestational hypertension. Which findings should be reported to the primary care provider? Select all that apply.
(a) dull headache
(b) weight gain of 1 lb (500 g) per week
(c) blurred vision
(d) 1+ urine protein
(e) fundal height of 28 cm
Answer:
(a) dull headache
(c) blurred vision
(d) 1+ urine protein
Explanation:
(a), (c), (d) The nurse must be alert for any signs and symptoms of superimposed preeclampsia in women with gestational hypertension. Dull headache, blurred vision, and protein in urine are all classic signs of preeclampsia in pregnancy and must be reported to the primary care provider immediately. Weight gain of 1 lb (500 g) per week is an expected finding. Fundal height of 28 cm is an expected finding.
Question 8.
When teaching a multigravid client diag¬nosed with mild preeclampsia about nutritional needs, the nurse should discuss which type of diet?
(a) high-residue diet
(b) low-sodium diet
(c) regular diet
(d) high-protein diet
Answer:
(c) regular diet
Explanation:
For clients with mild preeclampsia, a regular diet with ample protein and calories is recommended. If the client experiences constipation, she should increase the fiber in her diet, such as by eating raw fruits and vegetables, and increase fluid intake. A high-residue diet is not a nutritional need in preeclampsia. Sodium and fluid intake should not be restricted or increased. A high-protein diet is unnecessary.
Question 9.
A woman with preeclampsia is receiving magnesium sulfate via infusion pump at 1 g/h. The nurse’s assessment includes temperature 36.7°C; pulse 78; respirations 12/minute; blood pressure 128/82 mm Hg; urinary output 90 rnL in last 4 hours via urinary catheter; patellar-tendon reflex absent; ankle clonus absent; fetal heart rate 120 beats/min; cervix 4 cm dilated, 80% effaced, station -1.
Which is the most appropriate action for the nurse to take?
(a) Assess the urinary catheter for kinks in the drainage tubing, and obtain a urine sample.
(b) Document findings, and continue to monitor her progress in labor.
(c) Discontinue the magnesium sulfate infusion, and notify the health care provider (HCP).
(d) Increase fluid intake intravenously, and measure intake and output.
Answer:
(c) Discontinue the magnesium sulfate infusion, and notify the health care provider (HCP).
Explanation:
The nurse must be alert to signs of magnesium sulfate toxicity that include loss of deep tendon reflexes, which is often the first sign (patellar-tendon response is the most common reflex tested); urinary output decreases (should have at least 30 mL/h); and respirations decrease (12 respirations/min is low and could be developing respiratory distress). The first action would be to stop magnesium sulfate infusion and notify the HCPT The urinary catheter tubing maybe kinked; however, looking at all findings would indicate the woman is experiencing magnesium sulfate toxicity.
It is not a priority to obtain a urine sample. Documentation is extremely important to complete; however, the nurse must intervene by stopping the magnesium sulfate and notifying the primary care provider. Increasing fluid intake at this point is not appropriate with a woman who has magnesium sulfate toxicity. Intake and output should be ongoing for a client on intravenous fluids and magnesium sulfate and a diagnosis of preeclampsia.
Question 10.
A primigravid client at 38 weeks’ gestation diagnosed with mild preeclampsia calls the clinic nurse to say she has had a continuous headache for the past 2 days accompanied by nausea. The client does not want to take aspirin. What should the nurse tell the client?
(a) “Take two acetaminophen tablets. They are not as likely to upset your stomach.”
(b) “I think the health care provider should see you today. Can you come to the clinic this morning?”
(c) “You need to lie down and rest. Have you tried placing a cool compress over your head?”
(d) “I will ask the health care provider to call in a prescription for nausea medications. What is your pharmacy’s number?”
Answer:
(b) “I think the health care provider should see you today. Can you come to the clinic this morning?”
Explanation:
A client with preeclampsia and a continuous headache for 2 days should be seen by a health care provider (HCP) 2 immediately. Continuous headache, drowsiness, and mental confusion indicate poor cerebral perfusion and are symptoms of severe preeclampsia. Immediate care is recommended because these symptoms may lead to eclampsia or seizures if left untreated.
Advising the client to take two acetaminophen tablets would be inappropriate and may lead to further complications if the client is not evaluated and treated. Although the application of cool compresses may ease the pain temporarily, this would delay treatment. Treatment for nausea may be indicated, but only after the primary care primary provider has seen the client and determined if the preeclampsia requires further treatment.
Question 11.
When the nurse is preparing the room for admission of a multigravid client at 36 weeks’ gesta¬tion diagnosed with severe preeclampsia, which item is most important for the nurse to obtain?
(a) oxytocin infusion solution
(b) disposable tongue blades
(c) portable ultrasound machine
(d) padding for the side rails
Answer:
(d) padding for the side rails
Explanation:
The client with severe preeclampsia may develop eclampsia, which is characterized by seizures. The client needs a darkened, quiet room and side rails with thick padding. This helps decrease the potential for injury should a seizure occur. Airways, a suction machine, and oxygen also should be available. If the client is to undergo induction of labor, oxytocin infusion solution can be obtained at a later time.
Tongue blades are not necessary. However, the emergency cart should be placed nearby in case the client experiences a seizure. The ultrasound machine may be used at a later point to provide information about the fetus. In many hospitals, the client with severe preeclampsia is admitted to the labor area, where she and the fetus can be closely monitored. The safety of the client and her fetus is the priority.
Question 12.
A client who is 34 weeks pregnant is admitted to the labor and birth room with the diagnosis of preeclampsia. The client’s vital signs are as follows: blood pressure 149/92 mm Hg; pulse, 62 beats/min; respiratory rate, 18 breaths/min: temperature, 98.4°F (36.8°C). What is the priority intervention?
(a) Encourage the client to lie in a lateral position.
(b) Administer an antihypertensive agent.
(c) Notify the health care provider (HCP) of the client’s blood pressure.
(d) Check the cervix.
Answer:
(a) Encourage the client to lie in a lateral position.
Explanation:
Although the client is being admitted, the first response would be to attempt to lower blood pressure by putting the client in left lateral position. The other interventions may be appropriate later, but left lateral position would be the priority.
Question 13.
For the client who is receiving intravenous magnesium sulfate for severe preeclampsia, which assessment finding would alert the nurse to suspect hypermagnesemia?
(a) decreased deep tendon reflexes
(b) cool skin temperature C
(c) rapid pulse rate
(d) tingling in the toes
Answer:
(a) decreased deep tendon reflexes
Explanation:
Typical signs of hypermagnesemia include decreased deep tendon reflexes, sweating or a flushing of the skin, oliguria, decreased respirations, and lethargy progressing to coma as the toxicity increases. The nurse should check the client’s patellar, biceps, and radial reflexes regularly during magnesium sulfate therapy.
Cool skin temperature may result from peripheral vasodilation, but the opposite flushing and sweating are usually seen. A rapid pulse rate commonly occurs in hypomagnesemia. Tingling in the toes may suggest hypocalcemia, not hypermagnesemia.
Question 14.
A client at 28 weeks’ gestation presents to the emergency department with a “splitting headache.” What actions are indicated by the nurse at this time? Select all that apply.
(a) Reassure the client that headaches are a normal part of pregnancy.
(b) Assess the client for vision changes or epigastric pain.
(c) Obtain a nonstress test.
(d) Assess the client’s reflexes and presence of clonus.
(e) Determine if the client has a documented ultrasound for this pregnancy.
Answer:
(b) Assess the client for vision changes or epigastric pain.
(c) Obtain a nonstress test.
(d) Assess the client’s reflexes and presence of clonus.
Explanation:
(b), (c), (d) Headaches could be a sign of pre-eclampsia/eclampsia in pregnancy. The client should be assessed for headache, vision changes, epigastric pain, hyperreflexes, and the presence of clonus. Her fetus should be assessed using a nonstress test. An ultrasound done in this pregnancy does not give information to assess the presence of preeclampsia/eclampsia.
Question 15.
Which outcome would the nurse identify as the priority to achieve when developing the plan of care for a primigravid client at 38 weeks’ gestation who is hospitalized with severe preeclampsia and receiving intravenous magnesium sulfate?
(a) decreased generalized edema within 8 hours
(b) decreased urinary output during the first 24 hours
(c) sedation and decreased reflex excitability within 48 hours
(d) absence of any seizure activity during the first 48 hours
Answer:
(d) absence of any seizure activity during the first 48 hours
Explanation:
The highest priority for a client with severe preeclampsia is to prevent seizures, thereby minimizing the possibility of adverse effects on the mother and fetus, and then to facilitate safe birth. Efforts to decrease edema, reduce blood pressure, increase urine output, limit kidney damage, and maintain sedation are desirable but are not as important as preventing seizures.
It would take several days or weeks for the edema to be decreased. Sedation and decreased reflex excitability can occur with the administration of intravenous magnesium sulfate, which peaks in 30 minutes, much sooner than 48 hours.
Question 16.
The nurse is administering intravenous magnesium sulfate as prescribed for a client at 34 weeks’ gestation with severe preeclampsia. What are desired outcomes of this therapy? Select all that apply.
(a) temperature, 98°F (36.7°C); pulse, 72 beats/min; respiratory rate, 14 breaths/min
(b) urinary output < 30 mL/h
(c) fetal heart rate with late decelerations
(d) blood pressure of < 140/90 mm Hg
(e) deep tendon reflexes 2+
(f) magnesium level = 5.6 mg/dL (2.8 mmol/L)
Answer:
(a) temperature, 98°F (36.7°C); pulse, 72 beats/min; respiratory rate, 14 breaths/min
(e) deep tendon reflexes 2+
(f) magnesium level = 5.6 mg/dL (2.8 mmol/L)
Explanation:
(a), (e), (f) The use of magnesium sulfate as an anticonvulsant acts to depress the central nervous system by blocking peripheral neuromuscular transmissions and decreasing the amount of acetylcholine liberated. The primary goal of magnesium sulfate therapy is to prevent seizures. While being used, the temperature and pulse of the client should remain within normal limits.
The respiratory rate needs to be >12 respirations per minute (rpm). Rates at 12 rpm or lower are associated with respiratory depression and are seen with magnesium toxicity. Renal compromise is identified with a urinary output of < 30 mL/h. A fetal heart rate that is maintained within the 112 to 160 range is desired without later or variable decelerations.
While extreme elevations of blood pressure must be treated, achieving a normal pressure carries the risk of decreasing perfusion to the fetus. Deep tendon reflexes should not be diminished or exaggerated. The therapeutic magnesium sulfate level of 5 to 8 mg/ dL (2.5 to 4 mmol/L) is to be maintained.
Question 17.
Soon after admission of a primigravid client at 38 weeks’ gestation with severe preeclampsia, the primary health care provider (HCP) prescribes a continuous intravenous infusion of 5% dextrose in Ringer’s solution and 4 g of magnesium sulfate. While the medication is being administered, which assessment finding should the nurse report immediately?
(a) respiratory rate of 12 breaths/min
(b) patellar reflex of +2
(c) blood pressure of 160/88 mm Hg
(d) urinary output exceeding intake
Answer:
(a) respiratory rate of 12 breaths/min
Explanation:
A respiratory rate of 12 breaths/min suggests potential respiratory depression, an adverse effect of magnesium sulfate therapy. The medication must be stopped, and the HCP j[Q should be notified immediately. A patellar reflex of +2 is normal. Absence of a patellar reflex suggests magnesium toxicity. A blood pressure reading of 160/88 mm Hg would be a common finding in a client with severe preeclampsia. Urinary output exceeding intake is not likely in a client receiving intravenous magnesium sulfate. Oliguria is more common.
Question 18.
As the nurse enters the room of a newly admitted primigravid client diagnosed with severe preeclampsia, the client begins to experience a seizure. Which action should the nurse take first?
(a) Insert an airway to improve oxygenation.
(b) Note the time when the seizure begins and ends.
(c) Call for immediate assistance.
(d) Turn the client to her left side.
Answer:
(c) Call for immediate assistance.
Explanation:
Principles of emergency management begin with calling for assistance. If a client begins to have a seizure, the first action by the nurse is to remain with the client and call for immediate assistance. The nurse needs to have some assistance in managing this client. After the seizure, the client needs intensive monitoring.
An airway can be inserted, if appropriate, after the seizure ends. Noting the time the seizure begins and ends and turning the client to her left side should be done after assistance is obtained.
Question 19.
After administering hydralazine 5 mg intravenously as prescribed for a primigravid cli¬ent with severe preeclampsia at 39 weeks’ gestation, the nurse should assess the client for which complication?
(a) tachycardia
(b) bradypnea
(c) polyuria
(d) dysphagia
Answer:
(a) tachycardia
Explanation:
One of the most common adverse effects of the drug hydralazine is tachycardia. Therefore, the nurse should assess the client’s heart rate and pulse. Hydralazine acts to lower blood pressure by peripheral dilation without interfering with placental circulation. Bradypnea and polyuria are usually not associated with hydralazine use. Dysphagia is not a typical adverse effect of hydralazine.
Question 20.
A primigravid client with severe preeclamp¬sia exhibits hyperactive, very brisk patellar reflexes with two beats of ankle clonus present. How does the nurse document the patellar reflexes?
(a) 1+
(b) 2+
(c) 3+
(d) 4+
Answer:
(d) 4+
Explanation:
These findings would be documented as 4+ 1+ indicates a diminished response; 2+ indicates a normal response; 3+ indicates a response that is brisker than average but not abnormal. Mild clonus is said to be present when there are two movements.
Question 21.
A 16-year-old primigravid client at 37 weeks’ gestation with severe preeclampsia is in early active labor. The client’s blood pressure is 164/110 mm Hg. Which finding would alert the nurse that the client may be about to experience a seizure?
(a) decreased contraction intensity
(b) decreased temperature
(c) epigastric pain
(d) hyporeflexia
Answer:
(c) epigastric pain
Explanation:
Epigastric pain or acute right upper quadrant pain is associated with the development of eclampsia and an impending seizure; this is thought to be related to liver ischemia. Decreased contraction intensity is unrelated to the severity of the preeclampsia.
Typically, the client’s temperature increases because of increased cerebral pressure. A decrease in temperature is unrelated to an impending seizure. Hyporeflexia is not associated with an impending seizure. Typically, the client would exhibit hyperreflexia.
Question 22.
Following an eclamptic seizure, the nurse should assess the client for which complication?
(a) polyuria
(b) facial flushing
(c) hypotension
(d) uterine contractions
Answer:
(d) uterine contractions
Explanation:
After an eclamptic seizure, the client commonly falls into a deep sleep or coma. The nurse must continually monitor the client for signs of impending labor because the client will not be able to verbalize that contractions are occurring. Oliguria is more common than polyuria after an eclamptic seizure. Facial flushing is not common unless it is caused by a reaction to a medication. Typically, the client remains hypertensive unless medications such as magnesium sulfate are administered.
Question 23.
An obese 36-year-old multigravid client at 12 weeks’ gestation has a history of chronic hypertension. She was treated with methyldopa before becoming pregnant. When counseling the client about diet during pregnancy, the nurse realizes that the client needs additional instruction when she makes which statement?
(a) “I need to reduce my caloric intake to 1,200cal/day.”
(b) “A regular diet is recommended during pregnancy.”
(c) “I should eat more frequent meals if I get heartburn.”
(d) “I need to consume more fluids and fiber each day.”
Answer:
(a) “I need to reduce my caloric intake to 1,200cal/day.”
Explanation:
Pregnancy is not the time for clients to begin a diet. Clients with chronic hypertension need to consume adequate calories to support fetal growth and development. They also need an adequate protein intake. Meat and beans are good sources of protein. Most pregnant women report that eating more frequent, smaller meals decreases heartburn resulting from the reflux of acidic secretions into the lower esophagus. Pregnant women need adequate hydration (fluids) and fiber to prevent constipation.
Question 24.
After instructing a multigravid client at 10 weeks’ gestation diagnosed with chronic hypertension about the need for frequent prenatal visits, the nurse determines that the instructions have been successful when the client makes which statement?
(a) “I may develop hyperthyroidism because of my high blood pressure.”
(b) “I need close monitoring because I may have a small-for-gestational-age infant.”
(c) “It is possible that I will have excess amniotic fluid and may need a cesarean section.”
(d) “I may develop placenta accreta, so I need to keep my clinic appointments.”
Answer:
(b) “I need close monitoring because I may have a small-for-gestational-age infant.”
Explanation:
Women with chronic hypertension during pregnancy are at risk for complications such as preeclampsia (about 25%), abruptio placentae, and intrauterine growth retardation, resulting in a small- for-gestational-age infant. There is no association between chronic hypertension and hyperthyroid-ism. Pregnant women with chronic hypertension are not at an increased risk for hydramnios (polyhydramnios), an abnormally large amount of amniotic fluid.
Clients with diabetes and multiple gestations are at risk for this condition. Placenta accreta, a rare placental abnormality, refers to a condition in which the placenta abnormally adheres to the uterine lining. It is not associated with chronic hypertension.
Question 25.
After the nurse reinforces the danger signs to report with a gravida 2 client at 32 weeks’ gestation with an elevated blood pressure, which client state¬ments would demonstrate understanding of when to call the primary health care provider’s (HCP’s) office? Select all that apply.
(a) “if I feel dizzy when I get up quickly”
(b) “if I see any bleeding, even if I have no pain”
(c) “if I have a pounding headache that will not go away”
(d) “if I notice the veins in my legs getting bigger”
(e) “if the leg cramps at night are waking me up”
(f) “if the baby seems to be more active than usual”
Answer:
(b) “if I see any bleeding, even if I have no pain”
(c) “if I have a pounding headache that will not go away”
(e) “if the leg cramps at night are waking me up”
Explanation:
(b), (c), (e) Vaginal bleeding with or without pain could signify placenta previa or abruptio placentae. Continuous or pounding headache could indicate an elevated blood pressure, and change in the strength or frequency of fetal movements could indicate that the fetus is in distress. Orthostatic hypotension can occur during pregnancy and can be alleviated by rising slowly. Leg veins may increase in size due to additional pressure from the increasing uterine size, while leg cramps may also occur and can commonly be decreased with calcium supplements.
Question 26.
A client presents to the OB triage unit with no prenatal care and painless, bright red vaginal bleeding. Which interventions are most indicated?
(a) applying an external fetal monitor and completing a physical assessment
(b) applying an external fetal monitor and performing a sterile vaginal exam
(c) obtaining a fundal height physical assessment on the client
(d) obtaining fundal height and a sterile vaginal exam
Answer:
(a) applying an external fetal monitor and completing a physical assessment
Explanation:
Bright red vaginal bleeding without contractions could indicate a placenta previa. A sterile vaginal exam should never be done on a woman with a known or suspected placenta previa. Applying the external fetal monitor will allow the nurse to assess fetal status. A complete physical assessment of the client is indicated. A fundal height is used to monitor fetal growth during pregnancy but does not provide information related to vaginal bleeding.
Question 27.
The nurse is caring for a 22-year-old G2, P2 client who has disseminated intravascular coagulation after delivering a dead fetus. Which finding is the highest priority to report to the health care provider (HCP)?
(a) activated partial thromboplastin time (APTT) of 30 seconds
(b) hemoglobin of 11.5 g/dL (115 g/L)
(c) urinary output of 25 mL in the past hour
(d) platelets at 149,000/mm3 (149 x 109/L)
Answer:
(c) urinary output of 25 mL in the past hour
Explanation:
Urinary output of < 30 mL/h indicates renal compromise and would be the most important assessment finding to report to the HCP. The APTT is within normal limits, and the hemoglobin is lower than values for an adult female but within normal limits for a pregnant female. Although the platelet level is slightly low and may impact blood clotting, when compared to renal failure, it is less important.
Question 28.
A 24-year-old client, G3, Tl, Pi, Al, Ll at 32 weeks’ gestation, is admitted to the hospital because of vaginal bleeding. After reviewing the client’s history, which factor might lead the nurse to suspect abruptio placentae?
(a) several hypotensive episodes
(b) previous low transverse cesarean birth
(c) one induced abortion
(d) history of cocaine use
Answer:
(d) history of cocaine use
Explanation:
Although the exact cause of abruptio placentae is unknown, possible contributing factors include excessive intrauterine pressure caused by hydramnios or multiple pregnancy, cocaine use, cig¬arette smoking, alcohol ingestion, trauma, increased maternal age and parity, and amniotomy. A history of hypertension is associated with an increased risk of abruptio placentae. A previous low transverse cesarean section and a history of one induced abortion are associated with increased risk of placenta previa, not abruptio placentae.
Question 29.
When caring for a multigravid client admitted to the hospital with vaginal bleeding at 38 weeks’ gestation, the nurse would anticipate administering intravenously which therapeutic agent if the client develops disseminated intravascular coagulation (DIC)?
(a) Ringer’s lactate solution
(b) fresh frozen platelets
(c) 5% dextrose solution
(d) warfarin
Answer:
(b) fresh frozen platelets
Explanation:
Treatment of DIC includes treating the causative factor, replacing maternal coagulation factors, and supporting physiologic functions. Intravenous infusions of whole blood, fresh frozen plasma, or platelets are used to replace depleted maternal coagulation factors.
Although Ringer’s lactate solution and 5% dextrose solution may be used as intravenous fluid replacement, the client needs blood component therapy. Therefore, normal saline must be used. Intravenous heparin, not warfarin, may be administered to halt the clotting cascade
Question 30.
When the nurse is assessing a 34-year-old multigravid client at 34 weeks’ gestation experiencing moderate vaginal bleeding, which symptom would most likely alert the nurse that placenta previa is present?
(a) painless vaginal bleeding
(b) uterine tetany
(c) intermittent pain with spotting
(d) dull lower back pain
Answer:
(a) painless vaginal bleeding
Explanation:
The most common assessment finding associated with placenta previa is painless vaginal bleeding. With placenta previa, the placenta is abnormally implanted, covering a portion or all of the cervical os. Uterine tetany, intermittent pain with spotting, and dull lower back pain are not associated with placenta previa.
Uterine tetany is associated with oxytocin administration. Intermittent pain with spotting commonly is associated with a spontaneous abortion. Dull lower back pain is commonly associated with poor maternal posture or a urinary tract infection with renal involvement.
Question 31.
Following a cesarean birth for abruptio placentae, a multigravid client tells the nurse, “I feel like such a failure. None of my other births were like this.” Which factor is most important for the nurse to consider when responding to the client?
(a) The client will most likely have postpartum blues.
(b) Maternal-infant bonding is likely to be difficult.
(c) The client’s feeling of grief is a normal reaction.
(d) This type of birth was necessary to save the client’s life.
Answer:
(c) The client’s feeling of grief is a normal reaction.
Explanation:
Feelings of loss, grief, and guilt are normal after a cesarean birth, particularly if it was not planned. The nurse should support the client, listen with empathy, and allow the client time to grieve. The likelihood of the client experiencing postpartum blues is not known, and no evidence is presented.
Although maternal-infant bonding may be delayed owing to neonatal complications or maternal pain and subsequent medications, it should not be difficult. Although the nurse is aware that this type of birth was necessary to save the client's life, using this as the basis for the response does not acknowledge the mother’s feelings.
Question 32.
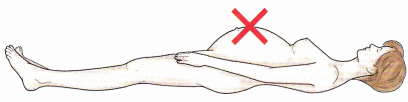
A client has received epidural anesthesia to control pain during a vaginal birth. Place an X over the highest point on the body locating the level of anesthesia expected for a vaginal birth.
Answer:
The level of anesthesia achieved via epidural anesthesia for a vaginal birth is TlO (approximately the level of the umbilicus). Epidural anesthesia for a cesarean birth would be at the level of T4 to T6, approximately the nipple line.
Question 33.
Which action should the nurse take first when admitting a multigravid client at 36 weeks’ gestation with a probable diagnosis of abruptio placentae?
(a) Prepare the client for a vaginal examination.
(b) Obtain a brief history from the client.
(c) Insert a large-gauge intravenous catheter.
(d) Prepare the client for an ultrasound scan.
Answer:
(c) Insert a large-gauge intravenous catheter.
Explanation:
Abruptio placentae is a medical emergency because the degree of hypovolemic shock may be out of proportion to visible blood loss. On admission, the nurse should plan to first insert a large-gauge intravenous catheter for fluid replacement and oxygen by mask to decrease fetal anoxia. Vaginal examination usually is not performed on pregnant clients who are experiencing third-trimester bleeding due to abruptio placentae because it can result in damage to the placenta and further fetal anoxia.
The client’s history can be obtained once the client has been admitted and the intravenous line has been started. The goal is birth of the fetus, usually by emergency cesarean section. The nurse should also plan to monitor the client’s vital signs and the fetal heart rate. Ultrasound is of limited use in the diagnosis of abruptio placentae.
Question 34.
The health care provider (HCP) has determined that a preterm labor client at 34 weeks’ gestation has no fetal fibronectin present. Based on this finding, the nurse would anticipate which other client finding within the next week?
(a) The client will develop preeclampsia.
(b) The fetus will develop mature lungs.
(c) The client will not develop preterm labor.
(d) The fetus will not develop gestational diabetes.
Answer:
(c) The client will not develop preterm labor.
Explanation:
The absence of fetal fibronectin in a vaginal swab between 22 and 37 weeks’ gestation indicates there is <1% risk of developing preterm labor in the next week. Fetal fibronectin is an extra cellular protein normally found in fetal membranes and deciduas and has no correlation with preeclampsia, fetal lung maturation, or gestational diabetes.
Question 35.
A nurse is discussing preterm labor in a prenatal class. After class, a client asks the nurse to identify again the nursing strategies to prevent preterm labor. The client needs further instruction when she makes which statement?
(a) “I need to stay hydrated all the time.”
(b) “Even dental infections can lead to preterm labor.”
(c) “I should include frequent rest breaks if I travel.”
(d) “Cutting back on my smoking will not help my baby.”
Answer:
(d) “Cutting back on my smoking will not help my baby.”
Explanation:
Smoking is a major risk factor for preterm labor and decreased fetal weight. Clients struggling to quit should know decreasing cigarette use will help improve outcomes even if they cannot totally quit. Dehydration is a risk factor for preterm labor as is prolonged standing and remaining in one position. Infection anywhere in the body can lead to preterm labor through the inflammation pathway. While taking trips, frequent emptying of the bladder prevents infection and ambulates the woman.
Question 36.
Which statement by the client indicates an understanding of the teaching regarding the use of corticosteroids during preterm labor?
(a) “I will be taking corticosteroids until my baby’s due date so that he or she will have the best chance of doing well.”
(b) “The corticosteroids may help my baby’s lungs mature.”
(c) “The goal of the corticosteroids is to stop contractions and help me get to my due date.”
(d) “If I take corticosteroids, my baby will not have to spend any time in the neonatal intensive care unit when he or she is born.”
Answer:
(b) “The corticosteroids may help my baby’s lungs mature.”
Explanation:
Corticosteroids given IM have been shown to increase fetal lung maturity by increasing surfactant and reduce the risk of respiratory distress syndrome in premature infants. It is not a guarantee that a premature newborn would not have problems at birth that would require time in the neonatal intensive care unit. The administration of the corticosteroids is normally completed within 24 to 48 hours.
Question 37.
In which maternal locations would the nurse place the ultrasound transducer of the external electronic fetal heart rate monitor if a fetus at 34 weeks’ gestation is in the left occipitoanterior (LOA) position?
(a) near the symphysis pubis
(b) 2 inches (5.1 cm) above the umbilicus
(c) below the umbilicus on the left side
(d) at the level of the umbilicus
Answer:
(c) below the umbilicus on the left side
Explanation:
As the uterus contracts, the abdominal wall rises and, when external monitoring is used, presses against the transducer. This movement is transmitted into an electrical current, which is then recorded. With the fetus in the LOA position, the cardio transducer should be placed below the umbilicus on the side where the fetal back is located and uterine displacement during contractions is greatest. If the fetal back is near the symphysis pubis, the fetus is presenting as a transverse lie. If the fetus is in a breech position, the fetal back may be at or above the umbilicus.
Question 38.
When preparing a multigravid client at 34 weeks’ gestation experiencing preterm labor for the shake test performed on amniotic fluid, the nurse would instruct the client that this test is done to evaluate the maturity of which fetal system?
(a) urinary
(b) gastrointestinal
(c) cardiovascular
(d) pulmonary
Answer:
(d) pulmonary
Explanation:
The shake test helps determine the maturity of the fetal pulmonary system. The test is based on the fact that surfactant foams when mixed with ethanol. The more stable the foam, the more mature the fetal pulmonary system. A lecithin/sphingomyelin ratio is usually determined in conjunction with the shake test. Amniotic fluid volumes are used to evaluate the GI and urinary systems. Ultrasound to evaluate the cardiovascular system.
Question 39.
The nurse is planning care for a multigravid client hospitalized at 36 weeks gestation with a confirmed rupture of membranes and no evidence of labor. What prescription would the nurse anticipate from the primary health care provider (HCP)?
(a) frequent assessments of cervical dilation
(b) intravenous oxytocin administration
(c) vaginal cultures for Neisseria gonorrhoeae
(d) sonogram for amniotic fluid volume index
Answer:
(c) vaginal cultures for Neisseria gonorrhoeae
Explanation:
Because an intrauterine infection may occur when membranes have ruptured, vaginal cultures for N. gonorrhoeae, group B streptococcus, and chlamydia are usually taken. Prophylactic antibiotics may be prescribed to reduce the risk of infection in the newborn. Frequent vaginal examinations should be avoided because they can further increase the client’s risk for infection.
Intravenous oxytocin to initiate labor may be used if an infection occurs. Bed rest can sometimes prolong the pregnancy and prevent a preterm birth. A sonogram may be used to validate rupture of the membranes with an amniotic fluid index. However, it is not needed if the HCP has confirmed the rupture.
Question 40.
A multigravid client at 34 weeks’ gestation visits the hospital because she suspects that her water has broken. After testing the leaking fluid with nitrazine paper, the nurse confirms that the client’s membranes have ruptured when the paper turns which color?
(a) yellow
(b) white
(c) blue
(d) red
Answer:
(c) blue
Explanation:
If the client’s membranes have ruptured, the nitrazine paper will turn blue, an alkaline reaction. False positives may occur when the nitrazine paper is exposed to blood or semen. The definitive test for rupture of membranes is fern testing, where amniotic fluid is allowed to dry on a slide and then viewed under a microscope. Dried amniotic fluid will form a fern pattern. No other fluid forms this type of pattern.
Question 41.
A primigravid client at 30 weeks’ gestation has been admitted to the hospital with premature rupture of the membranes without contractions.
Her cervix is 2 cm dilated and 50% effaced. Which factor is most important for the nurse to assess next?
(a) red blood cell count
(b) degree of discomfort
(c) urinary output
(d) temperature
Answer:
(d) temperature
Explanation:
Premature rupture of the membranes is commonly associated with chorioamnionitis, or an infection. A priority assessment for the nurse to make is to document the client’s temperature every 2 to 4 hours. Temperature elevation may indicate an infection.
Lethargy and an elevated white blood cell count also indicate an infection. The red blood cell count would provide information related to anemia, not infection. The client is not in labor. Therefore, assessing the degree of discomfort is not a priority at this time. Urinary output is not a reliable indicator of an infection such as chorioamnionitis.
Question 42.
A multigravid client at 34 weeks’ gestation with premature rupture of the membranes tests positive for group B streptococcus. The client is having contractions every 4 to 6 minutes. Her vital signs are as follows: blood pressure, 120/80 mm Hg; temperature, 100°F (37.8°C); pulse, 100 bpm; respirations,
18 breaths/min. Which medication would the nurse expect the primary health care provider (HCP) to prescribe?
(a) intravenous penicillin
(b) intravenous gentamicin sulfate
(c) intramuscular betamethasone
(d) intramuscular cefaclor
Answer:
(a) intravenous penicillin
Explanation:
Because group B streptococcus is a gram-positive bacterium, the HCP probably will prescribe intravenous penicillin to treat the mother’s infection and prevent fetal infection. Gentamicin sulfate, which acts on gram-negative bacteria, would be inappropriate. Administering a corticosteroid, such as betamethasone, is inappropriate because the premature rupture of the membranes enhances fetal lung maturity.
The lack of amniotic fluid causes early maturation of lung tissue. Cefaclor, which is available only in the oral form, is used for upper and lower respiratory tract infections and urinary tract infections by gram-negative staphylococci.
Question 43.
A primigravid client at 36 weeks’ gestation with premature rupture of the membranes is to be discharged home on bed rest with follow-up by the nurse. After instruction about care while at home, which client statement indicates effective teaching?
(a) “It is permissible to douche if the fluid irritates my vaginal area.”
(b) “I can take either a tub bath or a shower when I feel like it.”
(c) “I should limit my fluid intake to < 1 quart (0.95 L) daily.”
(d) “I should contact the health care provider if my temperature is 100.4°F (38°C) or higher.”
Answer:
(d) “I should contact the health care provider if my temperature is 100.4°F (38°C) or higher.”
Explanation:
Because of the client’s increased risk for infection, successful teaching is indicated when the client states that she will contact the primary care provider if her temperature is 100.4°F (38°C) or greater. The client should be instructed to monitor her temperature twice daily.
The client should refrain from coitus, douching, and tub bathing, which can increase the potential for infection. Showering is permitted because water in the shower does not enter the vagina and increase the risk of infection. A fluid intake of at least 2 L daily is recommended to prevent potential urinary tract infection.
Question 44.
A primigravid client at 34 weeks’ gestation is experiencing contractions every 3 to 4 minutes lasting for 35 seconds. Her cervix is 2 cm dilated and 50% effaced. While the nurse is assessing the client’s vital signs, the client says, “I think my bag of water just broke.” Which intervention would the nurse do first?
(a) Check the status of the fetal heart rate.
(b) Turn the client to her right side.
(c) Test the leaking fluid with nitrazine paper.
(d) Perform a sterile vaginal examination.
Answer:
(a) Check the status of the fetal heart rate.
Explanation:
The priority is to determine whether a prolapsed cord has occurred as a result of the spontaneous rupture of membranes. The nurse’s first action should be to check the status of the fetal heart rate. Complications of premature rupture of the membranes include a prolapsed cord or increased pressure on the fetal umbilical cord inhibiting fetal nutrient supply.
Variable decelerations or fetal bradycardia may be seen on the external fetal monitor. The cord also may be visible. Turning the client to her right side is not necessary. If the cord does prolapse, the client should be placed in a knee-to- chest or Trendelenburg position. Checking the fluid with nitrazine paper and vaginal examination are appropriate once the status of the fetus has been evaluated.
Question 45.
The antenatal clinic nurse is educating a client with gestational diabetes soon after diagnosis. Evaluation for this client session will include which outcome? Select all that apply.
(a) The client states the need to maintain blood glucose levels between 70 and 110 mg/dL (3.9 to 6.2 mmol/L).
(b) The client describes her planned walking program while pregnant.
(c) The client will strive to maintain a hemoglobin AlC of < 6%.
(d) The client verbalizes the need to maintain a dietary intake of < 1,500 cal/day to prevent hyperglycemia.
(e) The client will continue taking her prenatal vitamins, iron, and folic acid.
Answer:
(a) The client states the need to maintain blood glucose levels between 70 and 110 mg/dL (3.9 to 6.2 mmol/L).
(b) The client describes her planned walking program while pregnant.
(c) The client will strive to maintain a hemoglobin AlC of < 6%.
(e) The client will continue taking her prenatal vitamins, iron, and folic acid.
Explanation:
(a), (b), (c), (e) The gestational diabetic needs to maintain blood glucose levels as close to “normal” as the nondiabetic pregnant woman. Walking is an excellent form of exercise for anyone and works well for pregnant diabetics as it burns calories, accelerates the heart rate, and as a result maintains the blood sugar at a lower level.
During pregnancy, continuously high blood glucose levels measured by a hemoglobin AlC of > 6 mg/dL (60 g/L) carry risks for the dyad. The suggested diet for a gestational diabetic is 1,800 to 2,400 cal/day to avoid the body breaking down maternal fat to maintain blood glucose levels. Continuing prenatal vitamins, iron, and folic acid (800 mcg/day] are general nutritional recommendations for pregnancy.
Question 46.
A 27-year-old primigravid client with insulin-dependent diabetes at 34 weeks’ gestation undergoes a nonstress test, the results of which are documented as reactive. What should the nurse tell the client that the test results indicate?
(a) A contraction stress test is necessary.
(b) The nonstress test should be repeated.
(c) Chorionic villus sampling is necessary.
(d) There is evidence of fetal well-being.
Answer:
(d) There is evidence of fetal well-being.
Explanation:
The nonstress test is considered reactive when two or more fetal heart rate accelerations of at least 15 bpm occur (from a baseline fetal heart rate of 120 to 160 bpm], along with fetal movement, during a 10- to 20-minute period. A reactive nonstress test indicates fetal heart rate accelerations and well-being. There is no indication for further evaluation (such as a contraction stress test).
However, contraction stress tests are commonly scheduled for pregnant clients with insulin-dependent diabetes in the latter part of pregnancy and are repeated periodically until birth. Chorionic villus sampling is usually performed early in the pregnancy to detect fetal abnormalities.
Question 47.
A primigravid client with insulin-dependent diabetes tells the nurse that the contraction stress test performed earlier in the day was suspicious.
The nurse interprets this test result as showing which fetal heart rate pattern?
(a) frequent late decelerations
(b) decreased fetal movement
(c) inconsistent late decelerations
(d) lack of fetal movement
Answer:
(c) inconsistent late decelerations
Explanation:
A contraction stress test is used to evaluate fetal well-being during a simulated labor. A suspicious contraction stress test indicates inconsistent late deceleration patterns requiring further evaluation. A negative contraction stress test indicates no late decelerations and is the desired outcome. A positive contraction stress test indicates fetal compromise with frequent late decelerations.
Fetal movements are one of the parameters of a biophysical profile and are detected with nonstress testing. Decreased or absent fetal movements may indicate central nervous system dysfunction or prematurity. Lack of fetal movement or decreased fetal movement is not associated with contraction stress testing.
Question 48.
Which statement about a fetal biophysical profile would be incorporated into the teaching plan for a primigravid client with insulin-dependent diabetes?
(a) It determines fetal lung maturity.
(b) It is noninvasive using real-time ultrasound.
(c) It will correlate with the newborn’s Apgar score.
(d) It requires the client to have an empty bladder.
Answer:
(b) It is noninvasive using real-time ultrasound.
Explanation:
The fetal biophysical profile, a noninva- sive test using real-time ultrasound, assesses five parameters: fetal heart rate reactivity, fetal breathing movements, gross fetal body movements, fetal tone, and amniotic fluid volume. Fetal heart rate reactivity is determined by a nonstress test; the other four parameters are determined by ultrasound scanning.
The results are available as soon as the test is com-pleted and interpreted. The lecithin-sphingomyelin ratio is used to determine fetal lung maturity. Although the fetal biophysical profile is useful in predicting which fetuses may be at greater risk for compromise, there is no correlation with the newborn’s Apgar score. The biophysical score is some-times referred to as the fetal Apgar score. A score of 8 to 10 indicates fetal well-being. Use of an ultrasound requires the mother to have a full bladder.

Question 49.
A 30-year-old multigravid client at 8 weeks gestation has a history of insulin-dependent diabetes since age 20. When explaining the importance of blood glucose control during pregnancy, the nurse should tell the client what will occur regarding the client’s insulin needs during the first trimester.
(a) They will increase.
(b) They will decrease.
(c) They will remain constant.
(d) They will be unpredictable.
Answer:
(b) They will decrease.
Explanation:
During the first trimester, it is not unusual for insulin needs to decrease, commonly as a result of nausea and vomiting. Progressive insulin resistance is characteristic of pregnancy, particularly in the second half of pregnancy.
It is not unusual for insulin needs to increase by as much as four times the nonpregnant dose after about the 24th week of gestation. This resistance is caused by the production of human placental lactogen, also called human chorionic somatotropin, by the placenta and by other hormones, such as estrogen and progesterone, which are insulin antagonists.
Question 50.
The nurse explains the complications of pregnancy that occur with diabetes to a primigravid client at 10 weeks’ gestation who has a 5-year history of insulin-dependent diabetes. Which complication, if stated by the client, indicates the need for additional teaching?
(a) Candida albicans infection
(b) twin-to-twin transfusion
(c) polyhydramnios
(d) preeclampsia
Answer:
(b) twin-to-twin transfusion
Explanation:
Clients who are pregnant and have diabetes are not at greater risk for multifetal pregnancy and subsequent twin-to-twin transfusion unless they have undergone fertility treatments. The pregnant diabetic client is at higher risk for complications such as infection, polyhydramnios, ketoacidosis, and preeclampsia, compared with the pregnant non-diabetic client.
Question 51.
When developing a teaching plan for a primigravid client with insulin-dependent diabetes about monitoring blood glucose control and insulin dosages at home, the nurse would expect to include which desired target range for blood glucose levels?
(a) 40 to 60 mg/dL (2.2 to 3.3 mmol/L) between 14:00 and 16:00 hours
(b) 70 to 100 mg/dL (3.3 to 5.6 mmol/L) before meals and bedtime snacks
(c) 110 to 140 mg/dL (6.2 to 7.8 mmol/L) before meals and bedtime snacks
(d) 140 to 160 mg/dL (7.8 to 8.9 mmol/L) 1 hour after meals
Answer:
(b) 70 to 100 mg/dL (3.3 to 5.6 mmol/L) before meals and bedtime snacks
Explanation:
The goal is to maintain blood plasma glucose levels at 70 to 100 mg/dL [3.5 to 5.6 mmol/L] before meals and bedtime snacks. Below 60 mg/db (5.6 mmol/L) indicates hypoglycemia. A range of 110 to 140 mg/dL (6.2 to 7.8 mmol/L) suggests hyperglycemia. The target range for 1 hour after meals is 100 to 120 mg/dL (5.6 to 6.7 mmol/L).
Question 52.
When teaching a primigravid client with diabetes about common causes of hyperglycemia during pregnancy, the nurse would include which information?
(a) fetal macrosomia
(b) decreased fetal insulin
(c) maternal infection
(d) gestational hypertension
Answer:
(c) maternal infection
Explanation:
Maternal infection is the most common cause of maternal hyperglycemia and can lead to ketoacidosis, coma, and death. The client should notify the health care provider (HCP) [JJ immediately if she experiences symptoms of an infection. Fetal macrosomia results from maternal hyperglycemia but does not cause it.
Fetal insulin production increases as maternal glucose crosses the placenta. This helps control glucose in the fetus but has no bearing on maternal glucose levels. Gestational hypertension does not cause maternal hyperglycemia during pregnancy.
Question 53.
After teaching a diabetic primigravida about symptoms of hyperglycemia and hypoglycemia, the nurse determines that the client understands the instruction when she says that hyperglycemia may be manifested by which symptom?
(a) dehydration
(b) pallor
(c) sweating P
(d) nervousness
Answer:
(a) dehydration
Explanation:
Dehydration, polyuria, fatigue, flushed hot skin, dry mouth, and drowsiness are manifestations of hyperglycemia. Hyperglycemia is a medical emergency and requires immediate action to prevent maternal and fetal mortality. Pallor, sweating, and nervousness are early signs of hypoglycemia, not hyperglycemia.
Question 54.
At 38 weeks’ gestation, a primigravid client with poorly controlled diabetes and severe preeclampsia is admitted for a cesarean birth. The nurse explains to the client that birth helps to prevent which complication?
(a) neonatal hyperbilirubinemia
(b) congenital anomalies
(c) perinatal asphyxia
(d) stillbirth
Answer:
(d) stillbirth
Explanation:
Stillbirths caused by placental insufficiency occur with increased frequency in women with diabetes and severe preeclampsia. Clients with poorly controlled diabetes may experience unanticipated stillbirth as a result of premature aging of the placenta. Therefore, labor is commonly induced in these clients before term. If induction of labor fails, a cesarean section is necessary. Induction and cesarean section do not prevent neonatal hyperbilirubinemia, congenital anomalies, or perinatal asphyxia.
Question 55.
A primigravid client with diabetes at 39 weeks’ gestation is seen in the high-risk clinic. The primary health care provider (HCP) estimates that the fetus weighs at least 10 lb (4,500 g). The client asks, “What causes the baby to be so large?” The nurse’s response is based on the understand-ing that fetal macrosomia is most related to which factor?
(a) family history of large infants
(b) fetal anomalies
(c) maternal hyperglycemia
(d) maternal hypertension
Answer:
(c) maternal hyperglycemia
Explanation:
Maternal hyperglycemia and poor control of the mother’s diabetes mellitus have been implicated in fetal macrosomia. When the mother is hyperglycemic, large amounts of amino acids, free fatty acids, and glucose are transferred to the fetus. Although maternal insulin does not cross the placenta, the fetal pancreas responds by hypertrophy of the islet cells of the pancreas.
The islet cells produce large amounts of insulin, which acts as a growth hormone. A family history of large infants usually is not the reason for large-for-gestational-age fetuses in diabetic mothers. Maternal hypertension is associated with small-for-gestational-age fetuses because of vasoconstriction of the maternal and placental blood vessels.
Question 56.
With plans to breastfeed her neonate, a pregnant client with insulin-dependent diabetes asks the nurse about insulin needs during the postpartum period. Which statement about postpartum insulin requirements for breastfeeding mothers should the nurse include in the explanation?
(a) They fall significantly in the immediate postpartum period.
(b) They remain the same as during the labor process.
(c) They usually increase in the immediate postpartum period.
(d) They need constant adjustment during the first 24 hours.
Answer:
(a) They fall significantly in the immediate postpartum period.
Explanation:
Insulin needs fall significantly during the first 24 hours postpartum because the client has usually been on nothing-by-mouth status for a period of time during labor and the labor process has used maternal glycogen stores. If the client breastfeeds, lower blood glucose levels decrease the insulin requirements. With insulin resistance gone, the client commonly needs little or no insulin during the immediate postpartum period.
Although the need for insulin decreases during the intrapartum period, the insulin requirements fall further during the first 24 hours postpartum. After the first 24 hours postpartum, insulin requirements may fluctuate markedly, needing adjustment during the next few days as the mother’s body returns to a nonpregnant state.
Question 57.
After instruction of a primigravid client at 8 weeks’ gestation diagnosed with class I heart disease about self-care during pregnancy, which client statement would indicate the need for additional teaching?
(a) “I should avoid being near people who have a cold.”
(b) “I may be given antibiotics during my pregnancy.”
(c) “I should reduce my intake of protein in my diet.”
(d) “I should limit my salt intake at meals.”
Answer:
(c) “I should reduce my intake of protein in my diet.”
Explanation:
The client needs a diet that is adequate in protein and calories to prevent anemia, which can place additional strain on the cardiac system, further compromising the client’s cardiac status. The client should avoid contact with people who have infections because of the increased risk for developing endocarditis. The client may need antibiotics during the pregnancy to prevent endocarditis. Limiting sodium intake can help to prevent excessive expansion of blood volume and decrease cardiac workload.
Question 58.
While caring for a primigravid client with class II heart disease at 28 weeks’ gestation, the nurse would instruct the client to contact her primary health care provider (HCP) immediately if the client experiences which symptom?
(a) mild ankle edema
(b) emotional stress on the job
(c) weight gain of 1 lb (0.45 kg) in 1 week
(d) dyspnea at rest
Answer:
(d) dyspnea at rest
Explanation:
Clients with class II heart disease have dyspnea upon exertion but not at rest. Dyspnea at rest would indicate a change in condition that must be reported immediately because it may be indicative of increasing congestive heart failure. Mild ankle edema in the third trimester is a common finding. However, generalized or pitting edema, suggesting increasing congestive heart failure, must be reported immediately.
Emotional stress on the job increases cardiac demand. However, it needs to be reported only if the client experiences symptoms, such as palpitations or irregular heart rate, indicating heart failure related to the increased stress. Weight gain of 1 lb (0.45 kg) per week is a normal finding during the third trimester.
Question 59.
When developing the collaborative plan of care with the health care provider (HCP) for a multi- gravid client at 10 weeks’ gestation with a history of cardiac disease who was being treated with digitalis therapy before this pregnancy, the nurse should instruct the client about which modification regarding the client’s drug therapy regimen?
(a) possible need for an increased dosage
(b) need for weekly drug level monitoring
(c) switching to a different medication
(d) addition of a diuretic to the regimen
Answer:
(a) possible need for an increased dosage
Explanation:
Clients on cardiac medications may need dosage increases as their blood volume increases. Drug level monitoring may be needed after dose changes or if the client presents with toxicity, but weekly monitoring is unnecessary. The medication would be switched only if digitalis toxicity occurs. A diuretic is added only if congestive heart failure is not controlled by sodium and activity restrictions.
Question 60.
Which anticoagulants would the nurse expect to administer when caring for a primigravid client at 12 weeks’ gestation who has class II cardiac disease due to mitral valve stenosis?
(a) heparin
(b) warfarin
(c) enoxaparin
(d) ardeparin
Answer:
(a) heparin
Explanation:
Although there is no completely safe anticoagulant therapy during pregnancy, heparin is typically the drug of choice. Warfarin, a pregnancy category D drug, can cause fetal malformations. Enoxaparin is sometimes used, but clients are typically switched to heparin near labor because enoxa-parin used along with spinal or epidural anesthesia presents an increased risk of bleeding in the epidural or spinal space. Ardeparin also can cause fetal malformations.
Question 61.
A primigravid client with class II heart disease who is visiting the clinic at 8 weeks’ gestation tells the nurse that she has been maintaining a low- sodium, 1,800-cal diet. Which instruction should the nurse give the client?
(a) Avoid folic acid supplements to prevent megaloblastic anemia.
(b) Severely restrict sodium intake throughout the pregnancy.
(c) Take iron supplements with milk to enhance absorption.
(d) Increase caloric intake to 2,200 calories daily to promote fetal growth.
Answer:
(d) Increase caloric intake to 2,200 calories daily to promote fetal growth.
Explanation:
The client can continue a low-sodium diet but should increase the caloric intake to 2,200 calories daily to provide adequate nutrients to support fetal growth and development. Folic acid supplements, a standard component of care, are used to prevent folic acid deficiency, which is associated with megaloblastic anemia during pregnancy.
Severe restriction of sodium intake is not recommended because sodium is necessary to maintain fluid volume. Iron supplements should be taken with acidic foods and fluids (e.g., citrus juices) for maximum absorption. Milk decreases the absorption of iron.
Question 62.
On arrival at the emergency department, a client tells the nurse that she suspects that she may be pregnant but has been having a small amount of bleeding and has severe pain in the lower abdomen. The client’s blood pressure is 70/50 mm Hg, and her pulse rate is 120 bpm. The nurse notifies the primary health care provider (HCP) immediately because of the possibility of which complication?
(a) ectopic pregnancy
(b) abruptio placentae
(c) gestational trophoblastic disease
(d) complete abortion
Answer:
(a) ectopic pregnancy
Explanation:
The client’s signs and symptoms indicate a probable ectopic pregnancy, which can be confirmed by ultrasound examination or by cul- docentesis. The HCP 03 is notified immediately because hypovolemic shock may develop without external bleeding. Once the fallopian tube ruptures, blood will enter the pelvic cavity, resulting in shock.
Abruptio placentae would be manifested by a board-like uterus in the third trimester. The gestational trophoblastic disease would be suspected if the client exhibited no fetal heart rate and symptoms of pregnancy-induced hypertension before 20 weeks’ gestation. A client with a complete abortion would exhibit a normal pulse and blood pressure with scant vaginal bleeding.
Question 63.
The nurse is assessing a multigravid client at 12 weeks’ gestation who has been admitted to the emergency department with sharp right-sided abdominal pain and vaginal spotting. Which information should the nurse obtain about the client’s history? Select all that apply.
(a) history of sexually transmitted infections
(b) number of sexual partners
(c) last menstrual period
(d) cesarean section
(e) contraceptive use
Answer:
(a) history of sexually transmitted infections
(b) number of sexual partners
(c) last menstrual period
(e) contraceptive use
Explanation:
(a), (b), (c), (e) The client may be experiencing an ectopic pregnancy. Contributing factors to an ectopic pregnancy include a prior history of sexually transmitted infection that can scar the fallopian tubes. Multiple sex partners increase the risk of sexually transmitted infections.
Knowledge of the client’s last menstrual period and contraceptive use may support or rule out the possibility of an ectopic pregnancy. The client’s history of cesarean sections would not contribute information valuable to the client’s current situation or potential diagnosis of ectopic pregnancy.
Question 64.
Before surgery to remove an ectopic pregnancy and the fallopian tube, which sign or symptom would alert the nurse to the possibility of tubal rupture?
(a) amount of vaginal bleeding and discharge
(b) profuse sweating
(c) slow, bounding pulse rate of 80 bpm
(d) marked abdominal edema
Answer:
(b) profuse sweating
Explanation:
Diaphoresis, or profuse sweating, indicates shock, which occurs if the tube ruptures. Other common symptoms of tubal rupture include severe knife-like lower quadrant abdominal pain, referred shoulder pain, and falling blood pressure. The amount of vaginal bleeding that is evident is a poor estimate of actual blood loss. Slight vaginal bleeding, commonly described as spotting, is common. A rapid, thready pulse, a symptom of shock, is more common with tubal rupture than a slow, bounding pulse. Abdominal edema is a late sign of a tubal rupture in ectopic pregnancy.
Question 65.
A multigravid client diagnosed with a probable ruptured ectopic pregnancy is scheduled for emergency surgery. In addition to monitoring the client’s blood pressure before surgery, which factor is most important for the nurse to assess?
(a) uterine cramping
(b) abdominal distention
(c) hemoglobin and hematocrit
(d) pulse rate
Answer:
(d) pulse rate
Explanation:
Fallopian tube rupture is an emergency situation because of extensive bleeding into the peritoneal cavity. Shock soon develops if precautionary measures are not taken. The nurse readying a client for surgery should be especially careful to monitor blood pressure and pulse rate for signs of impending shock. The nurse should be prepared to administer fluids, blood, or plasma expanders as necessary through an intravenous line that should already be in place.
Because the fertilized ovum has implanted outside the uterus, uterine cramping is unlikely. However, abdominal tenderness or knife-like pain may occur. Abdominal fullness may be present, but abdominal distention is rare unless peritonitis has developed. Although the hemoglobin and hemato¬crit may be checked routinely before surgery, the laboratory results may not truly reflect the presence or degree of acute hemorrhage.
Question 66.
A 36-year-old multigravid client is admitted to the hospital with possible ruptured ectopic pregnancy. When obtaining the client’s history, which finding would be most important to identify as a predisposing factor?
(a) urinary tract infection
(b) marijuana use during pregnancy
(c) episodes of pelvic inflammatory disease
(d) use of estrogen-progestin contraceptives
Answer:
(c) episodes of pelvic inflammatory disease
Explanation:
Anything that causes a narrowing or constriction in the fallopian tubes so that a fertilized ovum cannot be properly transported to the uterus for implantation predisposes an ectopic pregnancy. Pelvic inflammatory disease is the most common cause of constricted or narrow tubes. Developmental defects are other possible causes.
Ectopic pregnancy is not related to urinary tract infections. Use of marijuana during pregnancy is not associated with ectopic pregnancy, but its use can result in cognitive reduction if the mother’s use during pregnancy is extensive. Progestin-only contraceptives and intrauterine devices have been associated with ectopic pregnancy.
Question 67.
A multigravid client is admitted to the hospital with a diagnosis of ectopic pregnancy. The nurse anticipates that because the client’s fallopian tube has not yet ruptured, which medication may be prescribed?
(a) progestin contraceptives
(b) medroxyprogesterone
(c) methotrexate
(d) dyphylline
Answer:
(c) methotrexate
Explanation:
Because the fallopian tube has not yet ruptured, methotrexate may be given, followed by leucovorin. This chemotherapeutic agent attacks the fast-growing zygote and trophoblast cells. RU-486 is also effective. A hysterosalpingogram is usually performed after chemotherapy to determine whether the tube is still patent. Progestin-only contraceptives and medroxyprogesterone are ineffective in clearing the fallopian tube. Dyphylline is a bronchodilator and is not used.
Question 68.
After the instruction of a primigravid client at 8 weeks’ gestation about measures to overcome early morning nausea and vomiting, which client statement indicates the need for additional teaching?
(a) “I will eat dry crackers or toast before arising in the morning.”
(b) “I will drink adequate fluids separate from my meals or snacks.”
(c) “I will eat two large meals daily with frequent protein snacks.”
(d) ‘‘I will snack on a small amount of carbohydrates throughout the day.”
Answer:
(c) “I will eat two large meals daily with frequent protein snacks.”
Explanation:
The client needs further instructions when she says she should eat two meals a day with frequent protein snacks to decrease nausea and vomiting. The client should eat more frequent, smaller meals, with frequent carbohydrate snacks to decrease nausea and vomiting. Eating dry crackers or toast before arising, consuming fluids separately from meals, and avoiding greasy or spicy foods may also help to decrease nausea and vomiting.
Question 69.
The prenatal client tells the nurse that she has been eating ginger cookies to treat her nausea and vomiting. Which response by the nurse is best?
(a) “When consumed as a spice in foods, ginger is generally considered safe in pregnancy.”
(b) “It is safer to use a prescription medication than eating ginger while you are pregnant.”
(c) “Wait at least 2 hours to take your prenatal vitamin after eating ginger cookies.”
(d) “You should immediately stop eating ginger-containing foods.”
Answer:
(a) “When consumed as a spice in foods, ginger is generally considered safe in pregnancy.”
Explanation:
The herbal supplement ginger is taken to reduce nausea and vomiting. When consumed as a spice in foods, such as ginger cookies, there is general consensus that ginger is safe. Prescription medications may be necessary to treat severe nausea and vomiting in pregnancy, but they can carry risks such as sedation. Prenatal vitamins should be taken when clients experience the least nausea rather than waiting a specific time after food. There is no known pregnancy risk from eating ginger as a spice in foods.
Question 70.
A multigravid client thought to be at 14 weeks’ gestation reports that she is experiencing such severe morning sickness that she “has not been able to keep anything down for a week.” The nurse should assess for signs and symptoms of which condition.
(a) hypercalcemia
(b) hypobilirubinemia
(c) hypokalemia
(d) hyperglycemia
Answer:
(c) hypokalemia
Explanation:
Gastrointestinal secretion losses from excessive vomiting, diarrhea, and excessive perspiration can result in hypokalemia, hyponatremia, decreased chloride levels, metabolic alkalosis, and eventual acidosis if precautionary measures are not taken. Ketones may be present in the urine. Dehydration can lead to poor maternal and fetal outcomes. Persistent vomiting can lead to hypocalcemia, not hypercalcemia.
Hyperbilirubinemia, not hypobilirubinemia, is typical in clients with hyperemesis. Persistent vomiting may affect liver function and subsequently the excretion of bilirubin from the body. Hypoglycemia, not hyperglycemia, may occur as a result of decreased intake of food and fluids, decreased metabolism of nutrients, and excessive vomiting.
Question 71.
A multigravid client is admitted at 16 weeks’ gestation with a diagnosis of hyperemesis gravidarum. The nurse should explain to the client that hyperemesis gravidarum is thought to be related to high levels of which hormone?
(a) progesterone
(b) estrogen
(c) somatotropin
(d) aldosterone
Answer:
(b) estrogen
Explanation:
Although the cause of hyperemesis is still unclear, it is thought to be related to high estrogen and human chorionic gonadotropin levels or to trophoblastic activity or gonadotropin production. Hyperemesis is also associated with infectious conditions, such as hepatitis or encephalitis, intestinal obstruction, peptic ulcer, and hydatidiform mole. Progesterone is a relaxant used during pregnancy and does not stimulate vomiting. Somatotropin is a growth hormone used in children. Aldosterone is a male hormone.
Question 72.
The primary health care provider (HCP) pre-scribes 1,000 mL of Ringer’s lactate intravenously over an 8-hour period for a 29-year-old primigravid client at 16 weeks’ gestation with hyperemesis. The drip factor is 12 gtts/mL. The nurse should administer the IV infusion at how many drops per minute? Record your answer using one decimal place.
Answer:
\(\frac{\text { gtts }}{\min }=\frac{12 \mathrm{gtts}}{1 \mathrm{~mL}} \times \frac{1,000 \mathrm{~mL}}{8 \mathrm{~h}} \times \frac{1 \mathrm{~h}}{60 \mathrm{~min}} \)= 25 gtts/min
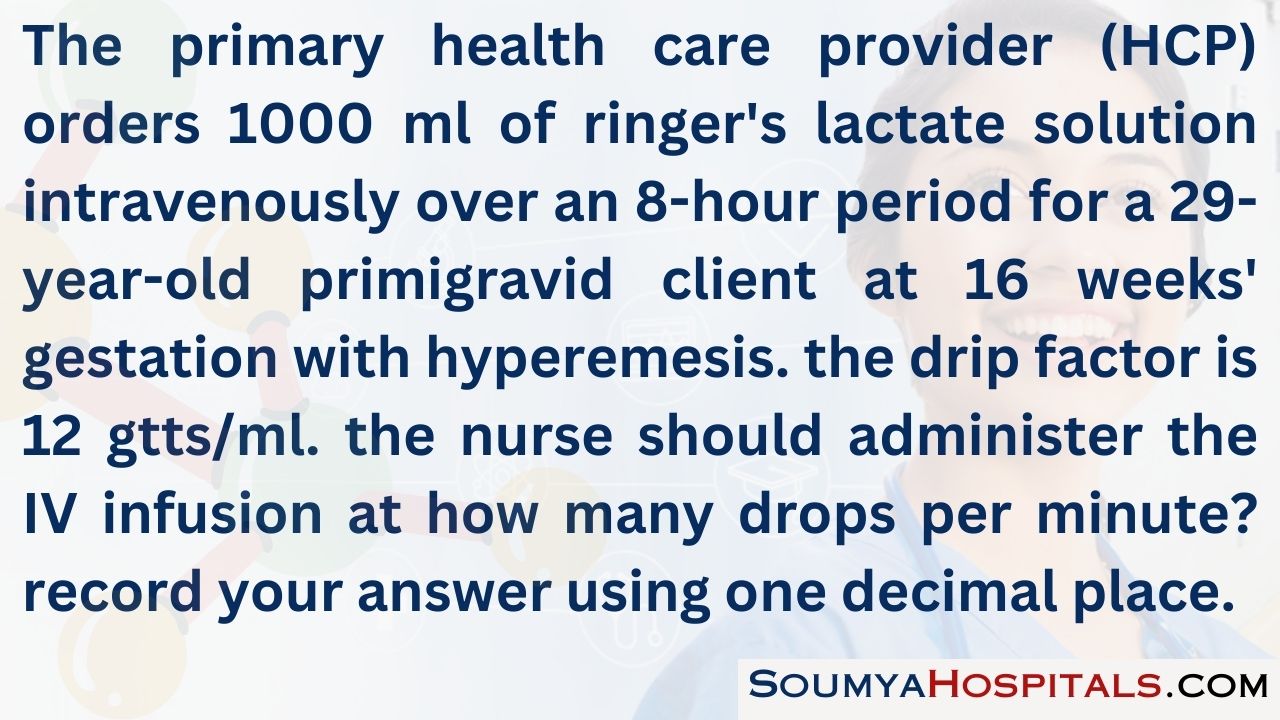
Question 73.
In caring for a pregnant client with hyperemesis gravidarum, which is the priority nursing intervention?
(a) providing adequate sleep for the client
(b) correction of fluid-electrolyte imbalance
(c) reviewing dietary choices and food intake
(d) acetaminophen suppositories
Answer:
(b) correction of fluid-electrolyte imbalance
Explanation:
Clients with hyperemesis gravidarum can experience severe vomiting. Some clients will require hospital care to treat dehydration including intravenous fluids, antiemetics, and enteral nutrition. Sleep and dietary choices are important to care but not the priority intervention. Acetaminophen suppositories are not indicated for the care of hyperemesis gravidarum.
Question 74.
A client at 15 weeks’ gestation presents at the obstetrical triage unit with dark brown vaginal bleeding and continuous nausea and vomiting. Her blood pressure is 142/98 mm Hg, and her fundal height is 19 cm. Which prescription is most important for the nurse to request from the primary care provider?
(a) a transfer to the antenatal unit
(b) NPO status for 24 hours
(c) intravenous magnesium sulfate
(d) stat ultrasound
Answer:
(d) stat ultrasound
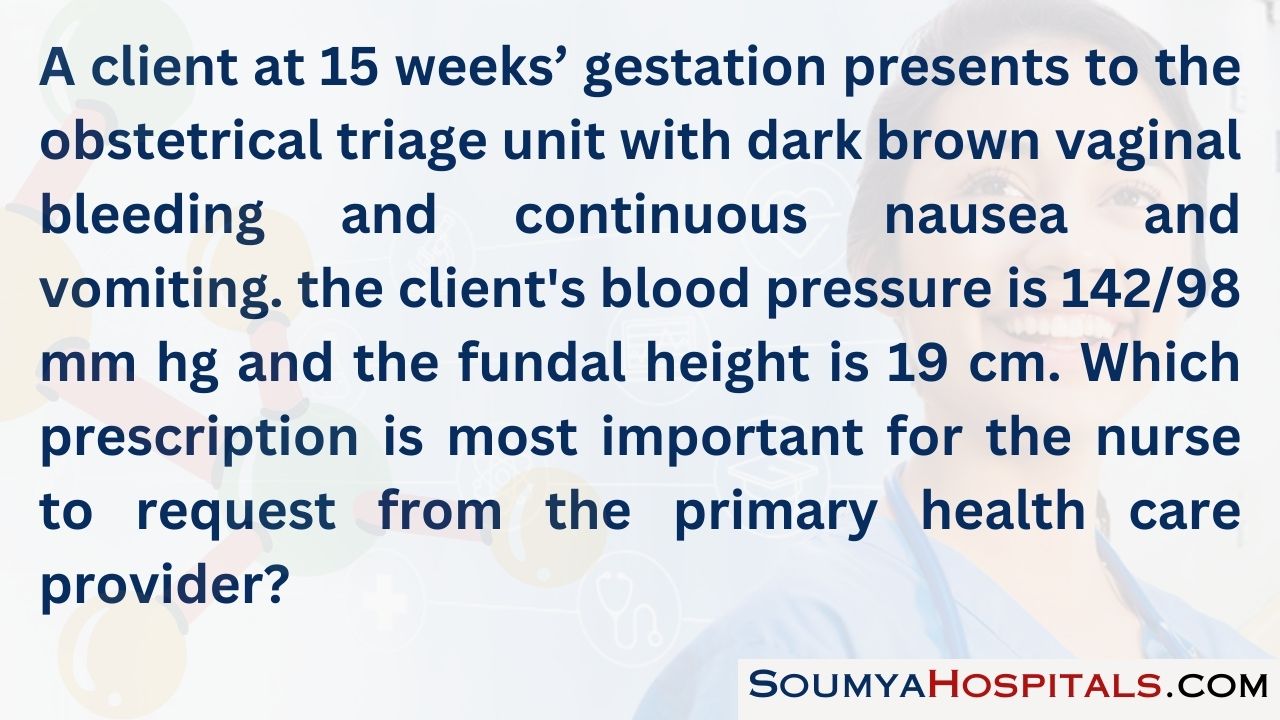
Explanation:
The nurse should prepare the client for an ultrasound to determine the cause of the symptoms. Elevated blood pressure at this point in the pregnancy could indicate chronic hypertension as well as hydatidiform mole. The fundal height of 19 cm is higher than is typically found at 15 weeks’ gestation and is indicative of a molar pregnancy (hydatidiform mole). The dark brown vaginal bleeding in isolation could indicate an abortion but when placed in context of the other symptoms is likely related to a hydatidiform mole.
The continuous nausea and vomiting is abnormal at this point in the pregnancy and can be a result of the high levels of progesterone from a molar pregnancy. There is no fetus involved; the blood pressure elevation and the continuous nausea and vomiting will resolve with evacuation of the mole, negating the need for magnesium sulfate therapy and placing the client on NPO status. Transferring the client to the antenatal unit is premature before a diagnosis has been made.
Question 75.
A 38-year-old client at about 14 weeks’ gestation is admitted to the hospital with a diagnosis of complete hydatidiform mole. Soon after admission, the nurse would assess the client for which signs and symptoms?
(a) gestational hypertension
(b) gestational diabetes
(c) hypothyroidism
(d) polycythemia
Answer:
(a) gestational hypertension
Explanation:
Hydatidiform mole is suspected when the following are present: gestational hypertension before the 24th week of gestation, brownish or prune-colored vaginal bleeding, anemia, absence of fetal heart tones, passage of hydropic vessels, uterine enlargement greater than expected for gesta-tional age, and increased human chorionic gonadotropin levels.
Gestational diabetes is related to an increased risk of preeclampsia and urinary tract infections, but it is not associated with hydatidiform mole. Hyperthyroidism, not hypothyroidism, occurs occasionally with hydatidiform mole. If it does occur, it can be a serious complication, possibly life threatening to the mother and fetus from car-diac problems. Polycythemia is not associated with hydatidiform mole. Rather, anemia from blood loss is associated with molar pregnancies.
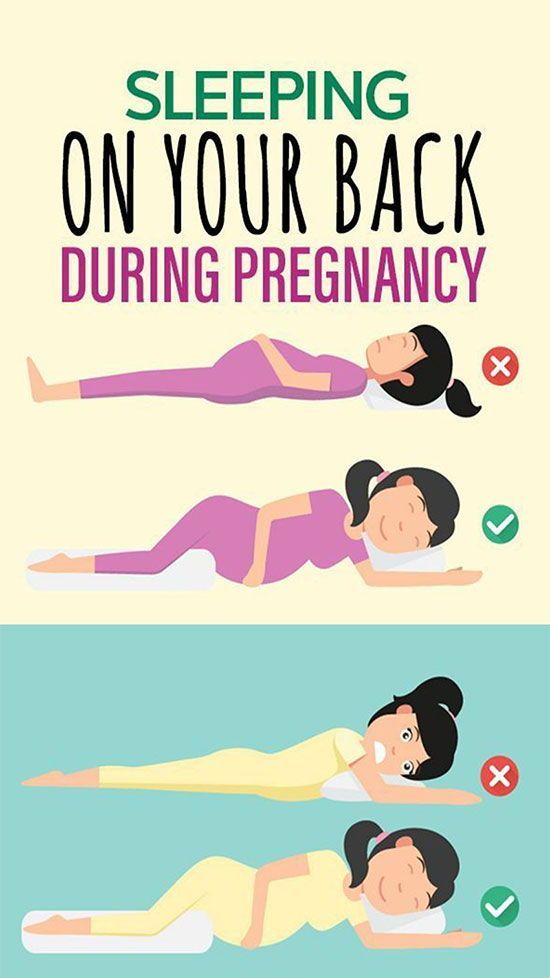
Question 76.
After a dilatation and curettage (D&C) to evacuate a molar pregnancy, assessing the client for which signs and symptoms would be most important?
(a) urinary tract infection
(b) hemorrhage
(c) abdominal distention
(d) chorioamnionitis
Answer:
(b) hemorrhage
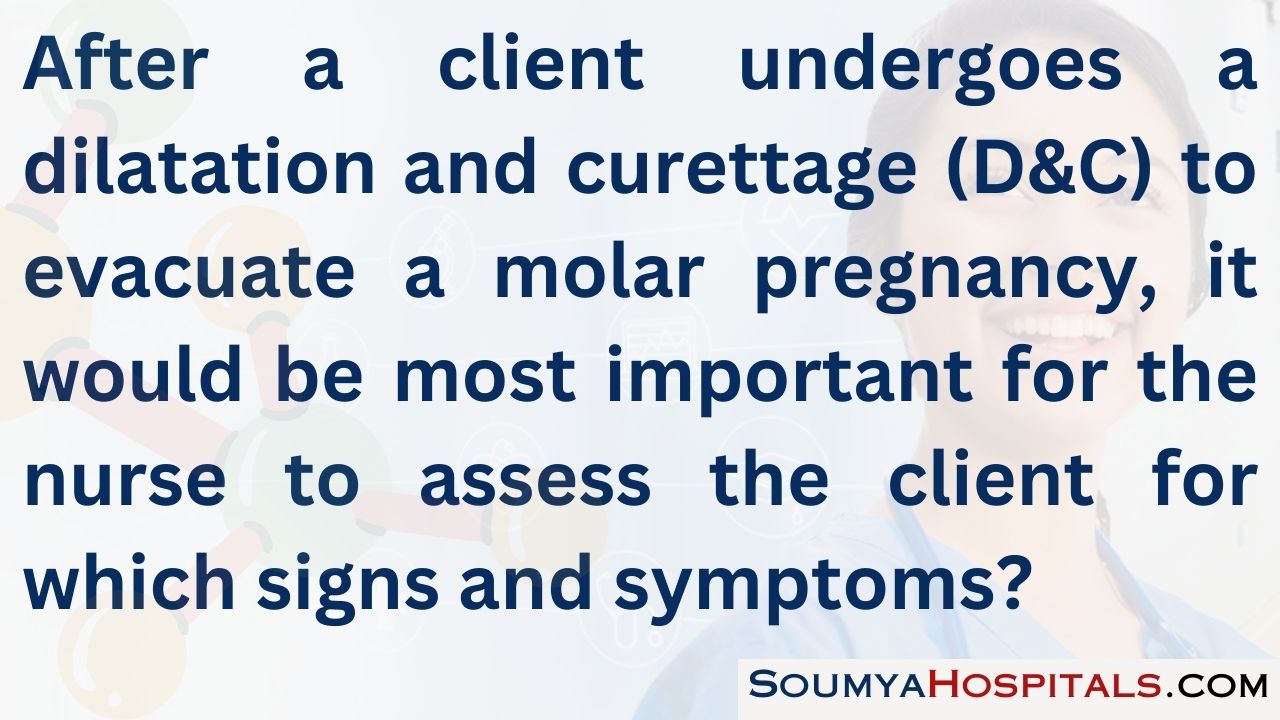
Explanation:
After D&C evacuates a molar pregnancy, the nurse should assess the client’s vital signs and monitor for signs of hemorrhage because the surgical procedure may have traumatized the uterine lining, leading to hemorrhage. Urinary tract infections, not common after evacuation of a molar pregnancy, are most commonly related to urinary catheterization.
Typically, urinary catheters are not used during the evacuation of a molar pregnancy. The client should not experience abdominal distention because the contents of the uterus have been removed. Chorioamnionitis is an inflammation of the amniotic fluid membranes. With a complete mole, no embryonic or fetal tissue or membranes are present.
Question 77.
When preparing a multigravid client who has undergone evacuation of a hydatidiform mole for discharge, the nurse explains the need for follow-up care. The nurse determines that the client understands the instruction when she says that she is at risk for developing which problem.
(a) ectopic pregnancy
(b) choriocarcinoma
(c) multifetal pregnancies
(d) infertility
Answer:
(b) choriocarcinoma
Explanation:
A client who has had a hydatidiform mole removed should have regular checkups to rule out the presence of choriocarcinoma, which may complicate the client’s clinical picture. The client’s human chorionic gonadotropin (hCG) levels are monitored for 1 year. During this time, she should be advised not to become pregnant because this would be reflected in rising hCG levels. Ectopic or multifetal pregnancy is not associated with hydatidiform mole. Women who have molar pregnancies have fertility rates similar to the general population.
Question 78.
After suction and evacuation of a complete hydatidiform mole, the 28-year-old multigravid client asks the nurse when she can become pregnant again. The nurse would advise the client not to become pregnant again for at least how long
(a) 6 months
(b) 12 months
(c) 18 months
(d) 24 months
Answer:
(b) 12 months
Explanation:
A client who has experienced a molar pregnancy is at risk for development of choriocarcinoma and requires close monitoring of human chorionic gonadotropin (hCG) levels. Pregnancy would interfere with monitoring these levels. High hCG titers are common for up to 7 weeks after the evacuation of the mole, but then, these levels gradually begin to decline.
Clients should have a pelvic examination and a blood test for hCG titers every month for 6 months and then every 2 months for 1 year. Gradually declining hCG levels suggest no complications. Increasing levels are indicative of a malignancy and should be treated with methotrexate. If after 1 year the hCG levels are negative, the client is theoretically free of the risk of a malignancy developing and could plan another pregnancy.
Question 79.
A woman is diagnosed with complete molar pregnancy. The nurse understands that the woman requires more teaching when she makes which statement?
(a) “I need to make follow-up appointments to have my hormone levels checked.”
(b) “I know the placenta caused problems, and my baby died in my uterus.”
(c) “I plan to get pregnant again next year.”
(d) “I understand I may develop a serious type of cancer.”
Answer:
(b) “I know the placenta caused problems, and my baby died in my uterus.”
Explanation:
Although the woman shows signs and symptoms typical of early pregnancy, in gestational trophoblastic disease, or molar pregnancy, gestational tissue exists, but the pregnancy is not viable. The woman must have follow-up human chorionic gonadotropin (hCG) levels for the remaining 12 months to ensure remaining tissue does not turn malignant.
Due to the risks of developing malignancy, the woman must avoid pregnancy for at least 1 year following gestational trophoblastic disease. In a complete molar pregnancy, the villi swell and form cysts, and the woman is at risk for choriocarcinoma, which is a rapidly spreading malignancy.
Question 80.
The nurse is working with four clients on the obstetrical unit. Which client will be the highest priority for a cesarean section?
(a) client at 40 weeks’ gestation whose fetus weighs 8 lb (3,630 g) by ultrasound estimate
(b) client at 37 weeks’ gestation with fetus in the right occiput posterior (ROP) position
(c) client at 32 weeks’ gestation with fetus in breech position
(d) client at 38 weeks’ gestation with active herpes lesions
Answer:
(a) client at 40 weeks’ gestation whose fetus weighs 8 lb (3,630 g) by ultrasound estimate
Explanation:
Herpes simplex virus can be transmitted to the infant during a vaginal birth. The neonatal effects of herpes are severe enough that a cesarean birth is warranted if active lesions-primary or secondary - are present. A client with a primary infection during pregnancy sheds the virus for up to 3 months after the lesion has healed. The client carrying an infant weighing 8lb (3,629 g) will be given a trial of labor before a cesarean.
The client with a fetus in the ROP position will have a slow labor with increased back pain but can give birth vaginally. The fetus in a breech position still has many weeks to change positions before being at term. At 7 months' gestation, the breech position is not a concern.
Question 81.
The nurse notices that a client who has just given birth is short of breath, is ashen in color, and begins to cough. She becomes limp on the birthing table. At the last assessment 30 minutes ago, her temperature was 98°F (36.7°C), her pulse was 78 beats/min, and her respirations were 16 breaths/min. Determine the nursing actions in the order they should occur. All options must be used.
(a) Open airway using head tilt-chin lift.
(b) Ask staff to activate the emergency response system,
(c) Establish unresponsiveness,
(d) Give two breaths.
(e) Begin compressions
Answer:
(c) Establish unresponsiveness,
(b) Ask staff to activate the emergency response system,
(e) Begin compressions
(a) Open airway using head tilt-chin lift.
(d) Give two breaths.
Explanation:
(c), (b), (a), (d), (e) The client’s actions indicate distress, and the nurse should initiate emergency procedures. The nurse should first establish unresponsiveness and then ask staff to activate the emergency response system. Next, the nurse should follow the CABs of CPR. The nurse should check the pulse and begin CPR, Then after 30 compressions, the nurse should ensure the open airway and give two breaths.
Question 82.
A client in sickle cell crisis has been hospitalized during her pregnancy. After giving discharge instructions, the nurse determines the client needs further teaching when she makes which statement.
(a) “I will need more frequent appointments during the remainder of the pregnancy.”
(b) “Signs of any type of infection must be reported immediately.”
(c) “At the earliest signs of a crisis, I need to seek treatment.”
(d) “I will need to take an iron supplement even if my laboratory values are normal.”
Answer:
(d) “I will need to take an iron supplement even if my laboratory values are normal.”
Explanation:
Sickle cell disease is an autosomal recessive disorder requiring both parents to have a sickle cell trait to pass the disease to a child. Deoxygenated hemoglobin cells assume a sickle shape and obstruct tissues. Tissue obstruction causes hypoxia to the area (vas occlusion) and results in pain, called sickle cell crisis. This type of anemia is an inherited disorder; it is not caused by a lack of iron in the diet.
Iron supplementation is needed only if there is laboratory evidence of iron deficiency anemia. Self-monitoring for any type of infection or sickle cell crisis and increased frequency of antenatal care visits are part of the teaching plan of care. compression on the cord is relieved, the increased oxygen will not serve its purpose. Placing the client in a Trendelenburg or knee-chest position would be position changes to increase perfusion to the infant by relieving cord compression.
Question 83.
A laboring client at -2 station has a spontaneous rupture of the membranes, and a cord immediately protrudes from the vagina. What should the nurse do first?
(a) Place gentle pressure upward on the fetal head.
(b) Place the cord back into the vagina to keep it moist.
(c) Begin oxygen by face mask at 8 to 10 L/min.
(d) Turn the client on her left side.
Answer:
(a) Place gentle pressure upward on the fetal head.
Explanation:
(a) The nurse should place a hand on the fetal head and provide gentle upward pressure to relieve the compression on the cord. Doing so allows oxygen to continue flowing to the fetus. The cord should never be placed back into the vagina because doing so may further compress it. Administering oxygen is an appropriate measure but will not serve a useful purpose until the pressure is relieved on the cord, enabling perfusion to the infant.
Turning the client to her left side facilitates better perfusion to the mother, but until the compression on the cord is relieved, the increased oxygen will not serve its purpose. Placing the client in a Trendelenburg or knee-chest position would be position changes to increase perfusion to the infant by relieving cord compression.
Question 84.
A client has just had a cesarean section for a prolapsed cord. In reviewing the client’s history, which factors place a client at risk for cord prolapse? Select all that apply.
(a) 2 station
(b) low-birth-weight infant
(c) rupture of membranes
(d) breech presentation
(e) prior abortion
(f) low-lying placenta
Answer:
(a) 2 station
(b) low-birth-weight infant
(c) rupture of membranes
(d) breech presentation
Explanation:
(a), (b), (c), (d) Having the fetus at a negative station places the client at risk for a cord prolapse. With a negative station, there is room between the fetal head and the maternal pelvis for the cord to slip through. A small infant is more mobile within the uterus, and the cord can rest between the fetus and the inside of the uterus or below the fetal head.
With a large infant, the head is usually in a vertex presentation and occludes the lower portion of the uterus, preventing the cord from slipping by. When membranes rupture, the cord can be swept through with the amniotic fluid. In a breech presentation, the fetal head is in the fundus, and smaller portions of the fetus settle into the lower portion of the uterus, allowing the cord to lie beside the fetus. Prior abortion and a low-lying placenta have no correlation with cord prolapse.
Question 85.
A woman who has given birth to a healthy neonate is being discharged. As part of discharge teaching, the nurse should instruct the client to observe vaginal discharge for postpartum hemorrhage and notify the health care provider (HCP) for which finding?
(a) bleeding that becomes lighter each day
(b) clots the size of grapes
(c) saturating a pad in less than an hour
(d) lochia that lasts longer than 1 week
Answer:
(c) saturating a pad in less than an hour
Explanation:
A postpartum client who saturates a pad in an hour or less at any time in the postpartum period is considered to be hemorrhaging. As the normal postpartum client heals, bleeding changes from red to pink to off-white. It also decreases in amount each day. Passing blood clots the size of a fist or larger is a reportable problem. Lochia varies in how long it lasts and is considered normal up to 6 weeks postpartum.
Question 86.
A woman who is Rh-negative has given birth to an Rh-positive infant. The nurse explains to the client that she will receive Rho(D) immune globulin. The nurse determines that the client understands the purpose of the treatment when she reports that Rho(D) immune globulin has which action?
(a) protecting her next baby if it is Rh-negative
(b) preventing antibody formation in her blood
(c) preventing antigen formation in her baby’s blood
(d) preventing jaundice in her baby
Answer:
(b) preventing antibody formation in her blood
Explanation:
Rho(D) immune globulin is given to new mothers who are Rh negative and not previously sensitized and who have given birth to an Rh-positive infant. Rho(D) immune globulin must be given within 72 hours of the birth of the infant because antibody formation begins at that time. The vaccine is used only when the mother has borne an Rh-positive infant not an Rh-negative infant.
Rho(D) immune globulin is not given to a newborn and does not affect antigen formation. Administering Rho(D) immune globulin after birth reduces risk of hyperbilirubinemia in newborns from future pregnancies, but it will not reduce the risk to the current newborn.
Question 87.
A client at 4 weeks postpartum tells the nurse that she cannot cope any longer and is overwhelmed by her newborn. The baby has old formula on her clothes and under her neck. The mother does not remember when she last bathed the baby and states she does not want to care for the infant. The nurse should encourage the client and her husband to call their health care provider (HCP) because the mother should be evaluated further for which complication?
(a) postpartum blues
(b) postpartum depression
(c) poor bonding
(d) infant abuse
Answer:
(b) postpartum depression
Explanation:
The client is experiencing and verbalizing signs of postpartum depression, which usually appears at about 4 weeks postpartum but can occur at any time within the first year after birth. It is more severe and lasts longer than postpartum blues, also called “baby blues.” Baby blues are the mildest form of depression and are seen in the later part of the first week after birth. Symptoms usually disappear shortly.
Depression may last several years and is disabling to the woman. Poor bonding may be seen at any time but commonly becomes evident as the mother begins interacting with the infant shortly after birth. Infant abuse may take the form of neglect or injuries to the infant. A depressed mother is at risk for injuring or abusing her infant.
Question 88.
The nurse and an unlicensed assistive personnel (UAP) are caring for clients in a birthing center. Which tasks should the nurse delegate to the UAP? Select all that apply.
(a) emptying a urinary catheter from a postpartum client
(b) assisting an active labor client with breathing and relaxation
(c) ambulating a postcesarean client to the bathroom
(d) calculating hourly IV totals for a preterm labor client
(e) intake and output catheterization for culture and sensitivity
(f) calling a report of normal findings to the health care provider (HCP)
Answer:
(a) emptying a urinary catheter from a postpartum client
(b) assisting an active labor client with breathing and relaxation
(c) ambulating a postcesarean client to the bathroom
Explanation:
(a), (b) ,(c) TheUAP could assist the client with breathing and relaxation, and ambulate the postcesarean client to the bathroom. UAP can empty catheters. Calculating the hourly IV totals for a preterm labor client would involve assessments that require nursing expertise. In-and-out catheterization, a sterile procedure, and calling reports to HCPs D which requires gathering and analysis of data, are responsibilities of the nurse.
Question 89.
Several pregnant clients are waiting to be seen in the triage area of the obstetrical unit. Which client should the nurse see first?
(a) a client at 13 weeks’ gestation who is experiencing nausea and vomiting three times a day with +1 ketones in her urine
(b) a client at 37 weeks’ gestation who is an insulin-dependent diabetic and experiencing 3 to 4 fetal movements per day
(c) a client at 32 weeks’ gestation who has preeclampsia and +3 proteinuria and who is returning for evaluation of epigastric pain
(d) a client at 17 weeks’ gestation who is not feeling fetal movement at this point in her pregnancy
Answer:
(c) a client at 32 weeks’ gestation who has preeclampsia and +3 proteinuria and who is returning for evaluation of epigastric pain
Explanation:
A preeclamptic client with +3 proteinuria and epigastric pain is at risk for seizing, which would jeopardize the mother and the fetus. Thus, this client would be the highest priority. The client at 13 weeks’ gestation with nausea and vomiting is a concern because the presence of ketones indicates that her body does not have glucose to break down. However, this situation is a lower priority than the preeclamptic client or the insulin-dependent diabetic.
The insulin-dependent diabetic is a high priority; however, fetal movement indicates that the fetus is alive but may be ill. As few as four fetal movements in 12 hours can be considered normal. (The client may need additional testing to further evaluate fetal well-being.) The client who is at 17 weeks’ gestation may be too early in her pregnancy to experience fetal movement and would be the last person to be seen.
Question 90.
The nurse is planning care for a group of pregnant clients. Which client should be referred to a health care provider (HCP) immediately?
(a) a woman at 10 weeks’ gestation who reports vomiting 3 times a day and has +1 ketones in her urine
(b) a woman at 36 weeks’ gestation with insulin dependent diabetes who reports having two to three hyperglycemic episodes per week
(c) a woman at 32 weeks’ gestation who is preeclamptic with +3 proteinuria
(d) a woman at 15 weeks’ gestation who reports she has not felt fetal movement
Answer:
(c) a woman at 32 weeks’ gestation who is preeclamptic with 3+ proteinuria
Explanation:
The nurse should refer the preeclamptic client with 3+ proteinuria to an HCP m The 3+ urine is significant, indicating there is much protein circulating. The woman who is 37 weeks’ gestation with insulin-dependent diabetes and who has experienced hypoglycemic episodes in the past week can be managed with food and glucose tablets until she can obtain an appointment with the care provider.
The client at 10 weeks’ gestation with nausea and vomiting and +1 ketones should also be seen by an HCP, but at this point, although this client is uncomfortable, her life is not in danger. The 15-week client would not be expected to feel her baby move this soon in the pregnancy, and this would not be considered a problem that requires immediate referral to an HCP.
Question 91.
A client with gestational hypertension is to receive magnesium sulfate to run at 3 g/h with normal saline to maintain the total IV rate at 125 mL/h. The nurse giving the end-of-shift report stated that the client’s blood pressures have been elevated during the night. The oncoming nurse checked the client and found magnesium sulfate running at 2 g/h. Identify the nursing actions to be taken from first to last. All options must be used.
(a) Notify the primary health care provider (HCP) of the incident.
(b) Assess the client’s current status.
(c) Correct the IV rates.
(d) Initiate an incident report.
Answer:
(c) Correct the IV rates.
(b) Assess the client’s current status.
(a) Notify the primary health care provider (HCP) of the incident.
(d) Initiate an incident report.
Explanation:
(c), (b), (a), (d) The nurse should first change the IV magnesium sulfate and normal saline infusion rates and then assess the current status of the client. The nurse should then notify the HCP to explain the error and report the action taken. A medication error has occurred, and the nurse will need to initiate an incident report.
Question 92.
As the nurse enters the room of a newly admitted primigravid client diagnosed with severe preeclampsia, the client begins to experience a seizure. The nurse should do which in order of priority from first to last? All options must be used.
(a) Call for immediate assistance.
(b) Turn the client to her side.
(c) Assess for ruptured membranes.
(d) Maintain airway.
Answer:
(a) Call for immediate assistance.
(b) Turn the client to her side.
(c) Assess for ruptured membranes.
(d) Maintain airway.
Explanation:
(a), (b), (c), (d) If a client begins to have a seizure, the first action by the nurse is to remain with the client and call for immediate assistance. Next, the nurse should turn the client to her side and then maintain the airway by keeping the neck hyper ex-tended. When the seizure is over, the nurse should assess the client for ruptured membranes and the fetal status.
Question 93.
The nurse is receiving shift report on four clients on an antenatal unit. The four clients are [1) a 35-week-gestation mother with severe preeclampsia started on a maintenance dose of magnesium sulfate 1 hour ago, (2) a 30-week-gestation client with preterm labor on an oral tocolytic and having no contractions in 6 hours, (3) a hyper-emesis client with emesis four times in the past 12 hours, and (4) a 33-week-gestation client with placenta previa who began to feel pelvic pressure during change of shift report. Which action should the nurse take first?
(a) Evaluate the client with preeclampsia for maternal and fetal tolerance of magnesium sulfate and the labor pattern.
(b) Assess the client with preterm labor for tolerance of tocolytics and the labor pattern.
(c) Assess the client with hyperemesis for nausea, further emesis, or dehydration.
(d) Evaluate the client with placenta previa without an exam.
Answer:
(d) Evaluate the client with placenta previa without an exam.
Explanation:
The first action taken should be to evaluate the placenta previa client who has pelvic pressure. The pelvic pressure may be caused by a fetal head creating pressure in the pelvis indicating a potential birth. This client should be evaluated without a pelvic exam and then consult with the health care provider (HCP) P. A vaginal exam is contraindicated as it may stimulate bleeding of the placenta.
The second action would be to complete an assessment on the client with preeclampsia and her fetus to evaluate for tolerance and effectiveness of the magnesium sulfate. The hyperemesis client needs to be evaluated for hydration status and for medication. The preterm labor client is stable on the oral medication and should be seen last.
Question 94.
Which client findings require the nurse’s attention first?
(a) a gravida 2, para 1 at 39 weeks’ gestation with spontaneous rupture of membranes 1 hour ago but no contractions
(b) a gravida 3, para 2 at 30 weeks’ gestation with nausea, vomiting, and epigastric pain
(c) a gravida 5, para 1 at 37 weeks’ gestation with pink vaginal discharge and abdominal cramping
(d) a gravida 1, para 0 at 39 weeks’ gestation with bruises on the arms and abdomen at various stages of healing
Answer:
(b) a gravida 3, para 2 at 30 weeks’ gestation with nausea, vomiting, and epigastric pain
Explanation:
A woman presenting at 30 weeks with nausea and vomiting and epigastric pain has signs and symptoms of preeclampsia and requires the nurse’s attention first. Gravida 2, para 1 with spontaneous rupture of membranes, but no contractions, is not a priority. Gravida 5, para 1 at 37 weeks with pink discharge and abdominal cramping could be in early labor and is not a priority at this time. A gravida 1, para 0 at 39 weeks with bruises at various stages of healing could indicate she is in an abusive relationship, but this is not a priority at this time.
Must Read: