Some NCLEX Prep Questions are adaptive, adjusting the difficulty level based on the student's performance to provide a personalized learning experience.
NCLEX Pediatric Nursing Questions - NCLEX Questions on Pediatric Nursing
Pediatric Nursing NCLEX Practice Questions
Question 1.
Mrs. Jones brings her 3-year-old son. Timmy, to the clinic because he has been vomiting for the past 12 hours. Upon assessment, the nurse notes that Timmy is alert but appears weak and dehydrated. His vomitus is yellow-green and has a sour smell. What should be the nurse's priority intervention for Timmy?
(a) Administer an antiemetic medication
(b) Assess the force of the vomiting
(c) Monitor electrolyte levels
(d) Provide oral rehydration therapy as tolerated and as prescribed
Answer:
(d) Provide oral rehydration therapy as tolerated and as prescribed
Explanation:
The priority intervention for Timmy is to provide oral rehydration therapy as tolerated and as prescribed because the major concerns when a child is vomiting are the risk of dehydration, the loss of fluid and electrolytes, and the development of metabolic alkalosis. In addition, the nurse should monitor the character, amount, and frequency of vomiting, assess the force of the vomiting, and monitor electrolyte levels. Administering an antiemetic medication may be necessary' but is not the priority intervention.
Patient History: The patient is a 7-year-old child who has been diagnosed with cystitis.
Nurse's Notes: presence of dysuria.
Physician Orders: antibiotics to treat the infection, advise the child to drink plenty of fluids and avoid irritants like caffeine, alcohol, and acidic foods or juice.
Question 2.
Which of the following is a common symptom that a nurse should expect when assessing a 7-year-old child diagnosed with cystitis?
(a) High fever
(b) Flank pain
(c) Costovertebral tenderness
(d) Dysuria
Answer:
(d) Dysuria
Explanation:
The correct answer is dysuria because it is a common symptom of cystitis. Options (a), (b), and (c) are incorrect because they are symptoms of pyelonephritis, an upper urinary tract infection. Cystitis is an infection or inflammation of the urinary bladder or any part of the urinary system caused by Escherichia coli (E. coli) bacteria.
The common symptoms include frequency, dysuria, urgency, suprapubic pain, cloudy urine, hematuria, nausea, vomiting, and fever. Pyelonephritis may have similar symptoms to cystitis, but it usually involves flank pain, high fever, and other systemic symptoms. Therefore, the nurse should expect dysuria as a common symptom when assessing a 7-year-old child with cystitis.
Question 3.
A child with a compromised immune system has been admitted to the hospital. The healthcare team is taking measures to protect the child from infections.
Which of the following measures are included in protecting the child from infection?
(a) Encouraging the child to eat raw fruits and vegetables
(b) Allowing fresh flowers in the child's room
(c) Limiting the number of caregivers entering the child's room
(d) Performing invasive procedures such as injections and urinary catheterization
Answer:
(c) Limiting the number of caregivers entering the child's room.
Explanation:
Option (a) is incorrect as raw fruits and vegetables can carry bacteria and other pathogens that may cause infection in a child with a compromised immune system. Therefore, the child's diet should be monitored and raw fruits and vegetables should be eliminated.
Option (b) is incorrect as fresh flowers can also carry bacteria and other pathogens that may cause infection in a child with a compromised immune system. Therefore, fresh flowers should not be allowed in the child's room.
Option (c) is the correct answer as limiting the number of caregivers entering the child's room can reduce the risk of infection transmission. The fewer people who enter the child's room, the less likely it is that pathogens will be introduced.
Option (d) is incorrect as invasive procedures such as injections and urinary catheterization can increase the risk of infection in a child with a compromised immune system. Therefore, these procedures should be avoided whenever possible.
Question 4.
A 7-year-old child was diagnosed with rubella (German measles) and has been admitted to the hospital. Which of the following statements regarding the patient needs nursing intervention or is either right or wrong?
(a) Rubella is a common viral disease that has teratogenic effects on the fetus during the first trimester of pregnancy.
(b) Rubella is transmitted by droplet and direct contact with an infected person.
(c) The discrete red maculopapular rash starts on the face and rapidly spreads to the entire body.
(d) Rash disappears within 3 days.
(e) Rubella is not contagious and does not require isolation.
(f) The patient may develop complications such as thrombocytopenia, encephalitis, and arthritis.
Answer:
Options (a), (b), (c), and (f) are correct.
Explanation:
Option (a) is correct because Rubella is a viral disease that has teratogenic effects on the fetus during the first trimester of pregnancy. Pregnant women who contract rubella can have babies with congenital rubella syndrome (CRS), which can cause a range of birth defects, including deafness, blindness, and heart defects.
Option (b) is correct because Rubella is transmitted by droplet and direct contact with an infected person. Therefore, the patient needs nursing intervention to prevent the spread of the disease to others. The patient should be placed in isolation until they are no longer contagious.
Option (c) is correct because the discrete red maculopapular rash starts on the face and rapidly spreads to the entire body. The rash may last for up to three days and is accompanied by fever, swollen glands, and joint pain.
Option (f) is correct because the patient may develop complications such as thrombocytopenia, encephalitis, and arthritis. Nursing interventions such as monitoring vital signs, administering medications, and providing supportive care can help prevent and manage these complications.
Option (d) is incorrect because the rash associated with rubella usually lasts for up to three days, not disappearing within three days.
Option (e) is incorrect because Rubella is highly contagious and requires isolation to prevent the spread of the disease to others. In conclusion, the correct answers are (a) (b), (c), and (f). The patient with rubella needs nursing intervention to prevent the spread of the disease to others, monitor for and manage potential complications, and provide supportive care.
Question 5.
A 5-year-old child is diagnosed with Varicella (chickenpox). Which of the following statements indicates the need for nursing intervention?
(a) The child should avoid contact with others until all lesions have crusted.
(b) The child can return to school once the fever has subsided.
(c) The child should receive the Varicella vaccine after recovery.
(d) Varicella is transmitted by contact with contaminated objects.
(e) The child should be given antiviral medication for the duration of the illness.
(f) The child may experience lesions that progress through various stages.
Answer:
(a) The child should avoid contact with others until all lesions have crusted.
(c) The child should receive the Varicella vaccine after recovery.
Explanation:
Option (a) is correct because the child should avoid contact with others until all lesions have crusted to prevent the spread of the infection. This is a crucial nursing intervention to ensure that the child does not infect others, especially those who are immunocompromised.
Option (c) is correct because the child should receive the Varicella vaccine after recovery to prevent future occurrences of the illness. This is also an essential nursing intervention to promote the child's health and prevent complications.
Option (b) is incorrect because the child should avoid contact with others until all lesions have caisted, not just when the fever has subsided.
Option (d) is incorrect because Varicella is transmitted by direct contact with an infected person, not by contact with contaminated objects.
Option (e) is incorrect because antiviral medication is not typically used to treat Varicella. The illness is usually allowed to run its course, and the symptoms are managed with antipyretics and analgesics.
Option (f) is incorrect because the progression of lesions is a typical characteristic of Varicella and does not require nursing intervention unless complications arise.
Question 6.
Anita, a 5-year-old child, presents with a fever and a rash that began on her face and has now spread to her trunk and extremities. Upon physical examination, her healthcare provider noted photophobia and Koplik spots on her buccal mucosa. Based on
these findings, which of the following statements regarding Anita's condition is true?
(a) Anita has mumps, which is a viral disease that can cause fever, headache, and parotid gland swelling.
(b) Anita has rubella, which is a viral disease that can cause teratogenic effects on the fetus during the first trimester of pregnancy.
(c) Anita has pertussis, which is an acute infectious respiratory disease usually occurring in infancy.
(d) Anita has varicella, which is a viral disease characterized by skin lesions that progress through macular, papular, vesicular, and pustular stages.
(e) Anita has rubeola (measles), which is a highly contagious viral disease that can lead to neurologic problems or death.
(f) Anita has both rubella and rubeola.
Answer:
(e) Anita has rubeola (measles), which is a highly contagious viral disease that can lead to neurologic problems or death.
(f) Anita has both rubella and rubeola.
Explanation:
The correct answer is (e) and (f). Anita has rubeola (measles), which is a highly contagious viral disease that can lead to neurologic problems or death. Rubeola is transmitted by direct contact with droplets from infected persons and is contagious mainly during the prodromal period, which is characterized by fever and upper respiratory symptoms. Classic symptoms include photophobia, Koplik spots on the buccal mucosa, and a confluent rash that begins on the face and spreads downward. Therefore, option (e) is correct.
Additionally, Anita could also have rubella (German measles), which is a common viral disease that has teratogenic effects on the fetus during the first trimester of pregnancy. Rubella is transmitted by droplet and direct contact with an infected person and is characterized by a discrete red maculopapular rash that starts on the face and rapidly spreads to the entire body. The rash disappears within 3 days. Therefore, option F is also correct.
Option (a) is incorrect because Anita does not have mumps, which is characterized by fever, headache, malaise, parotid gland swelling and tenderness, submaxillary and sublingual infection, orchitis, and meningoencephalitis. Option (b) is incorrect because Anita does not have rubella during pregnancy.
Option (c) is incorrect because Anita does not have pertussis, which is an acute infectious respiratory disease usually occurring in infancy and is characterized by upper respiratory symptoms and a paroxysmal stage characterized by prolonged coughing and crowing or whooping upon inspiration.
Option (d) is incorrect because Anita does not have varicella, which is a viral disease characterized by skin lesions that begin on the trunk and spread to the face and proximal extremities and progress through macular, papular, vesicular, and pustular stages.
Question 7.
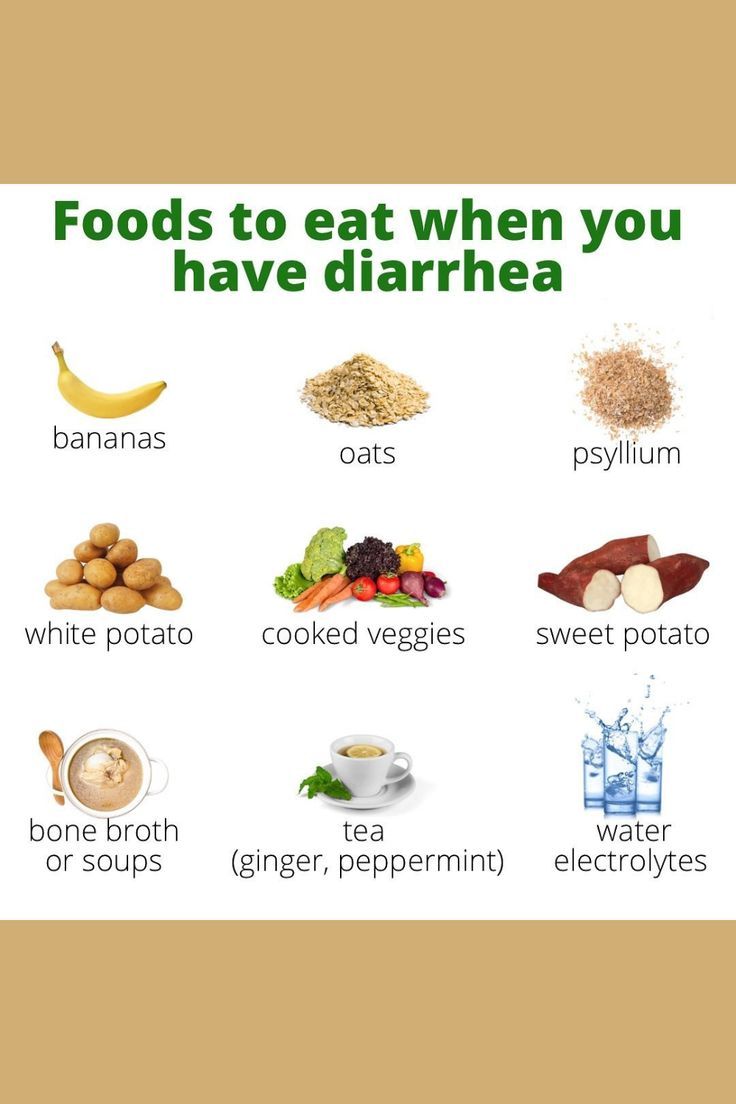
Nurse Saigrace is caring for a 5-year-old child who has been admitted to the hospital with diarrhea. The child's stool is watery and foul-smelling. What should be the nurse's priority intervention for the child?
(a) Monitor electrolyte levels
(b) Provide enteric isolation
(c) Monitor skin integrity
(d) Provide oral rehydration therapy with Pedialyte® or a similar rehydration solution as prescribed
Answer:
(d) Provide oral rehydration therapy with Pedialyte® or a similar rehydration solution as prescribed
Explanation:
The priority intervention for the child with diarrhea is to provide oral rehydration therapy with Pedialyte® or a similar rehydration solution as prescribed because the major concerns when a child has diarrhea are the risk of dehydration, the loss of fluid and electrolytes, and the development of metabolic acidosis.
In addition, the nurse should monitor the character, amount, and frequency of diarrhea, monitor electrolyte levels, monitor for signs and symptoms of dehydration, and provide enteric isolation as required. Monitoring skin integrity is also important but is not the priority intervention.
Patient's History: Sumitra, a pediatric patient, was admitted to the hospital with suspected rheumatic fever. She had been experiencing a fever for the past two days, and her parents noticed that she had a recent episode of pharyngitis.
Nurse's Notes: When obtaining Sumitra's history7, the nurse considered which information was most important. The nurse took note of the patient's symptoms, including vomiting and dizziness for two days, lack of interest in food, and a recent episode of pharyngitis.
Physician Orders: Based on Sumitra's symptoms and history, the physician ordered tests to confirm the diagnosis of rheumatic fever. The physician also prescribed medication to manage the patient's symptoms and reduce inflammation.
Lab Values: Lab tests showed elevated levels of anti-streptolysin O (ASO) antibodies, which confirmed the diagnosis of rheumatic fever.
Question 8.
What is the most important information for the nurse to consider when obtaining the patient's history for suspected rheumatic fever?
(a) Lack of interest in food
(b) A fever that started 2 days ago
(c) A recent episode of pharyngitis
(d) Vomiting and dizziness for 2 days
Answer:
(c) A recent episode of pharyngitis
Explanation:
The correct answer is (c) A recent episode of pharyngitis. Group A streptococcus (GAS) infections of the pharynx are the precipitating cause of rheumatic fever. A recent episode of pharyngitis is the most important factor in establishing the diagnosis of rheumatic fever. Option (b) is incorrect because fever is a common symptom in many illnesses and is not specific to rheumatic fever.
Option (a) is also incorrect because lack of interest in food can be seen in many illnesses and is not specific to rheumatic fever. Option (d) is incorrect because vomiting and dizziness are not specific to rheumatic fever.
Question 9.
Nurse Anne is developing a plan of care for a hospitalized child. She wants to know which age group of children is most likely to view illness as a punishment for misdeeds. Which age group of children is most likely to view illness as a punishment for misdeeds?
(a) Infancy
(b) Preschool age
(c) School age
(d) Adolescence
Answer:
(b) Preschool age
Explanation:
Preschool-age children, typically between the ages of 3 and 5, may believe that illness is a punishment for something they did or thought. This is because they are in the stage of moral development where they are learning about rules and consequences. Therefore, they may believe that their illness is a consequence of something they did wrong.
Option (a) Infants are not able to understand concepts of punishment or misdeeds as they are still in the early stages of development and are not yet able to understand abstract ideas.
Option (c) School-aged children may have fears related to death and dying, but they do not typically believe that illness is a punishment for misdeeds.
Option (d) Adolescents also have fears about death and dying, but they are typically more concerned with issues related to their identity, independence, and relationships with peers, rather than believing that illness is a punishment for misdeeds.
Question 10.
Molly is a 2-month-old infant who is brought to the pediatrician by her parents due to excessive crying, poor feeding, and frequent vomiting. The pediatrician suspects that Molly may be suffering from gastroesophageal reflux disease (GERD). The pediatrician explains to Molly's parents that GERD occurs when the stomach contents flow back into the esophagus or mouth and cause discomfort or pain. The pediatrician provides information about the signs and symptoms of GERD, as well as the interventions and positioning strategies to manage it.
Which of the following is a symptom of GERD?
(a) Weight gain
(b) Heartburn
(c) Normal breathing sounds
(d) No regurgitation
(e) No coughing after feeding
Answer:
(b) Heartburn
Explanation:
Option (b) is correct because heartburn is a common symptom of GERD.
Options (a), (c), (d), and (e) are incorrect because they are not symptoms of GERD. Poor weight gain, abnormal breathing sounds, regurgitation, and coughing are all potential symptoms of GERD.
Question 11.
Which of the following interventions are appropriate for managing GERD in infants?
(a) Assess for signs of dehydration.
(b) Provide small, frequent feedings with predigested formula.
(c) Place the infant in the prone position during sleep.
(d) Feed solids first, followed by liquids.
(e) Avoid feeding the child fatty foods, chocolate, tomato products, carbonated liquids, fruit juices, citrus products, and spicy foods.
Answer:
(a) Assess for signs of dehydration.
(b) Provide small, frequent feedings with predigested formula.
Explanation:
Options (a) and (b) are correct because assessing for signs of dehydration and providing small, frequent feedings with predigested formula are appropriate interventions for managing GERD in infants.
Options (c), (d), and (e) are incorrect because placing the infant in the prone position during sleep, feeding solids first followed by liquids, and avoiding certain foods are not appropriate interventions for managing GERD in infants. The infant should be placed in the supine position during sleep, with the head of the bed elevated, and the parents should be instructed to avoid certain foods if the infant is older than 1 year.
Question 12.
A pediatric nurse is reviewing information regarding hepatitis in children. Which of the following statements about hepatitis is correct?
(a) Elepatitis is a chronic condition caused by a virus, a medication reaction, or another disease process.
(b) Hepatitis A has the highest incidence among preschool or school- age children younger than 15 years.
(c) Hepatitis B is primarily transmitted through contaminated food or water.
(d) Hepatitis C is a rare condition that primarily affects adults.
Answer:
(b) Hepatitis A has the highest incidence among preschool or school- age children younger than 15 years.
Explanation:
Hepatitis A has the highest incidence among preschool or school-age children younger than 15 years. Option (a) is incorrect because hepatitis can be acute or chronic and may be caused by a virus, medication reaction, or another disease process. Option (c) is incorrect because Hepatitis B is primarily transmitted through perinatal transmission or exposure to infected blood or body fluids, such as during unprotected sexual contact, sharing needles, or accidental needlesticks.
Option (d) is incorrect because Hepatitis C primarily affects adults, but some children may be asymptomatic and develop chronic liver disease, cirrhosis, or hepatocellular carcinoma. In the case study, the nurse is reviewing information about Hepatitis in children. Hepatitis is an acute or chronic inflammation of the liver that can be caused by a virus, medication reaction, or another disease process. There are several types of hepatitis, including Hepatitis A, B, C, D, and E. each with different transmission modes, symptoms, and treatments.
Hepatitis A is primarily transmitted through the fecal-oral route and has the highest incidence among preschool or school-age children younger than 15 years. The symptoms of Hepatitis A can range from mild nausea, vomiting, and diarrhea to severe liver inflammation, but many infected children are asymptomatic and can still spread the vims to others.
Hepatitis B is primarily transmitted through perinatal transmission, exposure to infected blood or body fluids, such as during unprotected sexual contact, sharing needles, or accidental needlesticks. The severity of the infection can vary from no liver disease to fulminant or chronic active disease, and some infected children may become carriers and develop cirrhosis or hepatocellular carcinoma in adulthood.
Hepatitis C is primarily transmitted through the parenteral route, such as sharing needles or receiving contaminated blood transfusions. Some children may be asymptomatic and develop chronic liver disease, cirrhosis, or hepatocellular carcinoma, which can be challenging to treat.
Hepatitis D is a rare form of the disease that occurs in children already infected with Hepatitis B. It tends to be more severe than Hepatitis B and can lead to cirrhosis.
Hepatitis E is uncommon in children and is not a chronic condition. It does not cause chronic liver disease or a carrier state. Prevention and treatment of hepatitis include immunoglobulin for pre-exposure prophylaxis, vaccines for Hepatitis A and B, and standard precautions to prevent the spread of the vims.
Question 13.
A 3-year-old child was brought to the emergency department (ED) by his parents after they found him ingesting a bottle of household cleaner. Upon arrival, the nurse assessed the child's airway, breathing, and circulation, which were stable. The nurse identified the poison by questioning the parents and called for the health care provider's prescription to administer the appropriate antidote.
What is the first priority in treating a child with poisoning in the emergency department?
(a) Administering the antidote
(b) Identifying the poison
(c) Assessing the child's ABCs and vital signs
(d) Documenting the occurrence
Answer:
(c) Assessing the child's ABCs and vital signs
Explanation:
The first priority in treating a child with poisoning in the emergency department is to assess the child's ABCs and vital signs. This step ensures that the child's airway, breathing, and circulation are stable and that cardiopulmonary resuscitation is initiated immediately if necessary. After assessing the child, the nurse should terminate exposure to the poison by emptying the mouth of pills or other materials or flushing the skin or other body area.
Then, the nurse should identify the poison by questioning the parents or witnesses of the event to determine the appropriate treatment. The nurse should administer the antidote or take other measures as prescribed by the health care provider, such as administering activated charcoal. Finally, the nurse should document the occurrence, assessment findings, poison ingested, treatment measures, and the child's response for accurate and complete medical records.
Question 14.
Mrs. Miranda brings her 5-year-old son. Tommy, to the clinic because he has been experiencing abdominal cramps and intermittent loose stools for the past 3 days. Upon further assessment, the nurse practitioner suspects that Tommy may have intestinal parasites.
Which of the following interventions should be implemented to prevent the spread of intestinal parasites (including Giardiasis and pinworms)?
(a) Provide education to family and caregivers regarding sanitary practices.
(b) All members of the family should be treated for the infection.
(c) Perform a visual inspection of the anus with a flashlight.
(d) Medications are not usually prescribed for children younger than 2 years.
Answer:
(a) Provide education to family and caregivers regarding sanitary practices.
Explanation:
For Giardiasis, medications that kill the parasites may be prescribed, and caregivers should wash hands meticulously. For Pinworms, a visual inspection of the anus with a flashlight may be performed, the tape test is the most common diagnostic test, and medications that kill the parasites may be prescribed. It is also important to educate the family and caregivers regarding the tape test and the importance of meticulous hand washing and washing all clothes and bed linens in hot water to prevent the spread of intestinal parasites.
All members of the family may need to be treated for the infection if one family member is infected with Pinworms. Intestinal parasites are common in children and can cause a variety of symptoms. It is important to be aware of the causes, symptoms, and interventions for Giardiasis and Pinworms in order to provide appropriate care and prevent the spread of infection.
Question 15.
A 6-year-old child is brought to the clinic with a nosebleed. The nurse should:
(a) Panic and call for emergency assistance.
(b) Have the child lie down on their back.
(c) Assist the child to a sitting up and leaning forward position.
(d) Apply pressure to the upper portion of the nose.
Answer:
(c) Assist the child to a sitting up and leaning forward position.
Explanation:
When a child has a nosebleed, it is important for the nurse to remain calm and keep the child calm and quiet. Panic can cause the child to become agitated and difficult to cooperate. The child should be assisted to a sitting up and leaning forward position to prevent aspiration of blood. The child should not be placed in a lying down position because of the risk of aspiration. Nosebleeds usually originate in the anterior part of the nasal septum and can be controlled by applying pressure to the soft lower portion of the nose with the thumb and forefinger for at least 10 minutes.
Therefore, option (d) is incorrect as it suggests applying pressure to the upper portion of the nose. Option (b) is also incorrect as it advises lying down. Finally, option (a) is incorrect as it suggests panic, which is not an appropriate response. Option (c) is the correct answer because it advises assisting the child to a sitting up and leaning forward position to prevent aspiration of blood.