NCLEX Study Guide often include detailed explanations and rationales, helping students grasp the underlying concepts.
NCLEX Neonatal Client Questions - NCLEX Questions on Neonatal Client
Neonatal Client NCLEX Practice Questions
Question 1.
A primiparous woman has just given birth to a term infant. What topic should the nurse teach the client about first?
(a) sudden infant death syndrome (SIDS)
(b) breastfeeding
(c) infant bathing
(d) infant sleep-wake cycles
Answer:
(b) breastfeeding
Explanation:
Breastfed infants should eat within the first hour of life and approximately every 2 to 3 hours. Successful breastfeeding will likely require sustained support, encouragement, and instruction from the nurse. Information on SIDS, infant bathing, and sleep-wake cycles are also important topics for the new parent, but this information can be given at any time prior to discharge.
Question 2.
A newborn who is 20 hours old has a respiratory rate of 66 breaths/min, is grunting when exhaling, and has occasional nasal flaring. The newborn’s temperature is 98°F (36.6°C); he is breathing room air and is pink with acrocyanosis. The mother had membranes that were ruptured 26 hours before birth. What nursing actions are most indicated?
(a) Continue recording vital signs, voiding, stooling, and eating patterns every 4 hours.
(b) Place a pulse oximeter, and contact the health care provider (HCP) for a prescription to draw blood cultures.
(c) Arrange a transfer to the neonatal intensive care unit with diagnosis of possible sepsis.
(d) Draw a complete blood count (CBC) with differential and feed the infant.
Answer:
(b) Place a pulse oximeter, and contact the health care provider (HCP) for a prescription to draw blood cultures.
Explanation:
The concern with this infant is sepsis based on prolonged rupture of membranes before birth. Blood cultures would provide an accurate diagnosis of sepsis but will take 48 hours from the time drawn. Frequent monitoring of infant vital signs, looking for changes, and maintaining contact with the parents are also part of care management while awaiting culture results.
Continuing with vital signs, voiding, stooling, and eating every 4 hours is the standard of care for a normal newborn, but a respiratory rate > 60, grunting, and occasional flaring are not normal. Although not normal, the need for the intensive care unit is not warranted as newborns with sep¬sis can be treated with antibiotics at the maternal bedside. The CBC does not establish the diagnosis of sepsis, but the changes in the white blood cell levels can identify an infant at risk. Many experts suggest that waiting until an infant is 6 to 12 hours old to draw a CBC will give the most accurate results.
Question 3.
A neonate is born by cesarean birth at 36 weeks’ gestation. The temperature in the birthing room is 70°F (21.1°C). To prevent heat loss from convection, which action should the nurse take?
(a) Dry the neonate quickly after birth.
(b) Keep the neonate away from air conditioning vents.
(c) Place the neonate away from outside windows.
(d) Prewarm the bed.
Answer:
(b) Keep the neonate away from air conditioning vents.
Explanation:
The neonate should be kept away from drafts, such as from air conditioning vents, which may cause heat loss by convection. Evaporation is one of the most common mechanisms by which the neonate will lose heat, such as when the moisture on the newly bom neonate’s body is converted to vapor. Drying the infant prevents heat loss by evaporation.
Keeping infants away from outside windows helps prevent heat loss by radiation defined as heat loss between solid objects that are not in contact with one another such as walls and windows. Conduction is when heat is transferred between solid objects in contact with one another, such as when a neonate comes in contact with a cold mattress or scale. Placing the infant in a radiant warmer or skin to skin reduces heat loss from conduction.
Question 4.
The nurse reviews the daily weights of a breastfeeding term newborn. What conclusion does the nurse make about the weight loss?
|
Day |
Pounds |
Grams |
|
1 |
7 pounds 8 ounces |
3,401 |
|
2 |
7 pounds 4 ounces |
3,288 |
|
3 |
7 pounds |
3.175 |
(a) The newborn needs to be reweighed.
(b) Supplementation is now needed.
(c) Breastfeeding is going as expected.
(d) The health care provider needs to be notified.
Answer:
(c) Breastfeeding is going as expected.
Explanation:
Up to a 10% weight loss in the first few days of life is normal in a breastfeeding newborn. This newborn’s weight loss is under 10%, so the nurse can assume that breastfeeding is going as expected. There is no need to reweigh the newborn or notify the health care provider. Best breastfeeding practices do not include supplementation unless there is a medical reason.
Question 5.
The nurse makes a home visit to a 3-day-old full-term neonate who weighed 3,912 g (8 lb, 10 oz) at birth. Today the neonate, who is being bottle-fed, weighs 3,572 g (7 lb, 14lb). Which instructions should the nurse give to the mother?
(a) Continue feeding every 3 to 4 hours since the weight loss is normal.
(b) Contact the health care provider (HCP).
(c) Switch to a soy-based formula because the current one seems inadequate.
(d) Change to a higher-calorie formula to prevent further weight loss.
Answer:
(a) Continue feeding every 3 to 4 hours since the weight loss is normal.
Explanation:
This 3-day-old neonate’s weight loss falls within a normal range, and therefore no action is needed at this time. Full-term neonates tend to lose 5% to 10% of their birth weight during the first few days after birth, most likely because of minimal nutritional intake. With bottle-feeding, the neonate’s intake varies from one feeding to another. Typically, neonates regain any weight loss by 7 to 10 days of life. If the weight loss continues after that time, the HCP should be called.
Question 6.
Commercial formulas contain 20 calories per 30 mL. A 1-day-old infant was fed 45 mL at 0200, 0530, 0800, 1100, 1400, 1630, 2000, and 2230. What is the total amount of calories the infant received today? Record your answer using one decimal place.
A healthy neonate was just born in stable condition. In addition to drying the infant, what is the preferred method to prevent heat loss?
(a) placing the infant under a radiant warmer
(b) wrapping the infant in warm blankets
(c) applying a knit hat
(d) placing the infant skin to skin on the mother
Answer:
240 calories
Explanation:
Eight feedings x 45 mL per feeding equals 360 mL. 360 mL x 20 cal/30 mL = 240 calories.
Question 7.
A healthy neonate was just born in stable condition. In addition to drying the infant, what is the preferred method to prevent heat loss?
(a) placing the infant under a radiant warmer
(b) wrapping the infant in warm blankets
(c) applying a knit hat
(d) placing the infant skin to skin on the mother
Answer:
(d) placing the infant skin to skin on the mother
Explanation:
Placing an infant on a mother’s bare chest or abdomen facilitates transition to extrauterine life and is the preferred method of thermoregulation for stable infants. A radiant warmer should be used if an infant is unstable and needs medical intervention. Blankets may be placed over a newborn and mom’s chest. A hat may be added to prevent heat loss from the head, but these methods are supplemental to skin-to-skin care.
Question 8.
The nurse is preparing to administer a vitamin K injection to a male neonate shortly after birth. What statement by the mother indicates that she understands the purpose of the injection?
(a) “My baby does not have the normal bacteria in his intestines to produce this vitamin. "
(b) “My baby is at a high risk for a problem involving his blood’s ability to clot."
(c) “The red blood cells my baby formed during pregnancy are destroying the vitamin K."
(d) “My baby’s liver is not able to produce enough of this vitamin so soon after birth.”
Answer:
(a) “My baby does not have the normal bacteria in his intestines to produce this vitamin. "
Explanation:
For vitamin K synthesis in the intestines to begin, food and normal intestinal flora are needed. However, at birth the neonate’s intestines are sterile. Therefore, vitamin K is administered via injection to prevent a vitamin K deficiency that may result in a bleeding tendency. When administered, vitamin K promotes formation in the liver of clotting factors II, VII, IX, and X.
Neonates are not normally susceptible to clotting disorders, unless they are diagnosed with hemophilia or demonstrate a deficiency of or a problem with clotting factors. Hemolysis of fetal red blood cells does not destroy vitamin K. Hemolysis may be caused by Rh or ABO incompatibility, which leads to anemia and necessitates an exchange transfusion. Vitamin K synthesis occurs in the intestines, not the liver.
Question 9.
The nurse is teaching the mother of a new born to develop her baby’s sensory system. To further improve the infant’s most developed sense, what should the nurse instruct the mother to do?
(a) Speak in a high-pitched voice to get the new born’s attention.
(b) Place the newborn about 12 inches (30.5 cm) from maternal face for best sight.
(c) Stroke the newborn’s cheek with her nipple to direct the baby’s mouth to nipple.
(d) Give infant formula with a sweetened taste to stimulate feeding.
Answer:
(c) Stroke the newborn’s cheek with her nipple to direct the baby’s mouth to nipple.
Explanation:
Currently, touch is believed to be the most highly developed sense at birth. It is probably why neonates respond well to touch. Auditory sense typically is relatively immature in the neonate, as evidenced by the neonate’s selective response to the human voice. By 4 months, the neonate should turn the eyes and head toward a sound coming from behind.
Visual sense tends to be relatively immature. At birth, visual acuity is estimated at 20/100 to 20/150, but it improves rapidly during infancy and toddlerhood. Taste is well developed, with a preference toward glucose; however, touch is more developed at birth.
Question 10.
The nurse has completed discharge teaching with new parents who will be bottle-feeding their normal term newborn. Which statement by the parents reflects the need for more teaching?
(a) “Our baby will require feedings through the night for several weeks or months after birth.”
(b) “The baby should burp during and after each feeding with no projective vomiting.”
(c) “Our baby should have one to three soft, formed stools a day.”
(d) “We should weigh our baby daily to make sure he is gaining weight.”
Answer:
(d) “We should weigh our baby daily to make sure he is gaining weight.”
Explanation:
Healthy infants are weighed during their visits to their health care provider (HCP) J, so it is not necessary to monitor weights at home. Infants may require one to three feedings during the night initially. By 3 months, 90% of babies sleep through the night. Projective vomiting may indicate pyloric stenosis and should not be seen in a normal newborn. Bottle-fed infants may stool one to three times daily.
Question 11.
The nurse knows the mother of a neonate has understood the car seat safety instructions when she makes which statement?
(a) “I didn’t realize that even children between 1 to 2 years old are safer in rear-facing car seats.”
(b) “I should put my car seat in the front so I can watch my baby when I drive.”
(c) “I plan to use the car seat I saved from my last baby 10 years ago.”
(d) “The front-facing .car seats do a better job supporting the head and neck of my baby.”
Answer:
(a) “I didn’t realize that even children between 1 to 2 years old are safer in rear-facing car seats.”
Explanation:
The head and neck are best supported in a rear-facing seat in infants and toddlers, and infants should remain rear facing for as long possible until they outgrow their car seat. In the United States, the American Academy of Pediatrics recommends a rear-facing car seat for children younger than 2 years.
The middle of the back seat is safest for a car seat. Because plastic can become brittle over time, car seats have an expiration date that must be checked before use. Ten years would generally be outside of most car seats’ expiration dates.
Question 12.
While making a home visit to a primipa- rous client and her 3-day-old infant, the nurse observes the mother changing the baby’s disposable diaper. Before putting the clean diaper on the neonate, the mother begins to apply baby powder to the neonate’s buttocks. Which information about baby powder should the nurse relate to the mother?
(a) It may cause pneumonia to develop.
(b) It helps prevent diaper rash.
(c) It keeps the diaper from adhering to the skin.
(d) It can result in allergies later in life.
Answer:
(a) It may cause pneumonia to develop.
Explanation:
The nurse should inform the mother that baby powder can enter the neonate’s lungs and result in pneumonia secondary to aspiration of the particles. The best prevention for diaper rash is frequent diaper changing and keeping the neonate’s skin dry. The disposable diapers have moisture-collecting materials and generally do not adhere to the skin unless the diaper becomes saturated. Typically, allergies are not associated with the use of baby powder in neonates.
Question 13.
After teaching a new mother about the care of her neonate after circumcision with a Gornco clamp, which statement by the mother indicates to the nurse that the mother needs additional instructions?
(a) “The petroleum gauze may fall off into the diaper.”
(b) “A few drops of blood oozing from the site is normal.”
(c) “I will leave the gauze in place for 24 hours.”
(d) “I will remove any yellowish crusting gently with water.”
Answer:
(a) “The petroleum gauze may fall off into the diaper.”
Explanation:
The mother needs further instruction when she says that a yellowish crust should be removed with water. The yellowish crust is normal and indicates scar formation at the site. It should not be removed because to do so might cause increased bleeding. The petroleum gauze prevents the diaper from sticking to the circumcision site, and it may fall off in the diaper.
If this occurs, the mother should not attempt to replace it but should simply apply plain petroleum jelly to the site. The gauze should be left in place for 24 hours, and the mother should continue to apply petroleum jelly with each diaper change for 48 hours after the procedure. A few drops of oozing blood is normal, but if the amount is greater than a few drops, the mother should apply pressure and contact the health care provider (HCP) HI Any bleeding after the first day should be reported.
Question 14.
After completing discharge instructions for a primiparous client who is bottle-feeding her term neonate, the nurse determines that the mother understands the instructions when the mother says that she should contact the health care provider (HCP) if the neonate exhibits which sign or symptom?
(a) ability to fall asleep easily after each feeding
(b) spitting up of a tablespoon of formula after feeding
(c) passage of a liquid stool with a watery ring
(d) production of one to two light brown stools daily
Answer:
(c) passage of a liquid stool with a watery ring
Explanation:
The mother demonstrates an understanding of the discharge instructions when she says that she should contact the HCP Q if the baby has a liquid stool with a watery ring because this indicates diarrhea. Infants can become dehydrated very quickly, and frequent diarrhea can result in dehydration.
Normally, babies fall asleep easily after a feeding because they are satisfied and content. Spitting up a tablespoon of the formula is normal. However, projectile or forceful vomiting in larger amounts should be reported. Bottle-fed infants typically pass one to two light brown stools each day.
Question 15.
The nurse instructs a primiparous client about bottle-feeding her neonate. Which action demonstrates that the mother has understood the nurse’s instructions?
(a) placing the neonate on his back after the feeding
(b) bubbling the baby after 1 oz (30 mL) of formula
(c) putting three-quarters of the bottle nipple into the baby’s mouth
(d) pointing the nipple toward the neonate’s palate.
Answer:
(a) placing the neonate on his back after the feeding
Explanation:
Placing the neonate on his back after the feeding is recommended to minimize the risk of sudden infant death syndrome (SIDS). Placing the neonate on the abdomen after feeding has been associated with SIDS. The mother should bubble or burp the baby more than once during a feeding including at least after 0.5 oz (15 mL) of formula has been taken and then again when the baby is finished.
Waiting until the baby has eaten 1 oz (30 mL) of formula can lead to regurgitation. The entire nipple should be placed on top of the baby’s tongue and into the mouth to prevent excessive air from being swallowed. The nipple is pointed directly into the mouth, not toward the neonate’s palate, to provide adequate sucking.
Question 16.
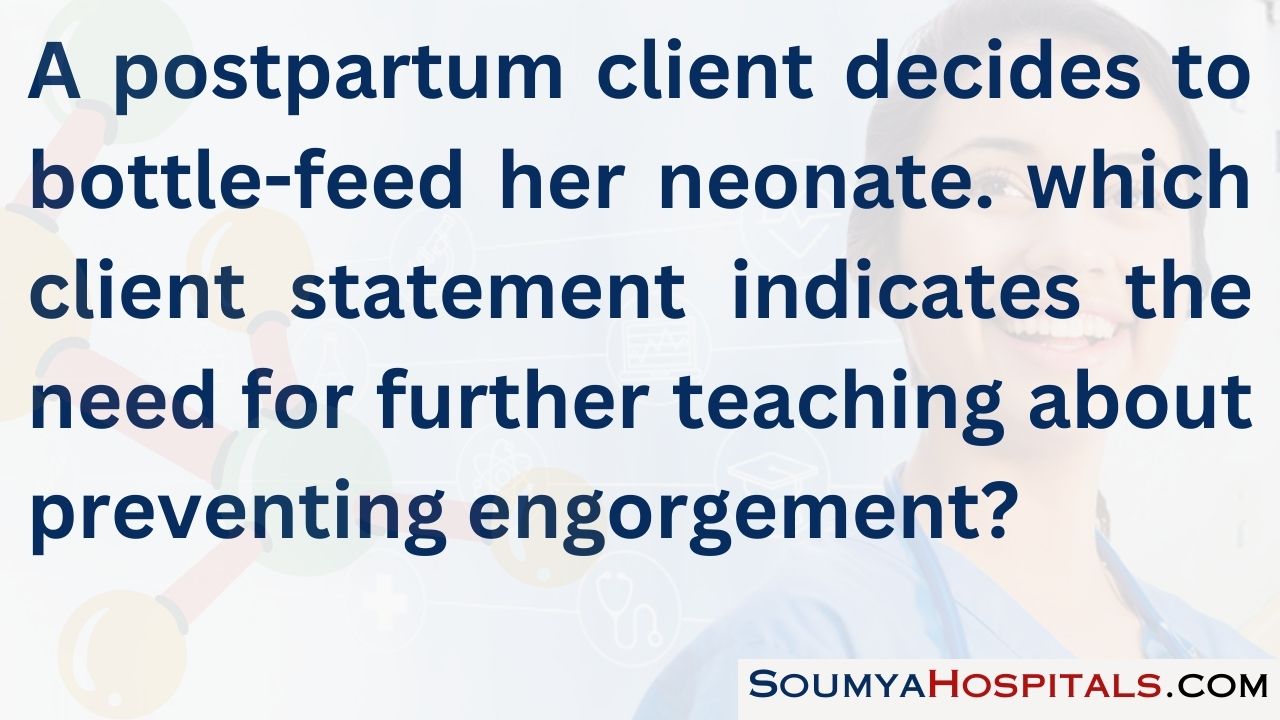
The nurse is to draw a blood sample for glucose testing from a term neonate during the first hour after birth. The nurse should obtain the blood sample from the neonate’s foot near which area?
Answer:

Explanation:
In a neonate, the lateral aspect of the heel is the most appropriate site for obtaining a blood specimen. Using this area prevents damage to the calcaneus bone, which is located in the middle of the heel. The middle of the heel is to be avoided because of the increased risk for damaging the calcaneus bone located there.
The middle of the foot contains the medial plantar nerve and the medial plantar artery, which could be injured if this site is selected. Using the base of the big toe as the site for specimen collection would cause a great deal of discomfort for the neonate; therefore, it is not the preferred site.
Question 17.
After circumcision with a Plastibell, the nurse should instruct the neonate’s mother to cleanse the circumcision site using which agent?
(a) antibacterial soap
(b) warm water
(c) povidone-iodine solution
(d) diluted hydrogen peroxide
Answer:
(b) warm water
Explanation:
After circumcision with a Plastibell, the most commonly recommended procedure is to clean the circumcision site with warm water with each diaper change. Other treatments are necessary only if complications, such as an infection, develop. Antibacterial soap or diluted hydrogen peroxide may cause pain and is not recommended. Povidone- iodine solution may cause stinging and burning, and therefore its use is not recommended.
Question 18.
Based on the understanding of periods of reactivity, what should the nurse encourage the mother of a term neonate to do approximately 90 minutes after birth?
(a) Feed the neonate.
(b) Allow the neonate to sleep.
(c) Get to know the neonate.
(d) Change the neonate’s diaper.
Answer:
(b) Allow the neonate to sleep.
Explanation:
As part of the neonate’s physiologic adaptation to birth at 90 minutes after birth the neonate typically is in the rest or sleep phase. During this time, the heart and respiratory rates slow and the neonate sleeps, unresponsive to stimuli. At this time, the mother should rest and allow the neonate to sleep. Feedings should be given during the first period of reactivity, considered the first 30 minutes after birth.
During this period, the neonate’s respirations and heart rate are elevated. Getting to know the neonate typically occurs within the first hour after birth and then when the neonate is awake and during feedings. Changing the neonate’s diaper can occur at any time, but at 90 minutes after birth, the neonate is usually in a deep sleep, unresponsive, and probably has not passed any meconium.
Question 19.
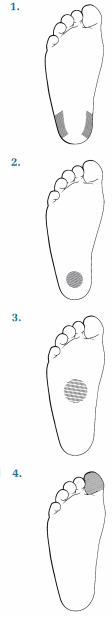
The nurse is to assess a newborn for incurving of the trunk. Which illustration indicates the position in which the nurse should place the newborn?
Answer:
Explanation:
When assessing the incurving of the trunk tests for automatic reflexes in the newborn, the nurse places the infant horizontally and in a prone position with one hand and strokes the side of the newborn’s trunk from the shoulder to the buttocks using the other hand. If the reflex is present, the newborn’s trunk curves toward the stimulated side. Answer 2 shows a figure for testing for a stepping response. Answer 3 shows a figure for testing for a tonic neck reflex. Answer 4 shows a figure for testing for the Moro (startle) reflex.
Question 20.
A full-term neonate is admitted to the normal newborn nursery. When lifting the baby out of the crib, the nurse notes the baby’s arms move sideways with the palms up and the thumbs flexed. What should the nurse do next?
(a) Activate rapid response teams.
(b) Identify this reflex as a normal finding.
(c) Place the neonate on seizure precautions.
(d) Start supplemental oxygen.
Answer:
(b) Identify this reflex as a normal finding.
Explanation:
The baby is displaying a normal Moro reflex that occurs with a sudden loss of support and requires no intervention. Activating rapid response teams, placing the neonate on seizure precautions, and starting supplemental oxygen are not necessary for a normally occurring reflex.
Question 21.
After the birth of a neonate, a quick assessment is completed. The neonate is found to be apneic. After quickly drying and positioning the neonate, what should the nurse do next?
(a) Assign the first Apgar score.
(b) Start positive pressure ventilation.
(c) Administer oxygen.
(d) Start cardiac compressions.
Answer:
(b) Start positive pressure ventilation.
Explanation:
If an infant is not breathing after the initial steps of resuscitation, the next thing the nurse must do is begin positive pressure ventilation. Apgar scores are an evaluation of the neonate’s status at 1 and 5 minutes of life. Waiting to restore respirations until after assigning an Apgar score would be a waste of valuable time. Oxygen alone does little good if the infant is not breathing. Chest compressions must be accompanied by adequate oxygenation.
Question 22.
A 6-lb, 8-oz (2,948 g) neonate was born vaginally at 38 weeks’ gestation. At 5 minutes of life, the neonate has the following signs: heart rate 110 bpm, intermittent grunting with respiratory rate of 70 breaths/min, flaccid tone, no response to stimulus, and overall pale white in color. What is the Apgar score?
(a) 2
(b) 3
(c) 4
(d) 6
Answer:
(c) 4
Explanation:
The neonate has a heart rate >100 bpm, which earns him 2 points. His respiratory rate of 70 breaths/min is equivalent to a 2 on the scale. His flaccid muscle tone is equal to 0 on the scale. The lack of response to stimulus also equals 0, as does his overall pale white color. Thus, the total score equals 4.
Question 23.
A neonate has a large amount of secretions. After vigorously suctioning the neonate, the nurse should assess for what possible result?
(a) bradycardia
(b) rapid eye movement
(c) seizures
(d) tachypnea
Answer:
(a) bradycardia
Explanation:
After performing vigorous suctioning, the nurse must watch for bradycardia due to potential vagus nerve stimulation. Rapid eye movement is not associated with vagus nerve stimulation. Vagal stimulation will not cause seizures or tachypnea.
Question 24.
After vaginal birth of a term neonate, the nurse observes that the neonate has one artery and one vein in the umbilical cord. The nurse notifies the health care provider (HCP) based on the analysis that this may be indicative of which anomalies?
(a) respiratory anomalies
(b) musculoskeletal anomalies
(c) cardiovascular anomalies
(d) facial anomalies
Answer:
(c) cardiovascular anomalies
Explanation:
Normally, the umbilical cord has two umbilical arteries and one vein. When a neonate is born with only one artery and one vein, the nurse should notify the HCP Q for further evaluation of cardiac anomalies. Other common congenital problems associated with a missing artery include renal anomalies, central nervous system lesions, tracheoesophageal fistulas, trisomy 13, and trisomy 18.
Respiratory anomalies are associated with dyspnea and respiratory distress; musculoskeletal anomalies include fractures or dislocated hip; and facial anomalies are associated with fetal alcohol syndrome or Down syndrome, not a missing umbilical artery.
Question 25.
While changing the neonate’s diaper, the client asks the nurse about some red-tinged drainage from the neonate’s vagina. Which response would be most appropriate?
(a) “It’s of no concern because it’s such a small amount.”
(b) “The cause is usually related to swallowing blood during the birth.”
(c) “Sometimes baby girls have this from hormones received from the mother.”
(d) “This vaginal spotting is caused by hemorrhagic disease of the newborn.”
Answer:
(c) “Sometimes baby girls have this from hormones received from the mother.”
Explanation:
The most appropriate response would be to explain that the vaginal spotting in female neonates is associated with hormones received from the mother. Estrogen is believed to cause slight vaginal bleeding or spotting in the female neonate. The condition disappears spontaneously, so there is no need for concern. Telling the mother that it is of no concern does not allay the mother’s worry. The vaginal spotting is related to hormones received from the mother, not to swallowing blood during the birth or hemorrhagic disease of the neonate. Anemia is associated with hemorrhagic disease.
Question 26.
Which finding would the nurse expect as common for a multiparous client giving birth to a viable neonate at 41 weeks’ gestation with the aid of a vacuum extractor?
(a) caput succedaneum
(b) cephalohematoma
(c) maternal lacerations
(d) neonatal intracranial hemorrhage
Answer:
(a) caput succedaneum
Explanation:
Caput succedaneum is common after the use of a vacuum extractor to assist the client’s expulsion efforts. This edema may persist for up to 7 days. Vacuum extraction is not associated with cephalo-hematoma. Maternal lacerations may occur, but they are more common when forceps are used. Neonatal intracranial hemorrhage is a risk with both vacuum extraction and forceps births, but it is not a common finding.
Question 27.
After explaining to a primiparous client about the causes of her neonate’s cranial molding, which statement by the mother indicates the need for further instruction?
(a) “The molding was caused by an overlapping of the baby’s cranial bones during my labor.”
(b) “The amount of molding is related to the amount and length of pressure on the head.”
(c) “The molding will usually disappear in a couple of days.”
(d) “Brain damage may occur if the molding does not resolve quickly.”
Answer:
(d) “Brain damage may occur if the molding does not resolve quickly.”
Explanation:
The mother needs further instruction if she says the molding can result in brain damage. Brain damage is highly unlikely. Molding occurs during vaginal birth when the cranial bones tend to override or overlap as the head accommodates the size of the mother's birth canal. The amount and duration of pressure on the head influence the degree of molding. Molding usually disappears in a few days without any special attention.
Question 28.
Which observation is expected when the nurse is assessing the gestational age of a neonate born at term?
(a) ear lying flat against the head
(b) absence of rugae in the scrotum
(c) sole creases covering the entire foot
(d) square window sign angle of 90 degrees
Answer:
(c) sole creases covering the entire foot
Explanation:
Sole creases covering the entire foot are indicative of a term neonate. If the neonate’s ear is lying flat against the head, the neonate is most likely preterm. An absence of rugae in the scrotum typically suggests a preterm neonate. A square window sign angle of 0 degrees occurs in neonates of 40 to 42 weeks’ gestation. A 90-degree square window angle suggests an immature neonate of approximately 28 to 30 weeks’ gestation.
Question 29.
While the nurse is performing a complete assessment of a term neonate, which finding would alert the nurse to notify the health care provider (HCP)?
(a) red reflex in the eyes
(b) expiratory grunt
(c) respiratory rate of 45 breaths/min
(d) prominent xiphoid process
Answer:
(b) expiratory grunt
Explanation:
An expiratory grunt is significant and should be reported promptly because it may indicate respiratory distress and the need for further intervention such as oxygen or resuscitation efforts. The presence of a red reflex in the eyes is normal. An absent red reflex may indicate congenital cataracts. A respiratory rate of 45 breaths/min and a prominent xiphoid process are normal findings in a term neonate.
Question 30.
After instructing a mother about normal reflexes of term neonates, the nurse determines that the mother understands the instructions when she describes the tonic neck reflex as occurring when the neonate displays which behavior?
(a) steps briskly when held upright near a firm, hard surface
(b) pulls both arms and does not move the chin beyond the point of the elbows
(c) turns head to the left, extends left extremities, and flexes right extremities
(d) extends and abducts the arms and legs with the toes fanning open
Answer:
(c) turns head to the left, extends left extremities, and flexes right extremities
Explanation:
The tonic neck reflex also called the fencing position, is present when the neonate turns the head to the left side, extends the left extremities, and flexes the right extremities. This reflex disappears in a matter of months as the neonatal nervous system matures.
The stepping reflex is demonstrated when the infant is held upright near a hard, firm surface. The prone crawl reflex is demonstrated when the infant pulls both arms but does not move the chin beyond the elbows. When the infant extends and abducts the arms and legs with the toes fanning open, this is a normal Babinski’s reflex.
Question 31.
A primiparous client expresses concern, asking the nurse why her neonate’s eyes are crossed. Which information would the nurse include when teaching the mother about neonatal strabismus?
(a) The neonate’s eyes are unable to focus on light at this time.
(b) Neonates commonly lack eye-muscle coordination.
(c) Congenital cataracts may be present.
(d) The neonate is able to fixate on distant objects immediately.
Answer:
(b) Neonates commonly lack eye-muscle coordination.
Explanation:
Convergent strabismus is common during infancy until about age 6 months because of poor oculomotor coordination. The neonate has peripheral vision and can fixate on close objects for short periods. The neonate can also perceive colors, shapes, and faces.
Neonates can focus on light and should blink or close their eyes in response to light. However, this is not associated with strabismus. An absent red reflex or white areas over the pupils, not strabismus, may indicate congenital cataracts. Most neonates cannot focus well or accommodate for distance immediately after birth.
Question 32.
While performing a physical assessment on a term neonate shortly after birth, which finding would cause the nurse to notify the health care provider (HCP)?
(a) deep creases across the soles of the feet
(b) frequent sneezing during the assessment
(c) single crease on each of the palms
(d) absence of lanugo on the skin
Answer:
(c) single crease on each of the palms
Explanation:
A single crease across the palm (simian crease) is most commonly associated with chromosomal abnormalities, notably Down syndrome. Deep creases across the soles of the feet is a normal finding in a term neonate. Frequent sneezing in a term neonate is normal. This occurs because the neonate is a nose breather and sneezing helps to clear the nares. An absence of lanugo on the skin of a term neonate is a normal finding.
Question 33.
Metabolic screening of an infant revealed a high phenylketonuria (PKU) level. Which statement by the infant’s mother indicates understanding of the disease and its management? Select all that apply.
(a) “My baby cannot have milk-based formulas.”
(b) “My baby will grow out of this by the age of 2.”
(c) “This is a hereditary disease, so any hi lure children will have it, too.”
(d) “My baby will eventually become mentally challenged because of this disease.”
(e) “We have to follow a strict low-phenylalanine diet.”
(f) “A dietitian can help me plan a diet that keeps a safe phenylalanine level but lets my baby grow.”
Answer:
(a) “My baby cannot have milk-based formulas.”
(e) “We have to follow a strict low-phenylalanine diet.”
(f) “A dietitian can help me plan a diet that keeps a safe phenylalanine level but lets my baby grow.”
Explanation:
(a), (e), (f) Phenylketonuria, an inherited autosomal recessive disorder, involves the body’s inability to metabolize the amino acid phenylalanine. A diet low in phenylalanine must be followed. Such foods as meats, eggs, and milk are high in phenylalanine. Assistance from a dietitian is commonly necessary to keep phenylalanine levels low and to provide the essential amino acids necessary for cell function and tissue growth.
With autosomal recessive disorders, future children will have a 25% chance of having the disease, a 50% chance of carrying the disease, and a 25% chance of being free of the disease. If a diet low in phenylalanine is followed until brain growth is complete (sometime in adolescence), the child should achieve normal intelligence.
Question 34.
Assessment of a term neonate at 2 hours after birth reveals a heart rate of < 100 bpm, periods of apnea approximately 25 to 30 seconds in length, and mild cyanosis around the mouth. The nurse notifies the health care provider (HCP) based on the interpretation that these findings may lead to which condition?
(a) respiratory arrest
(b) bronchial pneumonia
(c) intraventricular hemorrhage
(d) epiglottitis
Answer:
(a) respiratory arrest
Explanation:
Periods of apnea lasting longer than 20 seconds, mild cyanosis, and a heart rate of <100 bpm (bradycardia) are associated with a potentially life-threatening event and subsequent respiratory arrest. The neonate needs further evaluation by the HCP Q. Pneumonia is associated with tachycardia, anorexia, malaise, cyanosis, diminished breath sounds, and crackles. Intraventricular hemorrhage is associated with prematurity. Assessment findings include bulging fontanelles and seizures. Epiglottitis is a bacterial form of croup. Assessment findings include inspiratory stridor, cough, and irritability. It occurs most commonly in children aged 3 to 7 years.
Question 35.
A new mother asks, “When will the soft spot near the front of my baby’s head close?” When should the nurse tell the mother the soft spot will close?
(a) 2 to 3 months
(b) 6 to 8 months
(c) 9 to 10 months
(d) 12 to 18 months
Answer:
(d) 12 to 18 months
Explanation:
Normally, the anterior fontanelle closes between ages 12 and 18 months. Premature closure (craniostenosis or premature synostosis) prevents proper growth and expansion of the brain, resulting in an intellectual disability. The posterior fontanel typically closes by ages 2 to 3 months.
Question 36.
Which assessment finding in a term neonate would cause the nurse to notify the health care provider (HCP)?
(a) absence of tears
(b) unequally sized corneas
(c) pupillary constriction to bright light
(d) red circle on pupils seen with a penlight
Answer:
(b) unequally sized corneas
Explanation:
Corneas of unequal size should be reported because this may indicate congenital glaucoma. An absence of tears is common because the neonate’s lacrimal glands are not yet functioning. The neonate’s pupils normally constrict when a bright light is focused on them.
The finding implies that light perception and visual acuity are present, as they should be after birth. A red circle on the pupils is seen when a penlight or ophthalmoscope’s light shines onto the retina and is a normal finding. Called the red reflex, this indicates that the light is shining onto the retina.
Question 37.
At 24 hours of age, assessment of the neonate reveals the following: eyes closed, skin pink, no sign of eye movements, heart rate of 120 bpm, and respiratory rate of 35 breaths/min. What is this neonate most likely experiencing?
(a) drug withdrawal
(b) first period of reactivity
(c) a state of deep sleep
(d) respiratory distress
Answer:
(c) a state of deep sleep
Explanation:
At 24 hours of age, the neonate is probably in a state of deep sleep, as evidenced by the closed eyes, lack of eye movements, normal skin color, and normal heart rate and respiratory rate. Jitteriness, a high-pitched cry, and tremors are associated with drug withdrawal. The first period of reactivity occurs in the first 30 minutes after birth, evidenced by alertness, sucking sounds, and rapid heart rate and respiratory rate. There is no evidence to suggest respiratory distress because the neonate’s respiratory rate of 35 breaths/min is normal.
Question 38.
While assessing a male neonate whose mother desires him to be circumcised, the nurse observes that the neonate’s urinary meatus appears to be located on the ventral surface of the penis. The health care provider (HCP) is notified because the nurse suspects which complication?
(a) phimosis
(b) hydrocele
(c) epispadias
(d) hypospadias
Answer:
(d) hypospadias
Explanation:
The condition in which the urinary meatus is located on the ventral surface of the penis, termed hypospadias, occurs in 1 of every 500 male infants. Circumcision is delayed until the condition is corrected surgically, usually between 6 and 12 months of age. Phimosis is an inability to retract the prepuce at an age when it should be retractable or by age 3 years.
Phimosis may necessitate circumcision or surgical intervention. Hydrocele is a painless swelling of the scrotum that is common in neonates. It is not a contraindication for circumcision. Epispadias occurs when the urinary meatus is located on the dorsal surface of the penis. It is extremely rare and is commonly associated with bladder exstrophy.
Question 39.
The nurse is discussing kangaroo care with the parents of a premature neonate. The nurse should tell the parents that the advantages of skin to skin care include which benefits? Select all that apply.
(a) enhanced bonding
(b) increased IQ
(c) improved physiologic stability
(d) decreased length of stay in the neonatal intensive care unit
(e) improved breastfeeding
Answer:
(a) enhanced bonding
(c) improved physiologic stability
(d) decreased length of stay in the neonatal intensive care unit
(e) improved breastfeeding
Explanation:
(a), (c), (d), (e) Holding of a neonate skin to skin with a caregiver has been shown increased bonding, physiologic stability, decreased length of stay, and improved breastfeeding. Research has not shown an increase in IQ as a developmental outcome. The experience is usually limited to 1 to 2 hours, two to three times per day.
Question 40.
After a vaginal birth, a preterm neonate is to receive oxygen via mask. While administering the oxygen, the nurse would place the neonate in which position?
(a) left side, with the neck slightly flexed
(b) back, with the head turned to the left side
(c) abdomen, with the head down
(d) back, with the neck slightly extended
Answer:
(d) back, with the neck slightly extended
Explanation:
When receiving oxygen by mask, the neonate is placed on the back with the neck slightly extended, in the “sniffing” or neutral position. This position optimizes lung expansion and places the upper respiratory tract in the best position for receiving oxygen. Placing a small rolled towel under the neonate’s shoulders helps to extend the neck properly without overextending it.
Once stabilized and transferred to an isolette in the intensive care unit, the neonate can be positioned in the prone position, which allows for lung expansion in the oxygenated environment. Placing the neonate on the left side does not allow for maximum lung expansion. Also, slightly flexing the neck interferes with opening the airway. Placing the neonate on the back with the head turned to the left side does not allow for lung expansion. Placing the neonate on the abdomen interferes with proper positioning of the oxygen mask.

Question 41.
Which action should the nurse take when performing external chest compressions on a neonate born at 28 weeks’ gestation?
(a) Maintain a compression-to-ventilation ratio of 3 : 1.
(b) Compress the sternum with the palm of the hand.
(c) Compress the chest 70 to 80 times/min.
(d) Displace the chest wall half the depth of the anterior-posterior diameter of the chest.
Answer:
(a) Maintain a compression-to-ventilation ratio of 3 : 1.
Explanation:
Chest compressions should be alternated with ventilation to ensure breathing and circulation. Two fingers or two thumbs encircling hands, not the palm of the hand, are used to compress a neonate’s sternum. The chest is compressed 100 to 120 times/min. The proper technique recommended by the Neonatal Resuscitation Program is to use enough pressure to depress the sternum to a depth of approximately one-third of the anterior-posterior diameter of the chest.
Question 42.
A preterm neonate who has been stabilized is placed in a radiant warmer and is receiving oxygen via an oxygen hood. Which action should the nurse take while administering oxygen in this manner?
(a) Humidify the air being delivered.
(b) Cover the neonate’s scalp with a warm cap.
(c) Record the neonate’s temperature every 3 to 4 minutes.
(d) Assess the neonate’s blood glucose level.
Answer:
(a) Humidify the air being delivered.
Explanation:
Whenever oxygen is administered, it should be humidified to prevent drying of the nasal passages and mucous membranes. Because the neonate is under a radiant warmer, a stocking cap is not necessary. Temperature, continuously monitored by a skin probe attached to the radiant warmer, is recorded every 30 to 60 minutes initially. Although the oxygen concentration in the hood requires close monitoring and measurement of blood gases, checking the blood glucose level is not necessary.
Question 43.
Two hours ago, a neonate at 38 weeks’ gestation and weighing 3,175 g (7 lb) was born to a primiparous client who tested positive for beta-hemolytic Streptococcus. Which finding would alert the nurse to notify the health care provider (HCP)?
(a) alkalosis
(b) increased muscle tone
(c) temperature instability
(d) positive Babinski’s reflex
Answer:
(c) temperature instability
Explanation:
The neonate is at high risk for sepsis due to exposure to the mother’s infection. Temperature instability in a neonate at 38 weeks’ gestation is an early sign of sepsis. Other signs include tachycardia, decreased muscle tone, acidosis, apnea, respiratory distress, hypotension, poor feeding behaviors, vomiting, and diarrhea. Late signs of infection include jaundice, seizures, enlarged liver and spleen, respiratory failure, and shock.
Alkalosis is not typically seen in neonates who develop sepsis. Acidosis and respiratory distress may develop unless treatment such as antibiotics is started. A positive Babinski’s reflex is a normal finding and does not need to be reported.
Question 44.
Assessment of a 2-day-old neonate born at 34 weeks’ gestation reveals absent apical pulse left of the midclavicular line, cyanosis, grunting, and diminished breath sounds. After beginning oxygen, what is the priority intervention?
(a) Obtain a prescription for a stat chest X-ray.
(b) Reposition the neonate, and then assess if the grunting and cyanosis resolve.
(c) Obtain a prescription for an echocardiogram.
(d) Obtain a complete blood count to determine infection.
Answer:
(a) Obtain a prescription for a stat chest X-ray.
Explanation:
With an absent apical pulse left of the midclavicular line accompanied by cyanosis, grunting, and diminished breath sounds, the neonate is most likely experiencing pneumothorax. Pneumothorax occurs when alveoli are overdistended and subsequently the lung collapses, com-pressing the heart and lung and compromising the venous return to the right side of the heart.
This condition can be confirmed by X-ray. An echocar diogram would be indicated if the chest X-ray did not reveal a respiratory cause for the problem or suggested a cardiac problem. Repositioning the infant may open the airway, and obtaining blood studies for infection will rule that out, but until pneumothorax is resolved, the other symptoms will continue.
Question 45.
Twenty-four hours after cesarean birth, a neonate at 30 weeks’ gestation is diagnosed with respiratory distress syndrome (RDS). When explaining to the parents about the cause of this syndrome, the nurse should include a discussion about an alteration in the body’s secretion of which substance?
(a) somatotropin
(b) surfactant
(c) testosterone
(d) progesterone
Answer:
(b) surfactant
Explanation:
RDS, previously called hyaline membrane disease, is a developmental condition involving a decrease in lung surfactant leading to improper expansion of the lung alveoli. Surfactant contains a group of surface-active phospholipids, of which one component lecithin is the most critical for alveolar stability. Surfactant production peaks at about 35 weeks’ gestation.
This syndrome primarily attacks preterm neonates, although it can also affect term and post-term neonates. Altered somatotropin secretion is associated with growth disorders such as gigantism or dwarfism. Altered testosterone secretion is associated with masculinization. Altered progesterone secretion is associated with spontaneous abortion during pregnancy.
Question 46.
A viable neonate born to a 28-year-old multiparous client by cesarean birth because of placenta previa is diagnosed with respiratory distress syndrome (RDS). Which factor would the nurse explain as the factor placing the neonate at the greatest risk for this syndrome?
(a) mother’s development of placenta previa
(b) neonate bom preterm
(c) mother receiving analgesia 4 hours before birth
(d) neonate with sluggish respiratory efforts after birth
Answer:
(b) neonate bom preterm
Explanation:
RDS is a developmental condition that primarily affects preterm infants before 35 weeks’ gestation because of inadequate lung development from deficient surfactant production. The development of placenta previa has little correlation with the development of RDS.
Although excessive analgesia can depress the neonate’s respiratory condition if it is given shortly before birth, the scenario presents no information that this has occurred. The neonate’s sluggish respiratory activity postpartum is not the likely cause of RDS but may be a sign that the neonate has the condition.
Question 47.
While the nurse is caring for a neonate at 32 weeks’ gestation in an isolette with continuous oxygen administration, the neonate’s mother asks why the neonate’s oxygen is humidified. What should the nurse tell the mother?
(a) “The humidity promotes expansion of the neonate’s immature lungs.”
(b) “The humidity helps to prevent viral or bacterial pneumonia.”
(c) “Oxygen is drying to the mucous membranes unless it is humidified.”
(d) “Circulation to the baby’s heart is improved with humidified oxygen.”
Answer:
(c) “Oxygen is drying to the mucous membranes unless it is humidified.”
Explanation:
Oxygen should be humidified before administration to help prevent drying of the mucous membranes in the respiratory tract. Drying impedes the normal functioning of cilia in the respiratory tract and predisposes to mucous membrane irritation. Humidification of oxygen does not promote the expansion of the immature lungs.
Expansion is promoted by placing the infant in a prone position or providing the preterm infant with surfactant medication. Humidified oxygen does not prevent viral
or bacterial pneumonia. In fact, in some nurseries, Staphylococcus aureus has been detected in moist environments and on the hands and nails of staff members, predisposing the neonate to pneumonia. Humidified oxygen does not improve blood circulation in the cardiac system.
Question 48.
A preterm neonate admitted to the neonatal intensive care unit at about 30 weeks’ gestation is placed in an oxygenated isolette. The neonate’s mother tells the nurse that she is planning to breastfeed the neonate. Which instructions about breastfeeding would be most appropriate?
(a) Breastfeeding is not recommended because the neonate needs increased fat in the diet.
(b) Once the neonate no longer needs oxygen and continuous monitoring, breastfeeding can be done.
(c) Breastfeeding is contraindicated because the neonate needs a high-calorie formula every 2 hours.
(d) Gavage feedings using breast milk can be given until the neonate can coordinate sucking and swallowing.
Answer:
(d) Gavage feedings using breast milk can be given until the neonate can coordinate sucking and swallowing.
Explanation:
Many intensive care units that care for high-risk neonates recommend that the mother pump her breasts, store the milk, and bring it to the unit so the neonate can be fed with it, even if the neonate is being fed by gavage. As soon as the neonate has developed a coordinated suck-and-swallow reflex, breastfeeding can begin.
Secretory immunoglobulin A, found in breast milk, is an important immunoglobulin that can provide immunity to the mucosal surfaces of the gastrointestinal tract. It can protect the neonate from enteric infections, such as those caused by Escherichia coli and Shigella species.
Some studies have also shown that breastfed preterm neonates maintain transcutaneous oxygen pressure and body temperature better than bottle-fed neonates. There is some evidence that breast milk can decrease the incidence of necrotizing enterocolitis.
The preterm neonate does not need additional fat in the diet. However, some neonates may need an increased caloric intake. In such cases, breast milk can be fortified with an additive to provide additional calories. Neonates who are receiving oxygen can breastfeed. During feedings, supplemental oxygen can be delivered by nasal cannula.
Question 49.
What is the best reason for assessing a neonate weighing 1,500 g at 32 weeks’ gestation for retinopathy of prematurity (ROP)?
(a) The neonate is at risk because of multiple factors.
(b) Oxygen is being administered at a level of 21%.
(c) The neonate was alkalotic immediately after birth.
(d) Phototherapy is likely to be prescribed by the health care provider (HCP).
Answer:
(a) The neonate is at risk because of multiple factors.
Explanation:
ROP, previously called retrolental fibroplasia, is associated with multiple risk factors, including high arterial blood oxygen levels, prematurity, and very low birth weight (<1,500 g). In the early acute stages of ROP, the neonate’s immature retinal vessels constrict. If vasoconstriction is sustained, vascular closure follows, and irreversible capillary endothelial damage occurs.
Normal room air is at 21%. Acidosis, not alkalosis, is commonly seen in preterm neonates, but this is not related to the development of ROP. Phototherapy is not related to the development of ROP. However, during phototherapy, the neonate’s eyes should be constantly covered to prevent damage from the lights.
Question 50.
Which subject should the nurse include when teaching the mother of a neonate diagnosed with retinopathy of prematurity (ROP) about possible treatment for complications?
(a) laser therapy
(b) anti-inflammatory eye drops
(c) frequent testing for glaucoma
(d) corneal transplants
Answer:
(a) laser therapy
Explanation:
Because the retina may become detached with ROP, laser therapy has been used successfully in some medical centers to treat ROP. Antiinflammatory eye drops may be used to treat seasonal allergies. ROP is not associated with glau-coma, so frequent testing is not necessary. Because the vessels of the eye are affected and not the corneas, corneal transplantation is not used.
Question 51.
Three days after admission of a neonate born at 30 weeks’ gestation, the neonatologist plans to assess the neonate for intraventricular hemorrhage (IVH). The nurse should plan to assist the neonatologist by preparing the neonate for which test?
(a) cranial ultrasonography
(b) arterial blood specimen collection
(c) radiographs of the skull
(d) complete blood count specimen collection
Answer:
(a) cranial ultrasonography
Explanation:
Neonates who weigh <1,500 g or are born at <34 weeks’ gestation are susceptible to IVH. Cranial ultrasound scanning can confirm the diagnosis. The spinal fluid will show an increased number of red blood cells. Arterial blood gas specimen collection is done to evaluate the neonate’s oxygen saturation level. Skull radiographs are not commonly used because of the danger of radiation.
Additionally, computed tomography scans have replaced the use of skull X-ray films because they can provide more definitive results. Complete blood count specimen collection is usually performed to determine the hemoglobin, hematocrit, and white blood cell count. The results are not specific for IVH.
Question 52.
Which finding would the nurse most expect to find in a neonate born at 28 weeks’ gestation who is diagnosed with intraventricular hemorrhage (IVH)?
(a) increased muscle tone
(b) hyperbilirubinemia
(c) bulging fontanelles
(d) hyperactivity
Answer:
(c) bulging fontanelles
Explanation:
A common finding of IVH is a bulging fontanelle. The most common site of hemorrhage is the periventricular subependymal germinal matrix, where there is a rich blood supply and where the capillary walls are thin and fragile. Rapid volume expansion, hypercarbia, and hypoglycemia contribute to the development of IVH.
Other common manifestations include neurologic signs such as hypotonia, lethargy, temperature instability, nystagmus, apnea, bradycardia, decreased hematocrit, and increasing hypoxia. Seizures also may occur. Hyperbilirubinemia refers to an increase in bilirubin in the blood and may be seen if bleeding was severe.
Question 53.
An infant bom premature at 34 weeks is receiving gavage feedings. The client holding her infant asks why the nurse places a pacifier in the infant’s mouth during these feedings. The nurse replies that the pacifier helps in what ways? Select all that apply.
(a) coordinates the swallowing of feedings
(b) encourages sucking behaviors
(c) improves weight gain
(d) instills a calming effect
(e) improves digestion
Answer:
(b) encourages sucking behaviors
(c) improves weight gain
(e) improves digestion
Explanation:
(b), (c), (e) Noimutritive sucking has been seen in infants as early as 28 weeks, and ultrasound examinations have shown thumb sucking in utero even earlier. Nonnutritive sucking encourages sucking behaviors that help a baby to maintain the sucking reflex needed for subsequent breast- or bottle-feedings. Nonnutritive sucking promotes digestion by stimulating secretions of GI peptides that help with gastric emptying.
Nonnutritive sucking has a calming effect that improves physiological stability. When it takes place during tube feedings it helps the newborn make the association between sucking and the sensation of a full stomach. Improved digestion and physiological stability lead to improved weight gain. Sucking on a pacifier during a tube feeding does not lead to improved swallowing of feedings because milk is directly into the stomach.
Question 54.
While the nurse is caring for a neonate bom at 32 weeks’ gestation, which finding would most suggest the infant is developing necrotizing entero¬colitis (NEC)?
(a) the presence of 1 rnL of gastric residual before a gavage feeding
(b) jaundice appearing on the face and chest
(c) an increase in bowel peristalsis
(d) abdominal distention
Answer:
(d) abdominal distention
Explanation:
Indications of NEC include abdominal distention with gastric retention and vomiting. Other signs may include lethargy, irritability, positive blood culture in stool, absent or diminished bowel sounds, apnea, diarrhea, metabolic acidosis, and unstable temperature. A gastric residual of 1 mL is not significant. Jaundice of the face and chest is associated with the neonate’s immature liver function and increased bilirubin, not NEC. Typically with NEC, the neonate would exhibit absent or diminished bowel sounds, not increased peristalsis.
Question 55.
Which statement by the mother of a neonate diagnosed with bronchopulmonary dysplasia (BPD) indicates effective teaching?
(a) “BPD is an acute disease that can be treated with antibiotics.”
(b) “My baby may require long-term respiratory support.”
(c) “Bronchodilators can cure my baby’s condition.”
(d) “My baby may have seizures later on in life because of this condition.”
Answer:
(b) “My baby may require long-term respiratory support.”
Explanation:
BPD is a chronic illness that may require prolonged hospitalization and permanent assisted ventilation. The disease typically occurs in compromised very-low-birth-weight neonates who require oxygen therapy and assisted ventilation for treatment of respiratory distress syndrome.
The cause is multifactorial, and the disease has four stages. The neonate’s activities may be limited by the disease. Antibiotics may be prescribed and bronchodilators may be used, but these medications will not cure the chronic disease state. Seizure activity is associated with periventricular-intraventricular hemorrhage, not BPD.
Question 56.
A preterm infant born 2 hours ago at 34 weeks’ gestation is experiencing rapid respirations, grunting, no breath sounds on one side, and a shift in location of heart sounds. The nurse should prepare to assist with which procedure?
(a) placement of the neonate on a ventilator
(b) administration of bronchodilators through the nares
(c) suctioning of the neonate’s nares with wall suction
(d) insertion of a chest tube into the neonate
Answer:
(d) insertion of a chest tube into the neonate
Explanation:
The client data support the diagnosis of pneumothorax, which would be confirmed with a chest X-ray. Pneumothorax is an accumulation of air in the thoracic cavity between the parietal and visceral pleurae and requires immediate removal of the accumulated air. Resolution is initiated with insertion of a chest tube connected to continuous negative pressure.
The neonate does not need to be placed on a ventilator unless there is evidence of severe respiratory distress. The goal of treatment is to reinflate the collapsed lung. Administering bronchodilators through the nares or suctioning the neonate’s nares would do nothing to aid in lung reinflation.
Question 57.
Which finding would lead the nurse to suspect that a neonate born at 34 weeks’ gestation receiving intravenous fluids has developed overhydration?
(a) hypernatremia
(b) polycythemia
(c) hypoproteinemia
(d) increased urine specific gravity
Answer:
(c) hypoproteinemia
Explanation:
Decreased protein or hypoproteinemia is a sign of overhydration, which can lead to patent ductus arteriosus or congestive heart failure. Bulging fontanelles, decreased serum sodium, decreased urine specific gravity, and decreased hematocrit are other signs of overhydration. Hypernatremia (increased serum sodium concentration) or increased urine specific gravity would suggest dehydration, not overhydration. Polycythemia evidenced by an elevated hematocrit would suggest hypoxia or congenital heart disorder.
Question 58.
A newborn weighing 6.5 lb (2,950 g) is to be given naloxone due to respiratory depression as a result of a narcotic given to the mother shortly before birth. The drug is to be given 0.01 mg/kg into the umbilical vein. The vial is marked 0.4 mg/mL. How many milligrams would the newborn receive? Record your answer using two decimal places ................. mg.
Answer:
0.03 mg
2,950 g = 2.95 kg
2.95 kg x 0.01 mg = 0.029 mg,
rounded to 0.03 mg
Question 59.
After plotting a postterm neonate’s weight and length on a growth chart, the nurse determines that the infant is large for gestational age (LGA). Which laboratory value is most important for the nurse to assess next?
(a) blood type
(b) blood glucose
(c) hemoglobin/hematocrit
(d) white blood cell count
Answer:
(b) blood glucose
Explanation:
LGA neonates are at risk for hypoglycemia soon after birth because they frequently have increased insulin levels. All LGA infants should have blood glucose testing soon after birth. Accelerated growth states can lead to increased hemoglobin production in utero.
Hematocrit screening is needed if an LGA neonate shows signs and symptoms of polycythemia/hyperviscosity syndrome, including plethora, lethargy, or respiratory distress. A white blood cell count is only needed if the neonate has signs of sepsis. Review of the neonate’s blood type would be indicated if there was a risk for A-B-0 or Rh incompatibilities.
Question 60.
A neonate born by cesarean at 42 weeks’ gestation, weighing 4.1 kg (9 lb), with Apgar scores of 8 at 1 minute and 9 at 5 minutes after birth, devel¬ops an increased respiratory rate and tremors of the hands and feet 2 hours postpartum. What is the priority problem for this neonate?
(a) ineffective airway clearance
(b) hyperthermia
(c) decreased cardiac output
(d) hypoglycemia
Answer:
(d) hypoglycemia
Explanation:
Increased respiratory rate and tremors are indicative of hypoglycemia, which commonly affects the postterm neonate because of depleted glycogen stores. There is no indication that the neonate has ineffective airway clearance, which would be evidenced by excessive amounts of mucus or visualization of meconium on the vocal cords.
Lethargy, not tremors, would suggest infection or hyperthermia. Furthermore, the postterm neonate typically has difficulty maintaining temperature, resulting in hypothermia, not hyperthermia. Decreased cardiac output is not indicated, particularly because the neonate was born by cesarean birth, which is not considered a difficult birth.
Question 61.
At a home visit, the nurse assesses a neonate born vaginally at 41 weeks’ gestation 5 days ago. Which of these findings warrants further assessment?
(a) frequent hiccups
(b) loose, watery stool in diaper
(c) pink papular vesicles on the face
(d) dry, peeling skin
Answer:
(b) loose, watery stool in diaper
Explanation:
A loose, watery stool in the diaper is indicative of diarrhea and needs immediate attention. The infant may become severely dehydrated quickly because of the higher percentage of water content per body weight in the neonate, compared with the adult. Frequent hiccups are considered normal in a neonate and do not warrant additional investigation. Pink papular vesicles (erythema toxi-cum) on the face are considered normal in a neonate and disappear without treatment. Dry, peeling skin is normal in a postterm neonate.
Question 62.
The nurse assists the health care provider (HCP) with a lumbar puncture on a postterm neonate with signs of sepsis. What should the nurse do to assist in this procedure? Select all that apply.
(a) Administer the IV antibiotic.
(b) Hold the neonate steady in the correct position.
(c) Ensure a patent airway.
(d) Maintain a sterile field.
(e) Obtain a serum glucose level.
Answer:
(b) Hold the neonate steady in the correct position.
(c) Ensure a patent airway.
(d) Maintain a sterile field.
Explanation:
(b), (c), (d) Holding the neonate steady and in the proper position will help ensure a safe and accurate lumbar puncture. The neonate is usually held in a “C” position to open the spaces between the vertebral column. This position puts the neonate at risk for airway obstruction. Thus, ensuring the patency of the airway is the first priority, and the nurse should observe the neonate for adequate ventilation. Maintaining a sterile field is important to avoid infection in the neonate. It is not necessary to administer antibiotics or obtain a serum glucose level during the procedure.
Question 63.
A neonate is admitted to the neonatal intensive care unit for observation with a diagnosis of probable meconium aspiration syndrome (MAS). The neonate weighs 10 lb, 4lb (4,650 g) and is at 41 weeks’ gestation. What would be the priority problem for this neonate?
(a) impaired skin integrity
(b) hyperglycemia
(c) risk for impaired parent-infant-child attachment
(d) impaired gas exchange
Answer:
(d) impaired gas exchange
Explanation:
The priority problem for the neonate with probable MAS is impaired gas exchange related to the effects of respiratory distress. Obstruction of the airways may be complete or partial. Meconium aspiration may lead to pneumonia or pneumothorax. Establishing adequate respirations is the primary goal. Impaired skin integrity is a concern, but establishing and maintaining an airway and gas exchange is always the priority.
Hypoglycemia tends to be a problem for large-for-gestational-age babies, not hyperglycemia. If the parents do not express interest or concern for the neonate, then the risk for impaired parent-infant-child attachment may be appropriate once the airway is established.
Question 64.
The neonate in the nurse’s care has a pneumothorax. The nurse knows the signs of early decompensation and observes carefully for changes in which assessments. Select all that apply.
(a) blood pressure
(b) temperature
(c) urinary output
(d) color
(e) heart rate
Answer:
(d) color
(e) heart rate
Explanation:
(d), (e) The pneumothorax may affect cardiac output, thus affecting perfusion and causing a decrease in blood pressure and changes in color from pallor to cyanosis. As the neonate attempts to compensate, bradycardia or tachycardia may be exhibited. A change in temperature and urinary output are very late signs of decompensation.
Question 65.
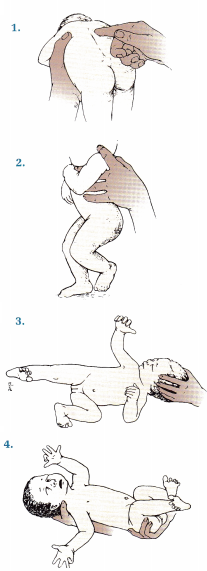
The nurse assesses the term newborn in the picture. The nurse knows to further assess for an elevation of which lab value?
(a) bilirubin
(b) BUN
(c) hematocrit
(d) potassium
Answer:
(a) bilirubin
Explanation:
Bruising causes red blood cell (RBC) destruction. A byproduct of RBC hemolysis is biliru¬bin, and thus infants who have significant bruising will have increased levels of bilirubin. Hematocrits may be decreased with bruising not increased. Bruising will have no effect on the BUN. Bruising in term infants does not affect potassium levels.
Question 66.
When developing a nursing care plan for an infant receiving phototherapy, the nurse should include what information in the plan of care? Select all that apply.
(a) adequate skin exposure to phototherapy
(b) allowing mother to hold infant as much as she wishes
(c) eye protection
(d) supplemental water between feedings
(e) thermoregulation
Answer:
(a) adequate skin exposure to phototherapy
(c) eye protection
(e) thermoregulation
Explanation:
(a) (c) (e) For phototherapy to be effective, the skin needs to be exposed to the light waves to allow for the conversion of bilirubin to water-soluble iso¬mers that are excreted without further metabolism by the liver. Eye protection is necessary to prevent retinal damage. As infants are usually dressed only in a diaper for maximum skin exposure to the light, thermoregulation is a concern.
The infants can be too cool or potentially overheat if the pho-totherapy lights are not positioned correctly. Most often mothers are allowed to hold their infants for feeding; there is usually a 30-minute time limit. In order for the phototherapy to be effective, the baby must be under the lights except for feedings. Water supplementation is not indicated as the baby needs the calories and nutrients that breast milk or formula provide. Extra water feedings will not prevent hyperbilirubinemia or decrease total serum bilirubin levels.
Question 67.
The nurse assesses a 15-hour-old infant and finds jaundice. What is the priority action the nurse needs to take?
(a) Continue with normal newborn care.
(b) Notify the health care provider of the finding.
(c) Provide an extra feeding for the infant.
(d) Wait and assess the skin color when the infant is over 24 hours old.
Answer:
(b) Notify the health care provider of the finding.
Explanation:
Jaundice that appears before 24 hours of age is considered pathologic. Jaundice appears when bilirubin levels reach 5 to 7 mg/dL (85.5 to 120 prnol). The health care provider should be notified for intervention to prevent kernicterus.
This disease process can cause lifelong central nervous system damage. Disregarding the finding or waiting to report the finding will delay treatment and potentially cause permeant harm to the infant. Providing an extra feeding will have no effect on the hyperbili rubinemia that is causing the jaundice.
Question 68.
The lab results show that a mother has a blood type of O positive and her infant has the blood type of A negative. As part of the plan of care, the nurse should assess the infant for which condition?
(a) breast milk jaundice
(b) pathologic hyperbilirubinemia
(c) physiologic hyperbilirubinemia
(d) Rh incompatibility
Answer:
(b) pathologic hyperbilirubinemia
Explanation:
With mother’s blood type being O and her infant being type A, there is the potential for an ABO blood antibody antigen reaction. The infant’s A antigen enters the mother, the mother produces antibodies, the antibodies then reenter the infant causing hemolysis and hyperbilirubinemia. Antigen-antibody reactions are a type of pathologic hyperbilirubinemia not physiologic. For there to be Rh incompatibility the mother would need to be O negative not O positive. Blood types have no influence on breast milk jaundice.
Question 69.
The nurse is providing teaching to the mother of a newborn with early jaundice about the condition’s progression. The nurse knows that the teaching regarding hyperbilirubinemia was successful when the mother makes which response?
(a) “Kernicterus is a consequence of elevated bilirubin levels and has possible lifelong effects.”
(b) “My baby should not get hyperbilirubinemia if I place him near a window in the sun light.”
(c) “My baby will be 3 days old at discharge, and I will not need to worry about hyperbilirubinemia.”
(d) “Since I’m exclusively breastfeeding, the risk of my baby having hyperbilirubinemia is very low.”
Answer:
(a) “Kernicterus is a consequence of elevated bilirubin levels and has possible lifelong effects.”
Explanation:
Kernicterus is a consequence of elevated bilirubin levels that can have lifelong central nervous effects. This is a true statement. Infants that have elevated bilirubin levels need close monitoring until the bilirubin levels fall. Placing the infant in the sun light may cause thermoregulation issues such as overheating. Infants will burn very easily in the sun.
Bilirubin level peak at 72 to 120 hours of age. If a baby is discharged at 3 days, the baby may need follow-up until the peak has been determined and the levels fall. Exclusive breastfeeding is a risk factor for an infant developing severe hyperbilirubinemia.
Question 70.
While performing an assessment, the nurse notes the infant’s jaundice has moved from the nipple line to the umbilicus in the past 24 hours. How does the nurse interpret this physical finding?
(a) A decrease in bilirubin level is probable.
(b) An increase in bilirubin level is probable.
(c) No further assessment is necessary.
(d) Where jaundice is located on the baby is not indicative of bilirubin level.
Answer:
(b) An increase in bilirubin level is probable.
Explanation:
Jaundice progresses in a cephalocaudal manner. The jaundice increased from the nipple line to the umbilicus indicates the bilirubin levels are increasing in this infant. Continued assessment is necessary to monitor the rise in bilirubin levels with the potential need for phototherapy to prevent possible kernicterus.
Question 71.
Which instructions should the nurse give to the parents of a neonate diagnosed with hyperbilirubinemia who is receiving phototherapy?
(a) Keep the neonate’s eyes completely covered.
(b) Use a regular diaper on the neonate.
(c) Offer feedings every 4 hours.
(d) Check the rectal temperature every 8 hours.
Answer:
(a) Keep the neonate’s eyes completely covered.
Explanation:
To prevent eye damage from phototherapy, the eyes must remain covered at all times while under the lights. The eye patches can be removed when the neonate is held out of the lights by the parents for feeding. Instead of a regular diaper, a “string” diaper or disposable face mask may be used to help contain loose stools, while allowing maximum skin exposure.
Feeding formula or breast milk every 2 to 3 hours is recommended to prevent hypoglycemia and to encourage gastrointestinal motility. Because the phototherapy lights can overheat the neonate, the temperature should be checked by the axillary route every 2 to 4 hours.
Question 72.
While caring for a term neonate who has been receiving phototherapy for 8 hours, the nurse should notify the health care provider (HCP) if which finding is noted?
(a) bronze-colored skin
(b) maculopapular chest rash
(c) urine specific gravity of 1.018
(d) absent Moro reflex
Answer:
(d) absent Moro reflex
Explanation:
An absent Moro reflex, lethargy, opisthotonos, and seizures are symptoms of bilirubin encephalopathy, which, although rare, can be life- threatening. Bronze discoloration of the skin and maculopapular chest rash are normal and are caused by the phototherapy. They will disappear once the phototherapy is discontinued. A urine specific gravity of 1.001 to 1.020 is normal in term neonates
Question 73.
A nurse is attempting to resuscitate a neonate. Thirty seconds of chest compressions have been completed. The neonate’s heart rate remains < 60 bpm. Epinephrine is given. What is the expected outcome for a neonate who has received epinephrine during resuscitation?
(a) increased urine output
(b) a normal heart rate
(c) pain relief
(d) sedation
Answer:
(b) a normal heart rate
Explanation:
Epinephrine is given for severe bradycardia and hypotension. An expected outcome would be an increased heart rate to a normal range. Epinephrine decreases renal blood flow, so a decrease in urine output would be expected. Epinephrine also stimulates alpha- and beta-adrenergic receptors, which do not offer pain relief or sedation.
Question 74.
A mother is visiting her neonate in the neonatal intensive care unit. Her baby is fussy, and the mother wants to know what to do. In order to quiet a sick neonate, what can the nurse teach the mother to do?
(a) Bring in toys for distraction.
(b) Place a musical mobile over the crib.
(c) Stroke the neonate’s back.
(d) Use constant, gentle touch.
Answer:
(d) Use constant, gentle touch.
Explanation:
Neonates that are sick do not have the physical resources or energy to respond to all elements of the environment. The use of a constant touch provides comfort and only requires one response to a stimulus. To comfort a sick neonate, the care provider applies gentle, constant physical support or touch. Toys for distraction are not developmentally appropriate for a neonate.
Sick neonates react to any stimulus; in responding, the sick neonate may have increased energy demands and increased oxygen requirements. A musical mobile may be too much audio stimulation and thus increases energy and oxygen demands. Repetitive touching with a hand going off and on the neonate, as with stroking or patting, requires the neonate to respond to every touch, thus increasing energy and oxygen demands.
Question 75.
A neonate born at 40 weeks’ gestation admitted to the nursery is found to be hypoglycemic. At 4 hours of age, the neonate appears pale, and his pulse oximeter is reading 75% on room air. What should the nurse do?
(a) Increase the IV rate.
(b) Provide supplemental oxygen.
(c) Record the finding on the medical record, and repeat the reading in 30 minutes.
(d) Wrap the neonate to increase body temperature.
Answer:
(b) Provide supplemental oxygen.
Explanation:
The recommended pulse oximetry reading in a full-term neonate is 95% to 100%. The saturation reading of only 75% is an indication that the neonate is not adequately oxygenating in room air. Providing supplemental oxygen will increase the neonate’s oxygen saturation. Increasing the IV rate will not improve the oxygen saturation.
Documenting the findings and taking no action is not appropriate with a saturation of 75%. Wrapping and increasing the body temperature of the neonate may increase the saturation reading only if it is inaccurate due to cold extremities. Caution must be used because overheating a neonate can be harmful.
Question 76.
A neonate with heart failure is being discharged home. When teaching the parents about the neonate’s nutritional needs, what should the nurse explain?
(a) Fluids must be restricted.
(b) Decreased activity levels should reduce the
need for additional calories.
(c) The formula should be low in sodium.
(d) The neonate may need a more calorie-dense formula.
Answer:
(d) The neonate may need a more calorie-dense formula.
Explanation:
Neonates with heart failure may need a calorie-dense formula to provide extra calories for growth. Fluids should not be restricted because the nutritional requirements are based on calories per ounce of formula. Decreasing fluid intake will decrease the calories needed for growth.
These neonates may have limited energy due to their heart condition but have a high caloric need to stimulate proper growth and development. The sodium level should be at a normal level to ensure adequate fluid and electrolyte balance unless prescribed by the health care provider (HCP)
Question 77.
During an assessment of a neonate born at 33 weeks’ gestation, a nurse finds and reports a heart murmur. An echocardiogram reveals patent ductus arteriosus, for which the neonate received indomethacin. What is the expected outcome after the administration of indomethacin to a neonate with patent ductus arteriosus?
(a) closure of a patent ductus arteriosus
(b) decreased bleeding time
(c) increased gastrointestinal function
(d) increased renal output
Answer:
(a) closure of a patent ductus arteriosus
Explanation:
The indication for the use of indomethacin is to close a patent ductus arteriosus. Adverse effects include decreased renal blood flow, platelet dysfunction with coagulation defects, decreased GI motility, and an increase in necrotizing enterocolitis. Thus, increased bleeding time, decreased gastrointestinal function, and decreased renal output would be expected outcomes after the administration of indomethacin.
Question 78.
A nurse is reviewing a client’s maternal prenatal record and notes that the mother used narcotics during her pregnancy. What nursing intervention should the nurse implement when caring for a drug-exposed neonate?
(a) Assess vital signs including blood pressure every hour.
(b) Minimize environmental stimuli.
(c) Place the infant in a well-lighted area.
(d) Increase eye contact with the caregiver.
Answer:
(b) Minimize environmental stimuli.
Explanation:
A quiet environment with decreased stimulation is the best treatment for a drug-exposed neonate. The drug-exposed neonate has a limited ability to deal with stress and cope with stimuli. Assessing vital signs with blood pressure every hour will disturb the neonate’s rest periods and cause increased physical and psychological demands. Placement in a well-lighted environment and increasing eye contact can be overwhelming for the neonate and will increase the neonate’s stress level.
Question 79.
The nurse is receiving over the telephone a laboratory results report of a neonate’s blood glucose level. What should the nurse do?
(a) Write down the results, read back the results to the caller from the laboratory, and receive confirmation from the caller that the nurse understands the results.
(b) Repeat the results to the caller from the laboratory, write the results on scrap paper first, and then transfer the results to the medical record.
(c) Indicate to the caller that the nurse cannot receive verbal results from laboratory tests for neonates, and ask the laboratory to bring the written results to the nursery.
(d) Request that the laboratory send the results by email to transfer to the client’s medical record.
Answer:
(a) Write down the results, read back the results to the caller from the laboratory, and receive confirmation from the caller that the nurse understands the results.
Explanation:
To ensure client safety, the nurse should first write the results on the medical record 03. then read them back to the caller, and wait for the caller to confirm that the nurse has understood the results. Using scrap paper increases the risk of losing the results as well as transcription errors. The nurse may receive results by telephone, and while electronic transfer to the client’s medical record is appropriate, the nurse can also accept the telephone results if the laboratory has called the results to the nursery. Sending client information via email is unacceptable due to potential security and privacy issues.
Question 80.
A multiparous client who has a neonate diagnosed with hemolytic disease of the newborn asks the nurse why the neonate has developed this problem. Which response by the nurse would be most appropriate?
(a) “You are Rh positive, and the baby is Rh negative.”
(b) “You and the baby are both Rh negative.”
(c) “You are Rh negative, and the baby is Rh positive.”
(d) “The baby and you are both Rh positive.”
Answer:
(c) “You are Rh negative, and the baby is Rh positive.”
Explanation:
Hemolytic disease of the newborn is associated with Rh problems. Hemolytic disease of the newborn occurs most commonly when the mother is Rh negative and the infant is Rh positive. About 13% of Caucasians, 7% to 8% of people of African descent, and 1% of people of Asian descent are Rh negative. Rh-positive cells enter the mother’s Rh-negative bloodstream, and antibodies to the Rh-positive cells are produced. In a subsequent pregnancy, the antibodies cross the placenta to the Rh-positive fetus and begin the destruction of Rh-positive cells through hemolysis. This results in severe fetal anemia.
Question 81.
After teaching the multiparous mother about hemolytic disease of the newborn and Rh sensitization, the nurse determines that the client understands why she was not sensitized during her other pregnancy when she makes which statement?
(a) “My other baby had a different father.”
(b) “Like most women, I have immunity against the Rh factor.”
(c) “Antibodies are not usually formed until after exposure to an antigen.”
(d) “My blood could not neutralize antibodies formed from my first pregnancy.”
Answer:
(c) “Antibodies are not usually formed until after exposure to an antigen.”
Explanation:
The problem of Rh sensitivity arises when the mother’s blood develops antibodies after fetal red blood cells enter the maternal circulation. In cases of Rh sensitivity, this usually does not occur until after the first pregnancy. Hence, hemo-lytic disease of the newborn is rare in a primiparous client. A mismatched blood transfusion in the past or an unrecognized spontaneous abortion could also result in hemolytic disease because the transfusion or abortion would have the same effects on the client.
The statement about the other baby having a different father may be true. However, if both fathers were Rh positive, then sensitization could occur. Most women do not have immunity against the antibodies formed when Rh-positive cells enter the mother’s bloodstream. Antibodies are not neutralized by the mother’s system.
Question 82.
After teaching a multiparous client about the effects of hemolysis due to Rh sensitization on the neonate at birth, the nurse determines that the client needs further instruction when the mother reports that the neonate may have which complication?
(a) cardiac decompensation
(b) polycythemia
(c) anemia
(d) splenic enlargement
Answer:
(b) polycythemia
Explanation:
The Rh-sensitized neonate generally does not have problems related to polycythemia. Therefore, the client needs additional teaching. In general, moderate-to-severe Rh sensitization can cause anemia, enlarged spleen, and cardiac decompensation. Cardiac decompensation (as in heart failure) occurs because of severe anemia. Anemia is caused by the destruction of red blood cells by antibodies as the severity of hemolytic disease of the neonate increases. Splenic enlargement is caused by the excessive destruction of fetal red blood cells.
Question 83.
After birth, a direct Coombs test is performed on the umbilical cord blood of a neonate with Rh-positive blood born to a mother with Rh-negative blood. The nurse explains to the client that this test is done to detect which information?
(a) appropriate dose of Rho(D) immune globulin
(b) degree of anemia in the neonate
(c) initial bilirubin level
(d) presence of maternal antibodies
Answer:
(d) presence of maternal antibodies
Explanation:
A direct Coombs test is also known as a direct antiglobulin test (DAT). The test is done on umbilical cord blood to detect maternal antibodies coating the neonate’s red blood cells. Rho(D) immune globulin doses are determined by amount of Rh-positive neonatal blood found in the mother after birth. Hematocrit is used to detect anemia. A direct Coombs test does not measure bilirubin but may help explain the underlying cause of increased bilirubin levels.
Question 84.
The nurse recognizes that teaching about the need for an exchange transfusion in a neonate with erythroblastosis fetalis has been effective if the parents describe the purpose of the transfusion is do what?
(a) to replenish the neonate’s leukocytes
(b) to restore the fluid and electrolyte balance
(c) to correct the neonate’s anemia
(d) to replace Rh-negative blood with Rh-positive blood
Answer:
(c) to correct the neonate’s anemia
Explanation:
An exchange transfusion is done to reduce the blood concentration of bilirubin and correct the anemia. The exchange transfusion does not replenish the white blood cells or restore the fluid and electrolyte balance. The neonate’s Rh-positive blood is replaced by Rh-negative blood.
Question 85.
The nurse explains to the mother of a neonate diagnosed with erythroblastosis fetalis that the exchange transfusion is necessary to prevent damage primarily to which organ in the neonate?
(a) kidneys
(b) brain
(c) lungs
(d) liver
Answer:
(b) brain
Explanation:
The organ most susceptible to damage from uncontrolled hemolytic disease is the brain. Bilirubin levels increase as the red blood cells are destroyed. Bilirubin crosses the blood-brain barrier and damages the cells of the central nervous system. This condition, called kernicterus, is potentially fatal. Although the kidneys, lungs, and liver may be affected by increased bilirubin levels, the brain will sustain the most life-threatening injury.
Question 86.
The nurse is caring for a newborn of a pri- miparous woman with insulin-dependent diabetes. When the mother visits the neonate at 1 hour after birth, the nurse explains to the mother that the neonate is being closely monitored for symptoms of hypoglycemia because of which reason?
(a) increased use of glucose stores during a difficult labor and birth process
(b) interrupted supply of maternal glucose and continued high neonatal insulin production
(c) a normal response that occurs during transition from intrauterine to extrauterine life
(d) increased pancreatic enzyme production caused by decreased glucose stores
Answer:
(b) interrupted supply of maternal glucose and continued high neonatal insulin production
Explanation:
Glucose crosses the placenta, but insulin does not. Hence, a high maternal blood glucose level causes a high fetal blood glucose level. This causes the fetal pancreas to secrete more insulin. At birth, the neonate loses the maternal glucose source but continues to produce much insulin, which commonly causes a drop in blood glucose levels (hypoglycemia), usually at 30 to 60 minutes postpartum.
Most neonates do not develop hypoglycemia if their mothers are not insulin dependent unless they are preterm. Therefore, hypoglycemia is not a normal response as the neonate transitions to extrauterine life.
Question 87.
When caring for a neonate weighing 4,564 g (10 lb, 1lb) born vaginally to a mother with diabetes, the nurse should assess the neonate for fracture of which area?
(a) clavicle
(b) skull
(c) wrist
(d) rib cage
Answer:
(a) clavicle
Explanation:
Infants born to mothers with diabetes tend to be larger than average, and this neonate weighs 10 lb, 1lb(4,564 g). The most common fractures are those of the clavicle and long bones, such as the femur. In a neonate, the skull bones are not fused and move to allow for vaginal birth, so skull fracture is rarely seen. Wrist and rib cages are rarely fractured.
Question 88.
While caring for a neonate of a woman with diabetes soon after birth, the nurse has fed the newborn formula to prevent hypoglycemia. The nurse checks the neonate’s blood glucose level, and it is 60 mg/dL (3.3 mmol/L), but the neonate continues to exhibit jitteriness and tremors. What should the nurse do first?
(a) Request a prescription for a blood calcium level.
(b) Administer intravenous glucose.
(c) Assess the neonate’s temperature.
(d) Refeed the infant.
Answer:
(a) Request a prescription for a blood calcium level.
Explanation:
This neonate has a mother with diabetes who tends to have higher calcium levels, which can cause secondary hypoparathyroidism in their neonates. This lack of calcium may be the cause of the tremors and jitteriness of this neonate, and a serum calcium level should be obtained. Other factors contributing to hypocalcemia in neonates include hypophosphatemia from tissue metabolism, vitamin D antagonism from increased cortisol levels, and decreased serum magnesium levels.
Beginning a glucose IV based on a normal infant glucose level would have no benefit. Rechecking the neonate’s temperature is a precaution that can be taken to assure that it is within normal limits but is not the action to take first. Refeeding the infant who has a normal newborn blood glucose level is not appropriate.
Question 89.
The nurse is caring for a neonate weighing 4,536 g (10 lb) who was bom via cesarean birth 1 hour ago to a mother with insulin-dependent diabetes. She asks the nurse, “Why is my baby in the neonatal intensive care unit?” The nurse bases a response on the understanding that neonates of mothers with diabetes commonly develop which condition?
(a) anemia
(b) persistent pulmonary hypertension
(c) hemolytic disease
(d) hypoglycemia
Answer:
(d) hypoglycemia
Explanation:
Hypoglycemia is caused by the rapid depletion of glucose stores. In addition, neonates born to women with insulin-dependent diabetes are about seven times more likely to suffer from respiratory distress syndrome than neonates born to nondiabetic women.
This neonate should be closely monitored for symptoms of hypoglycemia and respiratory distress. Neonates of diabetic mothers commonly have polycythemia, not anemia. Anemia and hemolytic disease are associated with erythroblastosis fetalis. Persistent pulmonary hypertension is associated with meconium aspiration syndrome.
Question 90.
While assessing a neonate weighing 3,175 g (7 lb) who was born at 39 weeks’ gestation to a primiparous client who admits to opiate use during pregnancy, which finding would alert the nurse to possible opiate withdrawal?
(a) bradycardia
(b) high-pitched cry
(c) sluggishness
(d) hypocalcemia
Answer:
(a) bradycardia
Explanation:
Manifestations of opiate withdrawal in the neonate, known as neonatal abstinence syndrome (NAS), include an increased central nervous system irritability, gastrointestinal symptoms, and metabolic, vasomotor, and respiratory disturbances. These signs usually appear within 72 hours and persist for several days. Infants have diarrhea not con-stipation. They typically display increased sucking behaviors, but are poor feeders. Vomiting is common with babies who have NAS.
Question 91.
The nurse recognizes that a parent needs more teaching about the complications of neonatal opioid exposure when the parent states that the baby may exhibit which gastrointestinal problem?
(a) constipation
(b) increased sucking
(c) poor feeding
(d) vomiting
Answer:
(c) poor feeding
Explanation:
Neonates experiencing opiate withdrawal have gastrointestinal problems similar to those of adults withdrawing from opiates. The neonates exhibit poor sucking, vomiting, drooling, diarrhea, regurgitation, and anorexia. In addition, they are difficult to console and difficult to feed. Because of these problems, the neonate withdrawing from opiates needs to be monitored carefully to prevent dehydration.
Neonates with opiate exposure experience hypertonia, not hypotonia, due to increased central nervous system irritability. Diarrhea, not constipation, is seen in these neonates. Abdominal distention is associated with necrotizing enterocolitis, not opiate withdrawal.
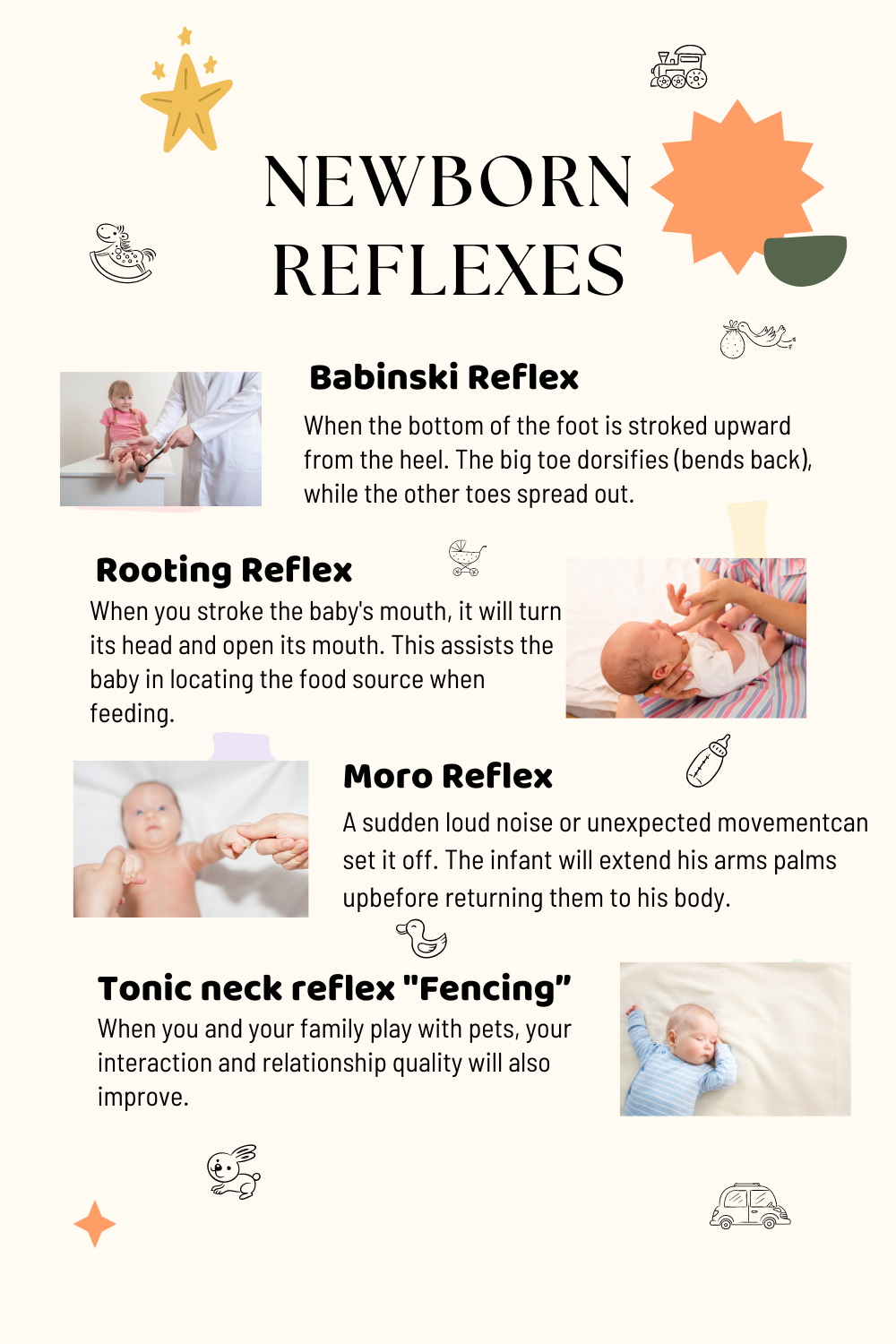
Question 92.
When teaching a primiparous client who used cocaine during pregnancy how to comfort her fussy neonate, the nurse can advise the mother to use which intervention?
(a) Tightly swaddle the neonate.
(b) Feed the neonate extra, high-calorie formula.
(c) Keep the neonate in a brightly lit environment.
(d) Touch the baby only when he or she is crying.
Answer:
(a) Tightly swaddle the neonate.
Explanation:
A neonate undergoing cocaine withdrawal is irritable, often restless, difficult to console, and often in need of increased activity. It is commonly helpful to swaddle the neonate tightly with a blanket, offer a pacifier, and cuddle and rock the neonate. Offering extra nourishment is not advised because overfeeding tends to increase gastrointestinal problems such as vomiting, regurgitation, and diarrhea.
Environmental stimuli such as bright lights and loud noises should be kept to a minimum to decrease agitation. Minimizing touching of the neonate only when he or she is crying will not aid the bonding process between mother and neonate. Frequent holding and touching are permissible.
Question 93.
A neonate born at 38 weeks’ gestation is admitted to the neonatal nursery for observation. The neonate’s mother, who is positive for human immunodeficiency virus (HIV) infection, has received no prenatal care. The mother asks the nurse if her neonate is positive for HIV. The nurse can tell the mother which information?
(a) “More than 50% of neonates born to mothers who are positive for HIV will be positive at 18 months of age.”
(b) “An enlarged liver at birth generally means the neonate is HIV positive.”
(c) “A complete blood count analysis is the primary method for determining whether the neonate is HIV positive.”
(d) “We will test your baby now, but testing will need to be repeated for an accurate diagnosis.”
Answer:
(d) “We will test your baby now, but testing will need to be repeated for an accurate diagnosis.”
Explanation:
New recommendations state that viro- logic diagnostic testing at birth should be considered for infants at high risk of HIV infection, but it may take several months before an accurate diagnosis can be made. New guidelines suggest that infants should be tested at 2 to 3 weeks, 1 to 2 months, and again 4 to 6 months. It is estimated that 15% to 30% of all HIV-positive mothers without treatment will give birth to HIV-positive infants.
With appropriate drug intervention to the mother during pregnancy, 95% of these neonates can be born unaffected. An enlarged liver at birth is associated with erythroblastosis fetalis, not HIV infection. Virologic testing, such as deoxyribonucleic acid polymerase chain reaction, viral culture, or ribonucleic acid plasma assay, can diagnose HIV infection by 6 months of age and commonly in the first month.
Question 94.
When caring for a multiparous client who is human immunodeficiency virus (HIV) positive and asking to breastfeed her neonate as soon as possible, the nurse should include which instructions about breast milk in the teaching plan?
(a) It may help prevent the spread of the HIV virus.
(b) It contains antibodies that can protect the neonate from HIV.
(c) It can be beneficial for the bonding process.
(d) It has been found to contain the retrovirus HIV.
Answer:
(d) It has been found to contain the retrovirus HIV.
Explanation:
Breast milk has been found to contain the retrovirus HIV. In general, mothers are discouraged from breastfeeding if they are HIV positive because of the risk of possible transmission of the vims if the neonate is HIV negative. Breast milk does contain some immunoglobulins, but it does not protect the neonate from HIV infection.
Question 95.
While caring for the neonate of a human immunodeficiency virus positive mother, the nurse prepares to administer a prescribed vitamin K intramuscular injection at 1 hour after birth. Which action should the nurse do first?
(a) Bathe the neonate.
(b) Place the neonate under a radiant warmer.
(c) Wash the injection site with povidone-iodine solution.
(d) Wait until the first dose of antiretroviral medication is given.
Answer:
(a) Bathe the neonate.
Explanation:
Newborns are typically bathed 2 to 4 hours after birth when their temperatures have had time to stabilize, but early/immediate bathing is recommended for the infants of HIV-positive mothers to decrease blood exposure. Placing the neonate under the radiant warmer for the vitamin K injection is not necessary unless the neonate’s temperature is subnormal.
Washing the injection site with povidone-iodine is not recommended and may increase the risk for possible allergy to iodine preparations. The first dose of zidovudine is given when the newborn is 6 to 12 hours old, but vitamin K is recommended to be given within an hour of birth to be most effective. Therefore, the vitamin K should not be delayed.
Question 96.
A 6-hour-old neonate born at 38 weeks’ gestation by cesarean birth after prolonged rupture of the membranes and a maternal oral temperature of 102°F (38.8°C) is being observed for signs and symp¬toms of infection. Which sign would alert the nurse to notify the health care provider (HCP)?
(a) WBC 15,000 cells/mm3 (15 x 109/L)
(b) apical heart rate of 132 bpm
(c) behavioral changes
(d) warm, moist skin
Answer:
(c) behavioral changes
Explanation:
Symptoms of infection in a neonate include subtle behavioral changes, such as lethargy and irritability, and color changes such as pallor or cyanosis. Other symptoms include temperature instability, poor feeding, gastrointestinal disorders, hyperbilirubinemia, and apnea.
An elevated white blood cell count possibly as high as 30,000 cells/ mm3 (30 x 109/L) or more, may be normal during the first 24 hours. An apical heart rate of 132 bpm is normal. Warm, moist skin is not a typical sign of infection in neonates. Typically, temperature instability is common. The neonate’s temperature is low, and the skin is cool and dry.
Question 97.
The nurse is caring for a neonate diagnosed with early-onset sepsis and is being treated with intravenous antibiotics. Which instruction will the nurse include in the parents’ teaching plan?
(a) Wear protective gear near the isolation incubator.
(b) Visit but do not touch the neonate.
(c) Wash hands thoroughly before touching the neonate.
(d) Wear a mask when holding the neonate.
Answer:
(c) Wash hands thoroughly before touching the neonate.
Explanation:
The parents of a neonate with an infection should be allowed to participate in daily care as long as they use good handwashing technique. This includes touching and holding the neonate. It is not necessary for parents to wear protective gear near the isolation incubator.
Restricting parental visits has not been shown to have any effect on the infection rate and may have detrimental effects on the neonate’s psychological development. Normally, the neonate does not need to be isolated. The baby will not spread sepsis via respiratory droplets to parents, so it is not necessary for the parents to wear a mask.
Question 98.
A female neonate bom vaginally at term with a cleft lip and cleft palate is admitted to the regular nursery. Which action should the nurse take the first time that the parents visit the neonate in the nursery?
(a) Explain the surgical interventions that will be performed.
(b) Stress that this defect is not life-threatening.
(c) Emphasize the neonate’s normal characteristics.
(d) Reassure the parents about the success rate of the surgery.
Answer:
(c) Emphasize the neonate’s normal characteristics.
Explanation:
On the initial visit, the parents may be shocked, fearful, and anxious. Nursing care should include spending time with the parents to allow them to express their emotions. The nurse should initially emphasize the neonate’s normal charac-teristics. After the parents have had sufficient time to adjust to the neonate’s special needs, surgical interventions can be discussed.
Telling the parents that this is not a life-threatening defect or that everything will be all right after the surgery is not helpful. Doing so discounts their feelings. Reassuring the parents about the success rate of the surgery can be done once the parents have had time to adjust to the neonate and express their emotions.
Question 99.
After teaching the parents of a neonate born with a cleft lip and cleft palate about appropriate feeding techniques, the nurse determines that the mother needs further instruction when the mother makes which statement?
(a) “I should clean her mouth each feeding.”
(b) “I should feed her in an upright position.”
(c) “I need to remember to burp her often.”
(d) “I may need to use a special nipple for feeding.”
Answer:
(a) “I should clean her mouth each feeding.”
Explanation:
It is not necessary to clean the mouth of an infant with an unrepaired cleft palate after each feeding. The neonate needs to be fed in an upright position to prevent aspiration. The neonate with a cleft lip and palate commonly swallows large amounts of air during feeding.
Therefore, the neonate needs to be burped frequently to help eliminate the air and decrease the risk for regurgitation. The neonate with a cleft lip and palate should be fed with a special soft nipple that fills the cleft and facilitates sucking.
Question 100.
A male neonate born at 36 weeks' gestation is admitted to the neonatal intensive care nursery with a diagnosis of probable fetal alcohol syndrome (FAS). The mother visits the nursery soon after the neonate is admitted. Which instructions should the nurse expect to include when developing the teaching plan for the mother about FAS?
(a) Withdrawal symptoms usually do not occur until 7 days postpartum.
(b) Large-for-gestational-age size is common with this condition.
(c) Facial deformities associated with FAS can be corrected by plastic surgery.
(d) Symptoms of withdrawal include tremors, sleeplessness, and seizures.
Answer:
(d) Symptoms of withdrawal include tremors, sleeplessness, and seizures.
Explanation:
The long-term prognosis for neonates with FAS is poor. Symptoms of withdrawal include tremors, sleeplessness, seizures, abdominal distention, hyperactivity, and inconsolable crying. Symptoms of withdrawal commonly occur within 6 to 12 hours or, at the latest, within the first 3 days of life.
The neonate with FAS is usually growth deficient at birth. Most neonates with FAS are mildly to severely mentally handicapped. The facial deformities, such as short palpebral fissures, epicanthal folds, broad nasal bridge, flattened midface, and short, upturned nose, are not easily corrected with plastic surgery.
Question 101.
Which characteristic should the nurse teach the mother about her neonate diagnosed with fetal alcohol syndrome (FAS)?
(a) Neonates are commonly lethargic.
(b) The IQ scores are usually average.
(c) Neurologic disorders are common.
(d) The mortality rate is 70% unless treated.
Answer:
(c) Neurologic disorders are common.
Explanation:
Neurologic disorders are common in neo¬nates with FAS. Speech and language disorders and hyperactivity are common manifestations of central nervous system dysfunction. Mild-to-severe mental retardation and feeding problems also are common. Delayed growth and development is expected.
These neonates feed poorly and commonly have persistent vomiting until age 6 to 7 months. These neonates do not have a 70% mortality rate, and there is no treatment for FAS, but early intervention improves client outcomes.
Question 102.
A newborn is diagnosed with fetal alcohol syndrome. The nurse is teaching this mother what to expect when she goes home with her baby. The nurse determines the mother needs further instruction when she makes which statement?
(a) “The way my baby’s face looks now will stay that way. ”
(b) “My baby may be irritable as a newborn.”
(c) “I may need some help coping with my newborn.”
(d) “My baby will be fine soon after we are home.”
Answer:
(d) “My baby will be fine soon after we are home.”
Explanation:
Changes seen in the facial features of newborns with fetal alcohol syndrome remain that way. These include epicanthal folds, whorls, irregular hair, cleft lip or palate, small teeth, and lack of philtrum. Newborns with fetal alcohol syndrome are usually difficult to calm and frequently cry for long periods of time.
Parents do need assistance with caring for themselves and their infants, particularly with continued alcohol use. A supportive family or support systems are essential. The problems seen with this newborn do not go away and remain with the infant throughout life and are compounded when the child begins to develop mentally.
Question 103.
The father of a neonate diagnosed with gas-troschisis tells the nurse that his wife had planned on breastfeeding the neonate. Which information should the nurse include in the preoperative teaching plan about feeding the neonate?
(a) The neonate will remain on nothing-by mouth (NPO) status until after surgery.
(b) An iron-fortified formula will be given before surgery.
(c) The neonate will need total parenteral nutrition for nourishment.
(d) The mother may breastfeed the neonate before surgery.
Answer:
(a) The neonate will remain on nothing-by mouth (NPO) status until after surgery.
Explanation:
The parents need to know that the neonate will be kept on NPO status and will receive intravenous therapy before surgery. After surgery, feeding will depend on the neonate’s condition. Total parenteral nutrition may be prescribed after surgery, but not before. Breastfeeding may be started after surgery if the neonate’s condition is stable. The mother can pump the breasts until that time.
Question 104.
The nurse is developing a plan of care for a neonate who is to undergo gastroschisis surgery. What should be included? Select all that apply.
(a) prevention of hypothermia
(b) maintenance of fluid and electrolyte balance
(c) controlling preoperative pain
(d) prevention of infection
(e) providing developmental care
Answer:
(a) prevention of hypothermia
(b) maintenance of fluid and electrolyte balance
(d) prevention of infection
Explanation:
(a), (b), (d) The major goals for the neonate include preventing hypothermia, maintaining fluid and electrolyte balance, and preventing infection. Pain medication will be needed after surgery but is not typically needed before the procedure. In many cases, surgery is done very soon after birth, so while developmen¬tal care is important, it should be addressed after the closure of the abdominal wall defect.
Question 105.
While caring for a male neonate diagnosed with gastroschisis, the nurse observes that the parents seem hesitant to touch the neonate because of his appearance. The nurse determines that the parents are most likely experiencing which stage of grief?
(a) denial
(b) shock
(c) bargaining
(d) anger
Answer:
(b) shock
Explanation:
After a neonate is diagnosed with a birth defect, parents often go through stages of grief similar to those they would have if they had lost the child. The physical appearance of the anomaly and the life-threatening nature of the disorder may result in shock to the parents. The parents may hesitate to form a bond with the neonate because of the guarded prognosis.
Denial would be evidenced if the parents acted as if nothing were wrong. Bargaining would be evidenced by parental statements involving “if-then” phrasing, such as, “If the surgery is successful, I will go to church every Sunday.” Anger would be evidenced if the parents attempted to blame someone, such as health care personnel, for the neonate’s condition.
Question 106.
The nurse is caring for a neonate at 38 weeks’ gestation when the nurse observes marked peristaltic waves on the neonate’s abdomen. After this observation, the neonate exhibits projectile vomiting. The nurse notifies the health care provider (HCP) because these signs are indicative of which problem?
(a) esophageal atresia
(b) pyloric stenosis
(c) diaphragmatic hernia
(d) hiatal hernia
Answer:
(b) pyloric stenosis
Explanation:
Marked visible peristaltic waves in the abdomen and projectile vomiting are signs of pyloric stenosis. If the condition progresses without surgical intervention, the neonate will become dehydrated and develop metabolic alkalosis. Signs of esophageal atresia include coughing and regurgitation with feedings.
Diaphragmatic hernia, a life-threatening event in which the abdominal contents herniate into the thoracic cavity, may be evidenced by breath sounds being heard over the abdomen and significant respiratory distress with cyanosis. Signs of hiatal hernia include vomiting, failure to thrive, and short periods of apnea.
Question 107.
The nurse is caring for a term neonate who is diagnosed with patent ductus arteriosus. While performing a physical assessment of the neonate, the nurse anticipates that the neonate will exhibit which signs?
(a) decreased cardiac output with faint peripheral pulses
(b) profound cyanosis over most of the body
(c) loud cardiac murmur through systole and diastole
(d) harsh systolic murmur with a palpable thrill
Answer:
(c) loud cardiac murmur through systole and diastole
Explanation:
With a patent ductus arteriosus, a cardiac defect marked by a failure of the patent ductus arteriosus to close completely at birth, blood from the aorta flows into the pulmonary arteries to be reoxygenated in the lungs and returned to the left atrium and ventricle. The effect of this altered circulation includes increased workload on the left side of the heart and increased pulmonary vascular congestion. Term infants are commonly asymptomatic, but a loud, machinery-like murmur may be heard throughout systole and diastole.
This murmur may be accompanied by a suprasternal thrill, and the heart may be enlarged. Decreased cardiac output with faint peripheral pulses, poor peripheral perfusion, feeding difficulties, and severe congestive heart failure are symptoms associated with severe aortic stenosis. With this defect, the aortic valve is thickened and rigid, leading to decreased cardiac output and reduced myocardial blood flow.
Profound cyanosis over most of the body, fatigue on exertion, feeding difficulties, and chronic hypoxemia are associated with tetralogy of Fallot. With this defect, malalignment of the ventricular system results in nonrestricted ventral septal defects, pulmonic stenosis, overriding of the aorta, and hypertrophy of the left ventricle. The heart appears boot-shaped. A harsh systolic murmur with a palpable thrill is associated with truncus arteriosus. It is marked by an incomplete division of the great vessel. This is caused by a ventral septal defect. Bounding pulses and a widening pulse pressure may also be present.
Question 108.
Assessment of a term neonate at 8 hours after birth reveals tachypnea, diminished femoral pulses, and poor lower body perfusion. The nurse notifies the health care provider (HCP) based on the interpretation that these symptoms are associated with which complication?
(a) coarctation of the aorta
(b) atrioventricular septal defect
(c) pulmonary atresia
(d) transposition of the great arteries
Answer:
(c) pulmonary atresia
Explanation:
Coarctation of the aorta accounts for 5% to 7% of congenital heart disease. There is localized constriction of the aorta, at or near the insertion site of the ductus arteriosus, that increases afterload and decreases cardiac output. The infant with coarctation of the aorta presents with symptoms of poor lower body perfusion, weak lower extremity pulses, and congestive heart failure, including respiratory distress.
The child with a partial atrioventricular septal defect may be asymptomatic at birth. The symptoms in a child with a complete defect depend on the pulmonary artery pressure. The child with pulmonary atresia has profound (complete) cyanosis. Transposition of the great arteries is associated with complete cyanosis during the first few hours of life.
Question 109.
Assessing a neonate at 8 hours of age, the nurse records findings on the medical record below:
|
Time |
1100 |
|
Respiration |
92, no nasal flaring, retractions, grunting |
|
Heat rate |
128, no murmur noted |
|
Temperature |
98.9°F (32.3°C) |
At 1130, the nurse notices the neonate has central cyanosis, and the respiratory rate is now 102 breaths/min; no nasal flaring, no retractions, or grunting was noted, and breath sounds were clear. What should the nurse do?
(a) Change the neonate’s position.
(b) Encourage the baby to cry.
(c) Notify the health care provider.
(d) Suction the nose and mouth.
Answer:
(c) Notify the health care provider.
Explanation:
The neonate is experiencing quiet tachypnea with central cyanosis, which is a sign of possible congenital heart disease, so notifying the HCP is the correct answer. The baby is showing no signs of increased work of breathing, except increased respiratory rate.
Breath sounds are clear; therefore, suctioning is not necessary and may cause further distress due to trauma to the nasal passage. Changing the neonate’s position would have no impact on the cyanosis. Encouraging the baby to cry would increase the distress by decreasing oxygen consumption.
Question 110.
The nurse is performing an admission assessment on a neonate and finds the femoral pulses to be weaker than the brachial and radial pulses. What nursing action should the nurse take next?
(a) Call for a cardiac consult.
(b) Note and tell the health care provider (HCP) when rounds are made.
(c) Place the neonate in reverse Trendelenburg position.
(d) Take the neonate’s blood pressure in all four extremities.
Answer:
(d) Take the neonate’s blood pressure in all four extremities.
Explanation:
The next nursing action in this situation would be to assess the blood pressure in all four extremities and compare the findings. A difference of 15 mm Hg in the systolic blood pressure between the arms and legs is an indication of a narrowed aorta. This could be an emergency, and the HCP ED needs to be notified as soon as the blood pressure data have been collected. Generally, prescribing an LfCP consult is not a nursing function. Placing the neonate in reverse Trendelenburg will only decrease the perfusion to the lower extremities.
Question 111.
A neonate is 4 hours of age. The nursing assessment reveals a heart murmur. What should the nurse do?
(a) Call the health care provider immediately.
(b) Continue routine care.
(c) Feed the neonate.
(d) Further assess for signs of distress.
Answer:
(d) Further assess for signs of distress.
Explanation:
Further assessment for signs of distress is necessary. At 4 hours of age, a transient murmur may be heard as the fetal shunts are closing. This is a normal finding. If no other distress is noted, the HCP m does not need to be called. Result can be noted on the medical record ED- Further assessment is needed to know if continuing routine care and feeding are appropriate and safe for the neonate.
Question 112.
During change of shift report, it was reported that a neonate was experiencing subcostal retractions. Identify where the nurse would expect to see the retractions.
imm
Answer:
imm
Explanation:
Subcostal retractions are noted under the rib cage. Intercostal retractions are noted between the ribs. Suprasternal retractions are found above the sternum, and the substernal retractions are found below the sternum.
Question 113.
A woman has just given birth to a stillborn baby at 39 weeks’ gestation. What is the most appropriate response to the mother the nurse would make at this time?
(a) “I understand how you must feel.”
(b) “I am sorry for your loss.”
(c) “Time heals all wounds.”
(d) “You can have another baby.”
Answer:
(b) “I am sorry for your loss.”
Explanation:
Parents who have experienced perinatal loss have described statements such as “I am sorry for your loss” as helpful. All other statements are not helpful. A nurse can empathize, but may not know what clients are feeling unless they have been given an opportunity to express their emotions. Stating that time heals is a cliche. Suggesting the client can have another child makes a false assumption that one child can replace another. Also, the client may not have the ability to have another child.
Question 114.
During a shift handoff, the nurse receives the following information: “The infant was born at 38 weeks’ gestation to a gravida 1, para 1, 26-year-old mother by spontaneous vaginal birth. Mother is breast¬feeding her infant.” What additional information does the nurse need to make an accurate assessment?
(a) age of infant in hours
(b) length of labor
(c) mother’s marital status
(d) mother’s nutritional status
Answer:
(a) age of infant in hours
Explanation:
Many of the circulatory transitions that infants make after birth are normal for a period of time and become abnormal as the infant ages. The closing of the fetal shunts is an example. Pathology of hyperbilirubinemia is determined by when jaundice appears and acceptable levels are age dependent. The length of labor, the mother’s marital status, and the mother’s nutritional status have no influence on the assessment of the infant.
Question 115.
The nurse has received a shift report on a group of newborns. The nurse should make rounds on which client first?
(a) a newborn who is large for gestational age (LGA) and who needs a repeat blood glucose prior to the next feeding in 15 minutes
(b) a neonate born at 36 weeks’ gestation weighing 5 lb (2,270 g) who is due to breastfeed for the first time in 15 minutes
(c) a neonate who was born 24 hours ago by cesarean birth and had a respiratory rate of 62 breaths/min 30 minutes ago
(d) a newborn who had a borderline low temperature and was double-wrapped with a hat 30 minutes ago to bring up the temperature
Answer:
(c) a neonate who was born 24 hours ago by cesarean birth and had a respiratory rate of 62 breaths/min 30 minutes ago
Explanation:
The nurse should make rounds and first assess the neonate with the respiratory rate of 62 breaths/min. The respiratory rate is out of the normal range and needs reevaluation. The nurse should next assess the newborn with a borderline low temperature to determine if the newborn’s body temperature is increasing. The newborn who is LGA still has 15 minutes before being due for the feeding, and much can be accomplished by the nurse in that time. A 36-week newborn weighing 5 lb (2,270 g) will need to be fed on time to maintain the blood glucose level.
Question 116.
The nurse is caring for a 2-hour-old, full-term, breastfeeding newborn. The nurse notes the following assessments: apical pulse, 122 bpm; axilla temperature, 96.6°F (35.9°C); jitteriness.
Based on this assessment, what should the nurse do first?
(a) Assist the newborn to breastfeed.
(b) Notify the health care provider (HCP).
(c) Obtain a blood glucose sample.
(d) Place the newborn under a radiant heater.
Answer:
(c) Obtain a blood glucose sample.
Explanation:
A temperature of 96.6°F (35.9°C) and jitteriness are signs of hypoglycemia in the new born. The nurse must first obtain a heel stick blood sample for blood glucose. Breastfeeding, preferably skin-to-skin, should be initiated immediately fol-lowing the heel stick puncture to treat the suspected hypoglycemia. The HCP Q can be notified once the blood glucose value is known and the baby is successfully breastfeeding. Normal newborn temperature ranges from 97.7°F (36.5°C) to 99.1°F (37.3°C).
A temperature of 96.6°F (35.9°C) is low, another sign of hypoglycemia; however, breastfeeding takes precedence over the radiant heater. Also, breast¬feeding via skin-to-skin contact has been found as the most effective way to maintain a newborn’s temperature.
Question 117.
The nurse is assigned to care for four mothers and their term newborns. Which mother and newborn couplet requires the nurse’s attention first?
(a) Mother: fundus is firm 2 cm below umbilicus, minimal lochia rubra. Infant: color is pink on room air, respirations 67 breaths/min; bilateral crackles on auscultation.
(b) Mother: fundus is firm 3 cm above umbilicus and to the right, moderate rubra lochia. Infant: color is pink when active, currently dusky while quiet, respirations 70 breaths/min.
(c) Mother: fundus is firm 1 cm above umbilicus, small amount lochia rubra. Infant: color is pink with acrocyanosis, respirations 68 breaths/min and intermittent expiratory grunting.
(d) Mother: fundus is firm at umbilicus, small amount lochia rubra. Infant: pale pink, quiet alert; respirations 65 breaths/min; periodic breathing noted.
Answer:
(b) Mother: fundus is firm 3 cm above umbilicus and to the right, moderate rubra lochia. Infant: color is pink when active, currently dusky while quiet, respirations 70 breaths/min.
Explanation:
The mother demonstrates signs of full bladder and vaginal bleeding and requires assis¬tance with bladder emptying and uterine massage to assess the origination of the bleeding. The newborn requires further assessment because turning dusky when quiet and respiration rate of 70 breaths/min indicate the beginning signs of respiratory distress and requires prompt intervention. All other mothers are recovering normally. While bilateral crackles in a newborn could indicate excessive fluid, a pink color indicates the infant is maintaining oxygenation.
Normal respiration is 30 to 60 breaths/min. While a respiratory rate of 67 breaths/min is slightly elevated, the baby is not demonstrating any other signs of respiratory distress. The newborn with acrocyanosis (bluish hands and feet) is a normal newborn finding and shows the ability to maintain oxygenation. Respirations of 70 breaths/min and intermittent expiratory grunting would indicate close observation but does not require immediate intervention if the infant is pink. The last newborn is maintaining oxygenation, with respirations just slightly above normal. Periodic breathing, featuring pauses in breathing of < 15 seconds, is a normal newborn finding.
Question 118.
The nurse in a postpartum couplet room is making rounds prior to ending the shift. Which findings indicate that the safety needs of the clients have been met? Select all that apply.
(a) infant lying on abdomen
(b) security tags in place
(c) identification system on mother and infant
(d) bulb syringe within sight
(e) someone in room able to care for infant
(f) infant in the mother’s arms, both asleep
Answer:
(b) security tags in place
(c) identification system on mother and infant
(d) bulb syringe within sight
(e) someone in room able to care for infant
Explanation:
(b), (c), (d), (e) A hospital-specific security system is the standard of care to prevent neonatal abduction. The bulb syringe should be visible and easily accessible to both the mother and the nurse in case of choking. Someone should remain in the room who is able to safely care for the infant. This may be the mother or a family member if the mother is physically not able to care for the infant.
The infant should be lying on the back or side, rather than the abdomen to prevent sudden infant death syndrome (“back to sleep”). Infant falls from a mother’s bed are a serious safety problem. The infant should be in the mother’s arms or in the crib rather than lying on a bed, even with the side rails up, as an infant can slip through the rails. A sleeping mother is not aware of the status of the infant who can easily fall out of her arms; the infant can be in the mother’s arms only if she is awake.
Question 119.
After receiving change of shift report in the normal newborn nursery, the nurse should see which neonate first?
(a) 3-hour-old neonate with increased respiratory secretions
(b) 6-hour-old neonate with a blood glucose of 25 mg/dL (1.38 mmol/L)
(c) 12-hour-oldneonate with a temperature of 97.4°F (36.4°C)
(d) 24-hour-old neonate with no urine output for the past 12 hours
Answer:
(b) 6-hour-old neonate with a blood glucose of 25 mg/dL (1.38 mmol/L)
Explanation:
The blood glucose of 25 mg/dL (1.38 mmol/L) is the most critical. Glucose is the only fuel that the brain can use. It is important to protect the central nervous system, and levels < 30 mg/dL (1.7 mmol/L) in the first 6 hours of life of a neonate indicate hypoglycemia. Increased respiratory secretions is a normal finding in the second period of reactivity. A temperature of 97.4°F (36.4°C) is only slightly low for a neonate at this age. Ninety-five percent of all neonates will void at least once in the first 24 hours. This is not unusual at this age.
Question 120.
The newborn nurse has just received shift report about a group of newborns and is to receive another admission in 30 minutes. In order to provide the safest care and plan for the new admission, the nurse should do which tasks in order of first to last? All options must be used.
(a) Move quickly from room to room, and assess all clients.
(b) Check the room to which the new client will be admitted to ensure all supplies and equipment are available.
(c) Log on to the clinical information system, and determine if there are new prescriptions.
(d) Review notes from shift report, and prioritize all clients; make rounds on the most critical first if there are new prescriptions.
Answer:
(d) Review notes from shift report, and prioritize all clients; make rounds on the most critical first if there are new prescriptions.
(a) Move quickly from room to room, and assess all clients.
(b) Check the room to which the new client will be admitted to ensure all supplies and equipment are available.
(c) Log on to the clinical information system, and determine if there are new prescriptions.
Explanation:
(d), (a), (c), (b) Based on the report given by the preceding nurse, the nurse should plan to prioritize all clients and first make rounds on the client needing the highest level of nursing care. The nurse can then make rounds on all other clients. The nurse can then check for new prescriptions and, finally, inspect the room in which the next client will be admitted to be sure all of the equipment is available.
Question 121.
The charge nurse in the newborn nursery and an unlicensed assistive personnel (UAP) are working together on a shift. Under their care are eight babies rooming in with their mothers, and one infant is in the nursery for the night on tube feedings. There is a new client whose infant will be brought to the nursery in 15 minutes. Which tasks would the nurse assign to the UAP? Select all that apply.
(a) newborn admission
(b) vital signs on all stable infants
(c) tube feeding
(d) document feedings of infants
(e) record voids/stools
(f) bath and initial feeding for new admission
Answer:
(b) vital signs on all stable infants
(d) document feedings of infants
(e) record voids/stools
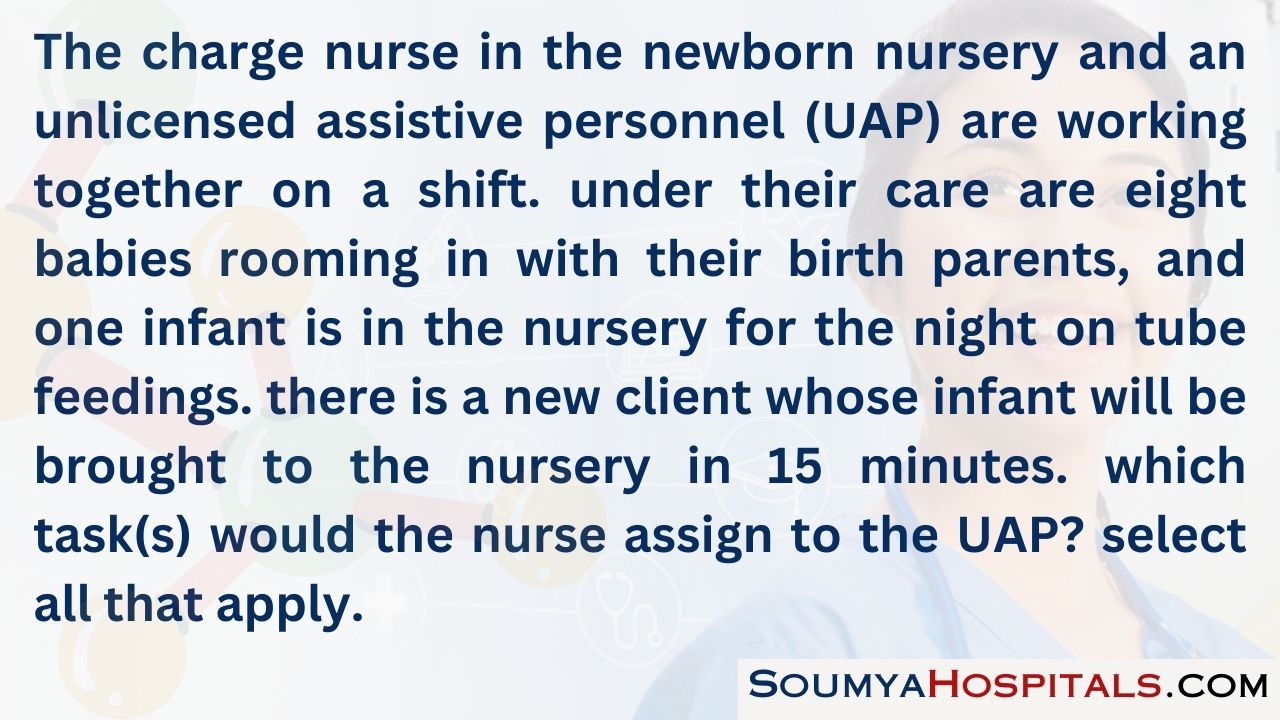
Explanation:
(b), (d), (e) The role of the UAP El allows this member of the health care team to take vital signs on clients, and record feedings, and voids and stools of infants according to hospital guidelines. The newborn assessment is completed by a licensed care provider as is the tube feeding. Bathing of the newborn is within the scope of practice for the UAP, but the initial assessment of patency of the gastrointestinal tract, which is initiated by the first feeding, is within the scope of licensed care providers. If there is a trachea esophageal fistula, this is the time when it may become evident.
Read More: