The variety of NCLEX Questions available allows students to cover a wide range of topics and increase their knowledge base.
NCLEX-RN Practice Test 5 with Rationale
Question 1.
The nurse at a college campus is preparing to medicate several students who have been exposed to meningococcal meningitis. Which would the nurse most likely administer?
(a) Ampicillin (Omnipen)
(b) Ciprofoxacin (Cipro)
(c) Vancomycin (Vancocin)
(d) Piperacillin/Tazobactam (Zosyn)
Answer:
(b) Ciprofoxacin (Cipro)
Rationale:
Answer (b) is correct. The nurse would be prepared to administer Cipro in combination with rifampin (Rifadin) for all others exposed or in contact with a patient who had meningococcal meningitis. Answers (a), (c), and (d) medications are given to the patient with Meningococcal meningitis.
Question 2.
A 65-year-old client is admitted after a stroke. Which nursing intervention would best improve tissue perfusion to prevent skin problems'?
(a) Assessing the skin daily for breakdown
(b) Massaging any erythematous areas on the skin
(c) Changing incontinence pads as soon as they become soiled with urine or feces
(d) Performing range-of-motion exercises and turning and repositioning the client
Answer:
(d) Performing range-of-motion exercises and turning and repositioning the client
Rationale:
Answer 0 is correct. Activity, exercise, and repositioning the client will increase circulation and improve tissue perfusion. Answer (a) will help to identify problem areas but will not improve the perfusion of the tissue. Answer (b) should be avoided because it could increase the damage if trauma was present. Answer (c) should be done to prevent irritation of the skin, but this action does not improve perfusion.
Question 3.
Which diet selection by a client with a decubitus ulcer would indicate a clear understanding of the proper diet for healing of the ulcer?
(a) Tossed salad, milk, and a slice of caramel cake
(b) Vegetable soup and crackers, and a glass of iced tea
(c) Baked chicken breast, broccoli, wheat roll, and an orange
(d) Hamburger, French fries, and corn on the cob
Answer:
(c) Baked chicken breast, broccoli, wheat roll, and an orange
Rationale:
Answer (c) is correct. This client needs a balanced nutritional diet with protein and vitamin C. Answers (a) and (b) both lack protein, which is very important in maintaining a positive nitrogen balance. Answer (d) has protein but is lacking in vitamin C.
Question 4.
The nurse is assessing elderly clients at a community center. Which of the following findings would be the most cause for concern?
(a) Dry mouth
(b) Loss of one inch of height in the last year
(c) Stiffened joints
(d) Rales bilaterally on chest auscultation
Answer:
(d) Rales bilaterally on chest auscultation
Rationale:
Answer (d) is correct. Rales would indicate lung congestion and the need for follow-up. Answers (a), (b), and (c) are all normal health-related changes associated with aging.
Question 5.
A client with chronic pain is being treated with opioid administration via epidural route. Which medication would it be most important to have available due to a possible complication of this pain relief procedure?
(a) Ketorolac (Toradol)
(b) Naloxone (Narcan)
(c) Diphenhydramine (Benadryl)
(d) Promethazine (Phenergan)
Answer:
(b) Loss of one inch of height in the last year
Rationale:
Answer (b) is correct. Respiratory depression can occur from the administration of opioids. Naloxone should be available as an antagonist for these drugs. Answers (a), (c), and (d) might also be needed, but the most important problem that could occur would be the respiratory depression. These clients might also develop itching and nausea, and would likely use Benadryl and Phenergan, respectively, for treatment. Toradol is classified as an NSAID and is useful for its anti-inflammatory properties.
Question 6.
The nurse is assessing a client for hypovolemia. Which laboratory result would help the nurse in confirming a volume deficit?
(a) Hematocrit 55%" '
(b) Potassium 5.0mEq/L
(c) Urine specific gravity 1.016
(d) BUN 18mg/dL
Answer:
(a) Hematocrit 55%" '
Rationale:
Answer A is correct. Hematocrit levels are elevated with hypovolemia. Answers (b), (c), and (d) are all normal levels. Potassium (normal 3.5-5.3mEq/L) levels can be either increased or decreased with hypovolemia; BUN (normal 5-20mg/dL) and specific gravity (1.016-1.022) levels would be elevated with hypovolemia.
Question 7.
A nurse is triaging in the emergency room when a client enters complaining of muscle cramps and a feeling of exhaustion after a running competition. Which of the following would the nurse sus-pect?
(a) Hypernatremia
(b) Hyponatremia
(c) Hyperkalemia
(d) Hypokalemia
Answer:
(b) Hyponatremia
Rationale:
Answer (b) is correct. Athletes can sometimes consume large amounts of water when competing. This can lead to decreased sodium levels. Symptoms of hyponatremia include an altered mental status, anorexia, muscle cramps, and exhaustion. Answers (a), (c), and (d) do not correlate with the history or the symptoms given.
Question 8.
A client was transferred to the hospital unit as a direct admit from a small community hospital. While the nurse is obtaining part of the admission history information, the client suddenly becomes semiconscious. Assessment reveals a systolic BP of 70, heart rate of 130, and respiratory rate of 24. What is the nurse’s initial action?
(a) Lower the head of the client’s bed.
(b) Initiate an IV with a large bore needle.
(c) Notify the physician of the assessment results.
(d) Call for the cardiopulmonary resuscitation team.
Answer:
(a) Lower the head of the client’s bed.
Rationale:
Answer (a) is correct. If the nurse suspects a leaking or a ruptured abdominal aortic aneurysm, the first action is to improve blood flow to the brain and elevate the blood pressure. This can be accomplished quickly with the change in position. Answers (b) and (c) would be appropriate, but not before answer (a). Answer (d) would not be required at this time.
Question 9.
The nurse is caring for a client post-myocardial infarction on the cardiac unit. The client is exhibiting symptoms of shock. Which clinical manifestation is the best indicator that the shock is cardiogenic rather than anaphylactic?
(a) BP 90/60
(b) Chest pain
(c) Increased anxiety
(d) Temp 98.6°F
Answer:
(b) Chest pain
Rationale:
Answer (b) is correct. Clients with cardiogenic shock often have chest pain. This symptom is not related to anaphylactic shock. Answers (a) and (c) can occur with both types of shock, but are not specific to the cardiogenic type. Answer (d) is a normal temperature reading.
Question 10.
While reading the progress notes on a client with cancer, the nurse notes a TNM classification of T1, N1, MO. What does this classification indicate?
(a) The tumor is in situ, no regional lymph nodes are involved, and there is no metastasis.
(b) No evidence of primary tumor exists, lymph nodes can't be assessed, and metastasis can’t be assessed
(c) The tumor is extended, with regional lymph node involvement and distant metastasis.
(d) The tumor is extended and regional lymph nodes are involved, but there is no metastasis.
Answer:
(d) The tumor is extended and regional lymph nodes are involved, but there is no metastasis.
Rationale:
Answer (d) is correct. This is the correct classification for the primary tumor of T1, N1, and MO. The letter T denotes the extent of the primary tumor, N indicates the absence or presence and extent of regional lymph nodes, and M denotes the absence or presence of distant metastasis. Answer (a) is correct for T1, NO, and MO. Answer (b) is correct for the classification of TX, NX, MX. Answer (c) is the correct classification for T1, N1, M1.
Question 11.
The nurse is caring for a client with leukemia who has received the drug Daunorubicin (Cerubidine). Which of the following common side effects would cause the most concern?
(a) Nausea
(b) Vomiting
(c) Cardiotoxicity
(d) Alopecia
Answer:
(c) Cardiotoxicity
Rationale:
Answer (c) is correct. (d) aunorubicin can damage the heart muscle and is the most serious of the ones listed. It can also cause bone marrow suppression. Answers (a), (b), and (d) are all common, but not as life-threatening as answer (c).
Question 12.
The nurse is caring for an organ donor client with a severe head injury from an MVA. Which of the following is most important when caring for the organ donor client?
(a) Maintenance of the BP at 90mmHg or greater
(b) Maintenance of a normal temperature
(c) Keeping the hematocrit at less than 28%
(d) Ensuring a urinary output of at least 300ml7hr
Answer:
(a) Maintenance of the BP at 90mmHg or greater
Rationale:
Answer (a) is correct. The organ donor must have a BP of 90 or greater to ensure tissue perfusion. Answers (b), (c), and (d) are not related to adequate tissue maintenance for an organ donation.
Question 13.
A client is being admitted with syndrome of inappropriate diuretic hormone. Which does the nurse expect to observe? Select ail that apply.
(a) Increased thirst
(b) Tachycardia
(c) Polyuria
(d) Hostility
(e) Muscle weakness
Answer:
(b) Tachycardia
(d) Hostility
(e) Muscle weakness
Rationale:
Answers (b), (d), and (e) are correct. These clients will have loss of thirst and decreased urinary output making choices (a) and (c) incorrect. The client may also exhibit irritability in addition to the answers given.
Question 14.
A client with a fractured leg is exhibiting shortness of breath, pain upon deep breathing, and hemoptysis. What do these clinical manifestations indicate to the nurse?
(a) Congestive heart failure
(b) Pulmonary embolus
(c) Adult respiratory distress syndrome
(d) Tension pneumothorax
Answer:
(b) Pulmonary embolus
Rationale:
Answer (b) is correct. Hemoptysis is a hallmark symptom of a pulmonary embolus, and this client’s fracture history and other clinical manifestations lead to this conclusion. The clinical manifestations do not correlate with the diagnoses in answers (a), (c), and (d).
Question 15.
A nurse is preparing to mix and administer chemotherapy. What equipment would be unnecessary to obtain?
(a) Surgical gloves
(b) Luer iok fitting IV tubing
(c) Surgical hat cover
(d) Disposable long-sleeve gown
Answer:
(c) Surgical hat cover
Rationale:
Answer (c) is correct. A surgical hat cover is not necessary to mix or administer chemotherapy. OSHA (Occupational Safety and Health Administration) and ONS (Oncology Nurse Society) recommend answers (a), (b), and (d) when mixing or administering chemotherapy. The nurse should dispose of all equipment used in chemotherapy preparation and administration as hazardous waste in leak-proof, puncture-proof containers.
Question 16.
The charge nurse is assigning staff for the day. Staff consists of an RM, an LPN, and a certified nursing assistant. Which client assignment should be given to the nursing assistant?
(a) Exploratory laparotomy with a colon resection the previous shift
(b) Client with a stroke who has been hospitalized for two days
(c) A client with metastatic cancer on PCA morphine
(d) A new admission with diverticulitis
Answer:
(b) Client with a stroke who has been hospitalized for two days
Rationale:
Answer (b) is correct. The client who had a stroke is the most stable client of the ones listed. The client in answer A needs extensive assessment. The client in answer (c) has a patient-controlled analgesic (PCA) pump and requires an RN because of the intravenous infusion. The client in answer (d) is a new admission with an infected diverticulum and would be less stable, with more unknowns.
Question 17.
The registered nurse is making shift assignments. Which client should be assigned to the licensed practical nurse (LPN)?
(a) A client who is a diabetic with a foot ulcer
(b) A client with a deep vein thrombosis receiving intra venous heparin
(c) A client being weaned from a tracheostomy
(d) A post-operative cholecystectomy with a T-tube
Answer:
(a) A client who is a diabetic with a foot ulcer
Rationale:
Answer (a) is correct. The diabetic with the foot ulcer is the most stable client and should be assigned to the LPN. Answer (b) requires assessments for clotting and bleeding complications, as well as monitoring of the IV heparin. Weaning from a tracheostomy could constitute an airway problem, making answer (c) incorrect. A postoperative client would be less stable and require more extensive care, so answer (d) is incorrect.
Question 18.
A client with metastatic cancer of the lung has just been told the prognosis by the oncologist. The nurse hears the client state, “I don’t believe the doctor; I think he has me confused with another patient.” This is an example of which of Kubler-Ross’ stages of dying?
(a) Denial
(b) Anger
(c) Depression
(d) Bargaining
Answer:
(a) Denial
Rationale:
Answer (a) is correct. Kubler-Ross identified five stages of dying as ways that people cope with death. The stage of denial can be used as a buffer and a way to adapt. When dealing with these clients, the nurse would need to use open-ended statements, such as, “Tell me more.” Other examples of statements made by the client in this stage are “This can’t be true” and “I want another opinion.” Answers (b), (c), and (d) are a few of the other stages of dying. In order, the stages are denial, anger, bargaining, depression, and acceptance.
Question 19.
The surgical nurse is preparing a patient for surgery on the lower abdomen. In which position would the nurse most likely place the client for surgery on this area?
(a) Lithotomy
(b) Sim’s
(c) Prone
(d) Trendelenburg
Answer:
(d) Trendelenburg
Rationale:
Answer (d) is correct. The Trendelenburg position is used for surgeries on the lower abdomen and pelvis. This position helps to displace intestines into the upper abdomen and out of the surgical area. Answer (a) is reserved for vaginal, perineal, and some rectal surgeries. Answer (b) is used for renal surgery, and answer (c) is used for back surgery and some rectal surgeries.
Question 20.
The nurse is performing a history on a client admitted for surgery in the morning. Which long-term medication in the client’s history would be most important to report to the physician?
(a) Prednisone-
(b) Lisinopril (Zestril)
(c) Docusate (Colace)
(d) Oscal D
Answer:
(a) Prednisone-
Rationale:
Answer (a) is correct. Abrupt withdrawal of steroids can lead to collapse of the cardiovascular system; therefore, the physician should be notified for drug coverage. The medications in answers (b), (c), and (d) would not be as important as the maintenance of the steroids. Answer (b) is an ace inhibitor used as an antihypertensive. Answer (c) is a stool softener, and answer (d) is a calcium and vitamin agent.
Question 21.
A nurse is working in an endoscopy recovery area. Many of the clients are administered midazolam (Versed) to provide conscious sedation. Which medication is important to have available as an antidote for Versed?
(a) Diazepam (Valium)
(b) Naloxone (Narcan)
(c) Flumazenil (Romazicon)
(d) Florinef (Fludrocortisone)
Answer:
(c) Flumazenil (Romazicon)
Rationale:
Answer (c) is correct. Versed is used for conscious sedation and is an antianxiety agent. The antidote for this drug is Romazicon, a benzodiazepine. Answers (a), (b), and (d) are not utilized as antagonists for Versed; however, answer (b) is the antagonist for narcotics.
Question 22.
The nurse is caring for a client with a cerebrovascular accident (CVA) who is complaining of being nauseated and is requesting an Detailed emesis basin. Which action would the nurse take first?
(a) Administer an ordered antiemetic.
(b) Obtain an ice bag and apply to the client’s throat.
(c) Turn the client to one side.
(d) Notify the physician.
Answer:
(c) Turn the client to one side.
Rationale:
Answer (c) is correct. Turning the client to the side will allow any vomit to drain from the mouth and decrease the risk for aspiration. Answers (a), (b), and (d) are all appropriate nursing interventions, but a patent airway and prevention of aspiration are priorities.
Question 23.
The nurse is assessing a client who had a colon resection two days ago. The client states, “I feel like my stitches have burst Detailed loose.” Upon further assessment, dehiscence of the wound is noted. Which action should the nurse take?
(a) Immediately place the client in the prone position.
(b) Apply a sterile, saline-moistened dressing to the wound.
(c) Administer atropine to decrease abdominal secretions.
(d) Wrap the abdomen with an ACE bandage.
Answer:
(b) Apply a sterile, saline-moistened dressing to the wound.
Rationale:
Answer (b) is correct. When dehiscence and/or evisceration of a wound occurs, the nurse should apply a sterile saline dressing before notifying the physician. Answer (a) is not the appropriate position; the client should be placed in low Fowler’s position. Answers (c) and (d) will not help in this situation.
Question 24.
A client with hepatitis C is scheduled for a liver biopsy. Which would the nurse include in the teaching plan for this client? Detailed
(a) The client should lie on the left side after the procedure.
(b) Cleansing enemas should be given the morning of the procedure.
(c) Blood coagulation studies might be done before the biopsy.
(d) The procedure is noninvasive and causes no pain.
Answer:
(c) Blood coagulation studies might be done before the biopsy.
Rationale:
Answer (c) is correct. There is a risk of bleeding with a liver biopsy; therefore, laboratory tests are done to determine any problems with coagulation before the biopsy. Answers (a), (b), and (d) are incorrect statements. The client lies on the right side, not the left; no enemas are given; and the test is invasive and can cause some pain.
Question 25.
The nurse is caring for a client after a laryngectomy. The client is anxious, with a respiratory rate of 32 and an oxygen saturation of 88. What should be the initial nursing action?
(a) Suction the client.
(b) Increase the oxygen flow rate.
(c) Notify the physician.
(d) Recheck the O2 saturation reading
Answer:
(a) Suction the client.
Rationale:
Answer (a) is correct. Obstruction of the tracheostomy can cause anxiety, increased respiratory rate, and an O2 saturation decrease. The nurse should first suction the client. If this doesn’t work, she should notify the physician, as in answer (c). Answer (b) would not help if the tube was obstructed. Answer (d) would be done to assess for improvement after the suctioning was performed.
Question 26.
The nurse is performing discharge teaching to a client who is on isoniazid (INH). Which diet selection by the client indicates to the nurse that further instruction is needed?
(a) Tuna casserole
(b) Ham salad sandwich
(c) Baked potato
(d) Broiled beef roast
Answer:
(a) Tuna casserole
Rationale:
Answer (a) is correct. Clients who are taking INH should avoid tuna, red wine, soy sauce, and yeast extracts because of the side effects that can occur, such as headaches and hypotension. Answers (b), (c), and (d) are all allowed with this drug.
Question 27.
A client with a head injury has an intracranial pressure (ICP) monitor in place. Cerebral perfusion pressure calculations are ordered. If the client’s ICP is 22 and the mean pressure reading is 70, what is the client’s cerebral perfusion pressure?
(a) 92
(b) 72
(c) 58
(d) 48
Answer:
(d) 48
Rationale:
Answer (d) is correct. The cerebral perfusion pressure is obtained by subtracting the ICP from the mean arterial pressure (MAP). A client must have a CPP of 70-100 to have a normal reading and adequate cerebral perfusion. Answers (a), (b), and (c) are all incorrect calculations.
Question 28.
A student nurse is observing a neurological nurse perform an assessment. When the nurse asks the client to “stick out his nerve?
(a) II optic
(b) I olfactory
(c) X vagus
(d) XII hypoglossal
Answer:
(d) XII hypoglossal
Rationale:
Answer (d) is correct. The XII hypoglossal cranial nerve deals with the function of the tongue and its movement. Clients can exhibit weakness and deviation with impairment of this cranial nerve. Answers (a), (b), and (c) are not tested by this procedure. Cranial nerve I is involved with smelling, cranial nerve II is involved with visual function, and cranial nerve X deals with the gag reflex.
Question 29.
Which set of vital signs would best indicate to the nurse that a client has an increase in intracranial pressure?
(a) BP 180/70, pulse 50, respirations 16, temperature 101°F
(b) BP 100/70, pulse 64, respirations 20, temperature 98.6°F
(c) BP 96/70, pulse 132, respirations 20, temperature 98.6°F
(d) BP 130/80, pulse 50, respirations 18, temperature 99.6°F
Answer:
(a) BP 180/70, pulse 50, respirations 16, temperature 101°F
Rationale:
Answer (a) is correct. Increased intracranial pressure vital sign changes include an elevated BP with a widening pulse pressure, decreased heart rate, and temperature elevation. Answer (c) could occur with shock or hypovolemia. Answer (b) does not correlate with increased ICP. Answer (d) is not as evident of increased intracranial pressure as answer (a).
Question 30.
The nurse is assessing the laboratory results of a client scheduled to receive phenytoin sodium (Dilantin). The Dilantin level, drawn two hours ago, is 30mcg/mL. What is the appropriate nursing action?
(a) Administer the Dilantin as scheduled.
(b) Hold the scheduled dose and notify the physician.
(c) Decrease the dosage from 100mg to 50mg.
(d) Increase the dosage to 200mg from 100mg.
Answer:
(b) Hold the scheduled dose and notify the physician.
Rationale:
Answer (b) is correct. The normal Dilantin level is 10-20mcg/mL; a level of 30 exceeds the normal. The appropriate action is to notify the physician for orders. Answer (a) would be inappropriate with a high level, and answers (c) and (d) would require changing the physician's prescription.
Question 31.
A client with sickle cell disease is admitted in active labor. Which nursing intervention would be most helpful in preventing a sickling crisis?
(a) Obtaining blood pressures every two hours
(b) Administering pain medication every three hours as ordered
(c) Monitoring arterial blood gas results
(d) Administering IV fluids at ordered rate of 200mL/hr
Answer:
(d) Administering IV fluids at ordered rate of 200mL/hr
Rationale:
Answer (d) is correct. Hydration is needed to prevent slowing of blood flow and occlusion. It is important to perform assessments in answers (a), (b), and (c), but answer (d) is the best intervention for preventing the crisis.
Question 32.
A client is admitted with a diagnosis of pernicious anemia. Which of the following signs or symptoms would indicate that the client has been noncompliant with ordered B12 injections?
(a) Hyperactivity in the evening hours
(b) Weight gain
(c) Paresthesia of hands and feet
(d) Diarrhea stools
Answer:
(c) Paresthesia of hands and feet
Rationale:
Answer (c) is correct. B12 is an essential component for proper functioning of the peripheral nervous system. Clients who have a B12 deficit will have symptoms such as paresthesia. Answers (a) and (d) do not occur with pernicious anemia; the client in answer (b) would have weight loss rather than weight gain.
Question 33.
The nurse has performed nutritional teaching on a client with gout who is placed on a low-purine diet. Which selection by the client would indicate that teaching has been ineffective?
(a) Boiled cabbage
(b) Apple
(c) Peach cobbler
(d) Spinach
Answer:
(d) Spinach
Rationale:
Answer (d) is correct. Spinach should be avoided on a low-purine diet; other foods to avoid include poultry, liver, lobster, oysters, peas, fish, and oatmeal. Answers (a), (b), and (c) are all foods included on a low-purine diet.
Question 34.
The nurse is caring for a 70-year-old client with hypovolemia who is receiving a blood transfusion. Assessment findings reveal crackles on chest auscultation and distended neck veins. What is the nurse’s initial action?
(a) Slow the transfusion.
(b) Document the finding as the only action.
(c) Stop the blood transfusion and turn on the normal saline.
(d) Assess the client’s pupils.
Answer:
(a) Slow the transfusion.
Rationale:
Answer (a) is correct. The client is exhibiting symptoms of fluid volume excess; slowing the rate is the proper action. The nurse would not stop the infusion of blood, as in answer (c), and answers (b) and (d) would not help.
Question 35.
The orthopedic nurse should be particularly alert for a fat embolus in which of the following clients having the greatest risk for this complication after a fracture?
(a) A 50-year-old with a fractured fibula
(b) A 20-year-old female with a wrist fracture
(c) A 21-year-old male with a fractured femur
(d) An 8-year-old with a fractured arm
Answer:
(c) A 21-year-old male with a fractured femur
Rationale:
Answer (c) is correct. Fat emboli occur more frequently with long bone or pelvic fractures and usually in young adults ages 20-30. Answers (a), (b), and (d) are not high-risk groups for this complication.
Question 36.
The nurse has performed discharge teaching to a client in need of a high-iron diet. The nurse recognizes that teaching has been effective when the client selects which meal plan?
(a) Hamburger, French fries, and orange juice
(b) Sliced veal, spinach salad, and whole-wheat roll
(c) Vegetable lasagna, Caesar salad, and toast
(d) Bacon, lettuce, and tomato sandwich; potato chips; and tea
Answer:
(b) Sliced veal, spinach salad, and whole-wheat roll
Rationale:
Answer (b) is correct. Sliced veal, a spinach salad, and a whole-wheat roll is the selection with the highest iron content. Other foods high in iron include cream of wheat, oatmeal, liver, collard greens, mustard greens, clams, chili with beans, brown rice, and dried apricots. Answers (a), (c), and (d) are not high in iron.
Question 37.
An elderly female is admitted with a fractured right femoral neck. Which clinical manifestation would the nurse expect to find?
(a) Free movement of the right leg
(b) Abduction of the right leg
(c) Internal rotation of the right hip
(d) Shortening of the right leg
Answer:
(d) Shortening of the right leg
Rationale:
Answer (d) is correct. Symptoms of a fractured femoral neck include shortening, adduction, and external rotation of the affected limb. Answer (a) is incorrect because the patient usually is unable to move the leg because of pain. Answers (b) and (c) are incorrect because the leg would be adducted and externally rotated if a fracture was present.
Question 38.
The nurse is performing the skill of intramuscular injection by the Z track method. Which technique would the nurse utilize to prevent tracking of the medication?
(a) Inject the medication in the deltoid muscle.
(b) Use a 22-gauge needle when preparing the syringe.
(c) Omit aspirating for blood before injecting.
(d) Draw up 0.2mL of air after the proper medication dose.
Answer:
(d) Draw up 0.2mL of air after the proper medication dose.
Rationale:
Answer (d) is correct. The 0.2mL of air that would be administered after the medication with an intramuscular injection would allow the medication to be dispersed into the muscle. In answer (a), the muscle is too small. Answer (c) is an incorrect procedure, and answer (b) does not help prevent tracking.
Question 39.
A client with asthma has an order to begin an aminophylline IV infusion. Which piece of equipment is essential for the nurse to safely administer the medication?
(a) Large bore intravenous catheter
(b) IV inline filter
(c) IV infusion device
(d) Cover to prevent exposure of solution to light
Answer:
(c) IV infusion device
Rationale:
Answer (c) is correct. Aminophylline must be regulated by an infusion device to prevent improper infusion rates. Answers (a), (b), and (d) are not necessary for administration of this drug so they are incorrect.
Question 40.
The nurse caring for a client with anemia recognizes which clinical manifestation as the one that is specific for a hemolytic type of
anemia?
(a) Jaundice
(b) Anorexia
(c) Tachycardia
(d) Fatigue
Answer:
(a) Jaundice
Rationale:
Answer (a) is correct. Hemolytic anemia involves the destruction of red blood cells that prompt the release of bilirubin, leading to a yellow hue of the skin. Answers (c) and (d) occur with several types of anemia but are not specific to hemolytic anemia. Answer (b) is not related to anemia.
Question 41.
A client with cancer who is receiving chemotherapeutic drugs has been given injections of pegfilgastrim (Neulasta). Which laboratory value reveals that the drug is producing the desired effect?
(a) Hemoglobin of 13.5g/dL
(b) White blood cells count of 6,000/mm
(c) Platelet count of 300,000/mm
(d) Hematocrit of 39%
Answer:
(b) White blood cells count of 6,000/mm
Rationale:
Answer (b) is correct. Neulasta is given to increase the white blood cell count in patients with leucopenia. This white blood cell count is within the normal range for showing an improvement. Answers (a), (c), and (d) are not specific to the drug’s desired effect.
Question 42.
The nurse is performing discharge teaching on a client with polycythemia vera. Which would be included in the teaching plan?
(a) Avoid large crowds and exposure to people who are ill.
(b) Keep the head of the bed elevated at night.
(c) Wear socks and gloves when going outside.
(d) Recognize clinical manifestations of thrombosis.
Answer:
(d) Recognize clinical manifestations of thrombosis.
Rationale:
Answer (d) is correct. Clients with a diagnosis of polycythemia have an increased risk for thrombosis and must be aware of the symptoms. Answers (a), (b), and (c) are not related to this disorder.
Question 43.
A client is being discharged after lithotripsy for removal of a kidney stone. Which statement by the client indicates understanding of the nurse’s instructions?
(a) “I’ll need to strain my urine starting in the morning.”
(b) “I will need to save all my urine.
(c) “I will be careful to strain all the urine and save the stone.”
(d) “I won’t need to strain my urine now that the procedure is complete.”
Answer:
(c) “I will be careful to strain all the urine and save the stone.”
Rationale:
Answer (c) is correct. The client should strain all urine after the procedure and save any stones for examination. The statements in answers (a), (b), and (d) indicate a misunderstanding of how to provide proper self-care after the lithotripsy procedure.
Question 44.
The nurse is caring for a client with osteoporosis who is being discharged on alendronate (Fosamax). Which statement would indicate a need for further teaching?
(a) “I should take the medication immediately before bedtime every night.”
(b) “I should remain in an upright position for 30 minutes after taking Fosamax.”
(c) “The medication should be taken by mouth with water.”
(d) “I should not have any food with this medication.”
Answer:
(a) “I should take the medication immediately before bedtime every night.”
Rationale:
Answer (a) is correct. The medication should be taken in the morning before food or other medications are ingested, with water as the only liquid. Answers (b), (c), and (d) are correct administrations. Answer (b) is an important choice for preventing esophageal problems with Fosamax administration.
Question 45.
A client is being evaluated for carpel tunnel syndrome. The nurse is observed tapping over the median nerve in the wrist and asking the client if there is pain or tingling. Which assessment is the nurse performing?
(a) Phalen’s maneuver
(b) Tinel’s sign
(c) Kernig’s sign
(d) Brudzinski’s sign
Answer:
(b) Tinel’s sign
Rationale:
Answer (b) is correct. Assessing for Tinel’s sign is done to check for paresthesia in the median nerve. An abnormal result would be pain or tingling as this procedure is done. This test can also be performed by inflating a blood pressure cuff to the client’s systolic pressure, resulting in pain and tingling. Answer (a) is another test in which the nurse asks the client to place the backs of the hands together and flex them at the same time. If the client experiences paresthesia within 60 seconds of performing the test, it is a positive result indicating carpel tunnel syndrome. Answers (c) and (d) are both assessment procedures for meningeal irritation.
Question 46.
The nurse is caring for a client who is recovering from a fractured femur. Which diet selection would be best for this client?
(a) Loaded baked potato, fried chicken, and tea
(b) Dressed cheeseburger, French fries, and a Diet Coke
(c) Tuna fish salad on sourdough bread, potato chips, and skim milk
(d) Mandarin orange salad, broiled chicken, and milk
Answer:
(d) Mandarin orange salad, broiled chicken, and milk
Rationale:
Answer (d) is correct. A diet of mandarin orange salad, broiled chicken, and milk is the most balanced and best selection for promoting healing. Answers (a), (b), and (c) are not as inclusive of the food groups that promote healing.
Question 47.
The nurse working in the emergency department realizes that it would be contraindicated to induce vomiting if someone had ingested which of the following?
(a) Ibuprofen
(b) Aspirin
(c) Vitamins
(d) Gasoline
Answer:
(d) Gasoline
Rationale:
Answer (d) is correct. Vomiting would be contraindicated with an acid, alkaline, or petroleum product. Answers (a), (b), and (c) do not contain any of these solutions, so vomiting would be a possible treatment.
Question 48.
A client with AIDS has impaired nutrition due to diarrhea. The nurse teaches the client about the need to avoid certain foods. Which diet selection by the client would indicate a need for further teaching?
(a) Tossed salad
(b) Baked chicken
(c) Broiled fish
(d) Steamed rice
Answer:
(a) Tossed salad
Rationale:
Answer (a) is correct. Clients with AIDS who are experiencing diarrhea should avoid bowel irritants such as raw vegetables, nuts, and fatty and fried foods. Answers (b), (c), and (d) would not serve as irritants to the bowels.
Question 49.
The nurse has just received a report from the previous shift.
Which of the following clients should the nurse visit first?
(a) A 50-year-old COPD client with a PCO2 of 50
(b) A 24-year-old admitted after an MVA complaining of shortness of breath
(c) A client with cancer requesting pain medication
(d) A one-day post-operative cholecystectomy with a temperature of 100°F
Answer:
(b) A 24-year-old admitted after an MVA complaining of shortness of breath
Rationale:
Answer (b) is correct. The nurse should prioritize these clients and decide to see the client with the shortness of breath because this could be a possible alteration in breathing. The client in answer (a) has an abnormal PCO2 (normal 35-45), but this would be expected in a client with COPD. The client’s condition in answer (c) can be corrected by pain medication that someone else could administer. Answer (d) is incorrect because a temperature elevation of this level would not be a reason for great concern in a client after gallbladder surgery.
Question 50.
The nurse is performing a breast exam on a client when she discovers a mass. Which characteristic of the mass would best indicate a reason for concern?
(a) Tender to the touch
(b) Regular shape
(c) Moves easily
(d) Firm to the touch
Answer:
(d) Firm to the touch
Rationale:
Answer (d) is correct. A malignant mass is usually firm and hard, typically is located in one breast, is not movable, and has an irregular shape. Answers (a), (b), and (c) are not characteristics of a malignancy.
Question 51.
The nurse is caring for a client after a motor vehicle accident. The client has a fractured tibia, and bone is noted protruding through the skin. Which action is of priority?
(a) Provide manual traction above and below the leg.
(b) Cover the bone area with a sterile dressing.
(c) Apply an ACE bandage around the entire lower limb.
(d) Place the client in the prone position.
Answer:
(b) Cover the bone area with a sterile dressing.
Rationale:
Answer (b) is correct. The client has an open fracture, so the priority would be to cover the wound and prevent further contamination. Swelling usually occurs with a fracture, making answer (c) incorrect. Manual traction should not be attempted, as in answer (a). Placing the client in the prone position, as in answer (d), provides excessive movement and is an inappropriate action.
Question 52.
The RN on the oncology unit is preparing to mix and administer amphoteracin B (Fungizone) to a client. Which action is contraindicated for administering this drug IV?
(a) Mix the drug with normal saline solution.
(b) Administer the drug over 4-6 hours.
(c) Hydrate with IV fluids two hours before the infusion is scheduled to begin.
(d) Premedicate the client with ordered acetaminophen (Tylenol) and diphenhydramine (Benadryl).
Answer:
(a) Mix the drug with normal saline solution.
Rationale:
Answer (a) is correct. The drug can be mixed with D5W only. Mixing with normal saline can cause precipitates to form. The answers in (b), (c), and (d) are appropriate implementations for administering amphoteracin B, so they are incorrect.
Question 53.
A nurse is administering a blood transfusion to a client on the oncology unit. Which clinical manifestation indicates an acute hemolytic reaction to the blood?
(a) Low back pain
(b) Headache
(c) Urticaria
(d) Neck vein distention
Answer:
(a) Low back pain
Rationale:
Answer (a) is correct. This clinical manifestation is due to the hemolysis of the red blood cells in the kidney. Answer (b) doesn’t occur in a hemolytic reaction. A rash or urticaria occurs with an allergic reaction, making answer (c) incorrect. Answer (d) is incorrect because this clinical manifestation usually occurs with circulatory overload.
Question 54.
The nurse caring for a client diagnosed with metastatic cancer of the bone is exhibiting mental confusion and a BP of 150/100. Which laboratory value would correlate with the client’s symptoms reflecting a common complication with this diagnosis?
(a) Potassium 5.2mEq/L
(b) Calcium 13mg/dL
(c) Inorganic phosphorus 1.7mEq/L
(d) Sodium 138mEq/L
Answer:
(b) Calcium 13mg/dL
Rationale:
Answer (b) is correct. Hypercalcemia is a common occurrence with cancer of the bone. Clinical manifestations of hypercalcemia include mental confusion and an elevated blood pressure. The potassium level in answer (a) is elevated, but this is not related to the diagnosis. Answers (c) and (d) are both normal levels.
Question 55.
A client with a stroke and malnutrition has been placed on Total Parenteral Mutrition (TPN). The nurse notes air entering the client via the central line. Which initial action is most appropriate?
(a) Notify the physician.
(b) Elevate the head of the bed.
(c) Place the client in the left lateral decubitus position.
(d) Stop the TPN and hang D5 1/2 NS.
Answer:
(c) Place the client in the left lateral decubitus position.
Rationale:
Answer (c) is correct. The client is at risk for an air embolus. Placing the client in a left lateral decubitus position will displace air from the right ventricle. Answers (b) and (d) would not help, and answer (a) would not be done first.
Question 56.
The nurse is preparing a client for cervical uterine radiation implant insertion. Which will be included in the teaching plan?
(a) TV or telephone use will not be allowed while the implant is in place.
(b) A Foley catheter is usually inserted.
(c) A high-fiber diet is recommended.
(d) Excretions will be considered radioactive.
Answer:
(b) A Foley catheter is usually inserted.
Rationale:
Answer (b) is correct. A catheter will allow urine elimination without disrupting the implant. There is usually no restriction on TV or phone use, as in answer (a). The client is placed on a low-residue diet, not a high-fiber diet, as stated in answer (c). Even though the implant is internally placed, neither the patient nor her secretions are radioactive, but the applicator is. Because secretions are not radioactive, answer (d) is incorrect.
Question 57.
The nurse is caring for a client with a head injury who has an intracranial pressure monitor in place. Assessment reveals an ICP reading of 66. What is the nurse’s best action?
(a) Notify the physician.
(b) Record the reading as the only action.
(c) Turn the client and recheck the reading.
(d) Place the client supine.
Answer:
(a) Notify the physician.
Rationale:
Answer (a) is correct. Normal ICP is 10-20. A reading of 66 is high, and the physician should be notified. Answers (c) and (d) would not be appropriate actions. Answer (b) would be the action if the reading was normal.
Question 58.
The nurse is caring for a client with leukemia who is receiving the drug doxorubicin (Adriamycin). Which toxic effects of this drug would be reported to the physician immediately?
(a) Rales and distended neck veins
(b) Red discoloration of the urine
(c) Nausea and vomiting
(d) Elevated BUN and dry, flaky skin
Answer:
(a) Rales and distended neck veins
Rationale:
Answer (a) is correct. Doxorubicin (Adriamycin) can cause cardiotoxicity exhibited by changes in the ECG and congestive heart failure. Rales and distended neck veins are clinical manifestations of congestive heart failure. Answer (b) is incorrect because the reddish discoloration of the urine is a harmless side effect of doxorubicin. Answer (d) is not specific to this drug, and answer (c) is common and not a reason to immediately notify the physician.
Question 59.
A client has developed diabetes insipidous after removal of a pituitary tumor. Which finding would the nurse expect?
(a) Polyuria
(b) Hypertension
(c) Polyphagia
(d) Hyperkalemia
Answer:
(a) Polyuria
Rationale:
Answer (a) is correct. Clients with diabetes insipidous have excessive urinary output because of the lack of antidiuretic hormone. Answers (b), (c), and (d) are not exhibited with diabetes insipidous so they are incorrect.
Question 60.
A client with cancer received platelet infusions 24 hours ago. Which of the following assessment findings would indicate the most therapeutic effect from the transfusions?
(a) Hemoglobin level increase from 8.9 to 10.6mg/dL
(b) Temperature reading of 99.4°F
(c) White blood cell count of 11,000/mm3
(d) Decrease in oozing of blood from IV site
Answer:
(d) Decrease in oozing of blood from IV site
Rationale:
Answer (d) is correct. Platelets deal with the clotting of blood and a lack of platelets can cause bleeding. Answers (a), (b), and (c) do not directly relate to platelets.
Question 61.
A client is admitted with Parkinson’s disease who has been taking Carbidopa/levodopa (Sinemet) for one year. Which clinical manifestation would be most important to report?
(a) Dry mouth
(b) Spasmodic eye winking
(c) Dark urine color
(d) Complaints of dizziness
Answer:
(b) Spasmodic eye winking
Rationale:
Answer (b) is correct. Spasmodic eye winking could indicate a toxicity or overdose of the drug Carbidopa/levodopa (Sinemet) and should be reported to the physician. Other signs of toxicity include involuntary twitching of muscles, facial grimaces, and severe tongue protrusion. Answers (a), (c), and (d) are side effects but do not indicate toxicity of the drug.
Question 62.
The nurse who is caring for a client with cancer notes a WBC of 500/mm3 on the laboratory results. Which intervention would be most appropriate to include in the client’s plan of care?
(a) Assess temperature every four hours because of risk for hypothermia.
(b) Instruct the client to avoid large crowds and people who are sick.
(c) Instruct in the use of a soft toothbrush.
(d) Assess for signs of bleeding.
Answer:
(b) Instruct the client to avoid large crowds and people who are sick.
Rationale:
Answer (b) is correct. With neutropenia, the client is at risk for infection; therefore, this client would need to avoid crowds and people who are ill. Answer A would not be appropriate, and answers (c) and (d) correlates with a risk for bleeding.
Question 63.
A client with Crohn’s disease requires TPN to provide adequate nutrition. The nurse finds the TPN bag empty. What fluid would the nurse select to hang until another bag is prepared in the pharmacy?
(a) Lactated Ringers
(b) Normal saline
(c) D10W solution
(d) Normosol R
Answer:
(c) D10W solution
Rationale:
Answer (c) is correct. D10W is the preferred solution to prevent complications from a sudden lack of glucose. Answers (a), (b), and (d) do not have glucose.
Question 64.
The nurse is caring for a client with possible cervical cancer. What clinical data would the nurse most likely find in the client’s history?
(a) Post-coital vaginal bleeding
(b) Nausea and vomiting
(c) Foul-smelling vaginal discharge
(d) Elevated temperature levels
Answer:
(a) Post-coital vaginal bleeding
Rationale:
Answer (a) is correct. Vaginal bleeding or spotting is a common symptom of cervical cancer. Nausea, vomiting, and foul-smelling discharge, in answers (b) and (c), are not specific or common to cervical cancer. Hyperthermia, in answer (d), is not related to the diagnosis.
Question 65.
The nurse is preparing to receive a client from admitting with tumor lysis syndrome (TLS). Which of the following would the nurse expect to find on the laboratory and patient history sections of the chart? Select all that apply.
(a) Low blood pressure
(b) Hyperactivity
(c) Hyperkalemia
(d) Hyperuricemia
(e) Mental changes
Answer:
(c) Hyperkalemia
(d) Hyperuricemia
(e) Mental changes
Rationale:
Answers (a), (d), and (e) are correct. TLS is a complication of chemotherapy that causes cells (especially potassium and purines) to be overabundant. Answers (c), (d), and (e) are all associated with TLS. Other symptoms associated with TLS include hypertension and fatigue, therefore answers (a) and (b) would not be selected.
Question 66.
A client is scheduled to undergo a bone marrow aspiration from the sternum. What position would the nurse assist the client into
(a) Dorsal recumbent
(b) Supine
(c) High Fowler’s
(d) Lithotomy
Answer:
(c) High Fowler’s
Rationale:
Answer (c) is correct. A bone marrow aspiration is usually done by the physician with specimens obtained from the sternum or the iliac crest. The high Fowler’s position is the best position in which to obtain a specimen from the client’s sternum. Answers (a), (b), and (d) are inappropriate positions for getting a bone marrow biopsy.
Question 67.
The nurse is caring for a client with a head injury who has increased ICP. The physician plans to reduce the cerebral edema by constricting cerebral blood vessels. Which physician order would serve this purpose?
(a) Hyperventilation per mechanical ventilation
(b) Insertion of a ventricular shunt
(c) Furosemide (Lasix)
(d) Solu medrol
Answer:
(a) Hyperventilation per mechanical ventilation
Rationale:
Answer (a) is correct. Hyperventilation is utilized to decrease the PCO2, producing cerebral blood vessel constriction. Answers (b), (c), and (d) can decrease cerebral edema, but not by constriction of cerebral blood vessels.
Question 68.
A client with a T6 injury six months ago develops facial flushing and a BP of 210/106. After elevating the head of the bed, which is the most appropriate nursing action?
(a) Notify the physician.
(b) Assess the client for a distended bladder.
(c) Apply ordered oxygen via nasal cannula.
(d) Increase the IV fluids.
Answer:
(b) Assess the client for a distended bladder.
Rationale:
Answer (b) is correct. The client is experiencing autonomic hyperreflexia, which can be caused by a full bowel or bladder or a wrinkled sheet. Answer (a) is not the appropriate action before performing the assessment of the bladder; answers (c) and (d) are not appropriate actions in this situation.
Question 69.
The nurse is performing an admission history for a client recovering from a stroke. Medication history reveals the drug clopidogrel (Plavix). Which clinical manifestation alerts the nurse to an adverse effect of this drug?
(a) Epistaxis
(b) Hypothermia
(c) Nausea
(d) Hyperactivity
Answer:
(a) Epistaxis
Rationale:
Answer (a) is correct. Plavix is an antiplatelet. Bleeding from the nose (epistaxis) could indicate a severe effect. Answers (b), (c), and (d) are not associated with the undesired effects of Plavix.
Question 70.
The nurse caring for a client with a head injury would recognize which assessment finding as the most indicative of increased ICP?
(a) Vomiting
(b) Headache
(c) Dizziness
(d) Papilledema
Answer:
(d) Papilledema
Rationale:
Answer (d) is correct. Papilledema is a hallmark symptom of increased intracranial pressure. Answers (a), (b), and (c) are not as conclusive.
Question 71.
A client with angina is experiencing migraine headaches. The physician has prescribed Sumatriptan succinate (Imitrex). Which nursing action is most appropriate?
(a) Call the physician to question the prescription order.
(b) Try to obtain samples for the client to take home.
(c) Perform discharge teaching regarding this drug.
(d) Consult social services for financial assistance with obtaining the drug.
Answer:
(a) Call the physician to question the prescription order.
Rationale:
Answer (a) is correct. Imitrex results in cranial vasoconstriction to reduce pain, but it can also cause vasoconstrictive effects systemically. Therefore, it is contraindicated in clients with angina, and the physician should be notified. Answers (b) and (d) are inappropriate actions from the information given. Answer (c) is appropriate, but answer (a) is the most appropriate.
Question 72.
A client with COPD is in respiratory failure. Which of the following results would be the most sensitive indicator that the client requires a mechanical ventilator?
(a) PCO2 58
(b) SaO2 90
(c) PH 7.23
(d) HCO3 30
Answer:
(c) PH 7.23
Rationale:
Answer (c) is correct. The pH is an accurate indicator of acute ventilatory failure and a need for mechanical ventilation. An elevated PCO2, as in answer A, is not an adequate criterion for instituting ventilator support. Answer (b), oxygen saturation of 90, would not be very abnormal for a COPD client. Answer (d) is normal.
Question 73.
The nurse in the emergency room is caring for a client with multiple rib fractures and a pulmonary contusion. Assessment reveals a respiratory rate of 38, a heart rate of 136, and restlessness. Which associated assessment finding would require immediate intervention?
(a) Occasional small amounts of hemoptysis
(b) Midline trachea with wheezing on auscultation
(c) Subcutaneous air and absent breath sounds
(d) Pain when breathing deeply, with rales in the upper lobes
Answer:
(c) Subcutaneous air and absent breath sounds
Rationale:
Answer (c) is correct. The absence of breath sounds and subcutaneous air, increased heart rate, dyspnea, and restlessness indicate a pneumothorax, which would require immediate intervention. Answer (a) could occur with the pulmonary contusion and would be expected. Answer (d) would be expected with fractured ribs. Answer (b) is not a cause for great concern because the midline trachea is a normal finding.
Question 74.
The nurse is caring for a client with myasthenia gravis who is having trouble breathing. The nurse would encourage which of the following positions for maximal lung expansion?
(a) Supine with no pillow, to maintain patent airway
(b) Side-lying with back support
(c) Prone with head turned to one side
(d) Sitting or in high Fowler’s
Answer:
(d) Sitting or in high Fowler’s
Rationale:
Answer (d) is correct. A position of sitting or high Fowler’s is the best choice for assisting the client to use respiratory muscles to breathe and lift the diaphragm from the abdominal area. Answer (a) is contraindicated, and answers (b) and (c) would not help as much as answer (d) for breathing.
Question 75.
The nurse is caring for clients on a respiratory unit. Upon receiving the following client reports, which client should be seen first?
(a) Client with emphysema expecting discharge
(b) Bronchitis client receiving IV antibiotics
(c) Bronchitis client with edema and neck vein distention
(d) COPD client with abnormal PO2
Answer:
(c) Bronchitis client with edema and neck vein distention
Rationale:
Answer (c) is correct. This client is exhibiting symptoms of heart failure that happen commonly in clients with a COPD disorder. The client in answer (a) is being discharged, and the client in answer (d) with an abnormal PO2 would not be cause for alarm in a COPD client. The client in answer (b) would not require immediate attention.
Question 76.
A client has sustained a severe head injury and damaged the pre- occipital lobe. The nurse should remain particularly alert for which of the following problems?
(a) Visual impairment
(b) Swallowing difficulty
(c) Impaired judgment
(d) Flearing impairment
Answer:
(a) Visual impairment
Rationale:
Answer (a) is correct. The occipital lobe is the visual lobe. If the client were having problems with the occipital lobe, it would mean that the edema and bleeding were increasing in that area. Answers (b), (c), and (d) are not related to the occipital lobe.
Question 77.
The nurse is caring for a client with epilepsy who is to receive phenytoin sodium (Dilantin) 100mg IV push. The client has an IV of D51/2NS infusing at 100mL/hr. When administering the Dilantin, which is the appropriate initial nursing action?
(a) Obtain an ambu bag and put it at bedside.
(b) Insert a 16g IV catheter.
(c) Flush the IV line with normal saline.
(d) Premedicate with promethiazine (phenergan) IV push.
Answer:
(c) Flush the IV line with normal saline.
Rationale:
Answer (c) is correct. Flushing of the line is required when giving Dilantin IV push because Dilantin crystallizes in the tubing if D5W is present. Answers (a), (b), and (d) would not be appropriate or necessary for this procedure.
Question 78.
A client with increased intracranial pressure is receiving Osmitrol (Mannitol) and Furosemide (Lasix). The nurse recognizes that these two drugs are given to reverse which effect?
(a) Energy failure
(b) Excessive intracellular calcium
(c) Cellular edema
(d) Excessive glutamate release
Answer:
(c) Cellular edema
Rationale:
Answer (c) is correct. Lasix and Mannitol are given for their diuretic effects in decreasing cerebral edema. Answers (a), (b), and (d) are not the effects of the drugs in this situation.
Question 79.
The nurse is assessing a client upon arrival to the emergency department. Partial airway obstruction is suspected. Which clinical manifestation is a late sign of airway obstruction?
(a) Rales in lungs
(b) Restless behavior
(c) Cyanotic ear lobes
(d) Inspiratory stridor
Answer:
(c) Cyanotic ear lobes
Rationale:
Answer (c) is correct. Cyanosis and loss of consciousness will occur later as the obstruction worsens. Answers (b) and (d) are both earlier symptoms of obstruction, and answer A is not a definite clinical manifestation of obstruction.
Question 80.
The nurse is working in the trauma unit of the emergency room when a 24-year-old female is admitted after an MVA. The client is bleeding profusely and a blood transfusion is ordered. Which would the nurse be prepared to administer without a type and crossmatch?
(a) AB positive
(b) AB negative
(c) 0 positive
(d) 0 negative
Answer:
(d) 0 negative
Rationale:
Answer (d) is correct. 0 negative blood type is universal blood type for females of childbearing age. Answers (a), (b), and (c) are not to be given to females of childbearing age if this is not their blood type. A blood type of 0 positive is given to males and postmenopausal women in emergencies.
Question 81.
When preparing a client for magnetic resonance imaging, the nurse should implement which of the following?
(a) Obtain informed consent and administer atropine 0.4mg.
(b) Scrub the injection site for 15 minutes.
(c) Remove any jewelry and inquire about metal implants.
(d) Administer Benadryl 50mg/mL IV.
Answer:
(c) Remove any jewelry and inquire about metal implants.
Rationale:
Answer (c) is correct. An MRI uses a powerful magnetic force; therefore, any metal or jewelry should be removed before this test. Answers (a), (b), and (d) are not appropriate for this test.
Question 82.
Upon admission to the hospital, a client reports having “the worst headache I’ve ever had.” The nurse should give the highest priority to which action?
(a) Administering pain medication
(b) Starting oxygen
(c) Performing neuro checks
(d) Inserting a Foley catheter
Answer:
(c) Performing neuro checks
Rationale:
Answer (c) is correct. The nurse should pay particular attention to any complaints of a headache when it is described in this way. The client could have a cerebral aneurysm. Pain medications are contraindicated in an undiagnosed neurological clients, so answer (a) is not appropriate. No criterion in the stem makes answers (b) or (d) appropriate.
Question 83.
A client has an order to administer cisplatin (Platinol). Which drug would the nurse expect to be ordered to reduce renal toxicity from the cisplatin infusion?
(a) Amifostine (Ethyol)
(b) Dexrazoxane (Zinecard)
(c) Mesna (Mesenex)
(d) Pamidronate (Aredia)
Answer:
(a) Amifostine (Ethyol)
Rationale:
Answer (a) is correct. Ethyol is used to reduce renal toxicity with cisplatin administration. The drugs in answers (b), (c), and (d) are cytoprotectants not used for cisplatin administration so they are incorrect.
Question 84.
The client is admitted to the ER with multiple rib fractures on the right. The nurse’s assessment reveals that an area over the right clavicle is puffy and that there is a “crackling” noise with palpation. The nurse should further assess the client for which of the following problems?
(a) Flail chest
(b) Subcutaneous emphysema
(c) Infiltrated subclavian IV
(d) Pneumothorax
Answer:
(d) Pneumothorax
Rationale:
Answer (d) is correct. The nurse should further assess the client for the cause of the symptoms, usually a pneumothorax. Answer (a) is another type of chest trauma not associated with the symptoms. Answer (b) is simply a term used to describe the symptoms, and answer (c) is not an appropriate assessment for these symptoms.
Question 85.
A client has an order for Demerol 75mg and atropine 0.4mg IM as a preoperative medication. The Demerol vial contains 50mg/mL, and atropine is available 0.4mg/mL. Flow much medication will the nurse administer in total?
(a) 1.0mL
(b) 1.7mLs
(c) 2.5mLs
(d) 3.0 mLs
Answer:
(c) 2.5mLs
Rationale:
Answer (c) is correct. The calculated dosage of Atropine is 1.OmL, and the calculated dosage of Demerol is 1.5mL, making a total of 2.5mL the correct answer. Answers (a), (b), and (d) are incorrect calculations.
Question 86.
Nimodipine (Nimotop) is ordered for the client with a ruptured cerebral aneurysm. What does the nurse recognize as a desired effect of this drug?
(a) Prevent the influx of calcium into cells.
(b) Restore a normal blood pressure reading.
(c) Prevent the inflammatory process.
(d) Dissolve the clot that has formed.
Answer:
(a) Prevent the influx of calcium into cells.
Rationale:
Answer (a) is correct. Nimotop is a calcium channel blocker and is used to prevent calcium influx. The etiology of vasospasm of the blood vessel has been thought to relate to this calcium influx; therefore, the drug is given to prevent this. Answers (b), (c), and (d) do not describe the action of this drug.
Question 87.
A client is admitted to the hospital with seizures. The client has jerking of the right arm and twitching of the face, but is alert and aware of the seizure. This behavior is characteristic of which type of seizure?
(a) Absence
(b) Complex partial
(c) Simple partial
(d) Tonic-clonic
Answer:
(c) Simple partial
Rationale:
Answer (c) is correct. A simple partial seizure is characterized by jerking of extremities, twitching of the face, and mental alertness. Answers (a), (b), and (d) are not characterized with these clinical manifestations. Answer (b) is differentiated by the client’s awareness of the seizure.
Question 88.
The intensive care unit is full and the emergency room just called in a report on a ventilator-dependent client who is being admitted to the medical surgical unit. It would be essential that the nurse have which piece of equipment at the client’s bedside?
(a) Cardiac monitor
(b) Intravenous controller
(c) Manual resuscitator
(d) Oxygen by nasal cannula
Answer:
(c) Manual resuscitator
Rationale:
Answer (c) is correct. The essential piece of equipment is the ambu bag (manual resus- citator). Ventilator clients must always have another means of ventilation in case of a problem, such as a power failure. Answers (a) and (b) may be needed, but not as much as answer (c). Answer (d) is inappropriate for a client on the ventilator.
Question 89.
The nurse is caring for a client on a ventilator that is set on intermittent mandatory ventilation (IMV). Assessment on the ventilator is IMV mode of eight breaths per minute. The nurse assesses the client’s respiratory rate of 13 per minute. What do these findings indicate?
(a) The client is “fighting” the ventilator and needs medication.
(b) Pressure support ventilation is being used.
(c) Additional breaths are being delivered by the ventilator.
(d) The client is breathing five additional breaths on his own.
Answer:
(d) The client is breathing five additional breaths on his own.
Rationale:
Answer (d) is correct. If the ventilator is set for eight breaths per minute and the client's rate is 13 per minute, subtract 8 from 13 to find that the client is actually breathing five breaths on his own. Answers (a), (b), and (c) are incorrect information for the description provided in the stem, so they are wrong.
Question 90.
The nurse has given instructions on pursed-lip breathing to a client with COPD. Which statement by the client would indicate effective teaching?
(a) “I should inhale through my mouth very deeply."
(b) “I should tighten my abdominal muscles with inhalation.”
(c) “I should contract my abdominal muscles with exhalation.”
(d) “I should make inhalation twice as long as exhalation.”
Answer:
(c) “I should contract my abdominal muscles with exhalation.”
Rationale:
Answer (c) is correct. Contracting the abdominal muscles with exhalation is the proper technique for pursed-lip breathing. Answers (a), (b), and (d) are all incorrect techniques. The goal is to increase the exhalation phase.
Question 91.
A client is receiving aminophylline IV. The nurse monitors the theophylline blood level and assesses that the level is within therapeutic range at which of the following levels?
(a) 5ug/mL
(b) 8ug/mL
(c) 15ug/mL
(d) 25ug/mL
Answer:
(c) 15ug/mL
Rationale:
Answer (c) is correct. A level of 15ug/mL is within the normal therapeutic theophylline level of 10-20ug/mL. Answers (a), (b), and (d) are not within the therapeutic range.
Question 92.
The nurse is assessing the arterial blood gases (ABG) of a chest trauma client with the results of pH 7.35, PO2 85, PCO2 55, and HCO3 27. What do these values indicate?
(a) Uncompensated respiratory acidosis
(b) Uncompensated metabolic acidosis
(c) Compensated respiratory acidosis
(d) Compensated metabolic acidosis
Answer:
(c) Compensated respiratory acidosis
Rationale:
Answer (c) is correct. Readings of pH 7.35, PO2 85, PCO2 55, and HCO3 27 represent compensated respiratory acidosis with increased PCO2 (normal 35-45), low pH of less than 7.4 (normal 7.35-7.45), and high HCO3 with compensation (normal 22-26). Answers A, B, and D are not reflected in the blood gas results listed in the stem.
Question 93.
A pneumonectomy is performed on a client with lung cancer. Which of the following would probably be omitted from the
client's plan of care?
(a) Closed chest drainage
(b) Pain-control measures
(c) Supplemental oxygen administration
(d) Coughing and deep-breathing exercises
Answer:
(a) Closed chest drainage
Rationale:
Answer (a) is correct. Closed chest drainage is not usually used because it is helpful for serous fluid to accumulate in the space to prevent mediastinal shift. Answers (b), (c), and (d) are all involved in care of a client with lung surgery.
Question 94.
When planning the care for a client after a posterior fossa (infratentorial) craniotomy, which action is contraindicated?
(a) Keeping the client flat on one side
(b) Elevating the head of the bed 30°
(c) Log-rolling or turning as a unit
(d) Keeping the neck in a neutral position
Answer:
(b) Elevating the head of the bed 30°
Rationale:
Answer (b) is correct. Any posterior craniotomy requires the client to lie flat and on one side as in answer (a), rather than with the head of the bed elevated, as stated in answer (b). A posterior fossa procedure would be at the lower back of the head. Answer (c) would not be contraindicated, and answer (d) would help to decrease intracranial pressure.
Question 95.
The nurse is performing discharge teaching on a client with ulcerative colitis who has been placed on a low-residue diet.
Which food would need to be eliminated from this client’s diet?
(a) Roasted chicken
(b) Noodles
(c) Cooked broccoli
(d) Roast beef
Answer:
(c) Cooked broccoli
Rationale:
Answer (c) is correct. Raw or cooked vegetables are not allowed on a low-residue diet. Answers (a), (b), and (d) are all allowed foods,
Question 96.
The nurse is assisting a client with diverticulitis to select appropriate foods. Which food should be avoided?
(a) Bran
(b) Fresh peach
(c) Tomatoes
(d) Dinner roll
Answer:
(c) Tomatoes
Rationale:
Answer (c) is correct. A client with diverticulitis should avoid high-fiber foods containing seeds or nuts. Other foods to avoid include corn, popcorn, celery, figs, and strawberries. Answers (a), (b), and (d) are foods that do not contain nuts or seeds and would not need to be avoided.
Question 97.
A client is admitted with a possible bowel obstruction. Which question during the nursing history is least helpful in obtaining information regarding this diagnosis?
(a) “Tell me about your pain.”
(b) “What does your vomit look like?”
(c) “Describe your usual diet.”
(d) “Have you noticed an increase in abdominal size?”
Answer:
(c) “Describe your usual diet.”
Rationale:
Answer (c) is correct. Asking the client about his usual diet is the least helpful information in identifying the problem. Answer (a) is important because the pain sometimes decreases as obstruction worsens. The distention in answer (d) indicates obstruction, and answer (b) is useful because a description of the vomit can help differentiate the type of obstruction.
Question 98.
The nurse is caring for a client with epilepsy who is being treated with carbamazepine (Tegretol). Which laboratory value might indicate a serious side effect of this drug?
(a) BUN 10mg/dL
(b) Hemoglobin 13.0gm/dL
(c) WBC 4,000/mm3
(d) Platelets 200,000/mm3
Answer:
(c) WBC 4,000/mm3
Rationale:
Answer C is correct. Tegretol can cause bone marrow depression, which is evident by the low WBC of 4,000 (normal 5,000-10,000). It can also cause problems with the liver that would raise the BUN (normal 5-25mg/dL). Answers (a), (b), and (d) are not related to the adverse effects of this drug.
Question 99.
A client is admitted with a tumor in the parietal lobe. Which symptoms would be expected due to this tumor’s location?
(a) Hemiplegia
(b) Aphasia
(c) Paresthesia
(d) Nausea
Answer:
(c) Paresthesia
Rationale:
Answer (c) is correct. The parietal lobe deals with sensation; therefore, anyone with a problem in this area of the brain can have problems with sensation. Answers (a), (b), and (d) are not directly associated with this part of the brain.
Question 100.
A client weighing 150 pounds has received burns over 50% of his body at 1200 hours. Using the Parkland formula, calculate the expected amount of fluid that the client should receive by 2000 hours.
(a) 3,400
(b) 6,800
(c) 10,200
(d) 13,600
Answer:
(b) 6,800
Rationale:
Answer (b) is correct. Every nurse must know military times, Parkland formula, and how to calculate the amount of fluid needed for replacement therapy. The Parkland formula is 4mL × Weight in kilograms × Percentage of body surface area burned = Amount of fluid to be given in 24 hours. The nurse is to give half this amount in the first eight hours.
4mL × 68kg × 50% BSA = 13,600ml (amount to be given in 24 hours)
Give half this amount in the first eight hours.
13,600 ÷ 2 = 6,800
Answers (a), (c), and (d) are incorrect calculations.
Question 101.
The nurse is caring for a client post-op femoral popliteal bypass graft. Which post-operative assessment finding would require immediate physician notification?
(a) Edema of the extremity and pain at the incision site
(b) A temperature of 99.6°F and redness of the incision
(c) Serous drainage noted at the surgical area
(d) A loss of posterior tibial and dorsalis pedis pulses
Answer:
(d) A loss of posterior tibial and dorsalis pedis pulses
Rationale:
Answer (d) is correct. A loss of pulse could indicate an occlusion in the graft that requires surgical intervention. Answers (a) and (c) are expected post-operative occurrences with this surgical procedure, which makes them incorrect. Answer (b) is not an immediate concern, so it is incorrect.
Question 102.
A client admitted with gastroenteritis and a potassium level of 2.9mEq/dL has been placed on telemetry. Which ECG finding would the nurse expect to find due to the client’s potassium
results?
(a) A depressed ST segment
(b) An elevated T wave
(c) An absent P wave
(d) A flattened QRS
Answer:
(a) A depressed ST segment
Rationale:
Answer (a) is correct. ECG changes associated with hypokalemia are peaked P waves, flat T waves, depressed ST segments, and prominent U waves. Answers (b), (c), and (d) are not associated with low potassium levels, so they are incorrect.
Question 103.
A client is experiencing acute abdominal pain. Which abdominal assessment sequence is appropriate for the nurse to use for examination of the abdomen?
(a) Inspect, palpate, auscultate, percuss
(b) Inspect, auscultate, percuss, palpate
(c) Auscultate, inspect, palpate, percuss
(d) Percuss, palpate, auscultate, inspect
Answer:
(b) Inspect, auscultate, percuss, palpate
Rationale:
Answer (b) is correct. Inspect, auscultate, percuss, and palpate is the correct sequence of assessing the abdomen. The initial step is to inspect the abdomen. Auscultation must be accomplished before touching because movement could make auscultation inaccurate. Answers (a), (c), and (d) are incorrect assessment sequences.
Question 104.
The nurse is to administer a cleansing enema to a client scheduled for colon surgery. Which client position would be appropriate?
(a) Prone
(b) Supine
(c) Left Sim’s
(d) Dorsal recumbent
Answer:
(c) Left Sim’s
Rationale:
Answer (c) is correct. Left Sim’s position is the best position because it follows the natural direction of the colon. In answer (a), the client would be placed on the abdomen. In answers (b) and (d), the client would be placed on the back, so these answers are incorrect.
Question 105.
The nurse is caring for a client following a crushing injury to the chest. Which finding would be most indicative of a tension pneumothorax?
(a) Expectoration of moderate amounts of frothy hemoptysis
(b) Trachea shift toward the unaffected side of the chest
(c) Subcutaneous emphysema noted at the anterior chest
(d) Opening chest wound with a whistle sound emitting from the area
Answer:
(b) Trachea shift toward the unaffected side of the chest
Rationale:
Answer (b) is correct. Trachea shift differentiates this clinical manifestation as a tension pneumothorax. When a person has a tension pneumothorax, air enters but cannot escape, causing a pressure buildup and shifting of the great vessels, the heart, and the trachea to the unaffected side. Answer (a) correlates with a pulmonary contusion, so it is incorrect. Answers (c) and (d) are associated with a pneumothorax; this makes them nonspecific for a tension pneumothorax and, thus, incorrect.
Question 106.
The nurse receives a report from the paramedic on four trauma victims. Which client would need to be treated first? A client with:
(a) Lower rib fractures and a stable chest wall
(b) Bruising on the anterior chest wall and a possible pulmonary contusion
(c) Gun shot wound with open pneumothorax unstabilized
(d) Dyspnea, stabilized with intubation and manual resus- citator
Answer:
(c) Gun shot wound with open pneumothorax unstabilized
Rationale:
Answer (c) is correct. A client with an open pneumothorax is in distress and should be seen by the nurse first. The key word in this correct response is unstable. The clients in answers (a), (b), and (d) are more stable clients or those that are not as severely ill as the client in (c), so they are incorrect.
Question 107.
The nurse is discharging a client with asthma who has a prescription for zafirlukast (Accolate). Which comment by the client would indicate a need for further teaching?
(a) “I should take this medication with meals.”
(b) “I need to report flu-like symptoms to my doctor.”
(c) “My doctor might order liver tests while I’m on this drug."
(d) “If I’m already having an asthma attack, this drug will not stop it.”
Answer:
(a) “I should take this medication with meals.”
Rationale:
Answer (a) is correct. Accolate should be taken one hour before or two hours after eating, to prevent slow absorption of the drug when taken with meals; therefore, this statement is incorrect and requires further teaching by the nurse. Answers (b), (c), and (d) are all true statements regarding this drug and are correct statements made by the client.
Question 108.
A client is four hours post-op left carotid endarterectomy. Which assessment finding would cause the nurse the most concern?
(a) Temperature 99.4°F, heart rate 110, respiratory rate 24
(b) Drowsiness, urinary output of 50mL in the past hour
(c) BP 120/60, lethargic, right-sided weakness
(d) Alert and oriented, BP 168/96, heart rate 70
Answer:
(c) BP 120/60, lethargic, right-sided weakness
Rationale:
Answer (c) is correct. The assessment finding that causes the most concern is the one indicating a possible stroke. Right-sided weakness would mean that there is a loss of muscular functioning on the side opposite the surgical procedure. Answers (a), (b), and (d) might indicate a need for reassessments but are not a cause for immediate concern or intervention, so they are incorrect.
Question 109.
The RN is making assignments on a 12-bed unit. Staff consists of one RN and two certified nursing assistants. Which client should be self-assigned?
(a) A client receiving decadron for emphysema
(b) A client with chest trauma and a new onset of hemoptysis
(c) A client with rib fractures and an O2 saturation of 93%
(d) A client two days post-operative lung surgery with a pulse oximetry of 92%
Answer:
(b) A client with chest trauma and a new onset of hemoptysis
Rationale:
Answer (b) is correct. This client is the least stable of the ones listed. The key term in this answer is the word new. Bleeding would also give this client a priority status because of the possible deficit in maintaining circulation. The clients in answers (a), (c), and (d) are more stable, so they can be assigned to other personnel.
Question 110.
The nurse is accessing a venous access port of a client about to receive chemotherapy.
Place the following steps in proper sequential order.
(a) Apply clean gloves.
(b) Clean the skin with antimicrobial and let air dry.
(c) Insert needle into port at a 90° angle.
(d) Connect 10 mL NS into extension of huber needle and prime.
(e) Instill heparin solution.
(f) Stabilize the part by using middle and index fingers.
(g) Wash hands and apply sterile gloves.
(h) Inject saline and assess for infiltration.
(i) Check placement of needle.
Answer:
(a) Apply clean gloves.
(b) Clean the skin with antimicrobial and let air dry.
(d) Connect 10 mL NS into extension of huber needle and prime.
(g) Wash hands and apply sterile gloves.
(f) Stabilize the part by using middle and index fingers.
(c) Insert needle into port at a 90° angle.
(i) Check placement of needle.
(h) Inject saline and assess for infiltration.
(e) Instill heparin solution.
Rationale:
The correct answer sequence is as follows:
(a) Apply clean gloves.
(b) Clean the skin with antimicrobial and let air dry.
(d) Connect 10 mL NS into extension of huber needle and prime.
(g) Wash hands and apply sterile gloves.
(f) Stabilize the part by using middle and index fingers.
(c) Insert needle into port at a 90° angle.
(i) Check placement of needle.
(h) Inject saline and assess for infiltration.
(e) Instill heparin solution.
Question 111.
A client is being discharged on Coumadin after hospitalization for a deep vein thrombosis. The nurse recognizes that which food would be restricted while the client is on this medication?
(a) Lettuce
(b) Apples
(c) Potatoes
(d) Macaroni
Answer:
(a) Lettuce
Rationale:
Answer (a) is correct. Vitamin K decreases the effects of Coumadin. The client should be taught to avoid green, leafy vegetables, such as broccoli, cabbage, turnip greens, and lettuce. Answers (b), (c), and (d) are food choices that are low in vitamin K, so they are incorrect.
Question 112.
Which assessment finding in a client with COPD indicates to the nurse that the respiratory problem is chronic?
(a) Wheezing on exhalation
(b) Productive cough
(c) Clubbing of fingers
(d) Generalized cyanosis
Answer:
(c) Clubbing of fingers
Rationale:
Answer C is correct. The clinical manifestation of clubbing of the fingers takes time, indicating that the condition is chronic and not acute. Answers A, B, and D are all nonspecific for chronicity, so they are incorrect.
Question 113.
A client who has just undergone a laparoscopic cholecystectomy complains of “free air pain.” What would be your best action?
(a) Ambulate the client.
(b) Instruct the client to breathe deeply and cough.
(c) Maintain the client on bed rest with his legs elevated.
(d) Insert an NG tube.
Answer:
(a) Ambulate the client.
Rationale:
Answer A is correct. Ambulating the client should help to pass the air. The air is used during the surgical procedure to assist in performance of the surgery. Answers (b) and (c) would not help, and answer (d) is not necessary or appropriate at this time.
Question 114.
The RN is planning client assignments. Which is the least appropriate task for the nursing assistant?
(a) Assisting a COPD client admitted two days ago to get up in the chair.
(b) Feeding a client with bronchitis who is paralyzed on the right side.
(c) Accompanying a discharged emphysema client to the transportation area.
(d) Assessing an emphysema client complaining of difficulty breathing.
Answer:
(d) Assessing an emphysema client complaining of difficulty breathing.
Rationale:
Answer (d) is correct. Assessment is not within the role of a nurse’s assistant, which makes this the least appropriate of the tasks listed. Answers A, B, and C are all appropriate tasks for an assistant, so they are incorrect.
Question 115.
When providing care for a client with pancreatitis, the nurse would anticipate which of the following orders?
(a) Force fluids to 3,000mL/24 hours.
(b) Insert a nasogastric tube to low intermittent suction.
(c) Place the client in reverse Trendelenburg position.
(d) Place the client in enteric isolation.
Answer:
(b) Insert a nasogastric tube to low intermittent suction.
Rationale:
Answer B is correct. An NG is inserted to decrease the secretion of pancreatic juices and assist in pain relief. Answer A is incorrect because these clients are held NPO. Clients are placed in semi-Fowler’s position, which makes answer C incorrect. Answer D is not appropriate because the wastes are not contaminated.
Question 116.
The nurse is performing a neurological assessment on a client admitted with TIAs. Assessment findings reveal an absence of the gag reflex. The nurse suspects injury to which of the following cranial nerves?
(a) XII (hypoglossal)
(b) X (vagus)
(c) IX (glossopharyngeal)
(d) VII (facial)
Answer:
(b) X (vagus)
Rationale:
Answer B is correct. To test for vagus nerve problems, the nurse uses a tongue blade and depresses the back of the throat to elicit a gag reflex. Another way to test for damage to the vagus nerve is to have the client say “Ah” while observing for uniform rising of the uvula and the soft palate. The absence of this reflex could indicate damage to the X cranial nerve. Answers A, C, and D are not tested in this manner, so they are incorrect.
Question 117.
The nurse arrives at a motorcycle accident and finds the client unresponsive, apneic, and pulseless. After calling for a spectator to help, what would be the nurse’s next action?
(a) Ventilate with a mouth-to-mask device.
(b) Begin chest compressions.
(c) Administer a precordial thump.
(d) Open the client’s airway.
Answer:
(d) Open the client’s airway.
Rationale:
Answer (d) is correct. The next step after calling for help is to open the airway to ventilate the client. Answers (a) and (b) are not performed until after answer (d), so they are incorrect. Answer (c) is not a correct procedure for this situation.
Question 118.
A client with gallstones and obstructive jaundice is experiencing severe itching. The physician has prescribed cholestyramine (Questran). The client asks, “How does this drug work?” What is the nurse’s best response?
(a) “It blocks histamine, reducing the allergic response.”
(b) “It inhibits the enzyme responsible for bile excretion.”
(c) “It decreases the amount of bile in the gallbladder.”
(d) “It binds with bile acids and is excreted in bowel movements with stool.”
Answer:
(d) “It binds with bile acids and is excreted in bowel movements with stool.”
Rationale:
Answer D is correct. Questran works by binding the bile acid in the Gl tract and eliminating it, decreasing the itching associated with jaundice. Answers A, B, and C are not how Questran works to decrease itching.
Question 119.
A client with inflammatory bowel disease (IBD) requires an ileostomy. The nurse would instruct the client to do which of the following measures as an essential part of caring for the stoma?
(a) Perform massage of the stoma three times a day.
(b) Include high-fiber foods in the diet, especially nuts.
(c) Limit fluid intake to prevent loose stools.
(d) Cleanse the peristomal skin meticulously.
Answer:
(d) Cleanse the peristomal skin meticulously.
Rationale:
Answer (d) is correct. Careful cleansing is necessary to prevent skin breakdown and skin irritation. Answer (a) is not an intervention used for ileostomies. Clients should avoid the high-fiber and gas-producing foods in answer (b). Answer (c) is incorrect because these clients are not on fluid restriction.
Question 120.
Diphenoxylate hydrochloride and atropine sulfate (Lomotil) is prescribed for the client with ulcerative colitis. Which of the following nursing observations indicates that the drug is having a therapeutic effect?
(a) There is an absence of peristalsis.
(b) The number of diarrhea stools decreases.
(c) Cramping in the abdomen has increased.
(d) Abdominal girth size increases.
Answer:
(b) The number of diarrhea stools decreases.
Rationale:
Answer B is correct. Lomotil’s desired effect is to decrease Gl motility and the number of diarrhea stools. Answers A and D do not occur with the use of Lomotil. The drug should decrease cramping instead of increasing it, as in answer C.
Question 121.
A nurse is assisting the physician with chest tube removal. Which client instruction is appropriate during removal of the tube?
(a) Take a deep breath, exhale, and bear down.
(b) Hold the breath for two minutes and exhale slowly.
(c) Exhale upon actual removal of the tube.
(d) Continually breathe deeply in and out during removal.
Answer:
(a) Take a deep breath, exhale, and bear down.
Rationale:
Answer (a) is correct. During chest tube removal this procedure prevents air entrance into the chest cavity. Answers (b) and (c) are inappropriate actions for chest tube removal. Answer (d) could allow the air to enter the thoracic cavity, so it is incorrect.
Question 122.
A client with advanced Alzheimer’s disease has been prescribed haloperidol (Haldol). What clinical manifestation suggests that the client is experiencing side effects from this medication?
(a) Cough
(b) Tremors
(c) Diarrhea
(d) Pitting edema
Answer:
(b) Tremors
Rationale:
Answer B is correct. Tremors are an extrapyramidal side effect that can occur when taking Haldol. Answers A, C, and D are not side or adverse effects of Haldol so are incorrect.
Question 123.
A student in a cardiac unit is performing auscultation of a client’s heart. Which stethoscope placement would indicate to the nurse that the student is performing pulmonic auscultation correctly?
(a) Between the apex and the sternum
(b) At the fifth intercostal space at the left midclavi- cular line
(c) At the second intercostal space, left of the sternum
(d) At the manubrium area of the chest
Answer:
(c) At the second intercostal space, left of the sternum
Rationale:
Answer (c) is correct. The pulmonic area is found in the second intercostal space, left of the sternum. Answer (b) is the correct location of the tricuspid area. Answers (a) and (d) are not assessment locations for heart auscultation.
Question 124.
A client with Alzheimer’s disease has been prescribed donepezil (Aricept). Which information should the nurse include in the teaching plan for a client on Aricept?
(a) “Take the medication with meals.”
(b) “The medicine can cause dizziness, so rise slowly.”
(c) “If a dose is skipped, take two the next time.”
(d) “The pill can cause an increase in heart rate.”
Answer:
(b) “The medicine can cause dizziness, so rise slowly.”
Rationale:
Answer (b) is correct. A side effect of Aricept is dizziness; therefore, the client should be reminded to move slowly when rising from a lying or sitting position. Answer (a) is incorrect because it should be taken at bedtime, with no regard to food. Increasing the number of pills can increase the side effects, so answer (c) is incorrect. Another effect of the drug is bradycardia, making answer (d) incorrect.
Question 125.
A client who had major abdominal surgery is having delayed healing of the wound. Which laboratory test result would most closely correlate with this problem?
(a) Decreased albumin
(b) Decreased creatinine
(c) Increased calcium
(d) Increased sodium
Answer:
(a) Decreased albumin
Rationale:
Answer (a) is correct. Protein is a necessary component of wound healing. An inadequate amount of protein would correlate with the client’s wound not healing properly. Answers (b), (c), and (d) do not directly relate to wound healing, so they are incorrect.
Question 126.
A client is admitted to the medical-surgical unit with a report of severe hematemesis. What is the priority nursing action?
(a) Performing an assessment
(b) Obtaining a blood permit
(c) Initiating an IV
(d) Inserting an NG tube
Answer:
(a) Performing an assessment
Rationale:
Answer (a) is correct. The first step is to assess the client, noting any signs or symptoms of a fluid volume deficit. Answers (b), (c), and (d) might all be required interventions at some point, but assessment is needed before any other actions, so they are incorrect.
Question 127.
The nurse caring for a client with a suspected peptic ulcer recognizes which exam as the one most reliable in diagnosing the disease?
(a) Upper-gastrointestinal x-ray
(b) Gastric analysis
(c) Endoscopy procedure
(d) Barium studies x-ray
Answer:
(c) Endoscopy procedure
Rationale:
Answer C is correct. All of the tests listed can be used to diagnose an ulcer, but an endoscopic exam is the only way to obtain accurate visual evidence. Answers A, B, and D are not as accurate or reliable, which makes them incorrect.
Question 128.
On the second post-operative day after a subtotal thyroidectomy, the client tells the nurse, “I feel numbness and my face is twitching.” What is the nurse’s best initial action?
(a) Offer mouth care.
(b) Loosen the neck dressing.
(c) Notify the physician.
(d) Document the finding as the only action.
Answer:
(c) Notify the physician.
Rationale:
Answer C is correct. The parathyroid gland can be inadvertently removed or injured with thyroid removal. This can cause hypocalcemia and symptoms of tetany, which requires notifying the physician. Answers A and B are ineffective for treating or obtaining treatment for hypocalcemia, and answer (d) would allow the condition to progress; thus, these are incorrect.
Question 129.
A client with adult respiratory distress syndrome has been placed on mechanical ventilation with PEEP. Which finding would indicate to the nurse that the client is experiencing the undesirable effect of an increase in airway and chest pressure?
(a) A PO2 of 88
(b) Rales on auscultation
(c) Blood pressure decrease to 90/48 from 120/70
(d) A decrease in spontaneous respirations
Answer:
(c) Blood pressure decrease to 90/48 from 120/70
Rationale:
Answer (c) is correct. PEEP can compress thoracic blood vessels, resulting in a decreased cardiac output and low BP. Answers (a), (b), and (d) don’t relate to PEEP and are not the result of increased thoracic pressure.
Question 130.
A nurse is teaching a group of teenagers the correct technique for applying a condom. Which point would the nurse include in the teaching plan?
(a) The condom can be reused one time.
(b) Unroll the condom all the way over the erect penis.
(c) Apply petroleum jelly to reduce irritation.
(d) Place water in the tip of the condom before use.
Answer:
(b) Unroll the condom all the way over the erect penis.
Rationale:
Answer B is correct. This is the accurate instruction for application of the condom. The condom can be used once, so answer A is incorrect. K-Y jelly and glycerin are the only solutions that can be safely used with condoms, making answer C incorrect. Answer D is incorrect because the air should be squeezed out and nothing should be in the tip of the condom before application.
Question 131.
A client with rheumatoid arthritis is being discharged with a prescription for etanercept (Enbrel). Which should the nurse teach the client to report immediately?
(a) Redness, itching, edema at injection site
(b) Exposure to chickenpox or shingles
(c) Headache
(d) Vomiting
Answer:
(b) Exposure to chickenpox or shingles
Rationale:
Answer B is correct. This information is important to report to the doctor when taking this drug. The answers in A, C, and D are side effects, but do not warrant immediate doctor notification, so they are incorrect.
Question 132.
The nurse in the ER has received report of four clients en route to the emergency department. Which client should the nurse see first? A client with:
(a) Third-degree burns to the face and neck area, with singed nasal hairs
(b) Second-degree burns to each leg and thigh area, who is alert and oriented
(c) A chemical burn that has been removed and liberally flushed before admission
(d) An electrical burn entering and leaving on the same side of the body
Answer:
(a) Third-degree burns to the face and neck area, with singed nasal hairs
Rationale:
Answer (a) is correct. Clients with face and neck burns and singed nasal hairs are more serious because of the likely respiratory and airway involvement. The clients in answers (b) and (c) are more stable. The danger of heart damage from an electrical burn occurs more often when the current enters and leaves on opposite sides of the body, which makes answer D incorrect.
Question 133.
Which clinical manifestations would the nurse expect a client with a diagnosis of acute osteomyelitis to exhibit? Select all that apply.
(a) Leukemia and normal sedimentation rate
(b) Pain and fever
(c) Low blood count
(d) Tenderness in affected area
(e) Edema and pus from the wound
Answer:
(b) Pain and fever
(d) Tenderness in affected area
(e) Edema and pus from the wound
Rationale:
Answers B, D, and E are correct. These answers are all symptoms of osteomyelitis. The answers in A and C are not associated with osteomyelitis, so they are incorrect.
Question 134.
The nurse recognizes which of the following clients as having the highest risk for pulmonary complications after surgery?
(a) A 24-year-old with open reduction internal fixation of the ulnar
(b) A 45-year-old with an open cholecystectomy
(c) A 36-year-old after a hysterectomy
(d) A 50-year-old after a lumbar laminectomy
Answer:
(b) A 45-year-old with an open cholecystectomy
Rationale:
Answer B is correct. The client with the most risk factors for pulmonary complications is the 45-year-old with an open cholecystectomy. These include abdominal surgery and prolonged bed rest. The clients in answers A, C, and D do not have as high of a risk factor, so these are incorrect.
Question 135.
Which clinical manifestation is most indicative to the nurse that a possible carbon monoxide poisoning has occurred?
(a) Pulse oximetry reading of 80%
(b) Expiratory stridor and nasal flaring
(c) Cherry red color to the mucous membranes
(d) Presence of carbonaceous particles in the sputum
Answer:
(c) Cherry red color to the mucous membranes
Rationale:
Answer (c) is correct. The hallmark symptom of carbon monoxide poisoning is the cherry red color. The answers in (a), (b), and (d) are not specific to carbon monoxide poisoning.
Question 136.
A client is admitted with a ruptured spleen following a fourwheeler accident. In preparation for surgery, the nurse suspects that the client is in the compensatory stage of shock because of which clinical manifestation?
(a) Blood pressure 120/70, confusion, heart rate 120
(b) Crackles on chest auscultation, mottled skin, lethargy
(c) Jaundice, urine output less than 30mL in the past hour, heart rate 170
(d) Rapid shallow respirations, unconscious, petechiae anterior chest
Answer:
(a) Blood pressure 120/70, confusion, heart rate 120
Rationale:
Answer (a) is correct. When a person is in the compensatory stage of shock, the BP remains within normal limits. Increased heart rate occurs, allowing cardiac output to be maintained. The client also exhibits confusion and cold, clammy skin. Answer (b) correlates with the progressive stage of shock, so it is incorrect. Answers (c) and (d) both indicate that the client is past compensation, so they are incorrect.
Question 137.
A client reports to the nurse that he believes he has an ulcer and wants to be checked for H. pylori. Which of the following medications in the client’s history would make the test invalid?
(a) Omeprazole (Prilosec)
(b) Furosemide (Lasix)
(c) Propoxyphene napsylate (Darvocet)
(d) Ibuprofen (Advil)
Answer:
(a) Omeprazole (Prilosec)
Rationale:
Answer (a) is correct. This drug would make the test read false negative. The drugs in (b), (c), and (d) do not affect H. pylori testing so they are incorrect.
Question 138.
A client arrives in the emergency room with severe burns of the hands, right arm, face, and neck. The nurse needs to start an IV. Which site would be most suitable for this client?
(a) Top of client's right hand
(b) Left antecubital fossa
(c) Top of either foot
(d) Left forearm
Answer:
(b) Left antecubital fossa
Rationale:
Answer (b) is correct. Burn clients need large veins to administer the volume of fluid necessary for fluid-replacement therapy. Answer (a) is contraindicated because of the area burned. Answer (c) is an area that is not recommended because of the possibility of deep vein thrombosis. The vein in the forearm is smaller than the antecubital; therefore, answer (d) is incorrect.
Question 139.
Which client clinical manifestation during a bone marrow transtransplantation procedure alerts the nurse to the possibility of an adverse reaction?
(a) Fever
(b) Red colored urine
(c) Hypertension
(d) Shortness of breath
Answer:
(d) Shortness of breath
Rationale:
Answer (d) is correct. Shortness of breath signifies an adverse reaction to the transplant procedure. Answers (a) and (c) can occur with the transplant process but do not signify an adverse reaction. Answer (b) is a normal finding with the bone marrow transplant.
Question 140.
The nurse is assessing the integumentary system of a darkskinned individual. Which area would be the most likely to show a skin cancer lesion?
(a) Chest
(b) Arms
(c) Face
(d) Palms
Answer:
(d) Palms
Rationale:
Answer (d) is correct. Palms of the hands and soles of the feet are areas in darkskinned clients where skin cancer is more likely to develop because of the decreased pigmentation found in these areas. Answers (a), (b), and (c) are not areas where low pigmentation occurs, so they are incorrect.
Question 141.
A client with a gastrointestinal bleed has an NG tube to low continuous wall suction. Which technique is the correct procedure for the nurse to utilize when assessing bowel sounds?
(a) Obtain a sample of the NG drainage and test the pH.
(b) Clamp the tube while listening to the abdomen with a stethoscope.
(c) Irrigate the tube with 30mL of NS while auscultating the abdomen.
(d) Turn the suction on high and auscultate over the naval area.
Answer:
(b) Clamp the tube while listening to the abdomen with a stethoscope.
Rationale:
Answer (b) is correct. It is important to clamp the tube while auscultating because the sound from the suction interferes with the auscultation process. Answer (a) is one measure used to determine whether the NG is in the stomach. Answers (c) and (d) are not the correct procedure for assessing bowel sounds, so they are incorrect.
Question 142.
A burn client’s care plan reveals an expected outcome of no localized or systemic infection. Which assessment by the nurse supports this outcome?
(a) Wound culture results showing minimal bacteria
(b) Cloudy, foul-smelling urine
(c) White blood cell count of 14,000/mm3
(d) Temperature elevation of 101 °F
Answer:
(a) Wound culture results showing minimal bacteria
Rationale:
Answer (a) is correct. A culture result that shows minimal bacteria is a favorable outcome. The answers in (b), (c), and (d) are abnormal and negative outcomes, so they are incorrect.
Question 143.
The nurse is discharging a client with a prescription of eyedrops. Which observation by the nurse would indicate a need for further client teaching?
(a) Shaking of the suspension to mix the medication
(b) Administering a second eyedrop medication immediately after the first one was instilled
(c) Washing the hands before and after the administration of the drops
(d) Holding the lower lid down without pressing the eyeball to instill the drops
Answer:
(b) Administering a second eyedrop medication immediately after the first one was instilled
Rationale:
Answer (b) is correct. The client should wait at least five minutes before instilling a second eye medication. Answers (a), (c), and (d) are correct procedures for eyedrop administration, so there is no need for further instruction with these observations.
Question 144.
The nurse is caring for a client with pneumonia who is allergic to penicillin. Which antibiotic is safest to administer to this client?
(a) Cefazolin (Ancef)
(b) Amoxicillin
(c) Erythrocin (Erythromycin)
(d) Ceftriaxone (Rocephin)
Answer:
(c) Erythrocin (Erythromycin)
Rationale:
Answer (c) is correct. Erythromycin is the only drug listed that is not penicillin based. Answers (a), (b), and (d) are in the same family as penicillin, so they are not as safe to administer; this makes them incorrect.
Question 145.
The nurse notes the following laboratory test results on a 24-hour post-burn client. Which abnormality should be reported to the physician immediately?
(a) Potassium 7.5mEq/L
(b) Sodium 131 mEq/L
(c) Arterial pH 7.34
(d) Hematocrit 52%
Answer:
(a) Potassium 7.5mEq/L
Rationale:
Answer (a) is correct. A normal potassium level is 3.5-5.0. Severe life-threatening complications can occur with hyperkalemia, requiring physician notification of any abnormality. Answers (b), (c), and (d) are normal results, making them incorrect.
Question 146.
The nurse is observing a student nurse administering ear drops to a two-year-old. Which observation by the nurse would indicate correct technique?
(a) Holds the child’s head up and extended
(b) Places the head in chin-tuck position
(c) Pulls the pinna down and back
(d) Irrigates the ear before administering medication
Answer:
(c) Pulls the pinna down and back
Rationale:
Answer C is correct. Pulling the pinna down and back is correct for administering ear drops to a child because a child’s ear canal is short and straight. The pinna is pulled up and back for adults. Answers A and B are improper techniques that would make it harder for the drops to be administered. Answer D would be incorrect because this is not a necessary part of the administration of ear drops, even though irrigation might be done to cleanse the ear before assessment.
Question 147.
The nurse is caring for a client with scalding burns across the face, neck, upper half of the anterior chest, and entire right arm. Using the rule of nines, estimate the percentage of body burned
(a) 18%
(b) 23%
(c) 32%
(d) 36%
Answer:
(b) 23%
Rationale:
Answer B is correct. The picture that follows depicts the percentages for each body part according to the Rule of Nines.
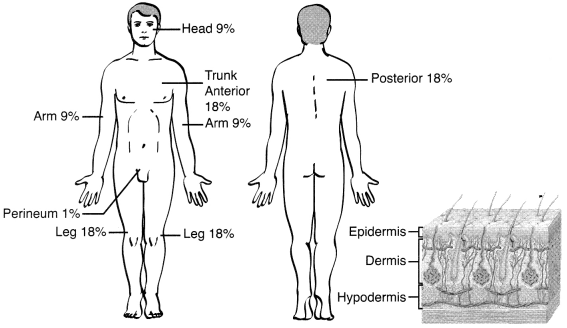
The percentages in Figure 5.1 total 100% of the body surface area. The burned areas in the question are 4.5%, 9%, and 9% equal to 22.5%, with the closest estimate at 23%. The answers in (a), (c), and (d) are not correctly calculated sums of the burned areas.
Question 148.
The nurse caring for a client in shock recognizes that the glomerular filtration rate of the kidneys will fail if the client’s mean arterial pressure falls below which of the following levels?
(a) 140
(b) 120
(c) 100
(d) 80
Answer:
(d) 80
Rationale:
Answer (d) is correct. Acute renal failure can occur with a lack of functioning in filtration when the MAP drops below 80. The mean arterial pressures in answers (a), (b), and (c) allow for proper functioning of the kidneys, which makes them incorrect.
Question 149.
The nurse is caring for a child with a diagnosis of possible hydro-cephalus. Which assessment data on the admission history would be the most objective?
(a) Anorexia
(b) Vomiting
(c) Head measurement
(d) Temperature reading
Answer:
(c) Head measurement
Rationale:
Answer (c) is correct. An increase in head growth is used as a diagnostic gauge for hydrocephalus. Answers (a) and (b) can also occur with hydrocephalus, but they are not as specific or diagnostic as head circumference. Answer (d) is not related to hydrocephalus, so it is incorrect.
Question 150.
A client is admitted after a motor vehicle accident. Based on the following results, what physician’s prescription will the nurse anticipate?
table
(a) Blood transfusion
(b) Potassium IVPB
(c) Mechanical ventilator
(d)Platelet transfusion
Answer:
(c) Mechanical ventilator
Rationale:
Answer C is correct. The arterial blood gases are abnormal indicating respiratory collapse with acidosis, making mechanical ventilation necessary. The Hgb, Hct, potassium, and platelets are all normal, making A, B, and D incorrect options.
Question 151.
The nurse is caring for a client after a burn. Which assessment finding best indicates that the client’s respiratory efforts are currently adequate?
(a) The client is able to talk.
(b) The client is alert and oriented.
(c) The client’s O2 saturation is 97%.
(d) The client’s chest movements are uninhibited
Answer:
(c) The client’s O2 saturation is 97%.
Rationale:
Answer C is correct. Oxygen saturation is the best indicator of respiratory status because it is more objective. Answers A, B, and D are subjective and nonspecific, so they are incorrect.
Question 152.
The nurse is performing discharge teaching to the parents of a seven-year-old who has been diagnosed with asthma. Which sports activity would be most appropriate for this client?
(a) Baseball
(b) Swimming
(c) Football
(d) Track
Answer:
(b) Swimming
Rationale:
Answer (b) is correct. Because of the moisturized air inhaled with swimming, it is an ideal sport for children with respiratory conditions. Answers (a), (c), and (d) can trigger an attack with asthma and would not be recommended.
Question 153.
The leukemic client is prescribed a low-bacteria diet. Which does the nurse expect to be included in this diet?
(a) Cooked spinach and sauteed celery
(b) Lettuce and alfalfa sprouts
(c) Fresh strawberries and whipped cream
(d) Raw cauliflower or broccoli
Answer:
(a) Cooked spinach and sauteed celery
Rationale:
Answer (a) is correct. Clients requiring low-bacteria foods cannot have raw fruits and vegetables. These types of foods must be cooked. Answers (b), (c), and (d) are raw fruits and vegetables, so they are incorrect.
Question 154.
A child is to receive heparin sodium five units per kilogram of body weight by subcutaneous route every four hours. The child weighs 52.8 lb. How many units should the child receive in a 24- hour period?
(a) 300
(b) 480
(c) 720
(d) 960
Answer:
(c) 720
Rationale:
Answer (c) is correct. The child weighs 24kg and should receive 5 units/kg, or 120 units every four hours. This would be 720 units in 24 hours. The answers in (a), (b), and (d) are incorrect dosages.
Question 155.
A client with cancer is experiencing a common side effect of chemotherapy administration. Which laboratory assessment finding would cause the most concern?
(a) A sodium level of 50mg/dL
(b) A blood glucose of 110mg/dL
(c) A platelet count of 100,000/mm3
(d) A white cell count of 5,000/mm3
Answer:
(a) A sodium level of 50mg/dL
Rationale:
Answer A is correct. Hyponatremia can result from anorexia and nausea and vomiting caused by chemotherapy drugs. Normal sodium is 135-145mEq, so 50mg/dL is a low blood level that should be reported. Answers B, C, and D are normal or near-normal readings, so they are incorrect.
Question 156.
A client’s admission history reveals complaints of fatigue, chronic sore throat, and enlarged lymph nodes in the axilla and neck. Which exam would assist the physician to make a tentative diagnosis of leukemia?
(a) A complete blood count
(b) An x-ray of the chest
(c) A bone marrow aspiration
(d) A CT scan of the abdomen
Answer:
(a) A complete blood count
Rationale:
Answer (a) is correct. CBC results would indicate an elevated WBC count with leukemia. Answers (b) and (d) would not assist with the diagnosis, and answer (c) would be utilized to confirm leukemia; thus, they are incorrect.
Question 157.
A client is admitted with symptoms of vertigo and syncope. Diagnostic tests indicate left subclavian artery obstruction. What additional findings would the nurse expect?
(a) Memory loss and disorientation
(b) Numbness in the face, mouth, and tongue
(c) Radial pulse differences over 10bpm
(d) Frontal headache with associated nausea or emesis
Answer:
(c) Radial pulse differences over 10bpm
Rationale:
Answer (c) is correct. Radial pulse differences over 10bpm are findings that relate to the location of the subclavian artery. Obstruction of the artery would also show a decrease in radial heart rate on the side of the obstruction. Answers (a), (b), and (d) are related to neurological problems as deficits, which makes them incorrect.
Question 158.
The nurse is performing discharge teaching on a client at high risk for the development of skin cancer. Which instruction should be included in the client teaching?
(a) “You should see the doctor every six months.”
(b) “Sunbathing should be done between the hours of noon and 3 p.m.”
(c) “If you have a mole, it should be removed and biop- sied.”
(d) “You should wear sunscreen when going outside.”
Answer:
(d) “You should wear sunscreen when going outside.”
Rationale:
Answer (d) is correct. Everyone should wear sunscreen when going outside, to protect them from ultraviolet exposure. Answer (a) is not necessary. Answer (b) is the period of day when the sun’s rays are most detrimental to the skin. Answer (c) is incorrect because only moles that are suspicious require removal and biopsy.
Question 159.
A client with pancreatitis has been transferred to the intensive care unit. The nurse assesses a pulmonary arterial wedge pressure (PAWP) of 14mmHg. Based on this finding, the nurse would want to further assess for what additional correlating wedge pressure data?
(a) A drop in blood pressure
(b) Rales on chest auscultation
(c) A temperature elevation
(d) Dry mucous membranes
Answer:
(b) Rales on chest auscultation
Rationale:
Answer (b) is correct. Normal pulmonary arterial wedge pressure is 4-12. This reading is elevated, indicating hypervolemia. The nurse should further assess for other indications of volume excess. Answers (a) and (d) correlate with hypovolemia. Answer (c) does not relate to the wedge pressure result.
Question 160.
The nurse is caring for a client with a diagnosis of hepatitis who is experiencing pruritis. Which would be the most appropriate nursing intervention?
(a) Suggest that the client take warm showers.
(b) Add baby oil to the client’s bath water.
(c) Apply powder to the client’s skin.
(d) Suggest a hot-water rinse after bathing.
Answer:
(b) Add baby oil to the client’s bath water.
Rationale:
Answer B is correct. Applying baby oil could help soothe the itchy skin. Answers A, C, and D would increase dryness and worsen the itching.
Question 161.
The school nurse assessed and referred a 14-year-old with scoliosis. An 18° curvature of the spine was diagnosed. Which treatment plan would the nurse expect?
(a) Application of a Milwaukee brace
(b) Electrical stimulation to the outward side of the curve
(c) Re-evaluation, with no treatment at this time
(d) Surgical realignment of the spine
Answer:
(c) Re-evaluation, with no treatment at this time
Rationale:
Answer (c) is correct. If a client has a curvature of less than 20°, it is considered mild, with no treatment required. If after re-evaluation the curve is progressing, treatment might be necessary. Answers (a) and (b) are done with curvatures of more than 20°, so they are incorrect. Answer (d) might be required with curvatures greater than 40°, making it incorrect.
Question 162.
The physician has ordered a homocysteine blood level on a client.
The nurse recognizes that the results will be increased in a client
with a deficiency in which of the following:
(a) Vitamin B12
(b) Vitamin C
(c) Vitamin A
(d) Vitamin E
Answer:
(a) Vitamin B12
Rationale:
Answer (a) is correct. Homocysteine levels are increased when a client has B12 deficiency. The answers in (b), (c), and (d) are incorrect because homocysteine levels are not increased by these disorders.
Question 163.
The registered nurse is assigning staff for four clients on the 3-11 shift. Which client should be assigned to the LPN?
(a) A client with a diagnosis of adult respiratory distress syndrome (ARDS) who was transferred from the critical care unit at 1400
(b) A one-hour post-operative colon resection
(c) A client with pneumonia expecting discharge in the morning
(d) A client with cirrhosis of the liver experiencing bleeding from esophageal varices
Answer:
(c) A client with pneumonia expecting discharge in the morning
Rationale:
Answer (c) is correct. The pneumonia client is the most stable of the four. The clients in answers (a) and (b) are recent arrivals to the unit, indicating extensive assessments. The client in answer (d) is in danger of fluid volume deficit, requiring RN interventions.
Question 164.
A client with multiple sclerosis has an order to receive Solu Medrol 200mg IV push. The available dose is Solu Medrol 250mg per mL. How much medication will the nurse administer?
(a) 0.5 mL
(b) 0.8 mL
(c) 1.1 mL
(d) 1.4 mL
Answer:
(b) 0.8 mL
Rationale:
Answer (b) is correct. The calculated dosage is 0.8mL. Answers (a), (c), and (d) are inaccurate dosages for the amount of medication ordered, making them incorrect.
Question 165.
The nurse is obtaining a history on a 74-year-old client. Which statement made by the client would most alert the nurse to a pos
sible fluid and electrolyte imbalance?
(a) “My skin is always so dry.”
(b) 1 often use a laxative for constipation.”
(c) “I have always liked to drink a lot of water.”
(d) “I sometimes have a problem with dribbling urine.”
Answer:
(b) 1 often use a laxative for constipation.”
Rationale:
Answer (b) is correct. The misuse and overuse of laxatives can cause serious fluid and electrolyte imbalances in the elderly. Answers (a) and (d) can be normal occurrences associated with the physiological changes of aging. Answer (c) is an incorrect response because the client states that increased fluid intake is not a new occurrence.
Question 166.
The nurse is caring for a client in the acute care unit. Initial labora tory values reveal serum sodium of l56mEq/L. What behavior
changes would the nurse expect the client to exhibit?
(a) Hyporetlexia
(b) Manic behavior
(c) Depression
(d) Muscle cramps
Answer:
(b) Manic behavior
Rationale:
Answer (b) is correct. The normal sodium level is 135-145mEq/L. When hypernatremia occurs, the client can exhibit manic and hyperactivity behaviors. Other symptoms of increased sodium include restlessness, twitching, seizures, and hyperreflexia. Answers (a), (c), and (d) are not symptoms of high sodium levels. Answer (d) is associated with low sodium levels.
Question 167.
The nurse is completing the preoperative checklist on a client scheduled for surgery and finds that the consent form has been signed, but the client is unclear about the surgery and possible complications. Which is the most appropriate action?
(a) Call the surgeon and ask him to come see the client to clarify the information.
(b) Explain the procedure and complications to the client.
(c) Check in the physician’s progress notes to see if understanding has been documented.
(d) Check with the client’s family to see if they understand the procedure fully.
Answer:
(b) Explain the procedure and complications to the client.
Rationale:
Answer A is correct. It is not a nursing responsibility to give detailed information about surgical procedures. The nurse can reinforce, but if the nurse feels that the client is not adequately informed, she can serve as an advocate and request that the surgeon visit the client to explain the procedure. Answer (b) is not the role of the nurse, so this is incorrect. Answers (c) and (d) are not appropriate and will not help in increasing or verifying patient understanding.
Question 168.
When preparing a client for admission to the surgical suite, the nurse recognizes that which one of the following items is most important to remove before sending the client to surgery?
(a) Hearing aid
(b) Contact lenses
(c) Wedding ring
(d) Dentures
Answer:
(a) Hearing aid
Rationale:
Answer (d) is correct. Safety and prevention of aspiration is the first priority. Answers (a), (b), and (c) would not be priority removals, so they are incorrect.
Question 169.
A client with cancer is to undergo a bone scan. The nurse should perform which of the following actions?
(a) Force fluids 24 hours before the procedure is scheduled to begin.
(b) Ask the client to void immediately before the study.
(c) Hold medication that affects the central nervous system for 12 hours pre- and post-test.
(d) Cover the client’s reproductive organs with an x-ray shield during the procedure.
Answer:
(d) Cover the client’s reproductive organs with an x-ray shield during the procedure.
Rationale:
Answer B is correct. The client is asked to void before the procedure to prevent blurring of the pelvic bones. Answer A is incorrect because, although the client does need fluids to distribute and eliminate the isotope, this is not necessary 24 hours before the procedure. Answers C and D are not appropriate actions for the bone scan exam.
Question 170.
A client with suspected leukemia is to undergo a bone marrow aspiration. The nurse plans to include which statement in the teaching session?
(a) “You will be lying on your abdomen for the examination procedure.”
(b) “Portions of the procedure will cause pain or discomfort.”
(c) “You will be given some medication to cause amnesia of the test.”
(d) “You will not be able to drink fluids for 24 hours before the study.”
Answer:
(b) “Portions of the procedure will cause pain or discomfort.”
Rationale:
Answer B is correct. There will be a sensation of pulling during the aspiration. This feeling is painful. Answer A is incorrect because the position is inappropriate for bone marrow aspiration. Answer D is not a required preprocedure diet change. Although the client might receive a local anesthetic and/or pain medication, amnesic medications such as Versed are not usually administered, so answer (c) is incorrect.
Question 171.
The nurse is caring for a client scheduled for a surgical repair of an abdominal aortic aneurysm. Which assessment is most crucial during the preoperative period?
(a) Assessment of the client’s level of anxiety
(b) Evaluation of the client’s exercise tolerance
(c) Identification of peripheral pulses
(d) Assessment of bowel sounds and activity
Answer:
(b) Evaluation of the client’s exercise tolerance
Rationale:
Answer (c) is correct. It is most important to identify the pulses pre-operatively to have a baseline for post-operative evaluation. The answers in (a), (b), and (d) are not priorities for the client pre-operatively.
Question 172.
The nurse should carefully monitor the client for which common dysrhythmia that can occur during suctioning?
(a) Bradycardia
(b) Tachycardia
(c) Ventricular ectopic beats
(d) Sick sinus syndrome
Answer:
(a) Bradycardia
Rationale:
Answer (a) is correct. Excessive vagal stimulation causes bradycardia because of parasympathetic stimulation. Answers (b), (c), and (d) are not common arrhythmias associated with suctioning, so they are incorrect.
Question 173.
The nurse is performing discharge instruction for a client with an implantable permanent pacemaker. What discharge instruction is an essential part of the plan?
(a) “You cannot eat food prepared in a microwave.”
(b) “You should avoid moving the shoulder on the side of the pacemaker site for six weeks.”
(c) “You will have to learn to take your own pulse.”
(d) “You will not be able to fly on a commercial airliner with the pacemaker in place.”
Answer:
(c) “You will have to learn to take your own pulse.”
Rationale:
Answer (c) is correct. The client must be able to check the heart rate and report any rate that differs from the preset rate. Answers (a) and (d) are not required or have no effect on the pacemaker. Answer (b) would be contraindicated because the lack of movement could cause an inability to move the shoulder.
Question 174.
The nurse is completing admission on a client with possible esophageal cancer. Which finding would not be common for this diagnosis?
(a) Foul breath
(b) Dysphagia
(c) Diarrhea
(d) Chronic hiccups
Answer:
(c) Diarrhea
Rationale:
Answer (c) is correct. Diarrhea is not associated with esophageal cancer. Answers (a), (b), and (d) are clinical manifestations of esophageal cancer, so they are incorrect. The nurse would also assess for weight loss, regurgitation, and vomiting associated with esophageal cancer.
Question 175.
A client arrives from surgery following an abdominal perineal resection with a permanent ileostomy. What should be the priority nursing care during the post-op period?
(a) Teaching how to irrigate the ileostomy
(b) Stopping electrolyte loss through the stoma
(c) Encouraging a high-fiber diet
(d) Facilitating perineal wound drainage
Answer:
(d) Facilitating perineal wound drainage
Rationale:
Answer I is correct. Perineal wound drainage is important to prevent abscess formation and infection. Answer (a) is incorrect because ileostomies produce liquid stools and do not require irrigation. Answer (b) cannot be done, and answer (c) would be inappropriate.
Question 176.
The nurse is making initial rounds on a client with a C5 fracture. The client is in a halo vest and is receiving O2 at 40% via mask to a tracheostomy. Assessment reveals a respiratory rate of 40 and O2 saturation of 88. The client is restless. Which initial nursing action is most indicated?
(a) Notifying the physician
(b) Performing tracheal suctioning
(c) Repositioning the client to the left side
(d) Rechecking the client’s O2 saturation
Answer:
(b) Performing tracheal suctioning
Rationale:
Answer (b) is correct. The client could have a mucus plug, so tracheal suctioning is the initial action most indicated. If suctioning doesn’t work, notifying the doctor, as in answer (a), is the next appropriate action. Answer (c) would not help, and answer (d) would be appropriate after the suctioning is done, to see if there has been any improvement.
Question 177.
A client has just finished her lunch, consisting of shrimp with rice, fruit salad, and a roll. The client calls for the nurse, stating, “My throat feels thick and I’m having trouble breathing.” What action should the nurse implement first?
(a) Place the bed in Trendelenburg position and call the physician.
(b) Take the client’s vital signs and administer Benadryl 50mg PO.
(c) Place the bed in high Fowler's position and call the physician.
(d) Start an Aminophylline drip and call the physician.
Answer:
(c) Place the bed in high Fowler's position and call the physician.
Rationale:
Answer (c) is correct. High Fowler’s is the best position for facilitating breathing. The nurse would suspect an allergic reaction to the shrimp. Answers (b) and D would both require an order from the physician. Answer A would worsen the client’s respiratory efforts, so it is incorrect.
Question 178.
The nurse is caring for a client with cirrhosis of the liver. Which is the best method to use for determining that the client has ascites?
(a) Inspection of the abdomen for enlargement
(b) Bimanual palpation for hepatomegaly
(c) Daily measurement of abdominal girth
(d) Assessment for a fluid wave
Answer:
(c) Daily measurement of abdominal girth
Rationale:
Answer C is correct. A measurement that reveals a numerical value would be the most accurate to detect changes in the size of the abdomen. Answers A, B, and D are less objective, so they are incorrect.
Question 179.
A client arrives in the emergency room after a motor vehicle accident. Witnesses tell the nurse that they observed the client’s head hit the side of the car door. Nursing assessment findings include BP 70/34, heart rate 130, and respirations 22. Based on the information provided, which is the priority nursing care focus?
(a) Brain tissue perfusion
(b) Regaining fluid volume
(c) Clearance of the client's airway
(d) Measures to increase sensation
Answer:
(b) Regaining fluid volume
Rationale:
Answer (b) is correct. The stem gives objective assessment data that indicates a fluid volume deficit, a low BP with an elevated heart rate. Answer (a) is incorrect because of the lack of objective information that supports this as a problem. Answers (c) and (d) have no supportive data, so they are incorrect.
Question 180.
The home health nurse is visiting a 30-year-old with sickle cell disease. Assessment findings include spleenomegaly. What information obtained on the visit would cause the most concern? The client:
(a) Eats fast food daily for lunch
(b) Drinks a beer occasionally
(c) Sometimes feels fatigued
(d) Works as a furniture mover
Answer:
(d) Works as a furniture mover
Rationale:
Answer D is correct. A client with an enlarged spleen has an increased risk for rupture; therefore, heavy lifting is contraindicated. Answers A, B, and C are not a cause for concern with an enlarged spleen.
Question 181.
The nurse on the oncology unit is caring for a client with a WBC of 1500/mm3. During evening visitation, a visitor brings in a fruit basket. What action should the nurse take?
(a) Encourage the client to eat small snacks of the fruit.
(b) Remove fruits that are not high in vitamin C.
(c) Instruct the client to avoid the high-fiber fruits.
(d) Remove the fruits from the client’s room.
Answer:
(d) Remove the fruits from the client’s room.
Rationale:
Answer (d) is correct. A client who is immuno-suppressed is not allowed fresh fruit. Answers (a), (b), and (c) would still allow the client to eat raw fruit, which makes them incorrect.
Question 182.
The nurse is giving an end-of-shift report when a client with a chest tube is noted in the hallway with the tube disconnected. What is the most appropriate action?
(a) Clamp the chest tube immediately.
(b) Put the end of the chest tube into a cup of sterile normal saline.
(c) Assist the client back to the room and place him on his left side.
(d) Reconnect the chest tube to the chest tube system.
Answer:
(b) Put the end of the chest tube into a cup of sterile normal saline.
Rationale:
Answer (b) is correct. The nurse must provide a water seal. Answer (a) could cause a tension pneumothorax if the client had no escape for the air. Answer (c) serves no purpose, and answer (d) would not allow maintenance of a sterile system.
Question 183.
A client with deep vein thrombosis is receiving a continuous heparin infusion and Coumadin PO. INR lab test result is 8.0. Which intervention would be most important to include in the nursing care plan?
(a) Assess for signs of abnormal bleeding.
(b) Anticipate an increase in the heparin drip rate.
(c) Instruct the client regarding the drug therapy.
(d) Increase the frequency of vascular assessments.
Answer:
(a) Assess for signs of abnormal bleeding.
Rationale:
Answer (a) is correct. An INR greater than 6.0 could result in spontaneous bleeding, so this would be a priority. Answers (b), (c), and (d) are not associated with the high INR result, so they are incorrect.
Question 184.
Which breakfast selection by a client with osteoporosis indicates that the client understands the dietary management of the disease?
(a) Scrambled eggs, toast, and coffee
(b) Bran muffin with margarine
(c) Granola bar and half of a grapefruit
(d) Bagel with jam and skim milk
Answer:
(d) Bagel with jam and skim milk
Rationale:
Answer (d) is correct. The highest calcium level is in the bagel with jam and skim milk. The client also needs to know that calcium in combination with high fiber and caffeine decreases the absorption; therefore, answers (a), (b), and (c) are incorrect.
Question 185.
A client with hepatitis C who has cirrhosis changes has just returned from a liver biopsy. The nurse will place the client in which position?
(a) Trendelenburg
(b) Supine
(c) Right side-lying
(d) Left Sim’s
Answer:
(c) Right side-lying
Rationale:
Answer (c) is correct. Hemorrhage can occur with liver biopsies. The client is positioned on the right side to keep pressure on the area and prevent bleeding. Answers (a), (b), and (d) are not correct positions because of the location of the liver.
Question 186.
The nurse is caring for a client who was admitted to the burn unit four hours after the injury with second-degree burns to the trunk and head. Which finding would the nurse least expect to find during this time period?
(a) Hypovolemia
(b) Laryngeal edema
(c) Hypernatremia
(d) Hyperkalemia
Answer:
(c) Hypernatremia
Rationale:
Answer (c) is correct. Hypernatremia is not an expected finding because hyponatremia is the likely occurrence when sodium moves out of the cell during the “fluid shift” phase of burn injury. The answers in (a), (b), and (d) are more of a priority for this client, which makes them incorrect.
Question 187.
The nurse is evaluating nutritional outcomes for a client with anorexia nervosa. Which one of the following is the most objective favorable outcome for the client?
(a) The client eats all the food on her tray.
(b) The client requests that family bring special foods.
(c) The client’s weight has increased.
(d) The client weighs herself each morning.
Answer:
(c) The client’s weight has increased.
Rationale:
Answer (c) is correct. Increased weight is the most objective answer. Answers (a), (b), and (d) also show favorable outcomes of anorexia nervosa but are not as objective, making them incorrect.
Question 188.
The client who is two weeks post-burn with a 40% deep partialthickness injury still has open wounds. The nurse’s assessment reveals the following findings: temperature 96.5°F, BP 87/40, and severe diarrhea stools. What problem does the nurse most likely suspect?
(a) Findings are normal, not suspicious of a problem
(b) Systemic gram positive infection
(c) Systemic gram negative infection
(d) Systemic fungal infection
Answer:
(c) Systemic gram negative infection
Rationale:
Answer (c) is correct. Gram negative infection invasion reveals clinical manifestations of severe diarrhea, hypothermia, and hypotension. Answer (a) is incorrect because the symptoms are abnormal. The infections identified in answers (b) and (d) are not consistent with the clinical manifestations identified in the question, so they are incorrect.
Question 189.
The nurse assesses a new order for a blood transfusion. The order is to transfuse one unit of packed red blood cells (contains 250mL) in a two-hour period. What will be the hourly rate of infusion?
(a) 50mL/hr
(b) 62mL/hr
(c) 125mL/hr
(d) 137mL/hr
Answer:
(c) 125mL/hr
Rationale:
Answer (c) is correct. A 250mL infusion of packed cells to infuse over two hours is calculated by 250 divided by 2 = 125mL/hr. The answers in (a), (b), and (d) are incorrect calculations for infusion of the blood in two hours.
Question 190.
A client has signs of increased intracranial pressure. Which one of the following is an early indicator of deterioration in the client’s condition?
(a) Widening pulse pressure
(b) Decrease in the pulse rate
(c) Dilated, fixed pupils
(d) Decrease in level of consciousness
Answer:
(d) Decrease in level of consciousness
Rationale:
Answer (d) is correct. The nurse observes for sluggishness or lethargy, for early indications of increased ICP. A change in vital signs and papillary changes, as in answers (a), (b), and C, are late signs of increased ICP.
Question 191.
Which of the following statements by a client with a seizure disorder who is taking topiramate (Topamax) indicates that the client has understood the nurse’s instruction?
(a) “I will take the medicine before going to bed."
(b) “I will drink 8 to 10 ten-ounce glasses of water a day.”
(c) "I will eat plenty of fresh fruits.”
(d) “I must take the medicine with a meal or snack.”
Answer:
(b) “I will drink 8 to 10 ten-ounce glasses of water a day.”
Rationale:
Answer (b) is correct. There is an increased risk for kidney stones with the use of topi- ramate (Topamax), so fluids are an important part of problem prevention. The drug is administered without regard to food and is not an hour-of-sleep medication, making answers (a) and (d) incorrect. Answer (c) is not required with the use of this medication.
Question 192.
A client with terminal lung cancer is admitted to the unit. A family member asks the nurse, “How much longer will it be?” Which response by the nurse is most appropriate?
(a) “This must be a terrible situation for you.”
(b) “I don’t know. I’ll call the doctor.”
(c) “I cannot say exactly. What are your concerns at this time?”
(d) “Don’t worry, from the way things look it will be very soon.”
Answer:
(c) “I cannot say exactly. What are your concerns at this time?”
Rationale:
Answer (c) is correct. The nurse responds appropriately by answering the question honestly and attempting to assess for more information, allowing the person to ventilate feelings. Answer (a) is an appropriate response but not as appropriate as answer (c). Answers (b) and (d) are nontherapeutic communication techniques.
Question 193.
A client with a history of colon cancer is admitted to the oncology unit. Laboratory results reveal a WBC of 1600/mm3. What plans will the nurse add to the care plan because of the WBC reading? Select all that apply.
(a) No sick visitors
(b) Private room necessary
(c) No Aspirin products
(d) Low bacteria diet
(e) Electric razors only
Answer:
(a) No sick visitors
(b) Private room necessary
(d) Low bacteria diet
Rationale:
Answers (a), (b), and (d) are correct. The WBC count is below normal making the client at risk for infection. The correct answers decrease a clients’ risk of infection. Answers (c) and (e) are related to platelet counts and a risk for bleeding, so they are incorrect.
Question 194.
The nurse is caring for a client with a closed head injury. Fluid is
assessed leaking from the ear. What is the nurse’s first action?
(a) Irrigate the ear canal gently.
(b) Notify the physician.
(c) Test the drainage for glucose.
(d) Apply an occlusive dressing.
Answer:
(c) Test the drainage for glucose.
Rationale:
Answer (c) is correct. The initial action is to test the drainage for glucose because this could indicate the presence of cerebrospinal fluid. The next action is to notify the physician, as stated in answer (b). Answers (a) and (d) are contraindicated, so they are incorrect.
Question 195.
The nurse has inserted an NG tube for enteral feedings. Which assessment result is the best indicator of the tube’s stomach placement?
(a) Aspiration of tan-colored mucus
(b) Green aspirate with a pH of 3
(c) A swish auscultated with the injection of air
(d) Bubbling noted when the end of the tube is placed in liquid
Answer:
(b) Green aspirate with a pH of 3
Rationale:
Answer (b) is correct. The aspirate of gastric content should be green, brown, clear, or colorless, with a gastric pH of between 1 and 5. Answer (a) would likely be from the lungs, so it is incorrect. Answers (c) and (d) are not as accurate as color and pH for confirming gastric location, so they are incorrect.
Question 196.
The nurse would identify which one of the following assessment findings as a normal response in a craniotomy client post-operatively?
(a) A decrease in responsiveness the third post-op day
(b) Sluggish pupil reaction the first 24-48 hours
(c) Dressing changes three to four times a day for the first three days
(d) Temperature range of 98.8°F to 99.6°F the first 2-3 days
Answer:
(d) Temperature range of 98.8°F to 99.6°F the first 2-3 days
Rationale:
Answer (d) is correct. A slight elevation in temperature would be expected from surgical intervention and would not be a cause for concern. Answers (a), (b), and (c) could indicate a progressing complication, so they are incorrect.
Question 197.
A client with alcoholism has been instructed to increase his intake of thiamine. The nurse knows the client understands the instructions when he selects which food?
(a) Roast beef
(b) Broiled fish
(c) Baked chicken
(d) Sliced pork
Answer:
(d) Sliced pork
Rationale:
Answer (d) is correct. Pork has more thiamine than beef, fish, or chicken, which makes answers (a), (b), and (c) incorrect.
Question 198.
The nurse is caring for a client who abuses narcotics. The client is exhibiting a respiratory rate of 10 and dilated pupils. Which drug would the nurse expect to administer?
(a) Meperidine (Demerol)
(b) Naloxone (Narcan)
(c) Chlordiazepoxide (Librium)
(d) Haloperidol (Haldol)
Answer:
(b) Naloxone (Narcan)
Rationale:
Answer (b) is correct. The client is exhibiting symptoms of respiratory depression from the use of a narcotic and requires an antagonist to reverse the effects. Answer A is a narcotic that would increase the negative effects the client is experiencing. Answers (c) and (d) are antianxiety and antipsychotic drugs, not narcotic-reversal agents.
Question 199.
A client has a CVP monitor in place via a central line. Which would be included in the nursing care plan for this client?
(a) Notify the physician of readings less than 3cm or more than 8cm of water.
(b) Use the clean technique to change the dressing at the insertion site.
(c) Elevate the head of the bed to 90° to obtain CVP readings.
(d) The 0 mark on the manometer should align with the client’s right clavicle for the readings.
Answer:
(a) Notify the physician of readings less than 3cm or more than 8cm of water.
Rationale:
Answer (a) is correct. The normal reading for central venous pressure is 3-8cm of H2O. The doctor should be notified of any abnormal readings. Answer (b) is incorrect because a sterile technique should be utilized. Answer (c) is incorrect because of the 90° angle; the angle should be supine up to 45°. The zero should align at the phlebo- static axis, fourth intercostals space midaxillary, instead of the right clavicle, so answer (d) is incorrect.
Question 200.
A client is admitted to the chemical dependency unit for poly-drug abuse. The client states, “I don’t know why you are all so worried; I am in control. I don’t have a problem.” Which defense mechanism is being utilized?
(a) Rationalization
(b) Projection
(c) Dissociation
(d) Denial
Answer:
(d) Denial
Rationale:
Answer (d) is correct. The statement in answer (d) reflects the use of denial as a means of coping with the illness. Answers (a), (b), and (c) are defense mechanisms not reflected by the statement, so they are incorrect.
Question 201.
A client scheduled for a carotid endarterectomy requires insertion of an intra-arterial blood pressure-monitoring device. The nurse plans to perform the Allen test. Which observation indicates patency of the ulnar artery?
(a) Blanching of the hand on compression and release of the ulnar artery
(b) Muscular twitching of the bicep muscle with use of a tourniquet at the wrist
(c) Hand turning pink after the nurse releases the pressure on the ulnar artery
(d) Flexion of the wrist when tapping the ulnar artery with a reflex hammer
Answer:
(c) Hand turning pink after the nurse releases the pressure on the ulnar artery
Rationale:
Answer (c) is correct. The Allen test is performed by having the client make a fist while the radial and ulnar arteries are compressed. When the hand blanches, the client is asked to release the fist while the nurse maintains pressure on the radial artery. Patency is indicated by the hand turning pink. Answers (a), (b), and (d) are incorrect for the Allen test procedure.
Question 202.
A client’s chest tube drainage device has continuous bubbling in the water seal chamber. What is the nurse checking for when she clamps different areas of the tube to find out where the bubbling stops?
(a) An air leak in the system
(b) The suction being too high
(c) The suction being too low
(d) A tension pneumothorax
Answer:
(a) An air leak in the system
Rationale:
Answer (a) is correct. Clamping various areas of the tube allows the nurse to assess for a leak in the tubing. When the bubbling stops, the leak has been located. Answers (b) and (c) are assessed by reading the suction gauge and observing the bubbling in the suction-control chamber. Answer (d) is a diagnosis confirmed by client symptoms and x-ray not related to the chest tube system.
Question 203.
The nurse should be particularly alert for which one of the following problems in a client with barbiturate overdose?
(a) Oliguria
(b) Cardiac tamponade
(c) Apnea
(d) Hemorrhage
Answer:
(c) Apnea
Rationale:
Answer (c) is correct. Respiratory depression is a sign of overdose. Other symptoms of overdose include seizures, shock, coma, and cardiovascular collapse. Answers (a), (b), and (d) lack any symptoms of overdose, so they are incorrect.
Question 204.
A client taking the drug disulfiram (Antabuse) is admitted to the ER. Which clinical manifestations are most indicative of recent alcohol ingestion?
(a) Vomiting, heart rate 120, chest pain
(b) Nausea, mild headache, bradycardia
(c) Respirations 16, heart rate 62, diarrhea
(d) Temp 101 °F, tachycardia, respirations 20
Answer:
(a) Vomiting, heart rate 120, chest pain
Rationale:
Answer A is correct. Vomiting, a heart rate of 120, and chest pain are symptoms of drinking alcohol while taking Antabuse. Additional symptoms include severe headache, nausea, cardiac collapse, respiratory collapse, convulsions, and death. Answers (b), (c), and (d) contain incomplete or inaccurate clinical signs of the combination of alcohol and Antabuse.
Question 205.
A client with cancer and metastasis to the bone is admitted to the hospital. Which symptom of hypercalcemia causes the nurse the most concern?
(a) Weakness
(b) Anorexia
(c) Flaccid muscles
(d) Cardiac changes
Answer:
(d) Cardiac changes
Rationale:
Answer (d) is correct. Clients with hypercalcemia can have dysrhythmias (heart block). This is the priority of the symptoms listed in (a), (b), and (c), so they are incorrect. Remember prioritization airway, breathing, and circulation.
Question 206.
The nurse expects that a client with cocaine addiction would most likely be placed on which medication?
(a) Amantidine (Symmetrel)
(b) Methadone
(c) THC
(d) Disulfiram (Antabuse)
Answer:
(a) Amantidine (Symmetrel)
Rationale:
Answer (a) is correct. Symmetrel is the drug used for addiction to cocaine. It is classified as an anti-Parkinsonian drug and gives clients with this addiction a substitute for the neurotransmitter dopamine. Answer (b) is used for opioid addiction. Answer (c) is marijuana and is not used for replacement therapy. Answer (d) is used for alcohol abuse.
Question 207.
The nurse is reviewing the laboratory values of a client with a myocardial infarction. Which laboratory test is used to identify injury to the myocardium and can remain elevated for up to three weeks?
(a) Total CK
(b) CK-MB
(c) Myoglobulin
(d) Troponin Tor I
Answer:
(d) Troponin Tor I
Rationale:
Answer (d) is correct. Troponin, T or I, is a protein found in the myocardium. Testing for protein is frequently used to identify an acute myocardial infarction. Answers (a), (b), and (c) return to normal in less than four days, which makes them incorrect.
Question 208.
A client with newly diagnosed epilepsy tells the nurse, “If I keep having seizures, I’m scared my husband will feel differently toward me.” Which response by the nurse would be most appropriate?
(a) “You don’t know if you’ll ever have another seizure. Why don’t you wait and see what happens?”
(b) “You seem to be concerned that there could be a change in the relationship with your husband.”
(c) “You should focus on your children. They need you.”
(d) “Let’s see how your husband reacts before getting upset.”
Answer:
(b) “You seem to be concerned that there could be a change in the relationship with your husband.”
Rationale:
Answer (b) is correct. The correct response uses the therapeutic technique of identifying the client’s feelings. Answers (a), (c), and (d) are nontherapeutic, closed statements that reflect judgment and opinions by the nurse, so they are incorrect.
Question 209.
While interviewing a client who abuses alcohol, the nurse learns that the client has experienced “blackouts.” The wife asks what this means. What is the nurse’s best response at this time?
(a) “Your husband has experienced short-term memory amnesia.”
(b) “Your husband has experienced loss of remote memory.”
(c) “Your husband has experienced a loss of consciousness.”
(d) “Your husband has experienced a fainting spell.”
Answer:
(a) “Your husband has experienced short-term memory amnesia.”
Rationale:
Answer (a) is correct. The most appropriate response is to answer the request of the client’s spouse and define blackouts. Answers (b), (c), and (d) are not accurate definitions of blackouts, so they are incorrect.
Question 210.
Which would the nurse include in the nursing care plan of a client experiencing severe delirium tremens?
(a) Placing the client in a darkened room
(b) Keeping the closet and bathroom doors closed
(c) Administering a diuretic to decrease fluid excess
(d) Checking vital signs every eight hours
Answer:
(b) Keeping the closet and bathroom doors closed
Rationale:
Answer (b) is correct. Closing the doors can prevent shadows and help with the client’s paranoia and hallucinations. A darkened room, as in answer (a), would increase the client’s anxiety. Answer (c) is an inappropriate intervention that does not usually occur with DTs, and vital signs would be assessed more frequently than in answer (d).
Question 211.
The nurse is caring for a client admitted with a diagnosis of epilepsy. The client begins to have a seizure. Which action by the nurse is contraindicated?
(a) Turning the client to the side-lying position
(b) Inserting a padded tongue blade and oral airway
(c) Loosening restrictive clothing
(d) Removing the pillow and raising padded side rails
Answer:
(b) Inserting a padded tongue blade and oral airway
Rationale:
Answer (b) is correct. Nothing should be put in the mouth of a client during a seizure. Answers (a), (c), and (d) are important nursing interventions to maintain a patent airway and prevent injury during a seizure, so they are incorrect.
Question 212.
A client has been placed on the drug valproic acid (Depakene). Which would indicate to the nurse that the client is experiencing an adverse reaction to this medication?
(a) Photophobia
(b) Poor skin turgor
(c) Lethargy
(d) Reported visual disturbances
Answer:
(c) Lethargy
Rationale:
Answer (c) is correct. Lethargy could indicate hepatatoxicity. The nurse should also observe for jaundice, nausea and vomiting, anorexia, facial edema, and unusual bleeding or bruising. Answers (a), (b), and (d) are not clinical manifestations of adverse effects of the drug Depakene.
Question 213.
A client has an order for vancomycin (Vancocin) 1 gram IVPB in 250 mL normal saline to infuse over 60 minutes. The nurse would set the IV drop rate to deliver how many drops per minute if the IV set delivers 15gtts/mL? Fill in the blank Gtts/m i n ute
Answer:
63gtts/minute
Rationale:
63 gtts/minute is correct:
\(\frac { 250mL x 15gtts/mL }{ 60 min }\) = \(\frac { 3750 }{ 60 }\) = 62.5 or 63 gtts/min
Question 214.
The nurse is performing fluid resuscitation on a burn client. Which piece of assessment data is the best indicator that it is effective?
(a) Respirations 24, unlabored
(b) Urine output of 30ml/hr
(c) Capillary refill < 4 seconds
(d) Apical pulse of 110/min
Answer:
(b) Urine output of 30ml/hr
Rationale:
Answer (b) is correct. Adequate output would be an accurate assessment of fluid volume. If the client was hypovolemic, the body would compensate by retaining fluids and decreasing the urinary output. Answers (a), (c), and (d) do not relate to the fluid volume, and heart rate increase occurs with fluid volume deficit, so they are incorrect.
Question 215.
A client diagnosed with COPD is receiving theophylline (Theodur). Morning laboratory values reveal a theophylline level of 38mcg/mL. Which is the most appropriate nursing action?
(a) Take no action; this is within normal range.
(b) Notify the physician of the level results.
(c) Administer Narcan 2mg IV push stat.
(d) Give the client an extra dose of the medication.
Answer:
(b) Notify the physician of the level results.
Rationale:
Answer (b) is correct. The therapeutic theophylline level is 10-20mcq/mL; therefore, notifying the physician is most appropriate. Answers (a) and (d) are not appropriate actions at this time, and answer (c) is a narcotic antagonist that is not used to reverse the effects of theophylline.
Question 216.
A client has suffered a severe electrical burn. Which medication would the nurse expect to have ordered for application to the burned area?
(a) Mafenide acetate (Sulfamylon)
(b) Silver nitrate
(c) Providone-iodine ointment
(d) Silver sulfadiazine (Silvadene)
Answer:
(a) Mafenide acetate (Sulfamylon)
Rationale:
Answer (a) is correct. Sulfamylon is the topical agent of choice for electrical burns because of its ability to penetrate thick eschar. Answers (b), (c), and (d) have little or no penetration through eschar tissue, making them incorrect.
Question 217.
A client with a head injury develops syndrome of inappropriate antidiuretic hormone (SIADH). Which physician prescription would the nurse question?
(a) D5W at 200mL/hr
(b) Demeclocycline (Declomycin) 150mg Q6h
(c) Daily weights
(d) Monitor intake and output
Answer:
(a) D5W at 200mL/hr
Rationale:
Answer (a) is correct. Fluid restriction is part of the treatment plan for clients with SIADH. This prescription gives the client too much fluid volume; therefore, the nurse should question this order. Answer (b) is a common medication for these clients. The weight and I and 0 are closely monitored, making answers (c) and (d) incorrect.
Question 218.
The nurse is caring for a postpartum client. Which of the following assessment findings would be a reason for concern during the client’s postpartum stay?
(a) Pulse rate of 70-90 the third postpartum day
(b) Diuresis her second and third postpartum days
(c) Vaginal discharge of rubra, serosa, then rubra
(d) Diaphoresis her third postpartum day
Answer:
(c) Vaginal discharge of rubra, serosa, then rubra
Rationale:
Answer (c) is correct. A change in the normal pattern of bleeding could indicate a problem in postpartum recovery. The normal pattern is lochia rubra, serosa, then alba. Answer (a) is a normal pulse rate. Diuresis and diaphoresis occur normally to rid the body of retained fluids, making answers (b) and (d) incorrect.
Question 219.
The nurse is caring for a postpartum client two hours post-delivery who is unable to void. Which of the following nursing interventions should be considered first?
(a) Insert a straight catheter for residual.
(b) Encourage oral intake of fluids.
(c) Check perineum for swelling or hematoma.
(d) Palpate bladder for distention and position.
Answer:
(d) Palpate bladder for distention and position.
Rationale:
Answer (d) is correct. Before taking any action, an assessment is necessary to further investigate the situation. Answers (a) and (b) are appropriate actions, but not initially. Assessing the perineum, as in answer (c), will not help the client to void or help assess for bladder distention, so it is incorrect.
Question 220.
A client is admitted to the intensive care unit after falling on an icy sidewalk and striking the right side of the head. An MRI revealed a right-sided epidural hematoma. Which physical force explains the location of the client’s injury?
(a) Coup
(b) Contrecoup
(c) Deceleration
(d) Acceleration
Answer:
(a) Coup
Rationale:
Answer (a) is correct. A coup type of injury occurs when the brain damage is directly under the site of impact. When the injury is opposite the side of impact, it is identified as contrecoup, as in answer (b). Answers (c) and (d) relate to the movement of brain tissue inside the head, not at impact.
Question 221.
The nurse is preparing to teach a client about phenytoin sodium (Dilantin). Which fact would be most important to teach the client regarding why the drug should not be stopped suddenly?
(a) Physical dependence can develop over time.
(b) Status epilepticus can develop.
(c) A hypoglycemic reaction can develop.
(d) Heart block can develop.
Answer:
(b) Status epilepticus can develop.
Rationale:
Answer (b) is correct. Abruptly discontinuing seizure medications can cause status epilepti- cus to occur. This disorder is life threatening, so this would be most important to tell the client. Answers (a), (c), and (d) are not correct statements about Dilantin, so they are incorrect.
Question 222.
One week after discharge of a postpartum client, the client’s husband calls the postpartum unit and asks the nurse, “Is it normal for my wife to cry at the drop of a hat? I’m worried I’ve done something to upset her.” What is the nurse’s best initial response?
(a) “Have you noticed any pattern to her periods of crying?”
(b) “Try not to worry about it. I'm sure it’s just the postpartum blues.”
(c) “Can you think of something you might have done to upset her?”
(d) “Let’s consider some of the ways you can decrease her depression.”
Answer:
(a) “Have you noticed any pattern to her periods of crying?”
Rationale:
Answer (a) is correct. The nurse should try to find out more information to assist in determining the diagnosis. Answers (b) and (d) contain a diagnosis of which the nurse is not aware, and answer (c) is nontherapeutic because it is accusatory.
Question 223.
A client is admitted with suspected Guillain-Barre syndrome. The nurse would expect the cerebrospinal fluid (CSF) analysis to reveal which of the following to confirm the diagnosis?
(a) CSF protein 10mg/dL and WBC 2 cells/mm3
(b) CSF protein of 60mg/dL and WBC 0 cells/mm3
(c) CSF protein of 50mg/dL and WBC 20 cells/mm3
(d) CSF protein of 5mg/dL and WBC 20 cells/mm3
Answer:
(b) CSF protein of 60mg/dL and WBC 0 cells/mm3
Rationale:
Answer (b) is correct. CSF evaluations are utilized to diagnose GB. An elevated protein without an increase in other cells is indicative of GB, which makes answers (a), (c), and (d) incorrect.
Question 224.
A client with burns is admitted and fluid resuscitation has begun. The client’s CVP reading is 14cm/H2O. Which evaluation by the nurse would be most accurate?
(a) The client has received enough fluid.
(b) The client’s fluid status is unaltered.
(c) The client has inadequate fluids.
(d) The client has a volume excess.
Answer:
(d) The client has a volume excess.
Rationale:
Answer (d) is correct. The normal CVP is 3-8cm of water. An elevation in CVP indicates a fluid volume excess. Answers (a), (b), and (c) indicate that the reading is normal or low, so they are incorrect.
Question 225.
The nurse is working on a neurological unit. If the following events occur simultaneously, which would receive RN priority?
(a) A client with a cerebral aneurysm complains of sudden weakness on the right side.
(b) A client with a suspected brain tumor complains of a frontal type headache.
(c) A client post-op lumbar laminectomy vomits.
(d) A client with Guillain-Barre syndrome has a temperature elevation.
Answer:
(a) A client with a cerebral aneurysm complains of sudden weakness on the right side.
Rationale:
Answer (a) is correct. A change in a client’s neurological status requires further immediate intervention to prevent rapid deterioration. Answers (b), (c), and (d) would not be a cause for immediate concern.
Question 226.
The nurse assesses a client’s fundal height every 15 minutes during the first hour postpartum. What should the height of the fundus be during this hour?
(a) 1-2 fingerbreadths under the umbilicus
(b) four fingerbreadths under the umbilicus
(c) one fingerbreadth above the umbilicus
(d) four fingerbreadths above the umbilicus
Answer:
(c) one fingerbreadth above the umbilicus
Rationale:
Answer (c) is correct. The correct location of the fundus for this time period is one fin- gerbreadth above the umbilicus. Answer (b) occurs on the fourth day post-delivery, and answer (a) is the location for 12 hours after delivery. Answer (d) could indicate a distended bladder; therefore, answers (a), (b), and (d) are incorrect.
Question 227.
The nurse assesses a client complaining of a headache. When the nurse shines a light on the frontal and maxillary sinuses, the light does not penetrate the tissues. What is the best interpretation of this finding?
(a) This is a normal finding indicating no problem.
(b) Inflammation is present in the sinuses.
(c) The cavity likely contains fluid or pus.
(d) The client has a sinus infection.
Answer:
(c) The cavity likely contains fluid or pus.
Rationale:
Answer (c) is correct. A normal finding is for the light to shine through the tissues and appear as a reddish glow. Answers (b) and (d) could also be true, but the best interpretation is that pus or fluid is present. Answer (a) is incorrect because it is not normal for the light to fail to penetrate the tissue.
Question 228.
A client with chronic obstructive pulmonary disease (COPD) is admitted to the respiratory unit. Which physician prescription should the nurse question?
(a) O2 at 5L/min by nasal cannula
(b) Solu Medrol 125mg IV push every six hours
(c) Ceftriaxone (Rocephin) 1 gram IVPB daily
(d) Darvocet N 100 po prn pain
Answer:
(a) O2 at 5L/min by nasal cannula
Rationale:
Answer (a) is correct. The client with COPD uses hypoxemia as a stimulus to breathe. Raising the client’s O2 blood level can suppress the respiratory drive; therefore, this is the prescription the nurse should question. Answers (b), (c), and (d) are correct physician prescriptions for COPD clients and would not need to be questioned.
Question 229.
A burn client begins treatments with silver sulfadiazine (Silvadene) applied to the wounds. The nurse should carefully monitor for which adverse affect associated with this drug?
(a) Hypokalemia
(b) Leukopenia
(c) Hyponatremia
(d) Thrombocytopenia
Answer:
(b) Leukopenia
Rationale:
Answer (b) is correct. A decreased WBC count can occur with the application of Silvadene. The nurse would need to assess the laboratory test results for this adverse effect. Decreased potassium, sodium, and platelets are not associated with Silvadene administration, which makes answers (a), (c), and (d) incorrect.
Question 230.
The nurse is caring for clients on the postpartum unit. Which of the following should the nurse assess first?
(a) A primapara who has delivered an 8-pound baby boy
(b) A gravida IV para IV who experienced one hour of labor
(c) A gravida II para II whose placenta was delivered 10 minutes after the infant
(d) A primapara receiving 100mg of meperidine (Demerol) during her laboring experience
Answer:
(b) A gravida IV para IV who experienced one hour of labor
Rationale:
Answer B is correct. The client most likely to experience complications is the one with the short delivery time due to the possible trauma and lacerations of the birth canal; therefore, she should be seen first. The clients in answers A, C, and D lack the criteria to make them a priority-level visit requirement.
Question 231.
The nurse is assessing a client for tactile fremitus. Which of the following diagnoses would most likely reveal a decrease in tactile fremitus?
(a) Emphysema
(b) Bronchial pneumonia
(c) Tuberculosis
(d) Lung tumor
Answer:
(a) Emphysema
Rationale:
Answer (a) is correct. Tactile fremitus is checked by asking the client to repeat terms such as one, two, three as the nurse’s hands move down the thorax. Air does not conduct sound as well as a solid substance, so fremitus is increased with a solid substance and decreased when air is present, as with emphysema. Answers (b) and (d) are solid-tissue illnesses that would result in increased, not decreased, tactile fremitus. Answer (C) is incorrect because bronchopneumonia usually develops with tuberculosis, causing increased fremitus.
Question 232.
A client who has been diagnosed with lung cancer is starting a smoking-cessation program. Which of the following drugs would the nurse expect to be included in the program’s plan?
(a) Bupropion SR (Zyban)
(b) Metaproterenol (Alupent)
(c) Oxitropuim (Oxivent)
(d) Alprazolam (Xanax)
Answer:
(a) Bupropion SR (Zyban)
Rationale:
Answer (a) is correct. Zyban and Wellbutrin are classified as antidepressants and have been proven to increase long-term smoking abstinence. Answers (b) and (c) are bron- chodilator drugs and are not used for smoking cessation. Answer (d) is a short-acting benzodiazepine and is not used for smoking-cessation therapy.
Question 233.
A client delivered a nine-pound infant two hours ago. The client has an IV of D5W with oxytocin. The nurse determines that the medication is achieving the desired effect when which of the following is assessed?
(a) A rise in blood pressure
(b) A decrease in pain
(c) An increase in lochia rubra
(d) A firm uterine fundus
Answer:
(d) A firm uterine fundus
Rationale:
Answer (d) is correct. Pitocin is administered post-delivery to contract the uterus, resulting in a firm uterus and less chance of hemorrhage. Answers (a) and (c) are not desired effects of this drug. The contraction of the uterus is painful, which makes answer (b) incorrect.
Question 234.
The nurse is evaluating cerebral perfusion outcomes for a client with a subdural hematoma. The nurse evaluates which of the fol- lowing as a favorable outcome for this client?
(a) Arterial blood gas PO2 of 98
(b) Increase in lethargy
(c) Pupils slow to react to light
(d) Temperature of 101 °F
Answer:
(a) Arterial blood gas PO2 of 98
Rationale:
Answer (a) is correct. Arterial blood gas PO2 of 98 indicates adequate oxygenation and a favorable outcome. Answers (b), (c), and (d) are undesirable negative assessment findings, which makes them incorrect.
Question 235.
The nurse is caring for a client with COPD. Which of the associated disorders has changes that are reversible?
(a) Bronchiectasis
(b) Emphysema
(c) Asthma
(d) Chronic bronchitis
Answer:
(c) Asthma
Rationale:
Answer (c) is correct. Asthma is the only disorder that is reversible with treatment or spontaneously after the attack. Answers (a), (b), and (d) can produce permanent damage to parts of the respiratory system, so they are incorrect.
Question 236.
A client experienced a major burn over 55% of his body 36 hours ago. The client is restless and anxious, and states, “I am in pain.” There is a physician prescription for intravenous morphine. What should the nurse do first?
(a) Administer the morphine
(b) Assess respirations
(c) Assess urine output
(d) Check serum potassium levels
Answer:
(b) Assess respirations
Rationale:
Answer (b) is correct. The client's respirations would be assessed before administering morphine because morphine can cause respiratory depression. Answers (c) and (d) have no correlation with morphine administration, so they are incorrect. Answer A would be the next action after the assessment of a normal respiratory rate, but it would not be the first action.
Question 237.
The nurse is caring for a client seven days post-burn injury with 60% body surface area involved What should be the primary
focus of nursing care during this time period?
(a) Meticulous infection-control measures :
(b) Fluid-replacement evaluation
(c) Psychological adjustment to the wound
(d) Measurement and application of a pressure garment
Answer:
(a) Meticulous infection-control measures :
Rationale:
Answer (a) is correct. The main cause of death after the immediate post-burn time frame is sepsis; therefore, preventing infection is a priority for this time period. Answer (b) would be emphasized earlier, and answer (d) requires a healed wound before it can be implemented. Answer (c) would be a necessary intervention during care, but it is not the primary focus.
Question 238.
The nurse is preparing a teaching plan for a client beginning exter- nal radiation treatments. Which of the following will be included in the teaching plan? Select all that apply.
(a) Space activities with rest periods.
(b) Avoid spicy and hot foods.
(c) Expose radiated areas to sunlight daily.
(d) Use moisturizers on skin.
(e) Expect to have difficulty swallowing.
Answer:
(a) Space activities with rest periods.
(b) Avoid spicy and hot foods.
(d) Use moisturizers on skin.
Rationale:
Answers (a), (b), and (d) are correct. These answers are all teaching points for clients using external radiation therapy. Clients should avoid exposure of the area to sunlight during treatment and up to 12 months after the treatments; therefore, answer (c) is incorrect. Answer (e) could indicate damage to the esophagus from the therapy and the physician should be notified.
Question 239.
The nurse is performing discharge teaching for a client after a cardiac catheterization. Which statement by the client indicates a need for further teaching?
(a) “I should not bend, strain, or lift heavy objects for one day."
(b) “If bleeding occurs, I should place an ice bag on the site for 10 minutes.”
(c) “I need to call the doctor if my temperature goes above 101 F°
(d) “I should talk to the doctor to find out when I can go back to work.”
Answer:
(b) “If bleeding occurs, I should place an ice bag on the site for 10 minutes.”
Rationale:
Answer (b) is correct. If there is any bleeding, new bruising, or pain at the puncture site, the physician should be notified. The information in answers (a), (c), and (d) are correct discharge teaching statements, so these answers are incorrect.
Question 240.
A burn client is in the acute phase of burn care. The nurse assesses jugular vein distention, edema, urine output of 20 mLin two hours, and crackles on auscultation. Which order would the nurse anticipate from the physician?
(a) Furosemide (Lasix) 40 mg IV push
(b) Irrigate the Foley catheter
(c) Increase the IV fluids to 200mL/hr
(d) Place the client in Trendelenburg position
Answer:
(a) Furosemide (Lasix) 40 mg IV push
Rationale:
Answer (a) is correct. The nurse suspects congestive heart failure and anticipates an order for a diuretic to remove excess fluid. Answer (b) has insufficient data to support the need. Answer (c) would increase the client’s fluid volume. Lowering the head, in answer (d), would be an expectation for a client with a fluid volume deficit.
Question 241.
The nurse is suctioning a tracheostomy, what is the maximum suction pressure the nurse should use?
(a) 120mmHg
(b) 145mmHg
(c) 160mmHg
(d) 185mmHg
Answer:
(a) 120mmHg
Rationale:
Answer A is correct. The suction source should not exceed 120mmHg when performing trachial suctioning. Answers B, C, and D exceed this amount and could cause damage to the trachea, so they are incorrect.
Question 242.
A client admitted with transient ischemia attacks has returned from a cerebral arteriogram. The nurse performs an assessment and finds a newly formed hematoma in the right groin area. What is the nurse’s initial action?
(a) Apply direct pressure to the site.
(b) Check the pedal pulses on the right leg.
(c) Notify the physician.
(d) Turn the client to the prone position.
Answer:
(a) Apply direct pressure to the site.
Rationale:
Answer (a) is correct. Bleeding at the site requires pressure to stop it. Answers (b) and (c) would be correct actions to take, but eliminating the bleeding process would take priority. Answer (d) is an inappropriate action, and the movement could increase the bleeding, so it is incorrect.
Question 243.
The nurse is assessing an ECG strip of a 42-year-old client and finds a regular rate greater than 100, a normal QRS complex, a normal P wave in front of each QRS, a PR interval between 0.12 and 0.20 seconds, and a P: QRS ratio of 1:1. What is the nurse’s interpretation of this rhythm?
(a) Premature atrial complex
(b) Sinus tachycardia
(c) Atrial flutter
(d) Supraventricular tachycardia
Answer:
(b) Sinus tachycardia
Rationale:
Answer (b) is correct. The systemic analysis of the electrocardiogram shows the information in the question as criteria for sinus tachycardia. Answer (a) would reveal an irregular rhythm and an early or different P wave. Answer (c) is incorrect because the P waves would be saw-toothed and the P: QRS ratio would be 2:1, 3:1, or 4:1. Answer (d) requires an unidentifiable P wave and a PR interval of less than 0.12 seconds, so it is incorrect.
Question 244.
A client is complaining of chest pain. Nursing assessment reveals a BP of 78/40, shortness of breath, and third-degree AV block on the heart monitor. What is the most appropriate initial action?
(a) Provide trancutaneous pacing.
(b) Turn the client on his side.
(c) Reassess the blood pressure.
(d) Consult with cardiology.
Answer:
(a) Provide trancutaneous pacing.
Rationale:
Answer (a) is correct. This is the most appropriate initial action for heart block. Turning the patient on the side (answer b) is an inappropriate action. Answers (c) and (d) are appropriate, but should not be the initial action.
Question 245.
The nurse is discussing cigarette smoking with an emphysema client. The client states, “I don’t know why I should worry about smoking.” The nurse’s response is based on the fact that smoking has which of the following negative effects to the emphysematous lung?
(a) Affects peripheral blood vessels
(b) Causes vasoconstriction to occur
(c) Destroys the lung parenchyma
(d) Paralyzes ciliary activity
Answer:
(d) Paralyzes ciliary activity
Rationale:
Answer (d) is correct. Cigarette smoking directly affects the sweeping action of the cilia, which interferes with the ability to remove mucus and clear the airway. Answers (a) and (b) are accurate statements but do not relate to emphysema. Answer (c) is not a direct effect of smoking.
Question 246.
The nurse is caring for a client admitted with congestive heart failure, Which finding would the nurse expect if the failure was on the right side of the heart?
(a) Jugular vein distention
(b) Dry, nonproductive cough
(c) Dyspneic when supine
(d) Crackles on chest auscultation
Answer:
(a) Jugular vein distention
Rationale:
Answer (a) is correct. The increase in venous pressure causes the jugular veins to distend. Other symptoms of right-sided heart failure include ascites, weakness, anorexia, dependent edema, and weight gain. Answers (b), (c), and (d) result from the left ventricle’s inability to pump blood out of the ventricle to the body and are specific for left-sided, not right-sided, heart failure.
Question 247.
A client with chest pain is scheduled for a heart catheterization. Which of the following would the nurse include in the client’s care plan?
(a) Keep the client NPO for 12 hours afterward.
(b) Inform the client that general anesthesia will be administered throughout the procedure.
(c) Assess the site for bleeding or hematoma once per shift.
(d) Instruct the client that he might be asked to cough and breathe deeply during the procedure.
Answer:
(d) Instruct the client that he might be asked to cough and breathe deeply during the procedure.
Rationale:
Answer (d) is correct. The client might be asked to cough and breathe deeply at certain times during the procedure. Answer (a) is incorrect because fluids are encouraged, to increase urine output and flush out the dye. The client will receive mild to moderate sedation, which makes answer (b) incorrect. Assessment of the site and pedal pulses are performed every 15 minutes for the first hour and then every 1-2 hours until pulses are stable, which makes answer (c) incorrect.
Question 248.
The nurse is caring for a COPD client who is discharged on p.o. Theophylline. Which of the following statements by the client would indicate a correct understanding of discharge instructions?
(a) “A slow, regular pulse could be a side effect.”
(b) “Take the pill with antacid or milk and crackers.”
(c) “The doctor might order it intravenously if symptoms worsen.”
(d) “Hold the drug if symptoms decrease.”
Answer:
(b) “Take the pill with antacid or milk and crackers.”
Rationale:
Answer (b) is correct. Theophylline should be taken with food to prevent Gl irritation. Because this drug can cause tachycardia, answer (a) is incorrect. The IV drug is amino- phylline and may not be ordered with worsening symptoms, so answer (c) is incorrect. Answer (d) is incorrect because the client should continue to take the drug when symptoms get better.
Question 249.
The nurse has just admitted a client with emphysema. Arterial blood gas results indicate hypoxia. Which physician prescription would the nurse implement for the best improvement in the client’s hypoxia?
(a) Elevate the head of the bed 45°.
(b) Encourage diaphragmatic breathing.
(c) Initiate an Alupent nebulizer treatment.
(d) Start O2 at 2L/min.
Answer:
(d) Start O2 at 2L/min.
Rationale:
Answer (d) is correct. The delivery of oxygen is the best measure to correct hypoxia. Answers (a), (b), and (c) should also improve the client’s hypoxia, but oxygen is the prescription that would deliver immediate relief.
Question 250.
The nurse is assessing the chart of a client with a stroke. MRI results reveal a hemorrhagic stroke to the brain. Which physician prescription would the nurse question?
(a) Normal saline IV at 50ml/hr
(b) O2 at 3L/min by nasal cannula
(c) Heparin infusion per pharmacist protocol
(d) Insert a Foley catheter to bedside drainage
Answer:
(c) Heparin infusion per pharmacist protocol
Rationale:
Answer (c) is correct. Delivering an anticoagulant to a client with a hemorrhagic stroke is contraindicated because of the likelihood of increasing the bleed and worsening the client's condition. Answers (a), (b), and (d) are necessary positive treatments for clients with strokes, so they would not be questioned.