The feedback provided with Free NCLEX Questions allows students to understand the reasoning behind correct and incorrect answers, facilitating deeper learning.
NCLEX Integumentary System Health Problems Questions
Integumentary System Health Problems NCLEX Practice Questions
Question 1.
There has been a fire in an apartment building. All residents have been evacuated, but many are burned. Which clients should be transported immediately to a burn center for treatment? Select all that apply.
(a) an 8-year-old with third-degree burns over 10% of the body surface area (BSA)
(b) a 20-year-old who inhaled the smoke of the fire
(c) a 50-year-old diabetic with first- and second-degree burns on the left forearm (about 5% of the body surface area [BSA])
(d) a 30-year-old with second-degree burns on the back of the left leg (about 9% of body surface area [BSA])
(e) a 40-year-old with second-degree bums on the right arm (about 10% of BSA)
Answer:
(a) an 8-year-old with third-degree burns over 10% of the body surface area (BSA)
(b) a 20-year-old who inhaled the smoke of the fire
(c) a 50-year-old diabetic with first- and second-degree burns on the left forearm (about 5% of the body surface area [BSA])
Explanation:
(a), (b), (c) Clients who should be transferred to a bum center include children under age 10 or adults over age 50 with second- and third-degree burns on 10% or greater of their BSA, clients between ages 11 and 49 with second- and third-degree burns over 20% of their BSA, clients of any age with third- degree bums on more than 5% of their BSA, clients with smoke inhalation, and clients with chronic diseases, such as diabetes and heart or kidney disease.
Question 2.
The nurse is assessing an 80-year-old client who has scald burns on the hands and both forearms (first- and second-degree burns on 10% of the body surface area). What should the nurse do first?
(a) Clean the wounds with warm water.
(b) Apply antibiotic cream.
(c) Refer the client to a burn center.
(d) Cover the burns with a sterile dressing.
Answer:
(c) Refer the client to a burn center.
Explanation:
The nurse should have the client transported to a burn center. The client’s age and the extent of the burns require care by a bum team, and the client meets triage criteria for referral to a burn center. Because of the age of the client and the extent of the burns, the nurse should not treat the burn. Scald bums are not at high risk for infection and do not need to be cleaned, covered, or treated with antibiotic cream at this time.
Question 3.
During the emergent (resuscitative) phase of burn injury, which finding indicates that the client requires additional volume with fluid resuscitation?
(a) serum creatinine level of 2.5 mg/dL (221 pmol/L)
(b) little fluctuation in daily weight
(c) hourly urine output of 60 mL
(d) serum albumin level of 3.8 mg/dL (38 g/L)
Answer:
(a) serum creatinine level of 2.5 mg/dL (221 pmol/L)
Explanation:
Fluid shifting into the interstitial space causes intravascular volume depletion and decreased perfusion to the kidneys. This would result in an increase in serum creatinine. Urine output should be frequently monitored and adequately maintained with intravenous fluid resuscitation that would be increased when a drop in urine output occurs. Urine output should be at least 30 mL/h. Fluid replacement is based on the Parkland or Brooke formula and also the client’s response by monitoring urine output, vital signs, and CVP readings.
Daily weight is important to monitor for fluid status. Little fluctua-tion in weight suggests that there is no fluid retention and the intake is equal to output. Exudative loss of albumin occurs in burns, causing a decrease in colloid osmotic pressure. The normal serum albumin is 3.5 to 5 g/dL (35 to 50 g/L).
Question 4.
A client is admitted to the hospital after sustaining bums to the chest, abdomen, right arm, and right leg. The shaded areas in the illustration indicate the burned areas on the client’s body. Using the “rule of nines,” estimate what percentage of the client’s body surface has been burned.
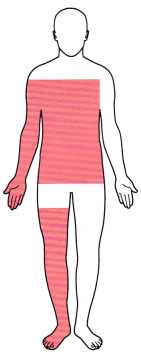
(a) 18%
(b) 27%
(c) 45%
(d) 64%
Answer:
(c) 45%
Explanation:
According to the rule of nines, this client has sustained burns on about 45% of the body surface. The right arm is calculated as being 9%, the right leg is 18%, and the anterior trunk is 18%, for a total of 45%.
Question 5.
The nurse is caring for a client with severe burns who is receiving fluid resuscitation. Which finding indicates that the client is responding to the fluid resuscitation?
(a) pulse rate of 112 bpm
(b) blood pressure of 94/64 mm Hg
(c) urine output of 30 mL/h
(d) serum sodium level of 136 mEq/L(136 mmol/L)
Answer:
(c) urine output of 30 mL/h
Explanation:
Ensuring a urine output of 30 to 50 mL/h is the best measure of adequate fluid resuscitation. The heart rate is elevated, but this is not an indicator of adequate fluid balance. The blood pressure is low, likely related to the hypovolemia, but urinary output is the more accurate indicator of fluid balance and kidney function. The sodium level is within normal limits.
Question 6.
A client is admitted with a 45% partial and full thickness burn. Which finding would alert the nurse that the client has a deficiency in fluid volume during the first 24 hours?
(a) serum creatinine of 1.1 mg/dL (97.2 pmol/L)
(b) serum potassium level of 3.7 mEq/L
(c) oxygen saturation of 94%
(d) urine output of <30 mL/h
Answer:
(d) urine output of <30 mL/h
Explanation:
It is critical that the nurse monitor the vital signs, hemodynamics and urine output during the emergent and resuscitative phase of the burn injury. The urine output of < 30 mL/h is an indication of hypovolemia in this client. The serum creatinine, serum potassium, and the oxygen saturation level are all within acceptable limits.
Question 7.
A client with burns is to have a whirlpool bath and dressing change. What should the nurse do 30 minutes before the bath?
(a) Soak the dressing.
(b) Remove the dressing.
(c) Administer an analgesic.
(d) Slit the dressing with blunt scissors.
Answer:
(c) Administer an analgesic.
Explanation:
Removing dressings from severe burns exposes sensitive nerve endings to the air, which is painful. The client should be given a prescribed analgesic about one-half hour before the dressing change to promote comfort. The other activities are done as part of the whirlpool and dressing change process and not one-half hour beforehand.
Question 8.
The client with a major burn injury receives total parenteral nutrition (TPN). What is the expected outcome of TPN?
(a) Correct water and electrolyte imbalances.
(b) Allow the gastrointestinal tract to rest.
(c) Provide supplemental vitamins and minerals.
(d) Ensure adequate caloric and protein intake.
Answer:
(d) Ensure adequate caloric and protein intake.
Explanation:
Nutritional support with sufficient calories and protein is extremely important for a client with severe burns because of the loss of plasma protein through injured capillaries and an increased metabolic rate. Gastric dilation and paralytic ileus commonly occur in clients with severe burns, making oral fluids and foods contraindicated.
Water and electrolyte imbalances can be corrected by administration of IV fluids with electrolyte additives, although TPN typically includes all necessary electrolytes. Resting the gastrointestinal tract may help prevent paralytic ileus, and TPN provides vitamins and minerals; however, the primary reason for starting TPN is to provide the protein necessary for tissue healing.
Question 9.
Which is an advantage of using biologic burn grafts such as porcine (pigskin) grafts?
Porcine grafts:
(a) encourage the formation of tough skin.
(b) promote the growth of epithelial tissue.
(c) provide for permanent wound closure.
(d) facilitate the development of subcutaneous tissue.
Answer:
(b) promote the growth of epithelial tissue.
Explanation:
Biologic dressings such as porcine grafts serve many purposes for a client with severe burns. They enhance the growth of epithelial tissues, minimize the overgrowth of granulation tissue, prevent loss of water and protein, decrease pain, increase mobility, and help prevent infection. They do not encourage the growth of tougher skin, provide for permanent wound closure, or facilitate the growth of subcutaneous tissue.
Question 10.
Which factor would have the least influence on the survival and effectiveness of a burn victim’s porcine grafts?
(a) absence of infection in the wounds
(b) adequate vascularization in the grafted area
(c) immobilization of the area being grafted
(d) use of analgesics as necessary for pain relief
Answer:
(d) use of analgesics as necessary for pain relief
Explanation:
Analgesic administration to keep a burn victim comfortable is important but is unlikely to influence graft survival and effectiveness. Absence of infection, adequate vascularization, and immobilization of the grafted area promote an effective graft.
Question 11.
When should the nurse initiate rehabilitation plans for the client who has severe burns?
(a) immediately after the burn has occurred
(b) after the client’s circulatory status has been stabilized
(c) after grafting of the burn wounds has occurred
(d) after the client’s pain has been eliminated
Answer:
(b) after the client’s circulatory status has been stabilized
Explanation:
Rehabilitation efforts are implemented as soon as the client's condition is stabilized. Early emphasis on rehabilitation is important to decrease complications and to help ensure that the client will be able to make the adjustments necessary to return to an optimal state of health and independence. It is not possible to completely eliminate the client’s pain; pain control is a major challenge in burn care.
Question 12.
What should the nurse assess the client for during the early phase of burn care?
(a) hypernatremia
(b) hyponatremia
(c) metabolic alkalosis
(d) hyperkalemia
Answer:
(d) hyperkalemia
Explanation:
Immediately after a burn, excessive potassium from cell destruction is released into the extracellular fluid. Hyponatremia is a common electrolyte imbalance in the burn client that occurs within the first week after being burned. Metabolic acidosis usually occurs as a result of the loss of sodium bicarbonate.
Question 13.
Which client with burns will most likely require an endotracheal or tracheostomy tube?
A client who has:
(a) electrical burns of the hands and arms causing arrhythmias.
(b) thermal burns to the head, face, and airway resulting in hypoxia.
(c) chemical burns on the chest and abdomen.
(d) secondhand smoke inhalation.
Answer:
(b) thermal burns to the head, face, and airway resulting in hypoxia.
Explanation:
Airway management is the priority in caring for a burn client. Tracheostomy or endotracheal intubation is anticipated when significant thermal and smoke inhalation burns occur. Clients who have experienced burns to the face and neck usually will be compromised within 1 to 2 hours.
Electrical burns of the hands and arms, even with cardiac arrhythmias, or a chemical burn of the chest and abdomen is not likely to result in the need for intubation. Secondhand smoke inhalation does influence an individual’s respiratory status but does not require intubation unless the individual has an allergic reaction to the smoke.
Question 14.
A client is receiving fluid replacement with lactated Ringer’s after 40% of the body was burned 10 hours ago. The assessment reveals temperature 97.1°F (36.2°C), heart rate 122 bpm, blood pressure 84/42 mm Hg, central venous pressure (CVP) 2 mm Hg, and urine output 25 mL for the last 2 hours. The IV rate is currently at 375 mL/h. Using the SBAR (Situation-Background-Assessment- Recommendation) technique for communication, what prescription should the nurse request from the health care provider?
(a) furosemide
(b) fresh frozen plasma
(c) IV rate increase
(d) dextrose 5%
Answer:
(c) IV rate increase
Explanation:
The decreased urine output, low blood pressure, low CVP, and high heart rate indicate hypovolemia and the need to increase fluid volume replacement. Furosemide is a diuretic that should not be given due to the existing fluid volume deficit. Fresh frozen plasma is not indicated. It is given for clients with deficient clotting factors who are bleeding. Fluid replacement used for burns is lactated Ringer’s solution, normal saline, or albumin.
Question 15.
After the initial phase of the burn injury, what goals should the nurse establish with the client?
(a) helping the client maintain a positive self-concept
(b) promoting hygiene
(c) preventing infection
(d) educating the client regarding care of the skin grafts
Answer:
(c) preventing infection
Explanation:
The inflammatory response begins when a burn is sustained. As a result of the burn, the immune system becomes impaired. There is a decrease in immunoglobulins, changes in white blood cells, alterations of lymphocytes, and decreased levels of interleukin. The human body’s protective barrier, the skin, has been damaged. As a result, the burn client becomes vulnerable to infections. Education and interventions to maintain a positive self-concept would be appropriate during the rehabilitation phase. Promoting hygiene helps the client feel comfortable; however, the primary focus is on reducing the risk for infection.
Question 16.
A client has burns on both hands and upper arms. Which nursing actions will be most helpful in preventing contractures? Select all that apply.
(a) Keep the hands elevated.
(b) Administer narcotic pain medications every 3 hours.
(c) Wash the fingers, hands, and upper arms with cool water.
(d) Apply moisturizer to the hands and fingers.
(e) Apply splints as prescribed.
(f) Collaborate with the physical therapist.
Answer:
(a) Keep the hands elevated.
(e) Apply splints as prescribed.
(f) Collaborate with the physical therapist.
Explanation:
(a), (e), (f) The most helpful strategies to prevent and manage contractures when a client has burns of the hands are to keep the hands elevated, use hand splints, and physical therapy. The nurse should collaborate with the entire burn team to prevent contractures. The nurse should administer pain medication and provide hygiene measures as prescribed, but these do not directly prevent con-tractures. The nurse should check with the health care provider before applying moisturizer or other substances to the burned area.
Question 17.
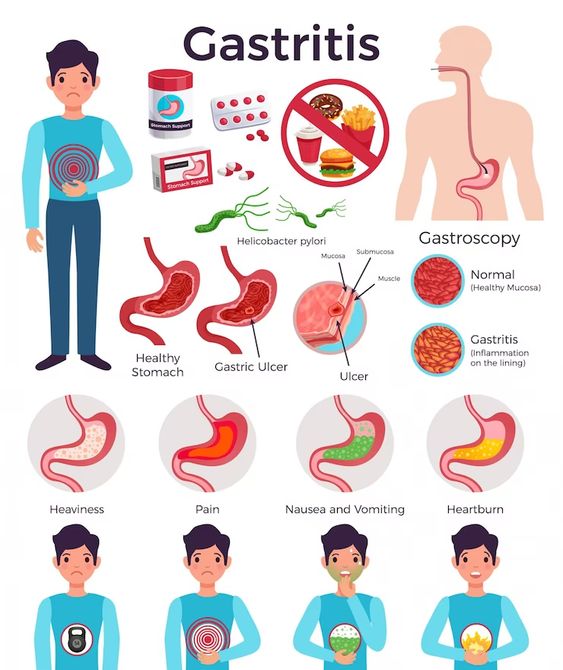
The nurse is conducting a focused assessment of the gastrointestinal system of a client with a burn injury. What should the nurse assess?
(a) paralytic ileus
(b) gastric distention
(c) hiatal hernia
(d) Curling’s ulcer
Answer:
(d) Curling’s ulcer
Explanation:
Curling’s ulcer, or gastrointestinal ulceration, occurs in about half of the clients with a burn injury. The incidence of ulceration appears proportional to the extent of the burns, and the ulceration is believed to be caused by hypersecretion of gastric acid and compromised gastrointestinal perfusion. Paralytic ileus and gastric distention do not result from hyper-secretion of gastric acid and stress and thus are not expected findings at this time. Hiatal hernia is not necessarily a potential complication of a burn injury.
Question 18.
In the acute phase of bum injury, which pain medication would most likely be given to the client to decrease the perception of the pain?
(a) oral analgesics such as ibuprofen or acetaminophen
(b) intravenous opioids
(c) intramuscular opioids
(d) oral antianxiety agents such as lorazepam
Answer:
(b) intravenous opioids
Explanation:
The severe pain experienced by bum clients requires opioid analgesics. In addition, opioids such as morphine sedate and alleviate apprehension. Oral analgesics such as ibuprofen or acetaminophen are unlikely to be strong enough to effectively manage the intense pain experienced by the client who is severely burned. Because of the altered tissue perfusion from the burn injury, intravenous medications are preferred. Antianxiety agents are not effective against pain.
Question 19.
Using the Parkland formula, calculate the hourly rate of fluid replacement with lactated Ringer’s solution during the first 8 hours for a client weighing 75 kg with total body surface area (TBSA) burn of 40%. Record your answer using a whole number ................... mL/h.
Answer:
750 mL/h.
Explanation:
750 mL/h. When calculating fluid replacement, only the burned portion of the TBSA is used to calculate fluid volume; thus, the nurse should administer the solution at 750 mL/h. Lactated Ringer’s solution 4 mL x weight in kg x TBSA; half given over the first 8 hours and half given over the next 16 hours.
4 mL × 75 kg × 40 = 12,000 mL or
\(\frac{4 \mathrm{~mL} \times 75 \mathrm{~kg} \times 40}{8 \text { hours }} \times \frac{1}{2}=\frac{750 \mathrm{~mL}}{\text { hour }}\)
12,000 mL × 21 = 6,000 mL
\(\frac{6,000 \mathrm{~mL}}{8 \text { hours }}\) = 750 mL/h
Question 20.
The nurse is assessing an older adult’s skin. The assessment will involve inspecting the skin for color, pigmentation, and vascularity. What should the nurse assess?
(a) similarities from one side to the other
(b) changes from the normal expected findings
(c) appearance of age-related wrinkles
(d) skin turgor
Answer:
(b) changes from the normal expected findings
Explanation:
Noting changes from the normal expected findings is the most important component when assessing an older client’s integumentary system. Comparing one extremity with the contralateral extremity (i.e., comparing one side with the other) is an important assessment step; however, the most important component is noting changes from an expected normal baseline.
Noting wrinkles related to age is not of much consequence unless the client is admitted for cosmetic surgery to reduce the appearance of age-related wrinkling. Noting skin turgor is an assessment of fluid status, not an assess-ment of the integumentary system.
Question 21.
Which change in the integumentary system is associated with normal aging?
(a) The outer layer of skin is replaced with new cells every 3 days.
(b) Subcutaneous fat and extracellular water decrease.
(c) The dermis becomes highly vascular and assists in the regulation of body temperature.
(d) Collagen becomes elastic and strong.
Answer:
(b) Subcutaneous fat and extracellular water decrease.
Explanation:
With age, there is a decreased amount of subcutaneous fat, muscle laxity, degeneration of elastic fibers, and collagen stiffening. The outer layer of skin is almost completely replaced every 3 to 4 weeks. The vascular supply diminishes with age. Collagen thins and diminishes with age.
Question 22.
Which findings should the nurse expect to assess as normal skin changes in an older adult? Select all that apply.
(a) diminished hair on scalp and pubic areas
(b) dusky rubor of left lower extremity
(c) solar lentigo
(d) wrinkles
(e) xerosis
(f) yellow pigmentation
Answer:
(a) diminished hair on scalp and pubic areas
(c) solar lentigo
(d) wrinkles
(e) xerosis
Explanation:
(a), (c), (d), (e) Skin changes associated with aging include the following: diminished hair on scalp and pubic areas, solar lentigo (liver spots), wrinkles, and xerosis (dryness). Dusky rubor of the left lower extremity may indicate the individual has a venous stasis problem in the affected extremity and is gen-erally associated with “unsuccessful aging.” Yellow pigmentation of the skin that may be associated with liver inflammation is generally known as jaundice.
Question 23.
An older adult is having abdominal surgery. The nurse should assess the client for which post-operative concern related to normal changes in the integumentary system of an older adult?
(a) increased scarring
(b) decreased melanin and melanocytes
(c) decreased healing
(d) increased immunocompetence
Answer:
(c) decreased healing
Explanation:
Normal aging consists of decreased proliferative capacity of the skin. Decreased collagen synthesis slows capillary growth, impairs phagocytosis among older clients, and results in slow healing. Increased scarring is not a result of age-related skin changes. Both melanin and melanocytes give color to the skin and hair but are increased with aging. There is a decrease in the immunocompetence of the aging client.
Question 24.
The nurse is instructing an older adult about ways to promote skin integrity. Which health main-tenance behavior by the client is most helpful?
(a) drinks 1,500 mL of fluids per day.
(b) consumes a balanced diet of 1,200 cal/day
(c) walks briskly for 10 minutes three times per week
(d) sleeps at least 8 hours each night
Answer:
(a) drinks 1,500 mL of fluids per day.
Explanation:
Drinking at least 1,500 mL of fluid per day helps the client stay well hydrated. Maintaining optimal fluid balance is important for all body systems, and particularly the skin. Caloric intake varies according to an individual’s size and activity level. An intake of 1,200 cal/day may be insufficient for some older clients. Walking 10 minutes/day is useful, but an otherwise healthy older client should try to walk 20 to 30 minutes/day three or more times a week. It is important to get adequate rest; however, the amount of sleep needed varies with the individual.
Question 25.
Which factor puts an older adult at the greatest risk for impaired wound healing after abdominal surgery?
(a) age over 75 years
(b) poorly controlled diabetes
(c) history of one myocardial infarction
(d) chronic peripheral vascular disease
Answer:
(b) poorly controlled diabetes
Explanation:
Poorly controlled diabetes is a serious risk factor for postoperative wound infection. Other factors that delay wound healing include nutritional deficiencies (vitamin C, protein, zinc), use of corticosteroid, infection, mechanical friction on the wound, obesity, anemia, and poor general health.
A previous myocardial infarction is not a risk factor for wound infection. Peripheral vascular disease is not as much of a risk factor for infection of an abdominal wound as it might be for more distal parts of the body. Being frail is not a specific risk factor for wound infection.
Question 26.
An older adult has several ecchymotic areas on the left arm. What should the nurse further assess? Select all that apply.
(a) elder abuse
(b) self-inflicted injury
(c) increased capillary fragility and permeability
(d) increased blood supply to the skin
(e) shingles
Answer:
(a) elder abuse
(b) self-inflicted injury
(c) increased capillary fragility and permeability
Explanation:
(a), (b), (c) The nurse should always assess an older adult who has signs of bruising (ecchymosis) for signs of abuse, self-inflicted injuries, or injuries that might have occurred from falls. Also, the aging process involves increased capillary fragility and permeability, and because older adults have a decreased amount of subcutaneous fat, it is also likely that there is an increased incidence of bruise like lesions caused by collection of extravascular blood in the loosely structured dermis.
In addition, older clients do not always realize that injury has occurred because of a diminished awareness of pain, touch, and peripheral vibration. Blood supply to the skin decreases with aging and thus is not a cause of the ecchymotic areas. Shingles presents as a red rash and fluid-filled blisters.
Question 27.
An older adult reports being cold in the room even though the thermostat is set at 75°F (24°C). The nurse can tell the client that older adults may feel cold for which reason?
Older adults have:
(a) increased cellular cohesion.
(b) increased moisture content of the stratum corneum.
(c) slower cellular renewal time.
(d) decreased ability to thermoregulate.
Answer:
(d) decreased ability to thermoregulate.
Explanation:
Older clients have a decreased thermoregulation that is related to decreased blood supply and reabsorption of body fat. As a result, older adults are at risk for hypothermia. Cellular cohesion and moisture content diminish with age, and cellular renewal time is slowed; however, these do not result in impaired thermoregulation.
Question 28.
What should the nurse instruct the client with tinea capitis to do? Select all that apply.
(a) Place a dressing saturated with vinegar and water on the area.
(b) Apply topical antibacterial ointment to the area.
(c) Shampoo hair two or three times with selenium sulfide shampoo.
(d) Use antibacterial soap for bathing.
(e) Take antifungal medication as prescribed.
Answer:
(c) Shampoo hair two or three times with selenium sulfide shampoo.
(e) Take antifungal medication as prescribed.
Explanation:
(c), (e) Tinea capitis is a contagious fungal infection of the hair shaft. The hair should be shampooed two or three times with selenium sulfide shampoo. An oral medication will typically be prescribed as well, since the shampoo alone will not cure tinea capitis.
Vinegar and water may be used to treat tinea pedis. The most common fungal skin infection is tinea (also called ringworm because of its characteristic appearance of a ring or rounded tunnel under the skin). Tinea infections affect the head, body, groin, feet, and nails. Antibacterial ointment and soap are not effective for treating fungal infections.
Question 29.
An older adult has pruritus on the arms and legs and is scratching the affected areas. Which is the priority nursing care for this client?
(a) preventing infection
(b) instructing the client not to scratch
(c) increasing fluid intake
(d) avoiding social isolation
Answer:
(a) preventing infection
Explanation:
The client is at risk for infection because of the pruritus, and the nurse should institute measures to help the client control the scratching such as cutting fingernails, using protective gloves or mitts, and, if necessary, using antianxiety medications. More information is required regarding the knowledge level of the client, but learning cannot take place when an individual’s attention is distracted by pruritus. Increasing fluid intake is not a priority at this time. There is no data to indicate the client is experiencing social isolation.
Question 30.
The nurse is applying a hand mitt restraint for a client with pruritus (see figure). What should the nurse do first?

(a) Verify the prescription to use the restraint.
(b) Secure the mitt with ties around the wrist tied to the bed frame.
(c) Place a folded pillow under the wrist.
(d) Place the mitt on top of the hand.
Answer:
(a) Verify the prescription to use the restraint.
Explanation:
Before using any restraints, the nurse must verify that a health care provider (HCP) Q has written a prescription for the restraint. The mitt does not need to be secured with ties. The client can move the hand as needed. It is not necessary to place a pillow under the wrist. The nurse should place the mitt on the palmar surface of the hand.
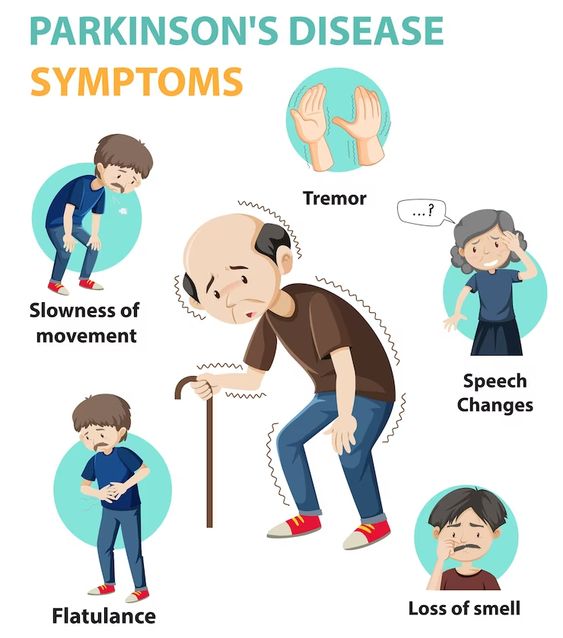
Question 31.
An older adult client in stage 2 of Parkinson’s disease is being discharged with cellulitis of the right lower extremity. The muse should base the discharge plan on which information? Select all that apply.
The client has:
(a) decreased tissue perfusion.
(b) risk for skin breakdown.
(c) potential for falls.
(d) difficulty communicating.
(e) limited activity.
Answer:
(b) risk for skin breakdown.
(c) potential for falls.
Explanation:
(b), (c) Usual aging is associated with dry skin; however, seborrhea (oily skin and dandruff) is one result of the biochemical changes associated with Parkinson’s disease. The client with Parkinson’s disease has a higher risk of skin breakdown due to the moist and oily skin. To maintain skin integrity, a client with Parkinson’s disease needs frequent skin care and aeration of the skin.
Gait instability in a client with Parkinson’s disease is a result of muscle rigidity, change in the center of gravity, and gait shuffling. Because of these changes in gait and balance, the client is at higher risk for injuries in the environment, such as hitting furniture or obstacles in the client’s path.
As a result, the environment should be evaluated for potential injury or falls. Tissue perfusion and verbal communication are not problems typically associated with Parkinson’s disease. The client should not experience activity intolerance from the cellulitis or Parkinson’s disease.
Question 32.
The nurse is discharging an older adult to home after hospitalization for cellulitis of the right foot, followed by an infection. After reviewing discharge instructions, what statement by the client indicates the need for further teaching by the nurse?
(a) “I will eat lots of fruit and vegetables and take vitamin C to help this heal.”
(b) “I will be sure to wear shoes to protect my feet when I go out to get the mail.”
(c) “I will manage my pain by putting this foot up on a pillow when it hurts.”
(d) “I will take the antibiotics until the redness goes away and my foot feels better.”
Answer:
(d) “I will take the antibiotics until the redness goes away and my foot feels better.”
Explanation:
It is important for the client to understand the need to complete the entire course of oral antibiotics as prescribed in order to prevent recurrence/worsening of cellulitis. Further, if the pain and redness continue despite antibiotics, the client needs to understand the need to follow up with the health care provider. Extra vitamin C, protective footwear, and elevating the foot are strategies to promote healing.
Question 33.
The nurse is assessing a group of older adults. Which client is at greatest risk for skin breakdown?
A person who has:
(a) altered balance.
(b) reduced sensation of pressure.
(c) impaired hearing ability.
(d) impaired visual acuity.
Answer:
(b) reduced sensation of pressure.
Explanation:
Pressure ulcers usually occur over bony prominences. An alteration in the protective pressure sensation results from a decline in the number of Meissner’s and pacinian corpuscles. Older adults do have altered balance that may result in falls but not skin breakdown. Impaired hearing and vision do not contribute to pressure ulcers.
Question 34.
The client has been diagnosed with herpes zoster (shingles). The nurse should include which information in a teaching plan? Select all that apply.
(a) Instruct the client about taking antiviral agents as prescribed.
(b) Demonstrate how to apply wet-to-dry dressings.
(c) Explain how to follow proper hand hygiene techniques.
(d) Assure the client that the pain from herpes zoster will be gone by 7 days.
(e) Tell the client to remain in isolation in a bed room until the lesions have healed.
Answer:
(a) Instruct the client about taking antiviral agents as prescribed.
(b) Demonstrate how to apply wet-to-dry dressings.
(c) Explain how to follow proper hand hygiene techniques.
Explanation:
(a), (b), (c) The nurse should instruct the client and family members about the importance of taking antiviral agents as prescribed. The client must be taught how to apply wet dressings or medication to the lesions and to follow proper hand hygiene techniques to avoid spreading the virus. The healing time varies from 7 to 26 days. The most common complication is postherpetic neuralgia, which may last longer than 6 months. It is not necessary for the client to remain in isolation.
Question 35.
Which client should receive a shingles vaccine?
A client who:
(a) has never had chickenpox
(b) is at risk for genital herpes
(c) is over 50 years of age
(d) has a compromised immune system
Answer:
(c) is over 50 years of age
Explanation:
People older than 50 years should receive shingles vaccine to prevent the disease. The vaccine is not effective for genital herpes. The vaccine can be given to persons who have or have not had chickenpox. The vaccine is not advised for persons with a compromised immune system, for example, those receiving chemotherapy or radiation therapy.
Question 36.
A 65-year-old client received Zostavax vac-cine for shingles 5 years ago. The client asks the nurse if the vaccine is still effective. What should the nurse tell the client?
(a) “Your vaccine is still up-to-date.”
(b) “This vaccine is no longer effective.”
(c) “You should be revaccinated with a newer vaccine.”
(d) “You’re too old to receive another vaccine.”
Answer:
(c) “You should be revaccinated with a newer vaccine.”
Explanation:
A newer vaccine, Shingrex, is available and offers greater protection against the shingles virus. The vaccine is administered in two doses 2 to 6 months apart. Even though the client has been vaccinated with Zostavax, the client should be revaccinated with the newer vaccine. The vaccine with Zostavax is not considered up-to-date, and is effective, but does not offer the same protection as being revaccinated. Clients over the age of 50 should receive the newer vaccine or be revaccinated as needed.
Question 37.
A nurse is caring for an older adult with shingles. The client is experiencing considerable pain related to open blisters on the client’s abdomen and back. The client is taking acyclovir and low-dose prednisone. The nurse has several prescriptions available. What additional medications or nursing care strategies to promote comfort may be helpful? Select all that apply.
(a) diphenhydramine 25 mg by mouth every 6 hours prn
(b) calamine lotion applied to the affected areas
(c) cool, wet compresses to the affected areas
(d) acetaminophen 325 mg by mouth every 6 hours prn
(e) ondansetron 4 mg by mouth every 4 hours prn
(f) diversionary activities to prevent client scratching
Answer:
(a) diphenhydramine 25 mg by mouth every 6 hours prn
(b) calamine lotion applied to the affected areas
(c) cool, wet compresses to the affected areas
(d) acetaminophen 325 mg by mouth every 6 hours prn
(e) ondansetron 4 mg by mouth every 4 hours prn
Explanation:
(a), (b), (c), (d), (e) Diphenhydramine is an antihistamine that reduces allergic reactions, calamine lotion is a topical antipruritic, and acetaminophen is an analgesic. These medications may help increase client comfort by reducing pain, inflammation, and itching, which, in turn, may reduce client scratching and potentially spreading the virus. Cool wet compresses also relieve itching and pain. Ondansetron
is an antiemetic and would not be helpful for this client’s discomfort.
Question 38.
The nurse is assessing a client with dark skin for the presence of a stage I pressure ulcer. Which is the best approach to making this assessment?
(a) Use a fluorescent light source to assess the skin.
(b) Inspect the skin only when the Braden score is above 12.
(c) Look for skin color that is darker than the surrounding tissue.
(d) Avoid touching the skin during inspection.
Answer:
(c) Look for skin color that is darker than the surrounding tissue.
Explanation:
When assessing a client with dark skin for the presence of a pressure ulcer, the nurse should observe for skin that is darker, brownish, purplish, or bluish compared to the surrounding skin. Fluorescent light casts a blue light, making skin assessment difficult; natural or halogen light sources help to accurately assess the skin. Risk assessment using the Braden Scale should be performed on all clients.
A Braden score of 12 indicates a high risk for pressure ulcer, and the lower the Braden score, the higher the risk (no risk 19 to 23, at risk 15 to 18, moderate risk 13 to 14, high risk 10 to 12, and very high risk 9 or below). The nurse should touch the skin to assess consistency and temperature differences.
Question 39.
The nurse is assessing a client who is immobile and notes that an area of sacral skin is reddened, but not broken. The reddened area continues to blanch and refill with fingertip pressure. What should the nurse do next?
(a) Apply a moist-to-moist dressing, being careful to pack just the wound bed.
(b) Consult with a wound-ostomy-continence nurse specialist.
(c) Reposition the client off of the reddened skin and reassess in a few hours.
(d) Complete and document a Braden skin breakdown risk score for the client.
Answer:
(c) Reposition the client off of the reddened skin and reassess in a few hours.
Explanation:
A stage I ulcer presents as an area of intact, nonblanchable redness, usually over a bony prominence, caused by pressure. If a reddened area blanches and refills with fingertip pressure, it indicates that there is still some blood flow to the injured area, and the redness may be reversible. It may be appropriate to complete and document a Braden score or consult a wound nurse specialist, but it is imperative to reposition the client of the reddened skin area first. Since there is no break in the skin, it is not appropriate to apply a moist-to-moist dressing.
Question 40.
A nurse utilizes an interpreter to teach a non-English-speaking client how to change a dressing. After explaining the procedure through the interpreter and giving the client an education document with pictures of the procedure, the nurse asks if the client understands the information. The client nods yes. What should the nurse do next? Select all that apply.
(a) Ask the interpreter to repeat the question to confirm the response.
(b) Request the client demonstrate the dressing change.
(c) Have the client sign the education document to confirm understanding.
(d) Review the educational instruction with the client a second time.
(e) Ask a question that does not involve a yes or no response.
Answer:
(b) Request the client demonstrate the dressing change.
(e) Ask a question that does not involve a yes or no response.
Explanation:
(b), (e) Clients from some cultures highly respect educated professionals and will nod “yes” in response to questions out of respect. Clients may also nod their heads to avoid loss of face if they do not understand the information. Having the interpreter repeat the question to confirm the response will result in the same response, and uncertainty related to understanding.
Having the client sign the patient education document to confirm understanding would not confirm client understanding. Unless the nurse tries a different approach to instructing the client, the client may continue to not understand how to change the dressing; observing the client change the dressing or having the client explain the procedure are effective ways to evaluate the client’s understanding of the procedure.
Question 41.
The nurse is assessing a hospitalized older client for the presence of pressure ulcers. The nurse notes that the client has a 1" x 1" (3 cm x 3 cm) area on the sacrum in which there is skin breakdown as far as the dermis. What should the nurse note on the medical record?
(a) stage I pressure ulcer
(b) stage II pressure ulcer
(c) stage III pressure ulcer
(d) stage IV pressure ulcer
Answer:
(b) stage II pressure ulcer
Explanation:
Stage I pressure ulcers appear as nonblanching macules that are red in color. Stage II ulcers have breakdown of the dermis. Stage III ulcers have full-thickness skin breakdown. In stage IV ulcers, the bone, muscle, and supporting tissue are involved. The nurse should immediately initiate plans to relieve the pressure, ensure good nutrition, and protect the area from abrasion.
Question 42.
The nurse is assessing a client with a pressure ulcer. Which indicates that a client has a stage II pressure ulcer?
(a) redness in the involved area
(b) muscle spasms in the involved area
(c) pain in the involved area
(d) tissue necrosis in the involved area
Answer:
(c) pain in the involved area
Explanation:
A stage II skin breakdown involves epidermal sloughing and pain. Redness without blanching is noted in stage I. Stage III involves tissue necrosis with subcutaneous involvement. Stage IV involves muscle or bone destruction. Muscle spasm is not a criterion used in the staging process.
Question 43.
The muse is using home telehealth monitoring to manage care for an 80-year-old who is home bound. The client spends most of the day in bed. Two months ago, the nurse detected sacral redness from friction and shearing force of being in bed. Last month, the client had increased sacral redness, and the area was classified as a stage I pressure ulcer. On this visit, the nurse is assessing the sacral area using a video camera. The nurse compares the site from a visit made 1 month ago (see figure part A) to the assessment made at this visit (see figure part B). Upon comparing the change of the pressure ulcer from this visit to the previous visit, what should the nurse do next?
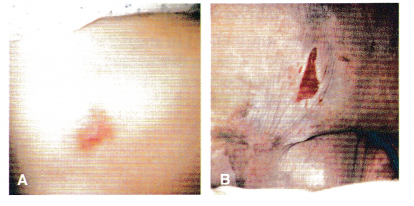
(a) Instruct the home health aide to reposition the client every 2 hours while the client is awake.
(b) Ask the client’s daughter to take pictures of the area and send them to the nurse.
(c) Contact the health care provider (HCP) to request a hydrocolloid dressing.
(d) Make a home visit to verify the changes in the ulcer.
Answer:
(c) Contact the health care provider (HCP) to request a hydrocolloid dressing.
Explanation:
The pressure ulcer has changed from stage I to stage II and requires the use of a protective dressing. Repositioning and use of foam mattresses are appropriate interventions for stage I pressure ulcers. While the daughter can take pictures and send them to the nurse, it is the nurse’s responsibility to make decisions about needed care. Telehealth monitoring equipment is providing sufficient visualization of the skin changes; the nurse does not need to make a home visit at this time.
Question 44.
Which factor places a client at greatest risk for skin cancer?
(a) fair skin and history of chronic sun exposure
(b) Caucasian race and history of hypertension
(c) dark skin and family history of skin cancer
(d) dark skin and history of hypertension
Answer:
(d) dark skin and history of hypertension
Explanation:
Caucasians who have fair skin and a high exposure to ultraviolet light are at increased risk for malignant neoplasms of the skin. The other risk factors include exposure to tar and arsenicals and family history. History of hypertension is a coronary artery disease risk factor. Clients with dark skin have increased melanin and are not as prone to skin cancer.
Question 45.
A nurse is teaching a client about skin can-cer. Which risk factors for skin cancer should the nurse explain? Select all that apply.
(a) increasing age
(b) exposure to chemical pollutants
(c) long-term exposure to the sun
(d) increased pigmentation
(e) genetics
(f) immunosuppression
Answer:
(a) increasing age
(b) exposure to chemical pollutants
(c) long-term exposure to the sun
(d) increased pigmentation
(f) immunosuppression
Explanation:
(a), (b), (c), (d), (f) Risk factors associated with skin cancer include age, exposure to chemical pollutants, exposure to the sun, genetics, and immunosuppres-sion. As individuals age, the risk of developing skin cancer increases.
Longtime exposure to the sun and exposure to chemical pollutants (nitrates, coal, tar, etc.) increase the risk of skin cancer. Individuals who have less skin pigmentation (e.g., fair, blueeyed people) have a higher risk of skin cancer because they tend to incur sunburns rather than tan. Family history plays a role in cancer. Regardless,
Question 46.
The nurse is developing a program about skin cancer prevention for a comm un i ty group. Which information should be included in the pro-gram? Select all that apply.
(a) Purchase sunscreen containing benzophe-nones to block UVA and UVB rays.
(b) Use sunscreen with a minimum of 30 sun protection factor (SPF).
(c) Obtain genetic screening to identify risk of melanoma.
(d) Apply sunscreen only on sunny days, especially between 1000 and 1400.
(e) Have a pigmented lesion biopsied by shaving if it looks suspicious.
Answer:
(a) Purchase sunscreen containing benzophe-nones to block UVA and UVB rays.
(b) Use sunscreen with a minimum of 30 sun protection factor (SPF).
Explanation:
(a), (b) Sunscreen should be applied 20 to 30 minutes before going outside, even in cloudy weather. Sunscreen with a minimum of 30 SPF should be used. Sunscreen containing benzophe- nones block both UVA and UVB rays. The rays of the sun are most dangerous between 1000 and 1400. Genetic screening is not indicated, although a mutated gene has been identified in some families with high incidence of melanoma. A prior diagnosis of melanoma and having a first-degree relative diagnosed with melanoma increase a person’s risk. Lesions should not be shave biopsied; excisional biopsy technique is used.
Question 47.
A client with malignant melanoma asks the nurse about the prognosis. The nurse should tell the client that the prognosis depends on which factor?
(a) the amount of ulceration of the lesion
(b) the age of the client
(c) the location of the lesion on the body
(d) the thickness of the lesion
Answer:
(d) the thickness of the lesion
Explanation:
Tumor or lesion thickness is the predictive factor for survival. Cutaneous melanoma that is confined to the epidermis has a high cure rate. Asymmetry, border, color, and diameter are known as the “ABCDs” of melanoma. Thus, the amount of ulceration, age, and location are not clearly associated with the prognosis.
Question 48.
The nurse finds an unlicensed assistive personnel (UAP) massaging the reddened bony prominences of a client on bed rest. What should the nurse do?
(a) Reinforce the UAP’s use of this intervention over the bony prominences.
(b) Explain that massage is effective because it improves blood flow to the area.
(c) Inform the UAP that massage is even more effective when combined with lotion during the massage.
(d) Instruct the UAP that massage is contraindicated because it decreases blood flow to the area.
Answer:
(d) Instruct the UAP that massage is contraindicated because it decreases blood flow to the area.
Explanation:
Massaging areas that are reddened due to pressure is contraindicated because it further reduces blood flow to the area. The UAP Q3 should not massage the bony prominences or use lotion on the area. Massage does improve circulation and blood flow to muscle areas; however, because the area is reddened, the client is at risk for further skin breakdown.
Question 49.
The nurse manager on the orthopedic unit is reviewing a report that indicates that in the last month, five clients were diagnosed with pressure ulcers. What should the nurse manager do?
(a) Use benchmarking procedures to compare the findings with other nursing units in the hospital.
(b) Ask the staff education department to conduct an educational session about preventing pressure ulcers.
(c) Institute a quality improvement plan that identifies contributing factors, proposes solu-tions, and sets improvement outcomes.
(d) Conduct a chart audit to determine which nurses on which shifts were giving nursing care to the clients with pressure ulcers.
Answer:
(c) Institute a quality improvement plan that identifies contributing factors, proposes solu-tions, and sets improvement outcomes.
Explanation:
The problem of pressure ulcers in hospitalized clients is best addressed by using quality improvement techniques to identify the problem, determining strategies for improvement, and setting goals for outcomes. Benchmarking for comparison will indicate where this nursing unit compares with other units, but does not address the problem for this unit; having clients with pressure ulcers on any unit is not acceptable. Educational programs are more effective after there is an understanding of the problem. Chart audits and blaming do not solve the problem or address quality improvement measures.
Question 50.
A client has been admitted to the hospital with draining foot lesions. What should the nurse do? Select all that apply.
(a) Place the client in a room with negative air pressure.
(b) Admit the client to a semiprivate room.
(c) Admit the client to a private room.
(d) Post a “contact isolation” sign on the door.
(e) Wear a protective gown when in the client’s room.
(f) Wear gloves when providing direct care.
Answer:
(c) Admit the client to a private room.
(d) Post a “contact isolation” sign on the door.
(e) Wear a protective gown when in the client’s room.
(f) Wear gloves when providing direct care.
Explanation:
(c), (d), (e), (f) Infection control policies must be followed to prevent the spread of infection. Until the pathogens are identified, the client must be isolated in a private room. Utilizing contact isolation and wearing a protective isolation gown and clean gloves, in addition to following isolation protocol to exit the room, may aid in the prevention of spread of infectious agents to others. A draining foot lesion does not require a negative air pressure room, which is primarily reserved for preventing spread of tuberculosis.
Question 51.
The nurse is to administer an antibiotic to a client with bums, but there is no medication in the client’s medication box. What should the nurse do
first?
(a) Inform the unit’s shift coordinator.
(b) Contact the client’s health care provider (HCP).
(c) Call the pharmacy department.
(d) Borrow the medication from another client.
Answer:
(c) Call the pharmacy department.
Explanation:
By contacting the pharmacy to report the absence of the medication, the pharmacy can bring the medication to the client’s medication box. From there on, the pharmacy can make sure the correct medications are present. Contacting the shift coor-dinator or the client’s HCP will not correct the original cause of the variance. It is never appropriate to “borrow” a medication from another client.
Question 52.
A client has a wound on the ankle that is not healing. The nurse should assess the client for which risk factors for delayed wound healing? Select all that apply.
(a) atrial fibrillation
(b) advancing age
(c) type 2 diabetes mellitus
(d) hypertension
(e) smoking
Answer:
(b) advancing age
(c) type 2 diabetes mellitus
(e) smoking
Explanation:
(b), (c), (e) Advancing age, type 2 diabetes mellitus, and smoking are risk factors for delayed healing. Advanced age slows collagen synthesis by fibroblasts, impairs circulation, and requires a longer time for epithelialization of the skin. Type 2 diabetes mellitus reduces supply of oxygen and nutrients secondary to vascular complications. Nicotine is a potent vasoconstrictor and impedes blood flow, which reduces the supply of oxygen and nutrients necessary for healing. Atrial fibrillation causes venous stasis in the atria, but it does not have an effect on wound healing. Hypertension does not have an effect on healing.
Question 53.
The nurse is assessing the left lower extremity of a client with type 2 insulin-requiring diabetes and cellulitis. What should the nurse do?
(a) Instruct the client to elevate the left leg when sitting in the chair.
(b) Encourage the client to ambulate in the halls on the unit.
(c) Massage the left leg with alcohol to stimulate circulation.
(d) Cleanse the left lower leg with perfumed liquid soap.
Answer:
(c) Massage the left leg with alcohol to stimulate circulation.
Explanation:
The client has cellulitis and should elevate the affected area above heart level. Ambulation stimulates circulation and promotes deposition of pathogens in other areas of the body. Alcohol and perfumed soaps are drying to the skin. Massaging the lower extremities could dislodge a clot.
Question 54.
A client is admitted with pneumonia and shingles with draining lesions over the right anterior and posterior chest wall. Of the nurses scheduled for the shift, which nurses may he assigned to care for this client? Select all that apply.
(a) 43-year-old female who had a preexposure varicella vaccination
(b) 48-year-old male who had shingles 1 year prior
(c) 32-year-old female who is in the first trimester of pregnancy
(d) 24-year-old female who has never had the pneumococcal vaccine
(e) 36-year-old male taking steroids for an auto immune disease.
Answer:
(a) 43-year-old female who had a preexposure varicella vaccination
(b) 48-year-old male who had shingles 1 year prior
(d) 24-year-old female who has never had the pneumococcal vaccine
Explanation:
(a), (b), (d) While the 43-year-old female has not had chickenpox, she has been vaccinated against the disease. A person can have shingles twice, but there is nothing in the 48-year-old nurse’s history that precludes him from caring for this client. Having or not having the pneumococcal vaccine does not preclude a health care worker for caring for someone with pneumonia or shingles.
Anyone who is immunocompromised or pregnant is at an increased risk for contracting varicella and should not be assigned to care for a client with shingles. All health care workers should have evidence of immunity to varicella and, if not, should receive two doses of vaccine at the recommended intervals at the time of employment. However, in this scenario, the immunity status of the pregnant nurse is not given, and risk reduction is warranted.