Regular practice with CEN Study Guide enhances critical thinking skills, which are vital for making sound clinical decisions.
Genitourinary Emergencies CEN Study Guide
Genitourinary Infections
- Epididymitis is inflammation of the epididymis. It is usually the result of a bacterial infection secondary to a UTI or sexually transmitted disease.
- Diagnosis: gradual onset pain posterior to testes; s/s lower UTI; positive Prehn sign; swelling and tenderness in testis; ultrasound showing enlarged epididymis; labs show infection
- Management: antibiotics; pain management (analgesics, ice packs, scrotal support or elevation); epididymectomy for severe infection
- Orchitis is inflammation of the testes usually caused by a bacterial or viral infection. It can occur secondary to epididymitis (epididymoorchitis).
- Diagnosis: unilateral, sudden onset of vain in testis; swelling and tenderness in testis; when associated with mumps, will appear 4-7 days after s/s of infection; ultrasound showing increased blood flow to the affected testis
- Management: antibiotics; anti-inflammatories; pain management (analgesics, ice packs, scrotal support or elevation)
- Prostatitis is inflammation of the prostate, usually caused by bacterial infection (E. coli). Asymptomatic cases are often discovered during unrelated assessments and are not usually treated.
- Diagnosis: urinary symptoms (e.g., frequent, urgent urination; dysuria); suprapubic, perineal, or low back pain; s/s of infection; labs show infection
- Management: antibiotics; analgesics
- Pyelonephritis is infection of the kidneys. Symptoms can develop over hours or days, with some patients waiting weeks before seeking care.
- Diagnosis: clinical triad (fever, nausea and vomiting, costovertebral pain); cloudy, dark, foul-smelling urine; hematuria; dysuria; suprapubic, cervical, or uterine tenderness; urinalysis shows infection
- Management:IV fluids (D5W); antibiotics; analgesics; antipyretics; antiemetics
- A urinary tract infection (UTI) is infection in the lower urinary tract (bladder and urethra) or in the upper urinary tract (kidneys and ureters).
- Diagnosis: frequent small amounts of urine; cloudy, dark, foul-smelling urine; hematuria; dysuria; pelvic, suprapubic, abdominal, or lower back pain or pressure; s/s of infection; altered mental status in patients > 65 years old; urinalysis shows infection
- Management: antibiotics; supportive treatment for symptoms
Priapism
Priapism is an unintentional, prolonged erection that is unrelated to sexual stimulation and is unrelieved by ejaculation. Nonischemic (high-flow) priapism is the unregulated circulation of blood through the penis resulting from a ruptured artery in the penis or perineum, ischemic (low-flow) priapism occurs when blood becomes trapped in the erect penis. Ischemic priapism is con¬ sidered a medical emergency requiring immediate intervention to preserve function ofthe penis.
Risk Factors
- trauma (straddle injury or acute spinal cord injury)
- medications:
- antidepressants
- anticoagulants
- prostaglandin Ei
- testosterone
- underlying disease (e.g., sickle cell disease, leukemia, malaria)
- recent urologic surgery
- cocaine use
Physical Examination
- ischemic priapism: rigid, painful erection unrelated to sexual activity lasting > 4 hours
- nonischemic priapism:
- recurrent episodes of persistent erections (may be partial)
- difficulty maintaining full erection
- no pain
- trauma (usually straddle injury)
- delay between injury and priapism
Diagnostic Tests
- ultrasound showing obstructed or decreased blood flow
- venous blood gas dark or black
Management
- ischemic priapism: blood should be drained from the vents within 4-6 hours to prevent permanent damage
- first-line treatment: aspiration with intracavernosal phenylephrine injection
- second-line treatment: a shunt (T-shunt, Al-Ghorab s shunt, or Ebbehoj s shunt)
- penile prostheses for priapism lasting > 36 hours
- nonischemic priapism: the condition will often spontaneously resolve
- monitor
- first-line treatment, if needed: elective arterial embolization
Renal Calculi
Pathophysiology
Renal calculi (kidney stones) are hardened mineral deposits (most often calcareous) that form in the kidneys. Renal calculi are usually asymptomatic but will cause debilitating pain and urinary symptoms once they pass into the urinary tract, where they are referred to as urinary calculi.
Physical Examination
- severe, sharp, intermittent flank vain
- urinary symptoms (e.g., dysuria, hematuria)
- signs and symptoms of infection
Diagnostic Tests
CT scan to diagnose calculi
Management
- small stones (< 5 mm) with minimal symptoms: will pass spontaneously
- analgesics (may require opioids for severe pain)
- alpha-blockers (can help the stone pass)
- encourage fluids
- large stones (> 5 mm) with symptoms: surgical intervention
Testicular Torsion
Pathophysiology
Testicular torsion occurs when the spermatic cord, which supplies blood to the testicles, becomes twisted, leading to an ischemic testicle. The condition is considered a medical emergency that requires immediate treatment to preserve the function of the testicle. Most testicular torsion cases are caused by bell-clapper deformity, in which the testicle is not correctly attached to the tunica vaginalis.
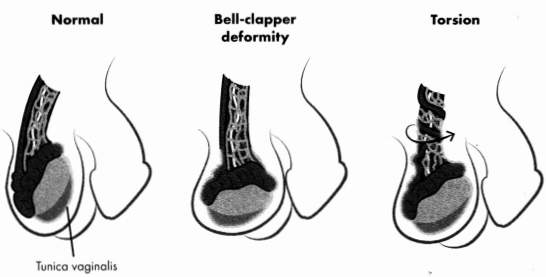
Figure 5.2. Testicular Torsion
Risk Factors
- male ages 10- 25
- bell-clapper deformity
- cold weather (especially sudden shift from warm to cold)
- trauma
Physical Examination
- sudden, severe unilateral scrotal vain
- high-riding testicle
- absent cremasteric reflex
- signs of inflammation in scrotal skin
Diagnostic Tests
ultrasound showing reduced or absent blood flow to affected testicle
Management
- analgesics
- prep for immediate exploratory surgery
Genitourinary Trauma
Pathophysiology
Genitourinary (GU) trauma can cause injury to the kidneys, bladder, urethra, or external genitalia. GU trauma symptoms can be nonspecific and can be masked by or related to other injuries. Trauma may occur from blunt or penetrating injury.
- Renal: The majority of renal trauma occurs from blunt trauma such as direct impact into the seatbelt or steering wheel in frontal MVCs or from body panel intrusion in side-impact crashes. Renal injuries are „ ranked graded from1 to 5 based on severity. Grade 5 renal injuries are referred to as shattered kidney and include severe renal vascular laceration.
- Bladder: The majority of bladder trauma occurs from blunt trauma, usually occurring with a pelvic fracture. Bladder rupture can also result from lap belt restraint. Leakage from ruptures may lead to peritonitis or sepsis.
- Urethral: Urethral injuries are more common in males and may result from trauma and pelvic fracture or from iatrogenic injuries resulting from catheterization.
- External genitalia: These injuries are more common in males due to anatomical presentation and greater participation in physical sports, acts of violence, and war. Up to two-thirds of all genitourinary traumas involve the external genitalia. Injuries to the penis and scrotum may occur from use of penile rings or other sexual pleasure devices.
Physical Examination
- pain (suprapubic, abdominal, groin/genital, or flank)
- urinary symptoms (e.g., hematuria, dysuria)
- bleeding at meatus
- ecchymosis
- distended bladder
- abdominal distention
- foul-smelling vaginal discharge
Diagnostic Tests
- urinalysis (for hematuria)
- decreased hemoglobin and hematocrit
- monitor for
- elevated BUN and creatinine
- fluid and electrolyte status
- diagnostic imaging (CT scan, KUB X-ray)
Management
- oxygen and IV fluids as needed
- analgesics as needed
- renal trauma may be admitted for monitoring (Hct, hemodynamic)
- keep bladder decompressed via Foley catheter (if no urethral injury present)
- manage sequelae (e.g, acute kidney injury, hemorrhage)
- penetrating injuries: surgical intervention
Urinary Retention
Pathophysiology
Urinary retention is the inability to void the bladder. The condition can be acute or chronic and is most often caused by either an obstruction (e.g., prostatic hyperplasia, organ prolapse) or an infection (e.g., prostatitis, vulvovaginitis). Acute urinary retention is a medical emergency that can result in bladder injuries, kidney infections, and sepsis if left untreated.
Physical Examination
- inability to urinate
- urinary frequency or urgency
- pelvic pressure or pain
Diagnostic Tests
renal/bladder ultrasound or CT scan to identify cause of retention
Management
- priority intervention: immediate voiding of bladder via catheter
- m treatment for underlying cause of retention after bladder is voided
Read More