Practicing with a variety of NCLEX PN Practice Questions exposes students to different question formats, such as multiple-choice and select-all-that-apply.
NCLEX Child with Dermatologic and Endocrine Health Problems Questions
Child with Dermatologic and Endocrine Health Problems NCLEX Practice Questions
Question 1.
A 17-year-old female with severe nodular acne is considering treatment with isotretinoin. What does the nurse instruct the client to do prior to beginning the medication?
(a) Enroll in a risk management plan.
(b) Have proof of a mental health evaluation.
(c) Begin an effective form of birth control with the first dose.
(d) Temporarily give up sports.
Answer:
(a) Enroll in a risk management plan.
Explanation:
Because of the risk of birth defects with isotretinoin, risk management plans require all clients to meet certain requirements to obtain the medication. Providers are advised to closely monitor clients for signs of depression, but a mental health evaluation is not universally required. It is not sufficient to begin a single form of effective method of birth control with the first dose of the medication.
Women of childbearing age must use two forms of effective birth control for 1 month before, during, and 1 month after taking the drug. Isotretinoin may cause muscle aches, and extreme exercise should be avoided, but general participation in sports should be considered on an individual basis.
Question 2.
When teaching an adolescent about measures to improve facial acne, the nurse should give the client what instructions about skin care?
(a) Wash the face twice a day with mild soap and water.
(b) Remove whiteheads and comedones after washing the face with antibacterial soap.
(c) Apply vitamin E ointment twice daily to the affected skin.
(d) Apply tretinoin daily in the morning and expose the face to the sun.
Answer:
(a) Wash the face twice a day with mild soap and water.
Explanation:
Washing the face once or twice a day with I a mild soap removes fatty acids from the skin. Acne is an inflammation of the sebaceous glands that produce sebum. Washing the face with mild soap and water keeps the sebaceous glands from becoming plugged. Excessive washing or squeezing the eruptions can cause rupture of these glands, spreading the sebum and causing further inflammation.
Applying vitamin E to the lesions does not reduce the inflammation and, due to the greasiness of the preparation, may plug the ducts. Isotretinoin should be applied at night. Exposure to the sun can result in sunburn and an increased risk of skin cancer and should be avoided. Sunscreen with a sun protection factor of at least 15 must be applied before the client can be exposed to the sun.
Question 3.
A 9-month-old infant with eczema has lesions that are secondarily infected. Which recommendation is the most appropriate to help the parents best meet the needs of the child?
(a) Prevent siblings from being in close contact.
(b) Send the child to day care as usual.
(c) Play video games for several hours each evening.
(d) Play with the child every day.
Answer:
(d) Play with the child every day.
Explanation:
The parents can best meet the needs of their 9-month-old infant by playing with the child every day. All infants need time with their parents to develop trust and thus attain optimal development. The parents of a child with a chronic problem may need more guidance to meet the child’s needs because of the focus on medical problems.
The child’s lesions are secondarily infected and therefore should not bo contagious. Siblings do not need lo slay away. Even with lesions that are infected, the child can still attend day care, but the child needs attention from the parents as well. Playing video games for several hours is not appropriate for a 9-month-old infant.
Question 4.
After the nurse teaches the mother of a child with atopic dermatitis how to bathe her child, which statement by the mother indicates effective teaching?
(a) “I let my child play in the tub for 30 minutes every night.”
(b) “My child loves the bubble bath I put in the tub.”
(c) “When my child gets out of the tub I just pat the skin dry.”
(d) “I make sure my child has a bath every night.”
Answer:
(b) “My child loves the bubble bath I put in the tub.”
Explanation:
Atopic dermatitis is a chronic pruritic dermatitis that usually begins in infancy. Many of the children diagnosed with it have a family history ps of eczema, allergies, or asthma. Atopic dermatitis ip is best treated with hydrating the skin, controlling the pruritus, and preventing secondary infection. Patting the skin dry removes less natural skin moisturizer and thus maintains skin hydration.
Playing in the tub for 30 minutes each night would deplete the skin of its natural moisturizers, thereby leading to increased pruritus and dry skin. Bubble baths are to be avoided in children with atopic dermatitis because they may act as an irritant, possibly exacerbating the condition. Also, bubble baths deplete the skin of its natural moisturizers. The issue is not whether the child bathes every night. Rather, the goal is to decrease dryness and itching.
Question 5.
A school-age child brought to the clinic with several superficial sores on the front of the left leg is diagnosed with impetigo. Which instructions should the nurse give the parent?
(a) Wash the child’s legs once a day with a mild soap.
(b) Cover the sores with loose gauze.
(c) Allow the child to go back to school after 24 hours of treatment.
(d) Have the child return in 1 week for a followup examination.
Answer:
(c) Allow the child to go back to school after 24 hours of treatment.
Explanation:
Impetigo involving several superficial lesions is usually treated topically, including washing the affected areas, removing crusts, and applying antibiotic ointment several times a day. The child can return to day care or school after being treated for 24 hours. The lesions do not need to be cov-ered, and they can remain open to the air. There is no need for follow-up unless the lesions have not resolved or have become more severe.
Question 6.
When developing the teaching plan for the mother of a toddler diagnosed with scabies, what information should the nurse expect to include?
(a) Disinfect all hard surfaces in the home.
(b) The child should be held frequently.
(c) Itching should cease in a few days.
(d) The entire family should be treated.
Answer:
(d) The entire family should be treated.
Explanation:
Scabies is caused by the scabies mite, Sarcoptes scabiei. The mite burrows into the stratum corneum of the epidermis, where the female deposits eggs and fecal material. These burrows are linear. Scabies is highly contagious. The length of time from infestation to physical symptoms is 30 to 60 days, so everyone in close contact with the child will need to be treated.
The bed linens and the child’s clothing should be washed in hot water and dried in a hot setting. Disinfect all hard surfaces to prevent the spread of scabies. The child should be held minimally until treatment is completed. Family members should wash their hands after contact with the child. Itching lasts for 2 to 3 weeks until the stratum corneum is replaced.
Question 7.
A school-age child has just spilled hot liquid on his arm, and a 4-inch (10-cm) area on his forearm is severely burned. His mother calls the emergency department. What should the nurse advise the mother to do?
(a) Keep the child warm.
(b) Cover the burned area with an antibiotic cream.
(c) Apply cool water to the burned area.
(d) Call 911 to transport the child to the hospital.
Answer:
(c) Apply cool water to the burned area.
Explanation:
To prevent further injury to the skin, the mother should apply cool water to the burn site. Doing so causes vasoconstriction, retards further damage to tissues, and decreases fluid loss. Keeping the child warm promotes vasodilation, increases fluid loss, and decreases blood pressure and, thus, circulation to the area.
Applying ointment to the burn is contraindicated because it does not allow healing to occur and may need to be removed in the hospital. Only a clean cloth should be used to cover the wound to prevent contamination or decrease pain or chilling. If only the arm is burned, a call to 911 for emergency care is not necessary, but the mother should seek health care services immediately.
Question 8.
A school-age child who has received burns over 60% of his body is to receive 2,000 mL of IV fluid over the next 8 hours. At what rate (in milliliters per hour) should the nurse set the infusion pump? Round your answer to a whole number ................... mL/h.
Answer:
250 mL/h
Explanation:
2,000 mL + 8h = 250 mL/h
Question 9.
Which interventions would be most appropriate to institute when a school-age child with burns becomes angry and combative when it is time to change the dressings and apply mafenide acetate?
(a) Ensure parental support during the dressing changes.
(b) Allow the child to assist in removing the dressings and applying the cream.
(c) Give the child permission to cry during the procedure.
(d) Allow the child to schedule the time for dressing changes.
Answer:
(b) Allow the child to assist in removing the dressings and applying the cream.
Explanation:
Expressions of anger and combativeness are often the result of a loss of control and a feeling of powerlessness. Some control over the situation is regained by allowing the child to participate in care. Although having parental support during the dressing changes may be helpful, this action does nothing to allow the child control. Giving the child permission to cry may help with verbalizing feelings, but doing so does nothing to provide the child with control over the situation.
Although allowing the child to determine the time for dressing changes may provide a sense of control over the situation, doing so is inappropriate because the dressing changes need to be performed as prescribed to ensure effectiveness and healing.
Question 10.
A school-age child with burns on the trunk and arms has no appetite. The nurse and the parent develop a plan of care to stimulate the child’s appetite. Which suggestion made by the parent would indicate the need for additional teaching?
(a) deciding that she will feed the child herself
(b) withholding dessert and treats unless meals are eaten
(c) offering the child finger foods that the child likes
(d) serving smaller and more frequent meals
Answer:
(b) withholding dessert and treats unless meals are eaten
Explanation:
Withholding certain foods until the child complies is punitive and rarely successful. Allowing the mother to feed the child, serving smaller and more frequent meals, and offering finger foods are all acceptable interventions for a 5-year-old child. This is true whether the child is well or ill.
Question 11.
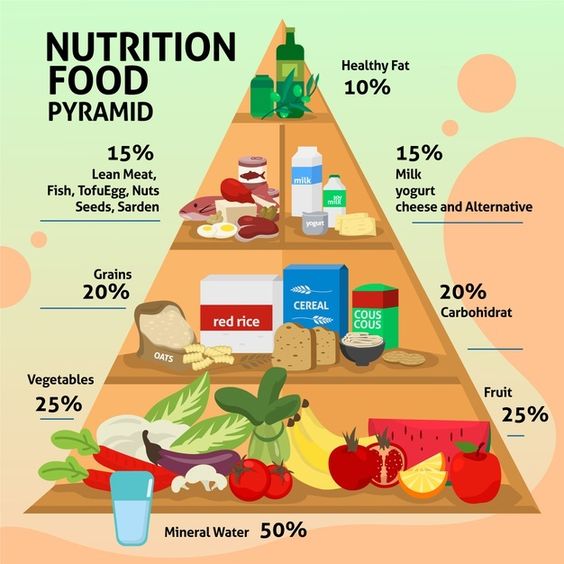
The nurses teaches the parent of a child with severe burns about the importance of specific nutritional support in burn management. The nurse recognizes the need for more teaching if the parents select which food for their child?
(a) bacon, lettuce, and tomato sandwich; milk and celery and carrot sticks
(b) cheeseburger; cottage cheese and pineapple salad; chocolate milk; and a brownie
(c) chicken nuggets; orange and grapefruit sections; and a vanilla milkshake
(d) beef, bean, and cheese burrito; a banana; fruit-flavored yogurt; and skim milk
Answer:
(a) bacon, lettuce, and tomato sandwich; milk and celery and carrot sticks
Explanation:
Hypoproteinemia is common after severe bums. The child’s diet should be high in protein to compensate for protein loss and to promote tissue healing. The child will also require a diet that is high in calories and rich in iron. The menu of bacon, lettuce, and tomato sandwich; milk; and celery sticks is lacking in sufficient protein and calories.
Question 12.
The nurse is caring for a child with moderate burns from the waist down. Which measure should the nurse implement when positioning the child?
(a) Place the child in a position of comfort.
(b) Allow the child to lie on the abdomen.
(c) Ensure the application of leg splints.
(d) Have the child flex the hips and knees.
Answer:
(c) Ensure the application of leg splints.
Explanation:
A child with moderate burns is at high risk for contractures. A position of comfort would encourage contracture formation. Therefore, splints need to be applied to maintain proper positioning and joint function, thereby preventing contractures and loss of function. Allowing the child to lie on the abdomen or with the hips and knees flexed often encourages contracture formation.
Question 13.
An adolescent is to receive radioactive iodine for Graves’ disease. Which statement by the client reflects the need for more teaching?
(a) “I plan to spend more time using social media since I have to keep several feet (meters) from my friends for 3 days.”
(b) “Taking radioactive iodine will not affect my ability to have children in the future.”
(c) “The advantage of radioactive iodine is that I will not need future medication for my disease.”
(d) “I should try to use a separate bathroom from the rest of my family for several days.”
Answer:
(c) “The advantage of radioactive iodine is that I will not need future medication for my disease.”
Explanation:
Most clients will need lifelong thyroid replacement after treatments with radioactive iodine. Most clients are treated as outpatients. To reduce the risk of exposure to radioactivity to others, clients are advised to avoid public places for at least 1 day and maintain a prudent distance from others for 2 to 3 days. Additionally, clients are advised to avoid close contact with pregnant women and children for 5 to 11 days.
The use of radioiodine to treat Graves’ disease has not been found to affect long-term fertility. Clients are taught not to share food, utensils, and towels. Use of a private bathroom is desirable. Clients are also instructed to flush the toilet more than one time after each use.
Question 14.
Which clinical manifestations would lead the nurse to suspect that an infant has hypothyroidism? Select all that apply.
(a) cool extremities
(b) increased appetite
(c) muscle weakness
(d) lethargy
(e) tachycardia
(f) bulging eyes
Answer:
(a) cool extremities
(b) increased appetite
(c) muscle weakness
(d) lethargy
Explanation:
(a), (b), (c), (d) Hypothyroidism is a disorder in which the levels of active thyroid hormone are decreased. Clinical manifestations include cool extremities, mottling, lethargy, constipation, muscle weakness, and a hoarse cry. Hyperthyroidism occurs when thyroid hormone levels are increased. Clinical manifestations include increased appetite, goiter, irritability, prominent eyes, and tachycardia.
Question 15.
What instructions should the nurse give to the family of a child with newly diagnosed hyperthyroidism?
(a) Keep their home warmer than usual.
(b) Encourage plenty of outdoor activities.
(c) Promote interactions with one friend instead of groups.
(d) Limit bathing to prevent skin irritation.
Answer:
(c) Promote interactions with one friend instead of groups.
Explanation:
Children with hyperthyroidism experience emotional lability that may strain interpersonal relationships. Focusing on one friend is easier than adapting to group dynamics until the child’s condition improves. Because of their high metabolic rate, children with hyperthyroidism feel too warm. Bright sunshine may be irritating because of disease-related ophthalmopathy. Sweating is common, and bathing should be encouraged.
Question 16.
A school-age child has been diagnosed with Graves’ disease and is to start drug therapy. Which instruction should the nurse include in the teaching plan for the child’s parent and teacher?
(a) Continue with the same amount of school-work and homework.
(b) Understand that mood swings are rare with this disorder.
(c) Limit the amount of food that is offered to the child.
(d) Provide the child with a calm, nonstimulating environment.
Answer:
(d) Provide the child with a calm, nonstimulating environment.
Explanation:
Because it takes approximately 2 weeks before the response to drug treatment occurs, much of the child’s care focuses on managing the child’s physical symptoms. Signs and symptoms of the disorder include inability to sit still or concentrate, increased appetite with weight loss, emotional lability, and fatigue. Nursing care is directed toward ensuring that the mother and teacher know how to handle the child and suggesting a shortened school day, a nonstimulating environment, and decreased stress and workload. The child should be encouraged to eat a well-balanced diet.
Question 17.
A student with type 1 diabetes tells the nurse she is feeling light-headed. The student’s blood sugar is 60 mg/dL (3.3 mmol/L). Using the 15-15 rule, what should the nurse do to treat the blood glucose?
(a) Administer 15 mL of juice, and give another 15 mL in 15 minutes.
(b) Administer 15 g of carbohydrate, and retest the blood sugar in 15 minutes.
(c) Administer 15 g of carbohydrate and 15 g of protein.
(d) Administer 15 oz of juice, and retest in 15 minutes.
Answer:
(b) Administer 15 g of carbohydrate, and retest the blood sugar in 15 minutes.
Explanation:
The 15-15 rule is a general guideline for treating hypoglycemia where the client consumes 15 g of carbohydrate and repeats testing the blood sugar in 15 minutes. Fifteen grams of carbohydrate equals 60 calories and is roughly equal to Vz cup (120 mL) of juice or soda, six to eight Life Savers, or a tablespoon of honey or sugar. The general recommendation is if the blood sugar is still low, the client may repeat the sequence.
Fifteen milliliters of juice would only provide 8 calories. This would not be sufficient carbohydrates to treat the hypoglycemia. Protein does not treat insulin-related hypoglycemia; however, a protein-starch snack may be offered after the blood glucose improves. Fifteen ounces of juice would be approximately 440 mL almost four times the recommended 4 oz (120 mL) of juice.
Question 18.
An overweight adolescent has been diagnosed with type 2 diabetes. What should the nurse do to increase the client’s self-efficacy to manage the disease?
(a) Provide the client with a written daily food and exercise plan.
(b) Discuss eliminating junk food in the home with the parents.
(c) Arrange for the school nurse to weigh the child weekly.
(d) Utilize a peer with type 2 diabetes to role model lifestyle changes.
Answer:
(d) Utilize a peer with type 2 diabetes to role model lifestyle changes.
Explanation:
Self-efficacy, or the belief that one can act in a way to produce a desired outcome, can be promoted through the observation of role models. Peers are particularly effective role models because clients can more readily identify with them and believe they are capable of similar behaviors. Providing a written plan alone does not promote self-efficacy. Having parents eliminate junk food and having the school nurse weigh the adolescent can be part of the plan, but these actions do not empower the client.
Question 19.
After 6 months of treatment with diet and exercise, an adolescent with type 2 diabetes still has a fasting blood glucose level of 140 mg/dL (7.8 mmol/L). The health care provider (HCP) has decided to begin metformin. The client asks how the medication works. The nurse should tell the client that the medicine decreases glucose production and performs which other function?
(a) replaces natural insulin
(b) helps the body make more insulin
(c) increases insulin sensitivity
(d) decreases carbohydrate adsorption
Answer:
(c) increases insulin sensitivity
Explanation:
Metformin is currently approved by the FDA and Health Canada to treat type 2 diabetes in children. The medication decreases glucogenesis in the liver and increases insulin sensitivity in the peripheral tissues. Only insulin can actually replace insulin. This treatment is reserved for clients with type 1 diabetes or those with type 2 who do not respond to diet, exercise, and an oral diabetic agent. Other oral medications used to treat diabetes augment insulin production or decrease carbohydrate absorption, but those medications are primarily used in adults.
Question 20.
The nurse is evaluating a child’s skills in self-administering insulin (see figure) What should the nurse do?
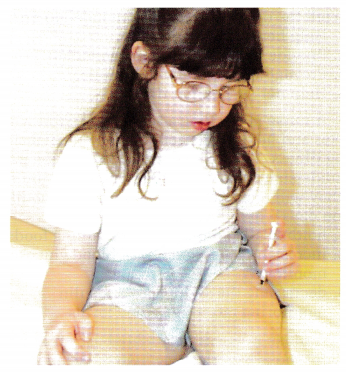
(a) Have the child use both hands on the syringe.
(b) Ask the child to place the needle at a 45-degree angle.
(c) Tell the child to use a site lower on her thigh.
(d) Remind the child to rotate sites.
Answer:
(d) Remind the child to rotate sites.
Explanation:
The child is using the correct injection technique, and the nurse can remind the child to rotate sites. The nurse should also reinforce that the child has used the correct technique and praise the child for doing so. If the child can manipulate the plunger of the syringe with one hand, this is appropriate.
Insulin is administered at a 90-degree angle as shown. The child should identify appropriate sites on the thighs as one handbreadth below the hip and above the knee; the child is using appropriate sites.
Question 21.
An adolescent client is using glargine and lispro to manage type 1 diabetes. The nurse reviews the prescription for sliding scale lispro (see exhibit).
Important notes:
Lispro subcutaneous give units according to sliding scale:
- Blood glucose: 70-150 mg/dL
- (3.9-8.3 mmol/L) = 0 units
- 151-200 mg/dL (8.4-11.1 mmol/L) = 1 unit
- 201-250 mg/dL (11.2-13.9 mmol/L) = 2 units
- 251-300 mg/dL (13.93-16.65 mmol/L) = 3 units
- 301-350 mg/dL (17-19.4 mmol/L) = 4 units
- Call for blood glucose > 350 (19.4 mmol/L)
- In addition give 1 unit for every 15 g of carbohydrate.
The morning blood glucose is 202 mg/dL (11.2 mmol/L), and the client is going to eat two carbohydrate exchanges. The nurse has the client administer how many units of lispro? ...................... units. Round your answer to a whole number.
Answer:
301-350 mg/dL (17-19.4 mmol/L) = 4 units
Explanation:
Four units. Each carbohydrate food exchange has 15 g of carbohydrate. Two units are needed to cover the current blood glucose, and 2 units are needed to cover the anticipated carbohydrate intake.
Question 22.
A school-age client with diabetes is placed on an intermediate-acting insulin and regular insulin before breakfast and before dinner. She will receive a snack of milk and cereal at bedtime. What does the nurse tell the client the snack is intended to do?
(a) Help her regain lost weight.
(b) Provide carbohydrates for immediate use.
(c) Prevent late night hypoglycemia.
(d) Help her stay on her diet.
Answer:
(c) Prevent late night hypoglycemia.
Explanation:
Intermediate-acting insulin peaks in 6 to 8 hours, which would occur during sleep. A bedtime snack is needed to prevent late-night hypoglycemia. The snack is not given to help regain weight. Milk contains fat and protein, which cause delayed absorption into the bloodstream and also maintain the blood glucose level at night when the intermediate-acting insulin will peak. The snack is not used to provide carbohydrates for immediate use because an intermediate-acting insulin, unlike regular insulin, does not peak immediately. The snack has nothing to do with a diet.
Question 23.
A nurse is teaching a school-age child with diabetes and her parents about managing diabetes during illness. The nurse determines that the parents understand the instruction when they indicate that they will make which treatment plan modification on days when the child is ill.
(a) holding all carbohydrate-containing foods
(b) increasing the frequency of blood glucose monitoring
(c) decreasing the sliding scale of insulin
(d) monitoring morning ketone levels
Answer:
(b) increasing the frequency of blood glucose monitoring
Explanation:
During an illness, cells become more insulin resistant, increasing the risk for hyperglycemia. Clients are advised to check their blood glucose more frequently, as often as every 2 to 3 hours. Clients should continue to take their insulin and are likely to need more during illness to achieve a normal blood glucose level.
Simple carbohydrates are often the nutrient source best tolerated if nausea is present, and clients must consume sufficient amounts of carbohydrates to prevent burning fat. Clients are advised that they should check blood or urine ketones every 4 hours to ensure they are not developing ketoacidosis.
Question 24.
A nurse is assessing a school-age child with diabetes who is experiencing hyperglycemia. Which symptoms indicate that the hyperglycemia requires immediate intervention? Select all that apply.
(a) weakness
(b) thirst
(c) shakiness
(d) hunger
(e) headache
(f) dizziness
Answer:
(a) weakness
(b) thirst
(f) dizziness
Explanation:
(a), (b), (f) Weakness, thirst, and dizziness are symptoms related to dehydration caused by excretion of large amounts of glucose and water in the urine. The nurse should notify the health care provider (HCP) JJ3- Shakiness, hunger, headache, and irritability are related to hypoglycemia and result from the brain and other cells being starved for nutrients.
Question 25.
The nurse talks to an adolescent about how she can tell her friends about her new diagnosis of diabetes. Which behavior by the adolescent indicates that the adolescent has responded positively to the discussion?
(a) She asks the nurse for material on diabetes for a school paper.
(b) She introduces the nurse to her friends as “the one who taught me all about my diabetes.”
(c) She says, “I will try to tell my friends, but they will probably quit hanging out with me.”
(d) She asks her friends what they think about someone who has a lifelong illness.
Answer:
(b) She introduces the nurse to her friends as “the one who taught me all about my diabetes.”
Explanation:
The ability to talk about her diabetes indicates that the adolescent feels good enough about herself to share her problem with her peers. Asking for reference material does not specifically indicate that the client’s self-esteem has improved or that she has accepted her diagnosis. Saying that her friends will probably desert her if she tells them about the illness indicates that the adolescent still needs to work on her self-esteem and her feelings about the disease.
Asking her friends what they think of someone with a lifelong illness would not indicate that the nurse’s interventions targeted toward improving self-esteem have been successful. Rather, this statement demonstrates the adolescent’s uncertainty about herself.
Question 26.
An adolescent with insulin-dependent diabetes is being taught the importance of rotating the sites of insulin injections. The nurse should judge that the teaching was successful when the adolescent identifies which complication that can result from using the same site?
(a) destruction of the fat tissue and poor absorption
(b) damage to nerves and painful neuritis
(c) thickening of the subcutis and too-rapid insulin uptake
(d) development of resistance to insulin and the need for increased amounts
Answer:
(a) destruction of the fat tissue and poor absorption
Explanation:
Repeated use of the same injection site can result in atrophy of the fat in the subcutane¬ous tissue and lead to poor insulin absorption. The neuritis that develops from diabetes is related to microvascular changes that occur. Subcutaneous tissue may thicken and harden, but this leads to decreased, not rapid, insulin absorption. Resistance to insulin is caused by an immune response to the insulin protein.
Question 27.
An adolescent has been diagnosed with polycystic ovarian syndrome (PCOS). Which statement by the adolescent indicates the need for more teaching?
(a) “High levels of male hormones contribute to my PCOS.”
(b) “I am at risk for type 2 diabetes.”
(c) “Maintaining a healthy weight is an important part of my treatment plan.”
(d) “Untreated PCOS will make getting pregnant impossible.”
Answer:
(d) “Untreated PCOS will make getting pregnant impossible.”
Explanation:
While pregnancy may be difficult for some clients, the nurse must work to prevent the false conception that a sexually active teen with PCOS does not need to use a reliable form of birth control. PCOS is associated with high levels of androgens and excessive insulin. It is the excess insulin that is thought to increase androgen production. Clients with PCOS are at risk for type 2 diabetes. Initial treatment focuses on weight management and exercise. These measures often reduce insulin production and restore normal menstrual cycles.
Question 28.
An adolescent female client suspects that she might have polycystic ovarian syndrome (PCOS). Which symptoms would be consistent with PCOS? Select all that apply.
(a) primary amenorrhea
(b) obesity
(c) increased body hair
(d) acne
(e) darkened skin in body fold
(f) enlarged breast
Answer:
(b) obesity
(c) increased body hair
(d) acne
(e) darkened skin in body fold
Explanation:
(b), (c), (d), (e) PCOS is associated with obesity, increased body or facial hair (hirsutism), acne, and darkening of the skin usually in body folds (acanthosis nigricans). When a female has never had a menstrual cycle, it is referred to as primary amenorrhea. PCOS is associated with irregular menstrual cycles and/or secondary amenorrhea, not primary amenorrhea. High androgen levels frequently lead to decreased versus enlarged breast size.
Question 29.
An adolescent client with polycystic ovarian syndrome (PCOS) has been placed on metformin. The nurse determines the client needs more teach¬ing about metformin if she states the medication helps achieve which outcome?
(a) reduced androgen levels
(b) normalization of the menstrual cycle
(c) increased insulin levels
(d) reduced blood glucose levels
Answer:
(c) increased insulin levels
Explanation:
Metformin works by decreasing the production of glucose in the liver and improving insulin sensitivity. These two mechanisms reduce insulin and blood glucose level. Reducing insulin levels reduces androgens and helps to restore menstruation.
Question 30.
An adolescent female with polycystic ovarian syndrome (PCOS) is extremely upset, saying, “I’m so embarrassed by hair on my face. I just don’t fit in.” Which intervention is most needed?
(a) Refer the client to a hair removal specialist.
(b) Screen the client for depression.
(c) Provide more information on causes and treatment options.
(d) Suggest the client join a support group.
Answer:
(b) Screen the client for depression.
Explanation:
Many clients with PCOS suffer from depression. As depression is associated with a significant risk of suicide, the priority would be to determine if the client has symptoms of depression requiring further evaluation and treatment.
Referrals to a hair removal specialist and possibly a support group would be appropriate, but only after determining if the client needs a referral for a major mood disorder. Providing more information on causes and treatment options is better saved for when the client is less distraught.
Question 31.
The parent of a 17-year-old client, who is hospitalized for complications related to type 1 diabetes, requests to review the adolescent’s medical record. The client reported receiving mental health counseling during the admission history but did not want his parent to know. The nurse is uncertain of how to protect the adolescent’s privacy and accommodate the parent’s request. Who is the most appropriate person to consult?
(a) the unit nurse manager
(b) the health care provider (HCP)
(c) the organization’s privacy officer
(d) the customer service representative
Answer:
(c) the organization’s privacy officer
Explanation:
Confidentiality legislation specifies that institutions designate a “privacy officer” who is responsible for developing and implementing privacy policies. This would be the very best resource for the nurse to contact. Depending on the nurse manager’s experience, he or she may or may not know the answer and may have to consult the privacy officer.
While HCPs would have an understanding of confidentiality laws, it is unlikely they understand the specifics of nursing policies. The customer service representatives typically address client concerns or complaints. At this time, the family has not voiced a complaint.
Question 32.
The charge nurse on the pediatric floor has assigned a 6-year-old girl with newly diagnosed type 1 diabetes and an 8-year-old girl recovering from ketoacidosis to the same semi-private room. The 6-year-old’s mother is upset because the parent staying with the other child is male, and the mother believes the arrangement violates her social norms. What should the nurse do?
(a) Explain to the parents that this room arrangement facilitates teaching.
(b) Reassign the children to different rooms.
(c) Offer the parent another place to sleep.
(d) Refer the parent to the customer service representative.
Answer:
(b) Reassign the children to different rooms.
Explanation:
Sleeping in the same room with a person of the opposite sex may be viewed as a violation of norms by persons of conservative faiths. If at all possible, the charge nurse should reassign the family to a different room. While it makes sense to have two clients with similar educational needs in the same room, it is likely that the arrangement would be distressing enough to create a learning barrier.
Offering the mother another place to sleep deprives the child of her parent at night. The customer service representative would only need to be involved if it became impossible to accommodate the mother’s needs.
Question 33.
A school-age client with type 1 diabetes is sick with the flu. What is the most important information for the nurse to convey regarding diabetes management during illness?
(a) Blood glucose needs to be checked more frequently during illness.
(b) Children require less insulin when they are sick with the flu.
(c) Urine ketones should be checked every other day during illness.
(d) Increase intake of fluids high in carbohydrates to prevent diarrhea.
Answer:
(a) Blood glucose needs to be checked more frequently during illness.
Explanation:
Blood sugar levels can go up during the flu; therefore, blood glucose levels should be monitored every 3 to 4 hours during the flu. Because glucose levels are higher when a client has the flu, clients should continue to take diabetes medications as prescribed. If the blood sugar level is over 240 mg/dL, ketones should be checked. If ketones are present, the client should be encouraged to drink calorie-free fluids and eat small meals.
Question 34.
Which nursing intervention should be done first when managing a pediatric client admitted to the emergency department with severe diabetic ketoacidosis (DKA)?
(a) Begin an insulin drip to lower the client’s blood glucose level.
(b) Correct any fluid deficit using an isotonic saline solution.
(c) Draw a blood glucose level and serum electrolyte panel.
(d) Secure the client’s airway to ensure adequate ventilation.
Answer:
(d) Secure the client’s airway to ensure adequate ventilation.
Explanation:
Treating pediatric clients with severe DKA is a medical emergency; therefore, attending to the airway, breathing, and circulation is the first priority. Once the airway is secured, the health care team should estimate the level of dehydration and begin replacement fluids of normal saline. An insulin drip should be started after the initial 1 to 2 hours of treatment at a rate of 0.1 units/kg/h. Blood glucose should be tested every 1 to 2 hours until the client is stable, then it should be every 6 hours. Additionally, serum electrolytes should be drawn every 1 to 2 hours until the client is stable, then every 4 to 6 hours.
Question 35.
The parent of a school-age client with diabetes tells the nurse that she does not want the school to know about her daughter’s condition. Which is the nurse’s best response?
(a) “Our office will not discuss your daughter’s diabetes with the school without your written permission.”
(b) “What is it that concerns you about having the school know about your daughter’s condition?”
(c) “It would be fine not to tell your daughter’s friends, but the teacher must know.”
(d) “In order to keep your daughter safe, it is necessary for all adults in the school to know her condition.”
Answer:
(b) “What is it that concerns you about having the school know about your daughter’s condition?”
Explanation:
The nurse’s first response should be to obtain more information about the mother’s concerns. The nurse can then facilitate a dialogue that will help the mother weigh her concerns against the potential risks to the child’s safety. It is true that the nurse would not discuss a client’s medical condition with a school without permission, but this statement does facilitate discussion.
It is also true that the child may have a diabetic reaction anywhere at school, and it is advisable that her teacher, classmates, and other adults know about her diabetes in order to help her; however, it is ultimately the client and her parents who will make the decision about informing the school. Dictating to the mother does not explain any rationale for the necessity of sharing the information.
Question 36.
The nurse reviews the plan of care of an adolescent client with diabetes using an insulin pump. This is the second visit that the client has come without his parent. The client’s hemoglobin AlC and blood glucose levels are normal. The client reports that he is playing a sport and has not had any hypoglycemic episodes. Which factor does the nurse determine is the best indicator that the client is transitioning to independent self-management?
(a) managing an insulin pump
(b) attending health care appointments alone
(c) having normal hemoglobin AlC and blood glucose levels
(d) playing sports without hypoglycemic episodes
Answer:
(b) attending health care appointments alone
Explanation:
During adolescence, the responsibility for chronic disease management is shared. As clients transition to adulthood, they assume more responsibility for their care. Attending appointments alone shows that the client is developing the decisionmaking skills needed to interact with the health care team without parental assistance. School-age children are often able to manage an insulin pump because they have developed the logical reasoning required to follow protocols.
Having normal hemoglobin AlC and blood glucose levels is positive, but the nurse does not know what role the parents may have played in the client’s management. The nurse would also not know if a coach or trainer played a significant role in reminding the client to monitor glucose needs during sports.