NCLEX Study Guide are an invaluable resource for nursing students striving to master the content required for their licensure exam.
NCLEX Cancer Questions - NCLEX Questions on Cancer
Cancer NCLEX Practice Questions
Question 1.
Which client is at highest risk for colorectal cancer?
The client:
(a) who smoked 1 pack a day for 30 years
(b) who follows a vegetarian diet
(c) who has been treated for Crohn’s disease for 20 years
(d) with a family history of lung cancer
Answer:
(c) who has been treated for Crohn’s disease for 20 years
Explanation:
Clients over age 50 who have a history of inflammatory bowel disease are at risk for colon cancer. The client who smokes is at high risk for lung cancer. While the exact cause is not always known, other risk factors for colon cancer are a diet high in animal fats, including a large amount of red meat and fatty foods with low fiber, and the presence of colon cancer in a first-generation relative.
Question 2.
A nurse is conducting a cancer risk screening program. Which client is at greatest risk for skin cancer?
(a) a 45-year-old health care worker
(b) a 15-year-old high school student
(c) a 30-year-old butcher
(d) a 60-year-old mountain biker
Answer:
(d) a 60-year-old mountain biker
Explanation:
Basal cell carcinoma occurs most commonly in sun-exposed areas of the body. The incidence of skin cancer is highest in older people who live in the mountains or spend outdoor leisure time at higher altitudes.
Question 3.
A client diagnosed with testicular cancer expresses concerns about fertility. The client and his spouse desire to eventually have a family, and the nurse discusses the option of sperm banking. What should the nurse tell the couple about the best time to donate the sperm?
(a) before treatment is started
(b) once the client tolerates the treatment
(c) upon completion of treatment
(d) when tumor markers drop to normal levels
Answer:
(a) before treatment is started
Explanation:
Because of the high risk of infertility with chemotherapy, pelvic irradiation, and retroperitoneal lymph node dissection that may follow an orchiectomy, cryopreservation of sperm is completed before treatment is started and should be discussed with the client.
Question 4.
A nurse is planning an educational program about cancer prevention and detection. Which group would benefit most from education regarding potential risk factors for melanoma?
(a) adults older than age 35
(b) senior citizens who have been repeatedly exposed to the effects of ultraviolet A and ultraviolet B rays
(c) parents with children
(d) employees of a chemical factory
Answer:
(c) parents with children
Explanation:
Sun damage is a cumulative process. Parents should be taught to apply sunscreen and teach their children to use sunscreen at an early age. Although preventive education is always valuable, serious sunburns in childhood are associated with an increased risk of melanoma. Adults and senior citizens have already been exposed to the harmful effects of the sun and, although they, too, should use sunscreen, they are not the group that will most benefit from intervention. Exposure to chemicals is not a risk factor for melanoma.
Question 5.
A nurse is providing education in a community setting about general measures to avoid excessive sun exposure. Which recommendation is appropriate?
(a) Use sunscreen only after going into the water.
(b) Avoid peak exposure hours from 0900 to 1300.
(c) Wear loosely woven clothing for added ventilation.
(d) Apply sunscreen with a sun protection factor (SPF) of 15 or more before sun exposure.
Answer:
(d) Apply sunscreen with a sun protection factor (SPF) of 15 or more before sun exposure.
Explanation:
A sunscreen with an SPF of 15 or higher should be worn on all sun-exposed skin surfaces. It should be applied before sun exposure and reapplied after being in the water. Peak sun exposure usually occurs from 0010 to 1400. Tightly woven clothing, protective hats, and sunglasses are recommended to decrease sun exposure. Sun tanning parlors should be avoided.
Question 6.
A 29-year-old woman is concerned about her personal risk factors for malignant melanoma. She is upset because her 49-year-old sister was recently diagnosed with the disease. After gathering information about the client’s history of sun exposure, what should the nurse tell the client?
(a) Some melanomas have a familial component, and she should seek medical advice.
(b) Her personal risk is low because most melanomas occur at age 60 or later.
(c) Her personal risk is low because melanoma does not have a familial component.
(d) She should not worry because she did not experience severe sunburn as a child.
Answer:
(a) Some melanomas have a familial component, and she should seek medical advice.
Explanation:
Malignant melanoma may have a familial basis, especially in families with dysplastic nevi syndrome. First-degree relatives should be monitored closely. Malignant melanoma occurs most often in the 20- to 45-year-old age group. Severe sunburn as a child does increase the risk; however, this client is at increased risk because of her family history.
Question 7.
A client with a family history of cancer asks the nurse what the single most important risk factor is for cancer. Which risk factor should the nurse discuss?
(a) family history
(b) lifestyle choices
(c) age
(d) menopause or hormonal events
Answer:
(c) age
Explanation:
Because more than 50% of the cancers occur in people who are older than age 65, the single most important factor in determining risk would be age.
Question 8.
A 42-year-old female highway construction worker is concerned about her cancer risks. She has been married for 18 years, has two children, smokes one pack of cigarettes per day, and occasionally drinks one to two beers. She is 30 lb (13.6 kg) overweight, eats fried fast food often, and rarely eats fresh fruits and vegetables. Her mother was diagnosed with breast cancer 2 years ago. Her father and an aunt both died of lung cancer. She had a basal cell carcinoma removed from her cheek 3 years earlier. What behavioral changes should the nurse coach this client to make to decrease her risk of cancer? Select all that apply.
(a) Improve nutrition.
(b) Decrease alcohol consumption.
(c) Use sunscreen.
(d) Stop smoking.
(e) Lose weight.
(f) Change her job to work inside.
Answer:
(a) Improve nutrition.
(c) Use sunscreen.
(d) Stop smoking.
(e) Lose weight.
Explanation:
(a), (c), (d), (e). The client is at increased risk for the development of lung, skin, or breast cancer. Consequently, the client should improve nutrition (e.g., eating food with lower animal fat content, increasing fiber, adding fruits and vegetables to the diet), stop smoking, use sunscreen, and lose weight. The client’s alcohol consumption is not excessive and not a risk. It is not necessary and would be difficult for the client to change jobs to work inside as long as the client uses protection from the sun.
Question 9.
The nurse is assessing a 60-year-old who has hoarseness and a chronic sore throat. What should the nurse determine while conducting a health history with this client? Select all that apply.
(a) use of acetaminophen
(b) exposure to sun
(c) consumption of a high-fat diet
(d) extent of tobacco use
(e) amount of alcohol consumption
Answer:
(d) extent of tobacco use
(e) amount of alcohol consumption
Explanation:
(d), (e). Hoarseness and chronic sore throat are indicative of cancer of head and neck cancers, particularly cancer of the pharynx. Tobacco use and heavy consumption of alcohol are risk factors for these cancers and may have a synergistic effect. Heavy use of acetaminophen is not a risk factor for head and neck cancer, but it is related to liver failure. Exposure to the sun increases the risk of skin cancers, but not cancers of the head and neck. Consuming a high-fat diet is not related to head and neck cancer, but it may be a risk factor for other cancers and heart disease. Exposure to wood dust and other inhaled particles is associated with lung cancer.
Question 10.
A 42-year-old is interested in making dietary changes to reduce the risk of colon cancer. What dietary selections should the nurse suggest?
(a) croissant, granola and peanut butter squares, whole milk
(b) bran muffin, skim milk, stir-fried broccoli
(c) granola, bagel with cream cheese, cauliflower salad
(d) oatmeal raisin cookies, baked potato with sour cream, turkey sandwich
Answer:
(b) bran muffin, skim milk, stir-fried broccoli
Explanation:
High -fiber, low-fat diets are recommended to reduce the risk of colon cancer. Stir-frying, poaching, steaming, and broiling are all low-fat methods to prepare foods. Croissants are made of refined flour. They are also high in fat, as are peanut butter squares and whole milk, granola, cream cheese, and sour cream.
Question 11.
The nurse is conducting a cancer risk assessment for a middle-aged client. Which risk factor is appropriate for motivational interviewing for this client as an approach to risk reduction?
(a) gender
(b) nutrition
(c) family history
(d) age
Answer:
(b) nutrition
Explanation:
Motivational interviewing is a technique used to guide clients to make changes in their behavior. A client’s diet and nutritional status can be changed. Gender, family history for cancer, and age are risk factors that cannot be changed.
Question 12.
A client at risk for lung cancer asks about the reason for having a computed tomography (CT) scan as part of the initial exam. What is the nurse’s best response? “A CT scan is:
(a) far superior to magnetic resonance imaging for evaluating lymph node metastasis.”
(b) noninvasive and readily available.”
(c) useful for distinguishing small differ ences in tissue density and detecting nodal involvement.”
(d) used to distinguish a malignant from a non-malignant adenopathy.”
Answer:
(c) useful for distinguishing small differ ences in tissue density and detecting nodal involvement.”
Explanation:
CT scanning is the standard noninvasive method used in a workup for lung cancer because it can distinguish small differences in tissue density and can detect nodal involvement. CT is comparable to magnetic resonance imaging in evaluating lymph node metastasis. CT is noninvasive and usually available, but these are not the main reasons for its use. CT can distinguish malignancy in some situations only.
Question 13.
The nurse is conducting a health history for a client at risk for cancer. Which lifestyle factor is considered a risk for colorectal cancer?
(a) a diet low in vitamin C
(b) a high dietary intake of artificial sweeteners
(c) a high-fat, low-fiber diet
(d) multiple sex partner
Answer:
(c) a high-fat, low-fiber diet
Explanation:
A high-fat, low-fiber diet is a risk factor for colorectal cancer. A diet low in vitamin C, use of artificial sweeteners, and multiple sex partners are not considered risk factors for colorectal cancer.
Question 14.
When planning a culturally sensitive health education program, the nurse should:
(a) locate the program at a facility that will not charge for use.
(b) integrate folk beliefs and traditions of the target population into the content.
(c) prepare materials in the primary language of the program sponsor.
(d) exclude community leaders from the dominant culture from initial planning efforts.
Answer:
(b) integrate folk beliefs and traditions of the target population into the content.
Explanation:
Strategies to reach clients in all cultures should include incorporating the folk beliefs and traditions of the target population into the program. Identification of a centrally located building with available access by the target population, use of materials in the native or primary language of the target population, and involvement by all community leaders will also help the program succeed.
Question 15.
A client in a hospice program has increasing pain, and the nurse is collaborating with the client to make a pain management plan. Which plan will be most effective for the client?
(a) administering doses of analgesic when pain is a 5 on a scale of 1 to 10
(b) providing enough analgesia to keep the client semi-somnolent
(c) allowing an analgesia-free period so that the client can carry out daily hygienic activities
(d) administering pain medications over a 24-hour period
Answer:
(d) administering pain medications over a 24-hour period
Explanation:
The desired outcome for management of pain is that the client’s or family’s subjective report of pain is acceptable and documented using a pain scale; the goal is that behavioral and physiologic indicators of pain are absent around the clock. The nurse and client/family should develop a systematic approach to pain management using information gathered from history and a hierarchy of pain measurement.
Pain should be assessed at frequent intervals. The client should not wait to receive medication until the pain is midpoint on the pain scale, nor should the client receive so much pain medication that he or she is not alert. Continuous pain relief is the goal, not just during particular periods during the day.
Question 16.
A client with pancreatic cancer has been receiving morphine via a subcutaneous pump for
2 weeks. The client is requiring an increased dose of the morphine to manage the pain. How should the nurse document this finding?
(a) tolerating the medication well
(b) showing addiction to morphine
(c) developing a tolerance for the medication
(d) experiencing physical dependence
Answer:
(c) developing a tolerance for the medication
Explanation:
Tolerance develops from taking opioids over an extended period. It is characterized by the need for an increased dose to achieve the same degree of analgesia. Addiction is characterized by a drive to take the medication for the psychic effect rather than the therapeutic effect. Physical dependence is a response to ongoing exposure to a medication manifested by withdrawal symptoms when discontinued abruptly.
Question 17.
A client with advanced ovarian cancer takes 150 mg of long-acting morphine orally every 12 hours for abdominal pain. When the client develops a small bowel obstruction, the health care provider (HCP) discontinues the oral morphine and prescribes morphine 6 mg/h IV. After calculating the equianalgesic conversion from oral to intravenous morphine, what should the nurse do?
(a) Continue the oral morphine for one more dose after the IV morphine is started.
(b) Contact the HCP to suggest a higher equianalgesic dose of IV morphine.
(c) Administer the morphine IV as prescribed.
(d) Clarify the prescription to recommend the initial morphine dose of 4 mg/h.
Answer:
(d) Clarify the prescription to recommend the initial morphine dose of 4 mg/h.
Explanation:
The conversion ratio for morphine is 10 mg IV equals 30 mg oral, or 1:3. The client is receiving 300 mg orally per 24 hours, which is equivalent to 100 mg of IV morphine. Morphine 100 mg IV/24 hours = approximately 4 mg/h IV. The effect of the IV morphine is quick, and the oral morphine should be discontinued prior to starting the IV morphine. Administering too much morphine can cause untoward side effects.
Question 18.
A client had a craniotomy for removal of a malignant brain tumor in the occipital region. The nurse should question a prescription for which of these drugs?
(a) ibuprofen
(b) naproxen
(c) morphine sulfate
(d) acetaminophen
Answer:
(c) morphine sulfate
Explanation:
Administration of morphine sulfate is contraindicated because morphine causes respiratory depression. It may also increase intracranial pressure if the client is not ventilating properly, which could result in an accumulation of CO2, a potent vasodilator. Ibuprofen, naproxen, and acetaminophen are not likely to mask symptoms of increased intracranial pressure or impact respiratory status.
Question 19.
A 62-year-old female is taking long-acting morphine 120 mg every 12 hours for pain from metastatic breast cancer. She can have 20 mg of immediate-release morphine every 3 to 4 hours as needed for breakthrough pain. The health care provider (HCP) should be notified if the client uses more than how many breakthrough doses of morphine in 24 hours?
(a) seven
(b) four
(c) two
(d) one
Answer:
(a) seven
Explanation:
If the maximum dose specified by the prescription is required every 3 to 4 hours for breakthrough pain, the HCP should be notified to increase the long-acting medication or rotate to another type of opioid. Around-the-clock dosing is mandatory to achieve a steady state of analgesia. The rescue dose for breakthrough pain is administered over and above the regularly scheduled medication. If three to four analgesic doses are required every 24 hours, the sustained-release around-the-clock dose should be increased to include the amount used for previous breakthrough pain while maintaining a dose for future breakthrough pain.
Question 20.
Assessment of a client taking a nonsteroidal anti-inflammatory drug (NSAID) for pain management should include specific questions regarding which body system?
(a) gastrointestinal
(b) renal
(c) pulmonary
(d) cardiac
Answer:
(a) gastrointestinal
Explanation:
The most common toxicities from NSAIDs are gastrointestinal disorders (nausea, epigastric pain, ulcers, bleeding, diarrhea, and constipation). Renal dysfunction, pulmonary complications, and cardiovascular complications from NSAIDs are much less common.
Question 21.
The nurse is assessing a client with chronic pain. What findings are expected for a client in chronic pain? Select all that apply.
(a) facial grimacing
(b) normal vital signs
(c) physical inactivity
(d) moaning
(e) depression
Answer:
(b) normal vital signs
(c) physical inactivity
Explanation:
(b), (c). In the client with chronic pain, physiologic adaptation results in minimal changes in behavior and vital signs; clients have normal vital signs and are generally physically inactive. Clients with chronic pain are not necessarily depressed. Elevated vital signs, grimacing, and moaning are characteristic responses to acute pain.
Question 22.
A client with lung cancer is being cared for by his wife at home. His pain is increasing in severity. The nurse recognizes that teaching has been effective when the wife uses which pain relief strategies? Select all that apply.
(a) gives her husband a long-acting or sustained- release oral pain medication regularly around the clock
(b) uses an immediate-release medication (oxycodone) for breakthrough pain
(c) avoids long-acting opioids due to her concern about addiction
(d) uses music for distraction as well as heat or cold in combination with medications
(e) substitutes acetaminophen to avoid tolerance to the medications
(f) has her husband use a pain rating scale to measure the effectiveness at reaching his individual pain goal
Answer:
(a) gives her husband a long-acting or sustained- release oral pain medication regularly around the clock
(b) uses an immediate-release medication (oxycodone) for breakthrough pain
(d) uses music for distraction as well as heat or cold in combination with medications
(f) has her husband use a pain rating scale to measure the effectiveness at reaching his individual pain goal
Explanation:
(a), (b), (d), (f). Scheduled use of long-acting opioids and an around-the-clock dosing are necessary to achieve a steady level of analgesia. Whatever the route or frequency, a prescription should be available for “breakthrough” pain medication to be administered in addition to the regularly scheduled medication. Oral drug administration is the route of choice for economy, safety, and ease of use. Even severe pain requiring high doses of opioids can be managed orally as long as the client can swallow medication and has a functioning gastrointestinal system.
Tolerance occurs due to the need for increasing doses to achieve the same pain relief and will not be avoided with the use of acetaminophen. Addiction is a complex condition in which the drug is used for psychological effect and not analgesia. Nurses need to educate families about the appro-priate use of opioids and assure them that addiction is not a concern when managing cancer pain. Nonpharmacologic methods are useful as an adjunct to assist in pain control. Self-report is the best assessment of pain and is an individual response.
Question 23.
A client was discharged from the hospital for cancer-related pain. While in the hospital the pain was well controlled on patient-controlled administration (PCA) of IV morphine, and on discharge 2 days ago was taking oral morphine. The client now reports pain as an 8 on a 10-point scale and is asking the nurse about using PCA for the morphine at home. Which explanation is the most likely for the client’s reports of inadequate pain control?
The client is:
(a) addicted to the IV morphine.
(b) going through withdrawal from the IV opioid.
(c) physically dependent on the IV morphine.
(d) undermedicated on the oral opioid.
Answer:
(d) undermedicated on the oral opioid.
Explanation:
Most clients with cancer who are experiencing inadequate pain control while taking an oral opioid after being switched from IV administration have been undermedicated. Equianalgesic conversions should be made to provide estimates of the equivalent dose needed for the same level of relief as provided by the IV dose. There is research to suggest that cancer clients do not become addicted to opioids when dosed adequately. There is no evidence to suggest that the client is physically addicted or is having withdrawal symptoms.
Question 24.
A nurse is assessing a client with bone cancer pain. Which part of a thorough pain assessment is most significant for this client?
(a) intensity
(b) cause
(c) aggravating factors
(d) location
Answer:
(a) intensity
Explanation:
Intensity is indicative of the severity of pain and is important for evaluating the efficacy of pain management. The cause and location of the pain cannot be managed, but the intensity of the pain can be controlled. The nurse and client can collaborate to reduce aggravating factors; however, the goal will ultimately be to reduce the intensity of the pain.
Question 25.
A client with chronic cancer pain has been receiving opiates for 4 months. She rated the pain as an 8 on a 10-point scale before starting the opioid medication. Following a thorough examination, there is no new evidence of increased disease, yet the pain is close to 8 again. What is the most likely explanation for the increasing pain?
(a) development of an addiction to the opioids
(b) tolerance to the opioid
(c) withdrawal from the opioid
(d) placebo effect has decreased
Answer:
(b) tolerance to the opioid
Explanation:
Tolerance to an opioid occurs when a larger dose of the analgesic is needed to provide the same level of pain control. The risk of addiction is low with opioids to treat cancer pain. There are no data to support that this client is experiencing withdrawal. Although the client may have experienced a placebo effect at one time, placebo effects tend to diminish over time, especially in regard to chronic cancer pain.
Question 26.
The nurse teaches the client with chronic cancer pain about optimal pain control. Which recommendation is most effective for pain control?
(a) Get used to some pain, and use a little less medication than needed to keep from being addicted.
(b) Take prescribed analgesics on an around-the- clock schedule to prevent recurrent pain.
(c) Take analgesics only when pain returns.
(d) Take enough analgesics around the clock so that you can sleep 12 to 16 hours a day to block the pain.
Answer:
(b) Take prescribed analgesics on an around-the- clock schedule to prevent recurrent pain.
Explanation:
The regular administration of analgesics provides a consistent serum level of medication, which can help prevent breakthrough pain. Therefore, taking the prescribed analgesics on a regular schedule is the best way to manage chronic cancer-related pain. There is little risk for the client with cancer-related pain to become addicted. Sleeping 12 to 16 hours a day would not allow the client to participate in usual daily activities or preferred activities.
Question 27.
When preparing to administer a chemotherapeutic agent to a client, what should the nurse do?
(a) Recap all needles used to prepare agents.
(b) Dispose of chemotherapy wastes in the client’s bedside trash.
(c) Use gloves and disposable long-sleeved gowns when handling agents.
(d) Administer only prepackaged agents from the manufacturer.
Answer:
(c) Use gloves and disposable long-sleeved gowns when handling agents.
Explanation:
Chemotherapeutic agents are very toxic; therefore, precautions are taken such as the use of gloves and long-sleeved gowns when handling agents to prevent incidental contact with skin. Recapping needles is against universal precaution standards, and chemotherapy waste is disposed of in biohazard containers according to institution policy. Prepackaged agents can still be hazardous if not handled properly.
Question 28.
A client who is receiving chemotherapy develops stomatitis. What should the nurse instruct the client to do?
(a) Rinse the mouth with full-strength hydrogen peroxide every 4 hours.
(b) Use a soft-bristled toothbrush after each meal.
(c) Drink hot tea with honey to soothe the painful oral mucosa.
(d) Avoid using dental floss until the stomatitis is resolved.
Answer:
(b) Use a soft-bristled toothbrush after each meal.
Explanation:
Stomatitis is an inflammation of the mucous membranes of the mouth resulting from chemotherapy. Using a soft-bristled toothbrush prevents further bleeding and irritation to the already irritated gums and mucous membranes. Hydrogen peroxide can further irritate the mouth. Fluids need to be lukewarm instead of hot; dental floss can be used if it is done gently.
Question 29.
A client is taking doxorubicin and is distressed about hair loss. What should the nurse do?
(a) Have the client wash and massage the scalp daily to stimulate hair growth.
(b) Explain that hair loss is temporary and will quickly grow back to its original appearance.
(c) Provide resources for a wig selection before hair loss begins.
(d) Recommend that the client limit social contacts until hair regrows.
Answer:
(c) Provide resources for a wig selection before hair loss begins.
Explanation:
Resources should be provided for acquiring a wig since it is easier to match hairstyle nd color before hair loss begins. The client has expressed negative feelings of self-image with hair loss. Excessive shampooing and manipulation of hair will increase hair loss. Hair usually grows back in 3 to 4 weeks after the chemotherapy is finished; however, new hair may have a new color or texture. A wig, hairpiece, hat, scarf, or turban can be used to conceal hair loss. Social isolation should be avoided, and the client should be encouraged to socialize with others.
Question 30.
A client is receiving chemotherapy for the diagnosis of brain cancer. When teaching the client about contamination from excretion of the chemotherapy drugs within 48 hours, what should the nurse tell the client?
(a) A bathroom can be shared with an adult who is not pregnant.
(b) Urinary and bowel excretions are not considered contaminated.
(c) Disposable plates and plastic utensils must be used during the entire course of chemotherapy.
(d) Any contaminated linens should be washed separately and then washed a second time, if necessary.
Answer:
(d) Any contaminated linens should be washed separately and then washed a second time, if necessary.
Explanation:
The client may excrete the chemotherapeutic agent for 48 hours or more after administration. Blood, emesis, and excretions may be considered contaminated during this time, and the client should notsshare a bathroom with children or pregnant women. Any contaminated linens or clothing should be washed separately and then washed a second time, if necessary. All contaminated disposable items should be sealed in plastic bags and disposed of as hazardous waste.
Question 31.
A client is receiving vincristine. What should the nurse instruct the client to do when taking this drug?
(a) Use loperamide for diarrhea.
(b) Restrict fluids to 1,500 mL/day.
(c) Follow a low-fiber, bland diet.
(d) Take a stool softener daily.
Answer:
(d) Take a stool softener daily.
Explanation:
A side effect of vincristine is constipation, and a bowel protocol should be considered. Loperamide is used to treat diarrhea. Fluids should be encouraged, along with high-fiber foods to prevent constipation.
Question 32.
The client who is receiving chemotherapy is not eating well but otherwise feels healthy. What should the nurse suggest the client eat?
(a) cereal with milk and strawberries
(b) toast, gelatin dessert, and cookies
(c) broiled chicken, green beans, and cottage cheese
(d) steak and French fries
Answer:
(c) broiled chicken, green beans, and cottage cheese
Explanation:
Carbohydrates are the first substance used by the body for energy. Proteins are needed to maintain muscle mass, repair tissue, and maintain osmotic pressure in the vascular system. Fats, in a small amount, are needed for energy production. Chicken, green beans, and cottage cheese are the best selection to provide a nutritionally well- balanced diet of carbohydrate, protein, and a small amount of fat. Cereal with milk and strawberries as well as toast, gelatin dessert, and cookies have a large amount of carbohydrates and not enough protein. Steak and French fries provide some carbohydrates and a good deal of protein; however, they also provide a large amount of fat.
Question 33.
A nurse is assessing a woman who is receiving the second administration of chemotherapy for breast cancer. When obtaining this client’s health history, the nurse should ask the client which question?
(a) “Has your hair been falling out in clumps?”
(b) “Have you had nausea or vomiting?”
(c) “Have you been sleeping at night?”
(d) “Do you have your usual energy level?”
Answer:
(b) “Have you had nausea or vomiting?”
Explanation:
Chemotherapy agents typically cause nausea and vomiting when not controlled by antiemetic drugs. Antineoplastic drugs attack rapidly growing normal cells, such as in the gastrointestinal tract. These drugs also stimulate the vomiting center in the brain. Hair loss, loss of energy, and sleep are important aspects of the health history, but are not as critical as the potential for dehydration and electrolyte imbalance caused by nausea and vomiting.
Question 34.
A client is receiving monthly doses of chemotherapy for treatment of stage III colon cancer. Which laboratory results should the nurse report to the oncologist before the next dose of chemotherapy is administered? Select all that apply.
(a) hemoglobin of 14.5 g/dL (145 g/L)
(b) platelet count of 40,000/mm3 (40 x 109/L)
(c) blood urea nitrogen (BUN) level of 12 mg/dL (4.3 mmol/L)
(d) white blood cell count of 2,300/mm3 (2.3 x 109/L)
(e) temperature of 101.2°F (38.4°C)
(f) urine specific gravity of 1.020
Answer:
(b) platelet count of 40,000/mm3 (40 x 109/L)
(d) white blood cell count of 2,300/mm3 (2.3 x 109/L)
(e) temperature of 101.2°F (38.4°C)
Explanation:
(a), (b), (d), (e). Chemotherapy causes bone marrow suppression and risk of infection. A platelet count of 40,000/mm3 (40 x 109/L) and a white blood cell count of 2,300/mm3 (2.3 x 109/L) are low. A temper-ature of 101.2°F (38.4°C) is high and could indicate an infection. Further assessment and examination should be performed to rule out infection. The BUN, hemoglobin, and specific gravity values are normal.
Question 35.
A client is struggling with the decision whether or not to continue chemotherapy. The client tells the nurse, “It’s making me so sick and ruining whatever time I have with my family.” What is the nurse’s role when caring for this client?
(a) Share stories about how others made this decision.
(b) Listen to the client’s concerns.
(c) Advocate for the client with the health care provider.
(d) Teach the client how to logically approach the situation.
Answer:
(b) Listen to the client’s concerns.
Explanation:
The nurse’s role while the client is making a decision is to support the client by listening to concerns, asking clarifying questions to help the client think things through, and providing unbiased information. The nurse should not lead the client to what the nurse thinks is best, but allow the client to make his or her own decision. Although the nurse may help the client think through the decision, the nurse would not teach the client how to make a decision because this could bias the client toward the nurse’s opinion (a subtle form of coercion).
There is no need for the nurse to advocate for the client until the client makes a decision.
Question 36.
When the nurse is caring for the client with a saline-only peripherally inserted central catheter (PICC line), what should the nurse do to maintain the catheter?
(a) Flush the port using 3 mL of saline after each use.
(b) Avoid flushing any ports unless they appear blocked.
(c) Utilize a 10-mL saline flush to maintain line patency.
(d) Add 10 units of heparin to each saline flush to prevent clotting.
Answer:
(c) Utilize a 10-mL saline flush to maintain line patency.
Explanation:
The nurse should use a large syringe for flushing this device because a syringe of smaller size requires an increase in force to instill the fluid, and this force leads to increased pressure that can damage the catheter/device and even blood vessels. Most manufacturers recommend a 10-mL syringe for this purpose. The 3-mL syringe will lead to a high pressure and possible damage to the device. The ports must be flushed on a regular basis per institutional policy. While heparin is added in a flush in some devices, the correct dosage is 10 units per mL.
Question 37.
The nurse is instructing a client with cancer who is receiving chemotherapy about reporting signs of infection. Which is the most reliable early indicator of infection in a client who is neutropenic?
(a) fever
(b) chills
(c) tachycardia
(d) dyspnea
Answer:
(a) fever
Explanation:
Fever is an early sign requiring clinical intervention to identify potential causes. Chills and dyspnea may or may not be observed. Tachycardia can be an indicator in a variety of clinical situations when associated with infection; it usually occurs in response to an elevated temperature or change in cardiac function.
Question 38.
A nurse is caring for a client who is undergoing chemotherapy. Current laboratory values are noted on the medical record. Which action would be most appropriate for the nurse to implement?
|
Test |
Result |
|
Hemoglobin |
12.0 g/dL (120 gIL) |
|
Platelet count |
108,000/mm3 (108 x 109/L) |
|
WBC count |
1,600/mm3 (1.6 X 109/L) |
|
ANC |
<1,000/mm3 (1 X 109/L) |
(a) wearing a protective gown and particulate respiratory mask when completing treatments
(b) washing hands before and after entering the room
(c) restricting visitors
(d) contacting the health care provider (HCP) for a prescription for hematopoietic factors such as erythropoietin
Answer:
(b) washing hands before and after entering the room
Explanation:
Chemotherapy causes myelosuppression with a decrease in red blood cells (RBCs), WBCs, and platelets. This client’s data demonstrate neutropenia, placing the client at risk for infection. An ANC of 500 to 1,000/mm3 (0.5 to 1 x 109/L) indicates a moderate risk of infection; <500/mm3 (0.5 x 109/L) indicates severe neutropenia and a high risk of infection. When the WBC count is low and immature WBCs are present, normal phagocytosis is impaired.
Precautions to protect the client from life-threatening infections may be instituted when ANC is <1,000/mm3 (1 x 109/L). Handwashing is the best way to avoid the spread of infection. It is not necessary to wear a gown and mask to take care of this client. It is also not necessary to restrict visitors; however, visitors should be screened to avoid exposing the client to possible infections. Erythropoietin is used for stimulating RBCs, not WBCs. Granulocyte colony-stimulating factors or granulocyte macrophage colony-stimulating factors are useful for treating neutropenia.
Question 39.
A client is receiving chemotherapy and tells the nurse about also taking herbal therapy. What should the nurse do next?
(a) Determine what substances the client is using, and make sure that the health care provider (HCP) is aware of all therapies the client is using.
(b) Guide the client in the decision-making process to select either Western or alternative medicine.
(c) Encourage the client to seek alternative modalities that do not require the ingestion of substances.
(d) Recommend that the client stop using the alternative medicines immediately.
Answer:
(a) Determine what substances the client is using, and make sure that the health care provider (HCP) is aware of all therapies the client is using.
Explanation:
The role of the nurse is to assess what substances or medications the client is using and to document and inform other members of the health care team. It is very important to encourage the client to keep the HCP LD informed of all therapeutic agents, medications, and supplements he or she is using, to avoid adverse interactions. It is not appropriate for the nurse to suggest that the client choose either Western or alternative therapies or to discourage the client’s use of alternative therapies. The nurse should remain objective about the client’s treatment choices and respect the client’s autonomy.
Question 40.
A client diagnosed with cancer is receiving chemotherapy. The nurses should assess which diagnostic value while the client is receiving chemotherapy?
(a) bone marrow cells
(b) liver tissues
(c) heart tissues
(d) pancreatic enzymes
Answer:
(a) bone marrow cells
Explanation:
The fast-growing, normal cells most likely to be affected by certain cancer treatments are blood-forming cells in the bone marrow, as well as cells in the digestive track, reproductive system, and hair follicles. Fortunately, most normal cells recover quickly when treatment is over. Bone marrow sup-pression (a decreased ability of the bone marrow to manufacture blood cells) is a common side effect of chemotherapy. A low white blood cell count (neutropenia) increases the risk of infection during chemotherapy, but other blood cells made in the bone marrow can be affected as well. Most cancer agents do not affect tissues and organs, such as heart, liver, and pancreas.
Question 41.
A client is receiving chemotherapy that has the potential to cause pulmonary toxicity. Which indicates a toxic response to the chemotherapy?
(a) decrease in appetite
(b) drowsiness
(c) spasms of the diaphragm
(d) cough and shortness of breath
Answer:
(d) cough and shortness of breath
Explanation:
Cough and shortness of breath are significant symptoms because they may indicate decreasing pulmonary function secondary to drug toxicity. Decrease in appetite, difficulty in thinking clearly, and spasms of the diaphragm may occur as a result of chemotherapy; however, they are not indicative of pulmonary toxicity.
Question 42.
A client is to start chemotherapy to treat lung cancer. A venous access device has been placed to permit the administration of chemotherapeutic medications. Three days later at the scheduled appointment to receive chemotherapy, the nurse assesses that the client is dyspneic and the skin is warm and pale. The vital signs are blood pressure 80/30 mm Hg, pulse 132 bpm, respirations 28 breaths/min, temperature 103°F (39.4°C), and oxygen saturation 84%. The central line insertion site is inflamed. After the nurse calls the rapid response team, what should the nurse do next?
(a) Place cold, wet compresses on the client’s head.
(b) Obtain a portable ECG monitor.
(c) Administer a prescribed antipyretic.
(d) Insert a peripheral intravenous fluid line and infuse normal saline.
Answer:
(d) Insert a peripheral intravenous fluid line and infuse normal saline.
Explanation:
The client is experiencing severe sepsis, and it is essential to increase circulating fluid volume to restore the blood pressure and cardiac output. The wet compress, administering the antipyretic, and monitoring the client’s cardiac status may be beneficial for this client, but they are not the highest priority action at this time. These three interventions may require the nurse to leave the client, which is not advisable at this time.
Question 43.
A client receiving chemotherapy for cancer has an elevated serum creatinine level. What should the nurse do next?
(a) Cancel the next scheduled chemotherapy.
(b) Administer the scheduled dose of chemotherapy.
(c) Notify the health care provider (HCP).
(d) Obtain a urine specimen.
Answer:
(c) Notify the health care provider (HCP).
Explanation:
Nephrotoxicity caused by chemotherapy is assessed by monitoring serum creatinine. Creatinine is the most sensitive indicator of proper kidney function. In this case, the client is experiencing decreased kidney function, most likely due to the chemotherapy. The nurse consults the HCP for guidance. Administering the next dose of chemotherapy could potentially cause further kidney damage. It is inappropriate to cancel the chemotherapy without checking with the HCP or to tell the client that the cancer is spreading. A urine specimen will not provide other helpful information.
Question 44.
The nurse is instructing a client about skin care while receiving radiation therapy to the chest. What should the nurse instruct the client to do?
(a) Apply lotion if the skin becomes dry.
(b) Shave the chest to prevent contamination from chest hair.
(c) Wash the area with tepid water and mild soap.
(d) Keep the area covered with a nonadherent dressing between treatments.
Answer:
(c) Wash the area with tepid water and mild soap.
Explanation:
Clients receiving radiation experience dryness or redness in the area of the radiation. The nurse instructs the client to wash the area with soap and water and keep the area dry. The client does not apply lotion, shave, or cover the area.
Question 45.
A client with cancer is receiving radiation therapy and develops thrombocytopenia. What is the priority nursing goal to prevent which effect of thrombocytopenia for this client?
(a) pain related to spontaneous bleeding episodes
(b) altered nutrition related to anemia
(c) injury related to the decreased platelet count
(d) skin breakdown related to decreased tissue perfusion
Answer:
(c) injury related to the decreased platelet count
Explanation:
This client is at high risk for bleeding because of the decreased platelet count. The priority nursing goal is to prevent injury to this client by preventing bleeding occurrences. Spontaneous bleeding may cause pain but is not the priority. The client has a low platelet count, but not a low hemoglobin count such as exists in anemia. Skin integrity is a risk but not a priority.
Question 46.
A client is beginning external beam radiation therapy to the right axilla after a lumpectomy for breast cancer. Which information should the nurse include in client teaching?
(a) Use a heating pad under the right arm.
(b) Immobilize the right arm.
(c) Place ice on the area after each treatment.
(d) Apply deodorant only under the left arm.
Answer:
(d) Apply deodorant only under the left arm.
Explanation:
The nurse should instruct the client to avoid applying chemicals (such as a deodorant) or heat or cold (such as with a heating pad or ice pack) to the area being treated. The client should be encouraged to use the extremity to prevent muscle atrophy and contractures.
Question 47.
A client receiving radiation therapy for lung cancer is having difficulty sleeping. What should the nurse do first when teaching the client about promoting sleep?
(a) Tell the client to stop watching television before bed.
(b) Ask the client about usual sleep patterns.
(c) Request the health care provider prescribe a sleeping pill.
(d) Suggest the client stop drinking coffee until the therapy is completed.
Answer:
(b) Ask the client about usual sleep patterns.
Explanation:
Since sleeplessness is often an adverse effect of radiation therapy, the nurse should first assess the client’s usual sleep patterns, hours of sleep required before treatment, and usual bedtime routine. Refraining from watching television before bedtime and avoiding caffeine intake may be helpful depending first on the client’s needs. Sleeplessness is not always an effect of radiation therapy, and the nurse should develop the care plan must to the client’s needs.
Question 48.
A 56-year-old female client is currently receiving radiation therapy to the chest wall for recurrent breast cancer. She has pain while swallowing and burning and tightness in her chest. The nurse should further assess the client for indications of which health problem?
(a) hiatal hernia
(b) stomatitis
(c) radiation enteritis
(d) esophagitis
Answer:
(d) esophagitis
Explanation:
Difficulty in swallowing, pain, and tightness in the chest are signs of esophagitis, which is a common complication of radiation therapy of the chest wall. Hiatal hernia is a herniation of a portion of the stomach into the esophagus. The client could experience burning and tightness
in the chest secondary to a hiatal hernia, but not pain when swallowing.
Also, hiatal hernia is not a complication of radiation therapy. Stomatitis is an inflammation of the oral cavity characterized by pain, burning, and ulcerations. The client with stomatitis may experience pain with swallowing, but not burning and tightness in the chest. Radiation enteritis is a disorder of the large and small bowel that occurs during or after radiation therapy to the abdomen, pelvis, or rectum. Nausea, vomiting, abdominal cramping, the frequent urge to have a bowel movement, and watery diarrhea are the signs and symptoms.
Question 49.
A 36-year-old female is scheduled to receive external radiation therapy and a cesium implant for cancer of the cervix and is asking about the effects of the radiation on sexual relations during and after the radiation therapy. The nurse should inform
the client about which potential effect of radiation therapy on sexuality?
(a) “You will be able to have sexual intercourse while the implant is in place.”
(b) “You will have vaginal dryness after treatment is completed.”
(c) “You will experience vaginal relaxation after treatment is completed.”
(d) “You will continue to have normal menstrual periods during treatment.”
Answer:
(b) “You will have vaginal dryness after treatment is completed.”
Explanation:
Radiation fields that include the ovaries usually result in premature menopause. Vaginal dryness will occur without estrogen replacement. There should be no sexual intercourse while the implant is in place. Cesium is a radioactive isotope used for therapeutic irradiation of cancerous tissue. There is no documentation to support vaginal relaxation after treatment. Because the client will have premature menopause, she will not have normal menstrual periods.
Question 50.
The nurse caring for a client who is receiving external beam radiation therapy for treatment of lung cancer. What should the nurse assess the client for while receiving radiation therapy?
(a) diarrhea
(b) improved energy level
(c) dysphagia
(d) normal white blood cell count
Answer:
(c) dysphagia
Explanation:
Radiation-induced esophagitis with dysphagia is particularly common in clients who receive radiation to the chest. The anatomic location of the esophagus is posterior to the mediastinum and is within the field of primary treatment. Diarrhea may occur with radiation to the abdomen, Decreased energy levels and decreased white blood cell count are potential complications of radiation therapy.
Question 51.
A client receiving radiation to the head and neck is experiencing stomatitis. What can the nurse recommend to relieve this symptom?
(a) evaluation by a dentist
(b) alcohol-based mouthwash rinses
(c) artificial saliva
(d) vigorous brushing of teeth after each meal
Answer:
(c) artificial saliva
Explanation:
Head and neck radiation can cause the complication of stomatitis and decreased salivary flow. A saliva substitute will assist with dryness, moistening food, and swallowing. Meticulous mouth care is needed; however, alcohol and vigorous brushing will increase irritation. Evaluation by a dentist to perform necessary dental work is done prior to initiation of therapy.
Question 52.
A client undergoing chemotherapy has a white blood cell count of 2,300/mm3 (2.3 x 109/L), hemoglobin of 9.8 g/dL (98 g/L), platelet count of 80,000/mm3 (80 x 1CF/L), and potassium of 3.8. Which finding should take priority?
(a) blood pressure 136/88 mm Hg
(b) emesis of 90 mL
(c) temperature 101°F (38.3°C)
(b) urine output 40 mL/h
Answer:
(c) temperature 101°F (38.3°C)
Explanation:
The client has a low white blood cell count from the chemotherapy and has a temperature. Signs and symptoms of infection may be diminished in a client receiving chemotherapy; therefore, the temperature elevation is significant. Early detection of the source of infection facilitates early intervention. Surveillance for bleeding is important with low hemoglobin and platelet count; however, high blood pressure does not indicate bleeding. Vomiting is a side effect of chemotherapy and should be treated. The urine output and potassium are within normal limits.
Question 53.
A nurse is caring for a client 24 hours after an abdominal-perineal resection for a bowel tumor. The client’s wife asks if she can bring him some of his favorite home-cooked Italian minestrone soup. What should the nurse do first?
(a) Auscultate for bowel sounds.
(b) Ask the client if he feels hunger or gas pains.
(c) Consult the dietician.
(d) Encourage the wife to bring the soup.
Answer:
(a) Auscultate for bowel sounds.
Explanation:
The nurse should perform a thorough assessment of the abdomen and auscultate for bowel sounds in all four quadrants. Clients who have gastrointestinal surgery may have decreased peristalsis for several days after surgery. The nurse should check the abdomen for distention and check with the client and the medical record j regarding the passage of flatus or stool. Consulting a dietician would be inappropriate because the client must be kept on nothing-by-mouth status until bowel sounds are present. The nurse should explain to the wife that it is too soon after surgery for her husband to eat.
Question 54.
Which nursing intervention would be most helpful in improving the respiratory effort of a client with metastatic lung cancer?
(a) teaching the client diaphragmatic breathing techniques
(b) administering cough suppressants as prescribed
(c) teaching and encouraging pursed-lip breathing
(d) placing the client in a low semi-Fowler’s position
Answer:
(c) teaching and encouraging pursed-lip breathing
Explanation:
For clients with obstructive versus restrictive disorders, extending exhalation through pursed- lip breathing will make the respiratory effort more efficient. The usual position of choice for this client is the upright position, leaning slightly forward to allow greater lung expansion. Teaching diaphrag-matic breathing techniques will be more helpful to the client with a restrictive disorder. Administering cough suppressants will not help respiratory effort. A low semi-Fowler’s position does not encourage lung expansion. Lung expansion is enhanced in the upright position.
Question 55.
Which information should be included in the teaching plan for a client with cancer who is experiencing thrombocytopenia? Select all that apply.
(a) Use an electric razor.
(b) Use a soft-bristle toothbrush.
(c) Avoid frequent flossing for oral care.
(d) Include an over-the-counter nonsteroidal antiinflammatory (NSAID) daily for pain control.
(e) Monitor temperature daily.
(f) Report bleeding, such as nosebleed, pete-chiae, or melena, to a health care provider (HCP).
Answer:
(a) Use an electric razor.
(b) Use a soft-bristle toothbrush.
(c) Avoid frequent flossing for oral care.
(f) Report bleeding, such as nosebleed, pete-chiae, or melena, to a health care provider (HCP).
Explanation:
(a), (b), (c), (f). Thrombocytopenia places the client at risk for bleeding. Therefore, electric razors will reduce the potential for skin nicks and bleeding. Oral hygiene should be provided with a soft toothbrush and with minimal friction to gently clean without trauma. Clients should be instructed to read labels on all over-the-counter medications and avoid medications such as aspirin or NSAIDs due to their effect on platelet adhesiveness. Clients should evaluate mucous membranes, skin, stools, or other sources of potential bleeding. Monitoring temperature may be an important part of assessment but is focused on neutropenia instead of the problem of thrombocytopenia.
Question 56.
A client with cancer is afraid of experiencing a febrile reaction associated with blood transfusions. What should the nurse tell the client about febrile transfusion reactions?
“Febrile reactions:
(a) are caused when antibodies on the surface of blood cells in the transfusion are directed against antigens of the recipient.”
(b) can usually be prevented by administering antipyretics and antihistamines before the start of the transfusion.”
(c) are rarely immune-mediated reactions and can be a sign of hemolytic transfusion.”
(d) usually occur within 15 minutes after initiation of the transfusion.”
Answer:
(b) can usually be prevented by administering antipyretics and antihistamines before the start of the transfusion.”
Explanation:
The administration of antipyretics and antihistamines before initiation of the transfusion in the frequently transfused client can decrease the incidence of febrile reactions. Febrile reactions are immune mediated and are caused by antibodies in the recipient that are directed against antigens present on the granulocytes, platelets, and lymphocytes in the transfused component. They are the most common transfusion reactions and may occur with onset, during transfusion, or hours after transfusion is completed.
Question 57.
A client had a right pneumonectomy for lung cancer yesterday and now has dyspnea. What position in bed will be best for this client?
(a) lying on the left side
(b) positioned for postural drainage
(c) head of bed elevated
(d) flat in bed on full bed rest
Answer:
(c) head of bed elevated
Explanation:
The client will be most comfortable and have the best lung expansion with the head of the bed elevated. When in a side lying position, the client should lie on the right side to permit expansion of the unaffected lung. Postural drainage positioning will lower the head of bed and increase dyspnea. Lying flat will increase the dyspnea; the client should be encouraged to be out of bed as tolerated.
Question 58.
A client undergoing chemotherapy tells the nurse, “I don’t want to get out of bed in the morning because I’m so tired.” What information should the nurse include in the care plan?
(a) education on the use of filgrastim
(b) individually tailored exercise program
(c) weight lifting when not experiencing fatigue
(d) bed rest until chemotherapy is completed
Answer:
(b) individually tailored exercise program
Explanation:
An individualized exercise program will increase stamina and endurance. Weight lifting may be too vigorous. Filgrastim is used to increase white blood cells and is not applicable in this situation. Decreased hemoglobin and hematocrit predisposes the client to fatigue due to decreased oxygen availability. Bed rest causes muscle atrophy, adding to fatigue, and can contribute to deep vein thrombosis (DVT).
Question 59.
A nurse is reviewing the medical record of an adult male with cancer. The health care provider (HCP) has prescribed filgrastim 400 meg, subcutaneously once daily. When the nurse reviews the laboratory report, which result indicates the treatment has been effective?
Laboratory Results
Hemoglobin: 16 g/dL (160 g/L)
White blood cell (WBC) count: 3,500/mm3 (3.5 x 109/L) Platelet count: 200,000/mm3 (200 x 109/L)
Red blood cell (RBC) count: 4.3 million/mm3 (4.3 x 1012/L)
(a) Hemoglobin is 16 g/dL (160 g/L).
(b) WBC count is 3,500/mm3 (3.5 x 109/L).
(c) Platelet count is 200,000/mm3 (200 x 109/L).
(d) RBC count is 4.3 million/mm3 (4.3 x 1012/L).
Answer:
(b) WBC count is 3,500/mm3 (3.5 x 109/L).
Explanation:
Chemotherapy may cause suppression of the immune system, resulting in a reduction in the WBC count and placing the client at risk for infection. This client has a normal white blood cell count, indicating that the filgrastim has been effective. Decreased hemoglobin (Hgb) indicates anemia. The Hgb is within normal limits for an adult male. A decreased platelet count would indicate thrombocytopenia, and platelets would be prescribed. The platelet count is within normal limits for an adult male. Epoetin alfa is used to treat low red blood cell counts (anemia) caused by chemotherapy.
Question 60.
The nurse is teaching the client who is receiving chemotherapy and the family how to manage possible nausea and vomiting at home. What information should the nurse include in the teaching plan?
(a) Eating frequent, small meals.
(b) Include soft foods in the diet.
(c) Drink a milkshake made with fruit every day.
(d) Limit the amount of fluid intake.
Answer:
(a) Eating frequent, small meals.
Explanation:
To reduce the adverse effects of chemotherapy such as nausea and vomiting, the nurse can suggest that the client eat small meals more frequently, which will be better tolerated while maintaining adequate nutrition. It is not necessary to eat soft food or milkshakes blended with fruit. Fluid intake should be encouraged to avoid dehydration.
Question 61.
A terminally ill client in hospice care is experiencing nausea and vomiting because of a partial bowel obstruction. To respect the client’s wishes for palliative care, what can the nurse recommend that the client use?
(a) a nasogastric (NG) suction tube
(b) IV antiemetics
(c) osmotic laxatives
(d) a clear liquid diet
Answer:
(d) a clear liquid diet
Explanation:
The use of diet modification is a conservative approach to treat the terminally ill or hospice clients who have nausea and vomiting related to bowel obstruction. Osmotic laxatives would be harder for the client to tolerate. An NG tube is more aggressive and invasive. IV antiemetics are also invasive. The hospice philosophy involves comfort and palliative care for the terminally ill.
Question 62.
A client with brown hair is concerned about losing hair as a result of chemotherapy. What should the nurse tell the client?
(a) “The new growth of hair will be gray.”
(b) “The hair loss is temporary.”
(c) “New hair growth will be the same texture and color as it was before chemotherapy.”
(d) “Avoid use of wigs when possible.”
Answer:
(b) “The hair loss is temporary.”
Explanation:
Alopecia from chemotherapy is temporary. The new hair will not be necessarily gray, but the texture and color of new hair growth may be different. Clients who will be receiving chemotherapy should be encouraged to purchase a wig while they still have hair so that they can match the color and texture of their hair. Loss of hair, or alopecia, is a serious threat to self-esteem and should be addressed quickly before treatment.
Question 63.
An adult with a history of chronic obstructive pulmonary disease (COPD) and metastatic carcinoma of the lung has not responded to radiation therapy and is being admitted to the hospice program. The nurse should conduct a focused assessment for which symptom?
(a) ascites
(b) pleural friction rub
(c) dyspnea
(d) peripheral edema
Answer:
(c) dyspnea
Explanation:
Dyspnea is a distressing symptom in clients with advanced cancer including metastatic carcinoma of the lung, previous radiation therapy, and coexisting COPD. Ascites does occur in clients with metastatic carcinoma; however, in the client with COPD and lung cancer, dyspnea is a more common finding. A pleural friction rub is usually associated with pneumonia, pleurisy, or pulmonary infarct.
Question 64.
The nurse is planning with a client who has cancer to improve the client’s independence in activities of daily living after radiation therapy. What should the nurse do?
(a) Refer the client to a community support group after discharge from the rehabilitation unit.
(b) Make certain that a family member is present for the rehabilitation sessions.
(c) Provide positive reinforcement for skills achieved.
(d) Inform the client of rehabilitation plans made by the rehabilitation team.
Answer:
(c) Provide positive reinforcement for skills achieved.
Explanation:
The positive reinforcement builds confidence and facilitates achievement of rehabilitation goals. Community support may or may not be applicable after discharge. Although family support is an important component of rehabilitation, reinforcing the skills the client has acquired is of greater importance when regaining independence. Rehabilitation plans should include the client, family, or both.
Question 65.
When teaching about prevention of infection to a client with a long-term venous catheter, the nurse determines that the client has understood discharge instructions when the client makes which statement?
(a) “I won’t remove the dressing until I return to the clinic next week.”
(b) “My husband will change the dressing three times a week, using sterile technique.”
(c) “I will monitor my temperature every other day.”
(d) “I know it’s very important to wash my hands after irrigating the catheter. ”
Answer:
(b) “My husband will change the dressing three times a week, using sterile technique.”
Explanation:
The most important intervention for infection control is to continue meticulous catheter site care. Dressings are to be changed two to three times per week depending on institutional policies. Temperature should be monitored at least once a day in someone with a vascular access device. Handwashing before and after irrigation or any manipulation of the site is a must for infection prevention.
Question 66.
When caring for a client with a central venous line, which nursing actions should be implemented in the plan of care for chemotherapy administration? Select all that apply,
(a) Verify patency of the line by the presence of a blood return at regular intervals.
(b) Inspect the insertion site for swelling, erythema, or drainage.
(c) Administer a cytotoxic agent to keep the regimen on schedule even if blood return is not present.
(d) If unable to aspirate blood, reposition the client and encourage the client to cough.
(e) Contact the health care provider about verifying placement if the status is questionable.
Answer:
(a) Verify patency of the line by the presence of a blood return at regular intervals.
(b) Inspect the insertion site for swelling, erythema, or drainage.
(d) If unable to aspirate blood, reposition the client and encourage the client to cough.
(e) Contact the health care provider about verifying placement if the status is questionable.
Explanation:
(a), (b), (d), (e). A major concern with IV administration of cytotoxic agents is vessel irritation or extravasation. The Oncology Nursing Society and hospital guidelines require frequent reevaluation of blood return when administering vesicant or nonvesicant chemotherapy due to the risk of extravasation. These guidelines apply to peripheral and central venous lines. The nurse should also assess the insertion site for signs of infiltration, such as swelling and redness.
In addition, central venous lines may be long-term venous access devices. Thus, difficulty drawing or aspirating blood may indicate the line is against the vessel wall or may indicate the line has occlusion. Having the client cough or move position may change the status of the line if it is temporarily against a vessel wall. Occlusion warrants more thorough evaluation via X-ray study to verily placement if the status is questionable and may require a declotting regimen. The nurse should not administer any drug if the IV line is not open or does not have an adequate blood return.
Question 67.
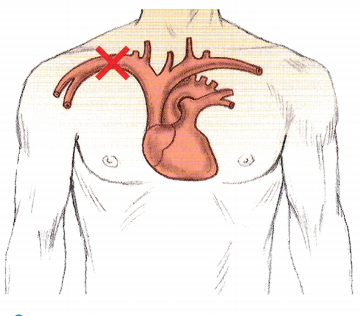
Indicate on the illustration the area that correctly identifies the position of the distal tip of a central line that is inserted into the subclavian vein.
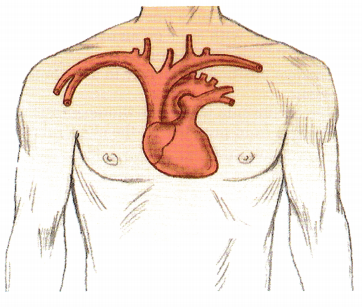
Answer:
The distal tip of a central line should be placed in the subclavian vein.
Question 68.
A client with pancreatic cancer, who has been bed-bound for 3 weeks, has just returned from having a left subclavian, long-term, tunneled catheter inserted for administration of analgesics. The nurse has not yet received radiographic results for confirmation of placement. The client becomes restless and dyspneic and has chest pain radiating to the middle of the back. Physical assessment reveals tachycardia and absent breath sounds in the left lung. What should the nurse further assess?
(a) an air embolus
(b) a pneumothorax
(c) a pulmonary embolus
(d) a myocardial infarction
Answer:
(b) a pneumothorax
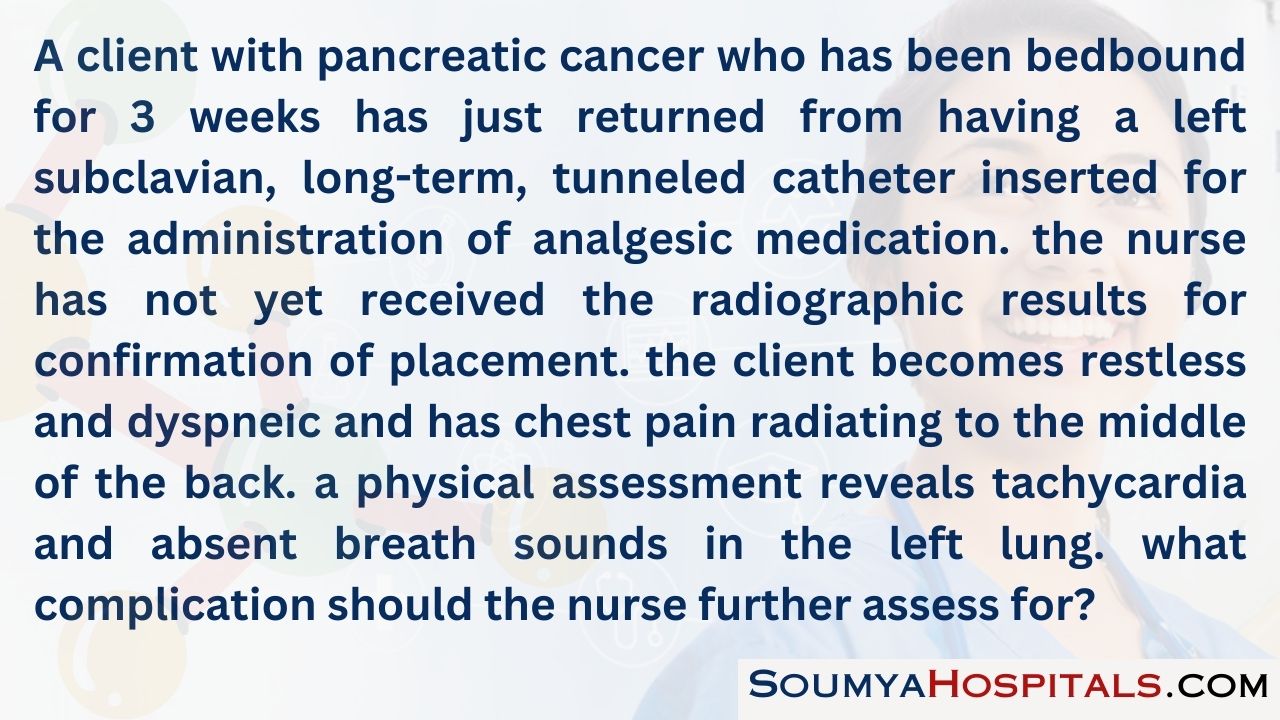
Explanation:
The client is exhibiting signs and symptoms of pneumothorax from the insertion of the subclavian venous catheter. Although it is possible that the client suffered an air embolus during the procedure, and the client is at risk for pulmonary emboli because of his immobility, absent breath sounds immediately after insertion of a subclavian line is strongly suggestive of a pneumothorax. Unilateral absent breath sounds are not associated with a myocardial infarction.
Question 69.
In setting goals for a client with advanced liver cancer who has poor nutrition, what is a desired outcome for the client?
The client will:
(a) have normalized albumin levels.
(b) return to ideal body weight.
(c) gain 1 lb (0.5 kg) every 2 weeks.
(d) maintain current weight.
Answer:
(d) maintain current weight.
Explanation:
An appropriate and realistic outcome would be for the client to maintain current weight or not lose weight. It is unrealistic to expect that the client with advanced liver cancer will have normal albumin levels or will be able to gain weight.
Question 70.
The nurse administers a bolus tube feeding to a client with cancer. To decrease the risk of aspiration, what should the nurse do?
(a) Place the client on bed rest with the head of the bed elevated to 60 degrees for 2 hours.
(b) Turn the client on the left side with the head of the bed at 45 degrees for 15 minutes.
(c) Assist the client out of bed to sit upright in a chair for 1 hour.
(d) Ask the client to rest in bed with the head of the bed elevated to 30 degrees for 20 minutes.
Answer:
(c) Assist the client out of bed to sit upright in a chair for 1 hour.
Explanation:
As long as the client is able to get out of bed, the preferred position and time frame for preventing aspiration after a bolus tube feeding is sitting upright out of bed in a chair for 30 to 60 minutes. The client should have the head of the bed elevated more than 60 degrees; it is not necessary to remain in an upright position for more than an hour after the feeding. Placing the client on the right, not the left, side may facilitate gastric emptying, but this is not the preferred position. Elevating the bed 30 degrees decreases the risk of aspiration, but this elevation must be maintained for at least 45 to 60 minutes.
Question 71.
A client with colon cancer had a left hemicolectomy 3 weeks ago. The client is still having difficulty maintaining an adequate oral intake to meet metabolic needs for optimal healing. The nurse should recommend to the health care provider which nutritional support to maintain the nutritional needs of the client?
(a) total parenteral nutrition through a central catheter
(b) IV infusion of dextrose
(c) nasogastric feeding tube with protein supplement
(d) jejunostomy for high-caloric feedings
Answer:
(a) total parenteral nutrition through a central catheter
Explanation:
Total parenteral nutrition solutions supply the body with sufficient amounts of dextrose, amino acids, fats, vitamins, and minerals to meet metabolic needs. Clients who are unable to tolerate adequate quantities of foods and fluids and those who have had extensive bowel surgery may not be candidates for enteral feedings. The nurse would anticipate total parenteral nutrition via central catheter to promote wound healing. IV dextrose does not supply all the nutrients required to promote wound healing.
Question 72.
A client with colon cancer undergoes surgical removal of a segment of colon and creation of a sigmoid colostomy. What assessments by the nurse indicate the client is developing complications within the first 24 horns? Select all that apply.
(a) coarse breath sounds auscultated bilaterally at the bases
(b) dusky appearance of the stoma
(c) no drainage in the ostomy appliance
(d) temperature >101.2°F (38.4°C)
(e) decreased bowel sounds
Answer:
(a) coarse breath sounds auscultated bilaterally at the bases
(b) dusky appearance of the stoma
(d) temperature >101.2°F (38.4°C)
Explanation:
(a), (b), (d). Elevated temperature in the first 24 hours along with coarse breath sounds may indicate a respiratory complication or the result of general anesthesia. Use of incentive spirometry and increasing activity would be key interventions. A healthy stoma will be beefy red. A dusky appearance of the stoma indicates decreased blood supply and is of concern. It is not uncommon to have decreased bowel sounds initially after gastrointestinal surgery. In addition, it usually will take time for the ostomy to function.
Question 73.
A client receiving chemotherapy for metastatic colon cancer is admitted to the hospital because of prolonged vomiting. Assessment findings include irregular pulse of 120 bpm, blood pressure of 88/48 mm Hg, respiratory rate of 14 breaths/min, serum potassium of 2.9 mEq/L (2.9 mmol/L), and arterial blood gas- pH 7.46, PCO2 45 mm Hg (6.0 kPa), PO2 95 mm Hg (12.6 kPa), and bicarbonate level 29 mEq/L (29 mmol/L). The nurse should implement which prescription first?
(a) oxygen at 4 L per nasal cannula
(b) repeat lab work in 4 hours
(c) 5% dextrose in 0.45% normal saline with KC1 40 mEq/L at 125 mL/h
(d) 12-lead ECG
Answer:
(c) 5% dextrose in 0.45% normal saline with KC1 40 mEq/L at 125 mL/h
Explanation:
The vital signs suggest that the client is dehydrated from the vomiting, and the nurse should first infuse the IV fluids with the addition of potassium. There is no indication that the client needs oxygen at this time since the PO2 is 95 mm Hg (12.6 kPa). Although the client has a rapid and irregular pulse, the infusion of fluids may cause the heart rate to return to normal, and the 12-lead ECG can be prescribed after starting the intravenous fluids.
Question 74.
One week after a left mastectomy, the client reports her appetite is still not good, she is not getting much sleep, and her husband is avoiding her. She is eager to get back to work. What should the nurse do first?
(a) Call the health care provider to discuss allowing the client to return to work earlier.
(b) Suggest that the client learn relaxation techniques for help with insomnia.
(c) Perform a nutritional assessment to assess for anorexia.
(d) Ask open-ended questions about sexuality issues related to her mastectomy.
Answer:
(d) Ask open-ended questions about sexuality issues related to her mastectomy.
Explanation:
The content of the client’s comments suggests that she is concerned about her husband avoiding her. Addressing sexuality issues is appropriate for a client who has undergone a mastectomy. Rushing her return to work may add to her exhaustion. Suggesting that she learn relaxation techniques for help with her insomnia is appropriate; however, the nurse must first address the psychosocial and sexual issues. A nutritional assessment may be useful, but there is no indication that she has anorexia.
Question 75.
The nurse is making a follow-up telephone call to a 52-year-old client with lung cancer. The client now has a low-grade fever (100.6°F [38.1°C]), nonproductive cough, and increasing fatigue. The client completed the radiation therapy to the mass in the right lung and mediastinum 10 weeks ago and has a follow-up appointment to see the health care provider in 2 weeks. What should the nurse advise the client to do?
(a) Take two acetaminophen tablets every 4 to 6 hours for 2 days and call the health care provider (HCP) if the temperature increases to 101°F (38.3°C] or greater.
(b) This is an expected side effect of the radiation therapy and to keep the follow-up appointment in 2 weeks.
(c) Contact the health care provider (HCP) for an appointment today.
(d) Go to the nearest emergency department.
Answer:
(c) Contact the health care provider (HCP) for an appointment today.
Explanation:
The client is exhibiting early symptoms of pulmonary toxicity as a result of the radiation therapy. These are not expected adverse effects of radiation. The client should be examined to differentiate between an infection and radiation pneumonitis. Suggesting that the client take acetaminophen and call back in 2 days is inappropriate. These signs and symptoms are not indicative of a true emergency, but the client should be seen by an HCP before the next appointment.
Question 76.
A client with malignant pleural effusions has dyspnea and chest pain. In which order of priority from first to last should the nurse manage the client’s care? All options must be used.
(a) Administer morphine sulfate 2 mg IV.
(b) Apply oxygen at 2 L via nasal cannula.
(c) Educate the client in anticipation of a thoracentesis.
(d) Coach the client on deep-breathing exercise.
Answer:
(b) Apply oxygen at 2 L via nasal cannula.
(a) Administer morphine sulfate 2 mg IV.
(d) Coach the client on deep-breathing exercise.
(c) Educate the client in anticipation of a thoracentesis.
Explanation:
(b), (a), (d), (c). The client is short of breath. The head of the bed should be elevated to enable breathing, and oxygen should be applied. Morphine should be administered for pain prior to initiating deep-breathing exercises. Deep-breathing exercises improve lung expansion and decrease dyspnea. Education can be provided on the thoracentesis that is anticipated once the symptoms are managed.
Question 77.
What instructions should the nurse provide to a client who develops cellulitis in the right arm after a right modified radical mastectomy?
(a) Antibiotics will need to be taken for 1 to 2 weeks.
(b) Arm exercises will get rid of the cellulitis.
(c) Ice packs should be applied to the affected area for 20-minute periods to reduce swelling.
(d) The right extremity should be lowered to improve blood flow to the forearm.
Answer:
(a) Antibiotics will need to be taken for 1 to 2 weeks.
Explanation:
Treatment for cellulitis includes oral or intravenous antibiotics for 1 to 2 weeks, elevation of the affected extremity, and application of warm, moist packs to the site. Arm exercises help to reduce swelling, but do not treat the infection.
Question 78.
An adult has just had a sclerosing agent instilled after chest tube drainage of a pleural effusion. What should the nurse instruct the client to do?
(a) Lie still to prevent a pneumothorax.
(b) Sit upright with arms on an overhead table to promote lung expansion.
(c) Change position frequently to distribute the agent.
(d) Lie on the side where the thoracentesis was done to hold pressure on the chest tube site.
Answer:
(c) Change position frequently to distribute the agent.
Explanation:
Changing positions frequently aids in distributing the agent to the pleura for sealing. The majority of the pleural fluid is drained, and the lung should already be reexpanded before instillation of the sclerosing agent. A pressure dressing is applied to the chest tube exit site, and it is not necessary to lie on that side to hold pressure on the area.
Question 79.
After surgery for head and neck cancer, a client has a permanent tracheostomy. Which is the most important point for the nurse to include in the teaching plan for the client and family?
(a) providing tracheostomy site care
(b) addressing the psychosocial issues related to tracheostomy
(c) observing for early signs and symptoms of skin breakdown around the tracheostomy site
(d) using humidifiers to prevent thick, tenacious secretions
Answer:
(d) using humidifiers to prevent thick, tenacious secretions
Explanation:
Providing adequate humidification for the client with a tracheostomy is essential. The client no longer has the functions of the nose for warming, moistening, or filtering the air when breathing through the tracheostomy site. Providing tracheostomy site care, addressing the psychosocial issues, and observing for early signs and symptoms of skin breakdown around the tracheostomy site are also important; however, using humidifiers to prevent thick, tenacious secretions is the most important recommendation for long-term management and the prevention of pulmonary infection.
Question 80.
A client has a malignant pleural effusion. The nurse should conduct a focused assessment to determine if the client has which signs and symptoms? Select all that apply.
(a) hiccups
(b) weight gain
(c) peripheral edema
(d) chest pain
(e) dyspnea
Answer:
(d) chest pain
(e) dyspnea
Explanation:
(d), (e). A malignant pleural effusion is an accumulation of excessive fluid within the pleural space that occurs when cancer cells irritate the pleural membrane. Dyspnea can result from the increased pressure, which may contribute to increased anxiety and fear of suffocation. Pain is caused by pleural irritation. Hiccups are usually associated with pericardial effusions. Weight gain and peripheral edema may occur with peritoneal effusion.
Question 81.
A client with suspected lung cancer is undergoing a thoracentesis. Which outcomes of the procedure are expected? Select all that apply.
(a) treatment of recurrent malignant effusion
(b) diagnosis of underlying disease
(c) palliation of symptoms
(d) relief of acute respiratory distress
(e) removal of the cancer cells
Answer:
(b) diagnosis of underlying disease
(c) palliation of symptoms
(d) relief of acute respiratory distress
Explanation:
(b), (c), (d). Thoracentesis is usually successful for diagnosis of underlying disease, palliation of symptoms, and treating acute respiratory distress; alleviation of the symptoms and distress is usually short-term. The thoracentesis is not used as a treatment for recurrent pleural effusion because the fluid accumulates rapidly. Thoracentesis does not remove cancer cells.
Question 82.
The nurse is assessing a client with anemia. In order to plan nursing care, the nurse should focus the assessment on which signs and symptoms?
(a) decreased salivation
(b) bradycardia
(c) cold intolerance
(d) nausea
Answer:
(c) cold intolerance
Explanation:
Cold intolerance may be associated with anemia because of the diminished oxygen supply to the peripheral circulation. Decreased salivation is not associated with anemia. Tachycardia may be expected in severe anemia. Clients with anemia are usually not nauseated.
Question 83.
A nurse is assessing an adult who has been receiving chemotherapy. The client has a platelet count of 22,000 cells/mm3 (22 x 109/L) and has petechiae on the lower extremities. What should the nurse instruct the client to do?
(a) Increase the amount of iron in the client’s diet.
(b) Apply lotion to the lower extremities.
(c) Elevate the legs.
(d) Consult the health care provider.
Answer:
(d) Consult the health care provider.
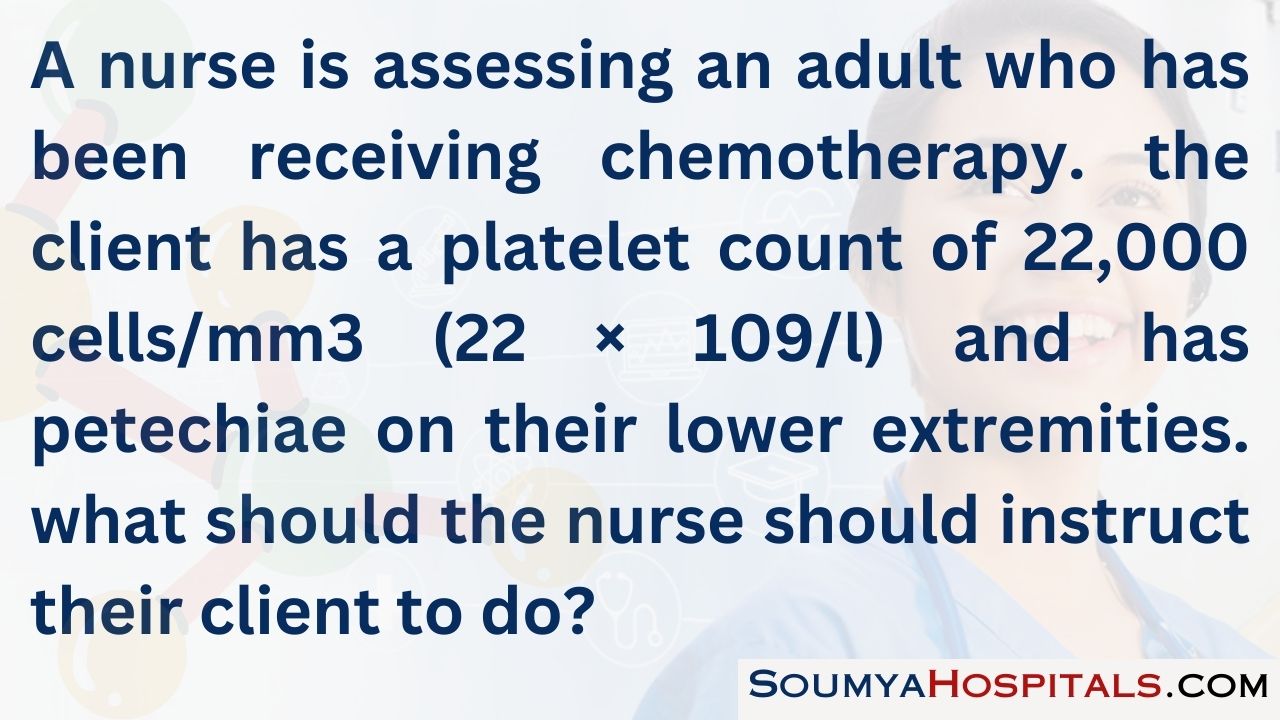
Explanation:
Petechiae are tiny, purplish, hemorrhagic spots visible under the skin. Petechiae usually appear when platelets are depleted. Bleeding gums or oozing of blood may accompany the petechiae, and the client should seek medical assistance immediately. Increasing iron in the diet will not improve the platelet count. The lotion will not treat the petechiae. Elevating the legs will not cause the petechiae to disappear.
Question 84.
A nurse is teaching an older adult who has had a left modified radical mastectomy with axillary node dissection about lymphedema. What should the nurse tell the client about when lymphedema occurs?
(a) if all cancer cells are not removed
(b) in older women
(c) at any time after surgery
(d) only with radical mastectomy
Answer:
(c) at any time after surgery
Explanation:
Lymphedema after breast cancer surgery is the accumulation of lymph tissue in the tissues of the upper extremity extending down from the upper arm. It may occur at any time after surgery in women of any age. It is caused by the interruption or removal of lymph channels and nodes after axillary node dissection. Removal results in less efficient filtration of lymph fluid and a pooling of lymph fluid in the tissues on the affected side. Treatments or interventions should be instituted as soon as lymphedema is noted to prevent or reduce further progression.
Range-of-motion exercises, elevation, and avoidance of injury in the affected arm are important when completing client teaching. The health care provider (HCP) may also prescribe a compression sleeve. Lymphoma is not caused by failure to remove all cancer cells. Lymphedema can occur after any surgery that disrupts lymph flow, not just radical mastectomy.
Question 85.
A middle-aged female with a history of breast-conserving surgery, axillary node dissection, and radiation therapy reports that her arm is red, warm to touch, and slightly swollen. Which action should the nurse suggest?
(a) Apply warm compresses to the affected arm.
(b) Elevate the arm on two pillows.
(c) See the health care provider immediately.
(d) Apply a compression sleeve.
Answer:
(c) See the health care provider immediately.
Explanation:
Redness, warmth, and swelling are all signs of infection. Treatment with antibiotics is usually indicated. Infection usually increases fluid accumulation and could worsen the lymphedema. Warm compresses could also increase fluid accumulation. Elevating the arm will not treat the infection, nor does wearing a compression sleeve. It is critical that the client not delay treatment.
Question 86.
The nurse is assessing a middle-aged client with cancer who has lost 1 lb (0.5 kg) in 4 weeks. The client is taking ondansetron for nausea and now has a temperature of 101°F (38.3°C). The nurse judges that the fever is a sign of what?
(a) inadequate nutrition
(b) new resistance to current antiemetic therapy
(c) expected response to chemotherapy treatment
(d) infection
Answer:
(d) infection
Explanation:
Fever is most commonly related to infection. In a neutropenic client, fever frequently occurs in the absence of the usual clinical signs and symptoms of infection. Inadequate nutrition or antiemetic therapy resistance would not result in fever. Fever
Question 87.
A nurse is assessing a client with lymphoma who reports distress 9 days after chemotherapy. Because of the risk for septic shock, the nurse should assess the client for which cluster of symptoms?
(a) flushing, decreased oxygen saturation, mild hypotension
(b) low-grade fever, chills, tachycardia
(c) elevated temperature, oliguria, hypotension
(d) high-grade fever, normal blood pressure, increased respirations
Answer:
(b) low-grade fever, chills, tachycardia
Explanation:
Nine days after chemotherapy, it is expected for the client to be immunocompromised. The clinical signs and symptoms of shock reflect changes in cardiac function, vascular resistance, cellular metabolism, and capillary permeability. Low- grade fever, tachycardia, and chills may be early signs of shock. The client with signs and symptoms of impending septic shock may not have decreased oxygen saturation levels. Oliguria and hypotension are late signs of shock. Urine output can be initially normal or increased.
Question 88.
A client receiving radiation therapy has fatigue. What should the nurse include in the teaching plan?
(a) increase fluid intake
(b) minimize naps or periods of rest during day
(c) conserve energy by prioritizing activities
(d) limit dietary intake of high-fiber foods
Answer:
(c) conserve energy by prioritizing activities
Explanation:
Prioritizing physical activities helps to conserve energy, which promotes adaptation to fatigue. The client should learn to take short naps or short rest periods during the day for additional energy conversation. Increased fluid intake is important but may interrupt rest periods by causing frequent urination. Limiting intake of high-fiber foods can add to constipation, which may be a problem because of inactivity in fatigued clients.
Question 89.
Which is the most appropriate nursing intervention for a hospitalized client with pruritus caused by medications used to treat cancer?
(a) administration of antihistamines
(b) steroids
(c) silk sheets
(d) medicated cool baths
Answer:
(d) medicated cool baths
Explanation:
Nursing interventions to decrease the discomfort of pruritus include those that prevent vasodilation, decrease anxiety, and maintain skin integrity and hydration. Medicated baths with salicylic acid or colloidal oatmeal can be soothing as a temporary relief. The use of antihistamines or topical steroids depends on the cause of the pruritus, and these agents should be used with caution. Using silk sheets is not a practical intervention for the hospitalized client with pruritus.
Question 90.
A client receiving chemotherapy has pruritus. In order to develop a care plan, the nurse should ask if the client about which measure?
(a) wearing clothes made from 100% cotton
(b) sleeping in a cool, humidified room
(c) increasing fluid intake to at least 3,000 mL/day
(d) taking daily baths with a deodorant soap
Answer:
(d) taking daily baths with a deodorant soap
Explanation:
Use of deodorant or fragrant soaps is drying to the skin. Cotton clothing gives the least irritation to skin. A cool, humidified environment adds to the client’s comfort as well as providing hydration for skin comfort. Fluid intake of 3,000 mL/day is recommended for adequate hydration.
Question 91.
Which factor is most important to assess when determining the impact of the cancer diagnosis and treatment modalities on a long-term survivor’s quality of life?
(a) occupation and employability
(b) functional status
(c) evidence of disease
(d) individual values and beliefs
Answer:
(d) individual values and beliefs
Explanation:
Individuals with cancer have various cultural values and beliefs that help them cope with the cancer experience. Quality of life cannot be evaluated solely by quantifiable factors such as employability, functional status, or evidence of disease. It must be evaluated by the survivors within the context of their subjective and individual values and beliefs.
Question 92.
A client with breast cancer has abdominal bloating and cramping with no bowel movement for 5 days. She says she usually has a bowel movement every day after her morning coffee. Bowel sounds are present in all four quadrants. She received 80 mg of doxorubicin hydrochloride 10 days ago. The nurse should contact the health care provider to request which prescription?
(a) a ready-to-use enema to stimulate peristalsis
(b) a soapsuds enema until clear
(c) an oral cathartic until the client has a bowel movement
(d) a mild opioid for abdominal discomfort
Answer:
(c) an oral cathartic until the client has a bowel movement
Explanation:
Constipation lasting 3 days or longer is unusual in this client and warrants immediate action. However, because the client had chemotherapy with doxorubicin 10 days ago, she is susceptible to infection and should avoid rectal medications and treatments. Abdominal discomfort secondary to constipation will be relieved after the client has a bowel movement; an opioid would contribute to the constipation.
Question 93.
A client with cancer has diarrhea and inflamed areas of skin around the rectum. What actions should the nurse take? Select all that apply.
(a) Use sitz baths.
(b) Apply zinc oxide ointment to the rectal area after each bowel movement.
(c) Apply a skin barrier dressing daily to the rectal area.
(d) Clean the rectal area with unscented soap and water after each bowel movement, rinse well, and pat dry.
(e) Increase fluid intake.
Answer:
(a) Use sitz baths.
(d) Clean the rectal area with unscented soap and water after each bowel movement, rinse well, and pat dry.
(e) Increase fluid intake.
Explanation:
(a), (d), (e). The rectal area needs to be cleaned and gently dried after each bowel movement to prevent skin breakdown and inhibit growth of bacteria. Sitz baths are appropriate because they promote comfort. The client should increase fluid consumption to prevent dehydration. Zinc oxide ointment does form a protective skin barrier, but it makes it difficult to thoroughly clean the perirectal area of feces and increases the risk of infection, as do skin barrier dressings.
Question 94.
When explaining the long-term toxic effects of cancer treatments on the immune system, what should the nurse tell the client?
(a) Clients with persistent immunologic abnormalities after treatment are at a much greater risk for infection than clients with a history of splenectomy.
(b) The use of radiation and combination chemotherapy can result in more frequent and more severe immune system impairment.
(c) Long-term immunologic effects have been studied only in clients with breast and lung cancer.
(d) The helper T cells recover more rapidly than do the suppressor T cells, which results in positive helper cell balance that can last 5 years.
Answer:
(b) The use of radiation and combination chemotherapy can result in more frequent and more severe immune system impairment.
Explanation:
Studies of long-term immunologic effects in clients treated for leukemia, Hodgkin’s disease, and breast cancer reveal that combination treatments of chemotherapy and radiation can cause overall bone marrow suppression, decreased leukocyte counts, and profound immunosuppression. Persistent and severe immunologic impairment may follow radiation and chemotherapy (especially multiagent therapy). There is no evidence of greater risk of infection in clients with persistent immunologic abnormalities. Suppressor T cells recover more rapidly than do the helper T cells.
Question 95.
A client is newly diagnosed with cancer and is beginning a treatment plan. Which action by the nurse will be most effective in helping the client cope?
(a) Assume decision-making for the client until treatment is completed.
(b) Encourage the client to observe strict compliance with all treatment regimens.
(c) Inform the client of all possible adverse treatment effects.
(d) Identify available resources for the client and family.
Answer:
(d) Identify available resources for the client and family.
Explanation:
Identifying available resources for the client and family represents a respectful effort to make options available and encourages the client to become involved in treatment decisions. Assuming decision-making for the client may foster dependence. Encouraging strict compliance with all treatment regimens may increase anxiety and limit the client’s options and treatment choices. Informing the client of all possible adverse treatment effects may increase anxiety and fear by focusing on adverse outcomes too soon.
Question 96.
A daughter is concerned that her mother is in denial because when they discuss the diagnosis of breast cancer, the mother says that breast cancer is not that serious and then changes the subject.
The nurse can tell the daughter that denial can be a healthy defense mechanism if it is used when?
(a) to permit her mother to seek unconventional treatments
(b) when making decisions about her care
(c) alone and not in combination with other defense mechanisms
(d) to allow her mother to continue in her role as a mother
Answer:
(d) to allow her mother to continue in her role as a mother
Explanation:
Denial is a defense mechanism used to shut out a situation that is too frightening or threatening to tolerate. In this case, denial allows the client to vacillate between acceptance of the illness and its treatment and denial of the actual or potential seriousness of the disease. This may allow the client more psychological freedom to maintain her current roles in the family and elsewhere. Denial can be harmful if the client ignores standard medical therapies in favor of unconventional treatments.
Denial is not helpful when it interferes with a client’s willingness to seek treatment or make decisions about care. Using any one defense mechanism exclusively usually reflects maladaptive coping. Other defense mechanisms that may be used include regression, humor, and sublimation.
Question 97.
A 45-year-old single mother of three teen- aged boys has metastatic breast cancer. Her parents live 750 miles (1,200 km) away and have only been able to visit twice since her initial diagnosis 14 months ago. The progression of her disease has forced the client to consider high-dose chemotherapy. She is concerned about her children’s welfare during the treatment. When assessing the client’s present support systems, the nurse will be most concerned about which potential problem?
(a) denial as a primary coping mechanism
(b) support systems and coping strategies
(c) decision-making abilities
(d) transportation and money for the boys
Answer:
(b) support systems and coping strategies
Explanation:
The client’s resources for coping with the emotional and practical needs of herself and her family need to be assessed because usual coping strategies and support systems are often inadequate in especially stressful situations. The nurse may be concerned with the client’s use of denial, decisionmaking abilities, and ability to pay for transportation; however, the client’s support systems will be of more importance in this situation.
Question 98.
Which characteristic displayed by the wife of a 36-year-old man with pancreatic cancer suggests that she may be at risk for negative bereavement outcomes?
(a) She is preparing for her husband’s death.
(b) She has a high socioeconomic status.
(c) She has strong family support.
(d) She blames herself for her husband’s cancer.
Answer:
(d) She blames herself for her husband’s cancer.
Explanation:
Variables that are most predictive of negative bereavement outcomes include anger and self-reproach, low socioeconomic status, lack of preparation for death, and lack of family support. Making preparations suggests that she is coping with her husband’s approaching death.
Question 99.
The nurse is counseling the family of an older adult who died today. Which factor facilitates attainment of a positive bereavement outcome?
(a) being a teenager
(b) having a history of anxiety
(c) being a spouse
(d) possessing adequate financial resources
Answer:
(d) possessing adequate financial resources
Explanation:
Having adequate financial resources facilitates bereavement. Younger people are at higher risk for negative bereavement outcomes. Having a history of depressive illness or anxiety is a risk factor for negative bereavement outcomes. Being a spouse does not make grieving easier.
Question 100.
Which nursing intervention will be most effective when caring for a client experiencing powerlessness?
(a) Make certain that all staff members focus only on the client’s capabilities.
(b) Encourage family members to become more responsible for the client’s care.
(c) Request a referral to a psychologist.
(d) Include the client in decision-making whenever possible.
Answer:
(d) Include the client in decision-making whenever possible.
Explanation:
Focusing on the client’s physical capabilities is important, but powerlessness reflects a perceived lack of control over the current situation and the belief that one’s actions will not affect the outcome. Participation in decision-making is key to getting the client involved and feeling more in control of his or her own care. Apathy and dependence on others are characteristics of powerlessness.
Encouraging others to take responsibility for the client’s care will increase the client’s feelings of powerlessness. A referral to a psychologist is not necessarily indicated. The nurse should implement strategies to involve the client in decisions about the client’s care and evaluate the response to this intervention before suggesting a referral.
Question 101.
A client has just been diagnosed with cancer. During the initial stage of adaptation to the diagnosis and its treatment, the nurse can facilitate the client’s adaptation by using which strategy?
(a) encouraging the client to maintain her usual role
(b) facilitating family-related disagreements and conflicts
(c) supporting the client in her use of denial as a coping strategy
(d) arranging transportation and child care on treatment days
Answer:
(a) encouraging the client to maintain her usual role
Explanation:
Maintaining role function has been found to be a supportive source of normalcy and positive selfesteem for the client and family during the cancer experience. Facilitating family-related disagreements and conflicts is not the nurse’s role. Supporting the client in her use of denial as a coping strategy will not help facilitate the client’s adaptation to the diagnosis. Arranging transportation and child care on treatment days may be helpful but does not necessarily facilitate adaptation to the diagnosis.
Question 102.
When explaining hospice care, what should the nurse tell the client?
“Hospice care:
(a) is available one month before treatment is no longer curative.”
(b) offers end-of-life care that includes palliative care and focuses on the client’s physical, emotional, and spiritual needs.”
(c) is coordinated by your health care provider.”
(d) helps clients die at home.”
Answer:
(b) offers end-of-life care that includes palliative care and focuses on the client’s physical, emotional, and spiritual needs.”
Explanation:
Hospice care services provide palliative care and also address the client’s physical, emotional, and spiritual needs. The focus of the care is on the care on the client and family. Hospice care services can begin 6 months before the illness is ter¬minal and can be renewed depending on the course of the disease. Hospice care collaborates with the client’s health care provider (HCP) but the HCP does not direct the care. Not all hospice clients want to die at home, nor is it a requirement to be at home to receive hospice care.

Question 103.
A client’s husband expresses concern that his dying wife keeps saying, “I have to go to the store.” Which statement by the nurse will be most effective in assisting the husband to understand the dying process?
(a) “Many dying clients are restless and can be treated with sedatives.”
(b) “The client may be fighting death, and you should leave her alone.”
(c) “Comments related to going somewhere or leaving on a trip are common in dying clients.”
(d) “You can tell your wife that you will take her to the store.”
Answer:
(c) “Comments related to going somewhere or leaving on a trip are common in dying clients.”
Explanation:
Mental changes and decreased level of consciousness are common in the dying process, and the client may talk about travel, trips, or going somewhere. Suggesting that the client be sedated ignores the husband’s question about what his wife is experiencing. Suggesting that the client is fighting death and that the husband should leave her alone is inappropriate and denies the husband time to spend with his wife. The husband should not make misleading statements to his wife.
Question 104.
The wife of a terminally ill client asks the nurse, “Why is my husband having frequent bowel movements if he is not eating?” What should the nurse tell the wife?
(a) “I know he’s having frequent loose stools and it’s distressing for you, but that’s just the way it is.”
(b) “I don’t know when the bowels will shut down, but they will eventually.”
(c) “The pain medication will eventually help to slow the process of bowel function.”
(d) “The intestines still produce some waste products even when a person is not eating.”
Answer:
(d) “The intestines still produce some waste products even when a person is not eating.”
Explanation:
It is important to give factual information to answer a loved one’s questions and concerns. Stating “That’s just the way it is” is unprofessional and uncaring. Saying “I don’t know when the bowels will shut down, but they will eventually” projects an uncaring attitude and does not address the wife’s concern for her husband or her need for information. Although it may be true that the pain medication will slow bowel function, this does not provide the wife with the information she is seeking.
Question 105.
The client who is in end stages of cancer is requesting spiritual support. What should the nurse do next?
(a) Review the client’s medical record to determine the client’s religion.
(b) Call a chaplain and set up an appointment for spiritual guidance.
(c) Request the family notify the client’s spiritual advisor.
(d) Ask the client what spiritual activities would be most helpful.
Answer:
(d) Ask the client what spiritual activities would be most helpful.
Explanation:
It is important to allow the client to choose his or her own form of spiritual support, and the nurse can begin by asking the client what would be most supportive now. It is not necessary to know the client’s religion before finding out what is important to the client. The client must be consulted before referral to a chaplain is made. It is not appropriate for the nurse to ask the family to contact a spiritual advisor; once the nurse understands the client’s needs the nurse and client can make a plan about how to meet them.
Question 106.
An older adult with end-stage cancer needs assistance with arranging the finances for end-of- life home care. The nurse should refer the client to which person?
(a) the business manager of the health care agency
(b) a social worker
(c) the health care provider (HCP)
(d) the executor of the client’s will
Answer:
(b) a social worker
Explanation:
A social worker can provide information for supportive services and can help the client determine which resources are necessary at this time. The business office of the health care agency does not provide advice about managing finances. The HCP will be part of the team but will focus on managing the client’s health and end-of-life care. The client may or may not have a will; it is not the role of an executor to make financial decisions about health care.
Question 107.
The family members of a client who is near death from colon cancer ask the nurse what to expect if the client becomes dehydrated. What should the nurse tell them?
(a) The health care provider (HCP) will make the decision regarding hydration therapy.
(b) Dehydration may prolong the dying process.
(c) Hydration is used only in extreme situations of dehydration.
(d) Dehydration is expected during the dying process.
Answer:
(d) Dehydration is expected during the dying process.
Explanation:
Dehydration is an expected event within the dying process. Hydration may be used in any situation of dehydration as long as it is within the client and family’s wishes. Rehydrating the client may actually prolong the dying process. Decisions about treatment are made with the family.
Question 108.
A client tells the nurse about experiencing “spiritual distress.” What should the nurse do first?
(a) Make a referral to a member of the clergy.
(b) Refer the client to a support group.
(c) Ask the client if having prayers would be helpful.
(d) Determine what spiritual distress means to the client.
Answer:
(d) Determine what spiritual distress means to the client.
Explanation:
The nurse must first allow the client to clarify the meaning of spiritual distress and explore his or her own beliefs and values before making referrals to clergy or a support group. The nurse should allow the client to indicate if praying would be helpful after helping the client clarify the meaning of spiritual distress.
Question 109.
A nurse is caring for a client who is receiving hospice care at home. The client’s neighbors have been calling the nurse to inquire about the client’s condition. What should the nurse tell the neighbors?
(a) "Please call the oncologist.”
(b) “The client is in a coma now.”
(c) “Please call the client’s sister.”
(d) “The client is not expected to live much longer.”
Answer:
(c) “Please call the client’s sister.”
Explanation:
The family is in the best position to give the information they elect to disclose to friends and community members. The hospice nurse and the oncologist must maintain client confidentiality and follow privacy guidelines for release of confidential information. Therefore, disclosing any information about the client’s condition would be inappropriate.
Question 110.
A 42-year-old client with breast cancer is concerned that her husband is depressed by her diagnosis. Which change in her husband’s behavior may confirm her fears?
(a) increased decisiveness
(b) problem-focused coping style
(c) increase in social interactions
(d) disturbance in his sleep patterns
Answer:
(d) disturbance in his sleep patterns
Explanation:
Depression can be a mixture of affective responses (feelings of worthlessness, hopelessness, sadness), behavioral responses (appetite changes, withdrawal, sleep disturbances, lethargy), and cognitive responses (decreased ability to concentrate, indecisiveness, suicidal ideation). Increased decisiveness, problem-solving ability, and increased social interactions are reflective of adaptive coping.
Question 111.
What is the most cost-effective suggestion for bereavement support for the hospice nurse to give a woman whose husband died 3 months ago and her three young children?
(a) Seek group counseling support for the three children.
(b) Request individual counseling and medication to manage depression.
(c) Remind her gently that bereavement care before death minimizes grieving.
(d) Continue bereavement support offered through hospice.
Answer:
(d) Continue bereavement support offered through hospice.
Explanation:
Bereavement support after death usually continues for about 1 year or as needed at little or no cost to the remaining family. Mutual support groups by nonprofessionals are usually free or inexpensive but are not necessarily appropriate for young children. Professional individual counseling and medication are expensive, and medication may not be appropriate for young children. To remind someone of what she should have done before the death is not helpful at this time.
Question 112.
Which strategy will be most effective in improving transcultural communications with clients with cancer and their families?
(a) Use touch to show concern and caring for the client.
(b) Focus attention on verbal communication skills only.
(c) Establish a rapport and listen to their concerns.
(d) Maintain eye contact at all times.
Answer:
(c) Establish a rapport and listen to their concerns.
Explanation:
It is important to establish rapport with the client and family by listening to verbal and nonverbal concern and showing respect for cultural differences. The use of touch or eye contact is culture-specific and cannot be generalized as an intervention for all individuals with cancer. Miscommunication between individuals of different cultures is often caused by language differences, rules of communication, age, and gender.
Question 113.
Which outcome is expected of a nursing referral to a cancer support group?
The client can:
(a) choose the best treatment options.
(b) find financial help.
(c) obtain home health care.
(d) cope with cancer.
Answer:
(d) cope with cancer.
Explanation:
Support groups are designed to educate clients and their families experiencing cancer about the disease and methods of coping positively with it. These are self-help and support groups monitored by professionals and cancer survivors who have undergone a training course that helps them to facilitate small groups.
Question 114.
A cancer survivor feels guilty when attending a cancer support group meeting. The nurse can help the client manage feelings of guilt by giving the client which information?
(a) These actually are feelings of anger at the terminally ill clients in the group.
(b) It is an unexpected response to volatile emotions.
(c) This is a spiritual response to the client’s own illness.
(d) This is a normal reaction when surviving a life-threatening experience.
Answer:
(d) This is a normal reaction when surviving a life-threatening experience.
Explanation:
Many cancer survivors question why they are doing so well and others are not. Often, they express feeling guilty when they hear that others are not doing well. Suggesting that the client does not know how to describe the client’s own emotions is inappropriate and may discourage the client from expressing feelings. Although the client may be experiencing volatile emotions, this is not the likely source of feelings of guilt. Guilt about doing well after cancer treatment is not a spiritual response to illness.
Question 115.
A 65-year-old client’s only son lives 500 miles (800 km) away. For which reason is the client at higher risk for psychosocial distress?
The client:
(a) has been successful in dealing with stress throughout life.
(b) does not have to deal with other stressors right now.
(c) is able to use denial as a coping mechanism.
(d) perceives having minimal social support.
Answer:
(d) perceives having minimal social support.
Explanation:
The person who has minimal social support, has not been successful in dealing with stressors, and has multiple other stressors is at greater risk for psychosocial distress. Being successful in dealing with stress throughout life would decrease the client’s risk for psychosocial distress. Not having to deal with other stressors would be helpful in managing the current stressful situation. The denial coping mechanism, if used for short periods, can decrease the risk for psychosocial distress.
Question 116.
A client with a diagnosis of cancer is frequently disruptive and challenges the nurse. This behavior may be caused by which factor?
(a) uncertainty and an underlying fear of recurrence
(b) the usual trajectory of a short-term illness
(c) a history of a behavioral illness
(d) the one-time crisis from learning of the diagnosis
Answer:
(a) uncertainty and an underlying fear of recurrence
Explanation:
Clients with cancer report that the lifelong fear of recurrence is one of the most disruptive aspects of the disease. The trajectory of the disease is unpredictable and can be intertwined with many short- and long-term illnesses related to cancer and the treatment modalities. A diagnosis of cancer challenges the individual and the family with a series of crises rather than a time-limited episode. There are no data to indicate that the client has an underlying behavioral disorder.
Question 117.
A 42-year-old husband and father of a 7-year-old girl and a 10-year-old boy is concerned about what he should tell his children regarding his wife’s impending death from aggressive breast cancer. How should the nurse respond to the husband and his family?
(a) Refer the family to pastoral care services.
(b) Encourage the husband to come to terms with his own grief.
(c) Suggest that the health care provider (HCP) tell the children about the seriousness of their mother’s illness.
(d) Begin education about strategies for communication with his children.
Answer:
(d) Begin education about strategies for communication with his children.
Explanation:
Without clear, consistent communication, the parent-child relationship may become strained during the illness and subsequent death of a parent. A great number of parents do not know how to communicate with their children, especially about difficult emotional topics at a time when they are also under great emotional stress. The nurse should begin by providing information and developmentally appropriate books about the grieving process for children.
Referral to pastoral care services may be appropriate; however, the nurse’s direct intervention of beginning education about strategies for communication will be of immediate and long-term benefit. The grieving process cannot be rushed for the husband, nor should an opportunity for the father and children to communicate and grieve together be delayed. Excluding children from participating in the grieving ritual does not shield them from the sorrow and sadness, and having the HCP tell the children does not promote healthy communication between the father and the children.
Question 118.
While talking to her husband, who is caring for their children, a middle-aged woman who has stage 4 breast cancer slams the phone down. She begins to cry and states that she is feeling guilty for being hospitalized. Which nursing action will best support the client emotionally?
(a) Ask the client if she would like to speak with a grief counselor.
(b) Call the health care provider, and request an antidepressant.
(c) Sit with the client, and help her acknowledge and discuss her feelings.
(d) Suggest the client call her husband when she is calmer.
Answer:
(c) Sit with the client, and help her acknowledge and discuss her feelings.
Explanation:
Acknowledgment and discussion of the client’s feelings begin the establishment of a therapeutic relationship between nurse and client. It also acknowledges the seriousness of the current situation and validates the client’s feelings. Grief counseling antidepressant medication may be options if the depression is severe and prolonged. The client is not ready at this point to continue the conversation with her husband.
Question 119.
A middle-aged woman who is receiving radiation therapy tells the nurse that she feels inadequate as a wife and mother because she can no longer carry out her usual duties with the same energy as before. What recommendations should the nurse make to help the client cope with this situation?
Suggest that she:
(a) reassign all household chores to other members of the family.
(b) prioritize her activities and ask for help fromfriends and family.
(c) ignore the household chores during the crisis period.
(d) not worry so much because it is normal to be tired during this phase of the therapy.
Answer:
(b) prioritize her activities and ask for help fromfriends and family.
Explanation:
Individuals who are experiencing fatigue need to prioritize their activities and ask for assistance from others. It is best not to take away all of the client’s activities because her role as wife and mother is obviously important to her and to her sense of self-worth. Suggesting that she ignore the household chores or telling her not to worry because everyone gets tired disregards the client’s feelings and is not appropriate.
Question 120.
An older adult woman who is usually meticulous about her appearance and dress arrives today for her 23rd day of radiation therapy. She appears disheveled and emotionally labile, and her responses to the usual questions are a little inappropriate. Her heart rate is 124 bpm, her respirations are 32 breaths/min, and her skin is cold and clammy. Based on these findings, the nurse should further assess the client for which condition?
(a) schizophrenia
(b) panic disorder
(c) depression
(d) delirium
Answer:
(d) delirium
Explanation:
Tachycardia, tachypnea, moist or clammy skin, and disorientation are classic symptoms of delirium. Clients with panic disorder do not exhibit disorientation. Clients with depression exhibit a flat affect, apathy, and sleep disturbances. Clients with schizophrenia have thought disorders such as hal-lucinations or delusions.
Question 121.
The nurse is planning future care with a middle-aged woman who has undergone surgical resection for lung cancer. Which plan will best promote adaptation and rehabilitation?
(a) arranging a visit from a client who has recovered from a similar surgery
(b) planning a progressive activity regimen
(c) teaching about dressing care
(d) requesting house cleaning services for 3 months
Answer:
(b) planning a progressive activity regimen
Explanation:
A progressive activity regimen may be prescribed to increase pulmonary function after surgical lung resection. Rehabilitation should include walking and some stair climbing as tolerated. It is not necessary at this point for the client to speak with someone who has had similar surgery. Depending on the surgeon’s preference, there may not be a dressing to change. There is no indication that the client would not be able to manage cleaning the house as her energy increases.
Question 122.
Which activity indicates that the client with cancer is adapting well to body image changes?
(a) The client names his brother as the person to call if he is experiencing suicidal ideation.
(b) The client continuously looks at the incision.
(c) The client discusses a date to return to work.
(d) The client serves as a volunteer in a client-to-client visitation program.
Answer:
(d) The client serves as a volunteer in a client-to-client visitation program.
Explanation:
Serving as a volunteer in a client-to-client program represents reintegration with constructive channeling of energies, which indicates a higher level of adaptation than attention to safety, knowledge, or planned activity. Discussing suicide is an indication the client is not adapting to the changes in health status. Continuing to look at the incision indicates the client is still concerned about the changes to the body. While looking forward to returning to work is a positive sign, being able to help others demonstrates an integration of the experience into the client’s life.
Question 123.
A 36-year-old female has increased vaginal dryness during sexual intercourse. She has received chemotherapy in the past and has menopausal symptoms due to ovarian suppression. The nurse should instruct the client on the use of which solution for vaginal dryness?
(a) vaginal dilators
(b) douching with a soothing solution
(c) water-soluble vaginal lubricants
(d) relaxation techniques
Answer:
(c) water-soluble vaginal lubricants
Explanation:
Water-soluble lubricants used during sexual intercourse can augment reduced natural vaginal lubrication caused by ovarian dysfunction and decreased circulating estrogen related to che-motherapy. The use of vaginal dilators, relaxation techniques, or nightly douches would not increase vaginal lubrication. Frequent douching can disrupt the normal vaginal environment.
Question 124.
A 49-year-old male with a tracheostomy tube confides to the nurse that he is beginning to avoid sexual activity because of the increased tracheostomy secretions. Which statement by the nurse will be most helpful to the client?
(a) “Use a scopolamine patch to decrease secretions.”
(b) “Avoid fluid intake 2 hours before sexual activity. ”
(c) “Place a thin piece of gauze over the tracheostomy.”
(d) “Wash the tracheostomy area with deodorizing antibacterial soap before sexual activity.”
Answer:
(c) “Place a thin piece of gauze over the tracheostomy.”
Explanation:
Placing a thin piece of gauze over the tracheostomy during sexual activity will help to contain the secretions and yet allow ventilation. Although a scopolamine patch may depress the salivary and bronchial secretions, it is not recommended for long-term use and would not be indicated in this situation. Avoiding fluids before sexual activity is not recommended to decrease secretions. Washing the tracheostomy area with any deodorizing soap may cause skin irritation and place the client at risk for infection.
Question 125.
A 52-year-old client is scheduled for a total abdominal hysterectomy for cervical cancer. When discussing the potential impact of this procedure on the client’s sexuality, how should the nurse respond to the client?
(a) “All women experience sexual problems with this surgical procedure. Do you have any questions?”
(b) “When can I schedule an appointment with you and your partner to discuss any issues either of you may have regarding sexuality?”
(c) “Do you anticipate any problems with sex related to your scheduled hysterectomy?”
(d) “Most women have concerns about their sexuality after this type of surgery. Do you have any concerns or questions?”
Answer:
(d) “Most women have concerns about their sexuality after this type of surgery. Do you have any concerns or questions?”
Explanation:
This question introduces some basic information and allows for support for the client who may be experiencing some sexuality concerns. Not all women experience sexual problems after undergoing a hysterectomy. Assuming that the client will want to schedule an appointment with her partner is inappropriate and may embarrass her. Simply asking the client whether she expects to have problems with sex is too abrupt and does not provide any information.
Question 126.
A young man with early-stage testicular cancer is scheduled for a unilateral orchiectomy. The client confides to the nurse that he is concerned about what effects the surgery will have on his sexual performance. Which response by the nurse provides accurate information about sexual performance after an orchiectomy?
(a) “Most impotence resolves in a couple of months.”
(b) “You could have early ejaculation with this type of surgery.”
(c) “We will refer you to a sex therapist because you will probably notice erectile dysfunction.”
(d) “Because your surgery does not involve other organs or tissues, you will likely not notice much change in your sexual performance.”
Answer:
(d) “Because your surgery does not involve other organs or tissues, you will likely not notice much change in your sexual performance.”
Explanation:
Although there may not be a big change in sexual function with a unilateral orchiectomy, the loss of a gonad and testosterone may result in decreased libido and sterility. Sperm banking may be an option worth exploring if the number and motility of the sperm are adequate. The population most affected by testicular cancer is generally young men aged 15 to 34, and in this crucial stage of life, sexual anxieties may be a large concern. Since there will likely not be a big change in sexual function, it is not appropriate to tell the client he will experience impotence, have early ejaculation, or require a referral to a sex therapist.
Question 127.
A young female client is receiving chemotherapy and mentions to the nurse that she and her husband are using a diaphragm for birth control. Which information is most important for the nurse to discuss?
(a) inconvenience of the diaphragm
(b) transmission of sexually transmitted diseases
(c) body changes related to hormones
(d) infection control
Answer:
(d) infection control
Explanation:
The risk of becoming neutropenic during chemotherapy is very high. Therefore, an inserted foreign object such as a diaphragm may be a nidus for infection. Although the nurse may wish to inform the client about the ease with which various contraceptive modalities may be used, the focus of this discussion should be on preventing an infection, which can be fatal for the neutropenic client. There are no data to suggest the client is at risk for acquiring a sexually transmitted disease. The client will not be experiencing body changes directly related to hormonal changes.
Question 128.
To promote comfort and optimal respiratory expansion for a client with chronic obstructive pulmonary disease during sexual intimacy, the nurse can suggest the couple do what?
(a) Use a nasal decongestant inhaler.
(b) Raise the affected partner’s head and upper torso on pillows.
(c) Have the affected partner assume a dependent position.
(d) Limit the duration of the sexual activity.
Answer:
(b) Raise the affected partner’s head and upper torso on pillows.
Explanation:
Raising the upper torso for the affected partner facilitates respiratory function. The client should not use inhalers that are not a part of the treatment plan, and if the client’s health is well managed, it is not necessary to take additional medications to improve respiratory function. A dependent position may compromise respiratory expansion, even though energy may be conserved. Duration of sexual activity is not necessarily related to exertion.
Question 129.
A hospitalized client with end-stage heart failure does not want to be resuscitated. The health care provider (HCP) has written the do-not-resuscitate (DNR) prescription on the client’s record. The client has a cardiac arrest, and the wife tells the nurse she wants the client to be resuscitated and asks the nurse to “do something.” What should the nurse do?
(a) Begin CPR.
(b) Call a “code.”
(c) Page the HCP.
(d) Discuss the DNR prescription with the wife.
Answer:
(d) Discuss the DNR prescription with the wife.
Explanation:
The nurse must respect the wishes of the client who has indicated that he does not wish to be resuscitated and not to initiate CPR. Nurses who resuscitate clients who have directed otherwise may be considered to be battering the client. In this situation, the HCP has written the DNR prescription, and it is not necessary for the nurse to page the HCP. The nurse can be most helpful by explaining the client’s decision to the wife and helping her manage her understand her husband’s wishes and manage her own grief.
Question 130.
A registered nurse (RN) is assigning care on the oncology unit and assigns the client with Kaposi’s sarcoma and human immunodeficiency virus (HIV) infection to the unlicensed assistive personnel (UAP). This person does not want to care for this client. How should the nurse respond?
(a) “I will assign this client to another nurse.”
(b) “I will help you take care of this client so you are confident with the care.”
(c) “You seem worried about this assignment.”
(d) “I will review blood and body fluid precautions with you.”
Answer:
(c) “You seem worried about this assignment.”
Explanation:
The RN assigning care should first give the UAP the opportunity to explore concerns and fears about caring for a client with HIV infection. Reassigning care for this client, assisting with care, and reviewing precautions do not address the present concern or create an environment that will generate useful knowledge regarding future assignments for client care.
Question 131.
A woman employed full-time wants to request a leave of absence to care for her father who is being treated for colon cancer 300 miles (480 km) away. What should the nurse advise the client to do first?
(a) Contact her employee resources department about policies guiding leaves of absence.
(b) Make a plan to see how long she can be out of work without financial concerns.
(c) Find someone to do her work while she is away.
(d) Ask her father if he can afford a caregiver.
Answer:
(a) Contact her employee resources department about policies guiding leaves of absence.
Explanation:
The nurse should advise the client to check with her employer to determine the policies and legislation followed there regarding leaves of absence. While the client can consider the other options, the first step is to obtain information from her employer.
Question 132.
The nurse is developing a care plan for a client with cancer receiving hospice home care. Which would be the most appropriate action for managing the client’s chronic pain?
(a) Administer analgesics regularly and additionally as needed for breakthrough pain.
(b) Sedate the client with tranquilizers.
(c) Avoid intravenous pain medication until the client is terminal.
(d) Administer analgesics when vital signs indicate increased pain severity.
Answer:
(a) Administer analgesics regularly and additionally as needed for breakthrough pain.
Explanation:
Maintaining a steady blood level of analgesics is beneficial for clients with chronic cancer pain. Administering analgesics regularly helps control pain more efficiently. Additional doses of medication may be necessary as ordered for breakthrough pain. Keeping the client overly sedated may not help to control pain. Intravenous analgesics are more effective than oral medications at controlling pain because their distribution is more predictable. Vital signs are not a reliable indicator of how much pain the client is experiencing.
Question 133.
A client and nurse have established a goal for the client to be more autonomous in decision-making. Which situation indicates that the goal has been met?
(a) The health care provider (HCP) directs the client’s care.
(b) The nurse provides the client with the facts and then allows the client to make an independent decision.
(c) The nurse respects a client’s choice not to know particular information.
(d) The health care team makes health and treatment decisions.
Answer:
(c) The nurse respects a client’s choice not to know particular information.
Explanation:
The goal of client autonomy is to respect the client’s choice not to know particular information. The client’s best interests should be determined by the client after he or she receives all the necessary information and in conjunction with other people of the client’s choice, including family, HCP yl], and other health care personnel. The client’s best interests are not totally directed by the HCP or the health care team.
Question 134.
A client who is near death is receiving hospice care to manage severe pain. The client is receiving a narcotic pain medication intravenously per a patient-controlled analgesia (PCA) pump. The client is lethargic, is sleeping much of the time, and has not had any pain for the last 12 hours. What information should the nurse use to make decisions about the care plan?
The client:
(a) received too much medication through an overdose of medication administered through the PCA pump.
(b) may be nearing death as specific dosages and time intervals for self-administration of the analgesic is programmed into the PCA pump to prevent overdose.
(c) has obtained sufficient pain relief because of not having pain in the last 12 hours.
(d) has an IV that has infiltrated and the analgesic has been injected into the subcutaneous tissues, thereby being absorbed faster than prescribed.
Answer:
(b) may be nearing death as specific dosages and time intervals for self-administration of the analgesic is programmed into the PCA pump to prevent overdose.
Explanation:
The client is likely becoming more comatose and is not self-administering the pain medication. The client is not receiving too much medication because the PCA pump has controls to prevent overdose. The client is likely having pain but is not able to recognize it. There is no indication that the IV has infiltrated.
Question 135.
The family of a hospitalized client demonstrates understanding of the teaching about legal documents related to end-of-life care such as “advance directive” and “power of attorney” when they make which statements? Select all that apply.
(a) “Advance directives give instructions about future medical care and treatment.”
(b) “If people are not capable of communicating their wishes, health care providers and family together can agree on measures or actions that will be taken.”
(c) “Ethics experts agree that the family is the sole deciding factor when the client is competent.”
(d) “Medical power of attorney gives primarily financial access to the designee.”
(e) “Medical power of attorney or durable power of attorney for health care is a document that lists who can make health care decisions should a person be unable to make an informed decision for himself or herself.”
(f) “Advance directives give details about the client’s past medical history.”
Answer:
(a) “Advance directives give instructions about future medical care and treatment.”
(b) “If people are not capable of communicating their wishes, health care providers and family together can agree on measures or actions that will be taken.”
(e) “Medical power of attorney or durable power of attorney for health care is a document that lists who can make health care decisions should a person be unable to make an informed decision for himself or herself.”
Explanation:
(a), (b), (e). Advance directives are written statements of person’s wishes related to health care if they are unable to decide for themselves. Power of attorney is a written authorization to represent or act on another’s behalf in private affairs, business, or some other legal matter. These documents relate to current or future health care and not past medical history.
Competent adults are responsible for their own health care decisions and their own right to accept or refuse treatment. Advance directives are used when the person cannot make the decision. Medical power of attorney is a term used to describe the person who makes health care decisions should someone be unable to make informed decisions for himself or herself. The focus is not primarily financial access.
Question 136.
The nurse can be an important advocate for the client who is considering an alternative method of cancer treatment. Which statement best demonstrates the nurse as client advocate?
The nurse will:
(a) provide the information about standard therapies.
(b) monitor blood tests as indicated by the alternative therapy.
(c) document the client’s desire to try an alternative therapy.
(d) allow the client to make health care choices but will assist in ensuring the client is fully informed when making those decisions.
Answer:
(d) allow the client to make health care choices but will assist in ensuring the client is fully informed when making those decisions.
Explanation:
The advocacy role of the nurse implies that the nurse will ensure that the client’s wishes are being respected and the client is making informed decisions. Therefore, the nurse will assist in ensuring that the client is fully informed. The other interventions are appropriate for the nurse but are not related to client advocacy. The client may not understand or have all the necessary information for standard therapy.
A client who is taking an alternative therapy should be monitored for adverse effects. If a client is taking an alternative therapy, it is essential for the health care provider fHCPl lCl| to know so that the therapy can be incorporated into the client’s treatment plan and to ensure that there are no incompatibilities with other therapies or medications.
Question 137.
After completing the nursing assessment for a client and family entering the palliative care program. Which are appropriate nursing goals at this time? Select all that apply.
(a) Modify the family’s usual coping strategies.
(b) Achieve a dignified and respectful death.
(c) Maximize the client’s quality of life.
(d) Provide comfort during the dying process.
(e) Offer support for the client’s family.
(f) Prolong life.
Answer:
(b) Achieve a dignified and respectful death.
(c) Maximize the client’s quality of life.
(d) Provide comfort during the dying process.
(e) Offer support for the client’s family.
Explanation:
(b), (c), (d), (e). Palliative care is health care aimed at symptom management rather than curative treatment for diseases. Nursing care goals include providing comfort and support for the client and family and maximizing the client’s quality of life. Grief counseling is a component, and efforts would be to enhance the coping of all involved, but the family’s usual coping methods would not be altered. Palliative care does not involve advocating to prolong the client’s life.
Question 138.
A client and family have just received the initial diagnosis of colon cancer. In which way can the nurse act as an advocate?
(a) helping them maintain a sense of optimism and hopefulness
(b) determining their understanding of the results of the diagnostic testing
(c) listening carefully to their perceptions of what their needs are
(d) providing them with written materials about the cancer site and its treatment
Answer:
(c) listening carefully to their perceptions of what their needs are
Explanation:
The best nursing advocacy intervention is listening carefully to the client’s and family’s perceptions of their needs. Studies have demonstrated that these needs are not necessarily what the nurse thinks they are. Intervening without listening carefully may result in a lack of responsiveness to the real needs. Helping the client and family maintain a sense of optimism and hopefulness is appropriate but is not necessarily advocacy. Determining the client’s and family’s understanding of the results of the diagnostic testing and providing written materials about the cancer site and its treatment are examples of the nurse’s role as educator.
Question 139.
A client who is dying of acquired immunodeficiency syndrome (AIDS] is admitted to the inpatient psychiatric unit because he attempted suicide. His close friend recently died of AIDS. The client begins to talk about his feelings related to his illness and the loss of his friend. He begins to cry. Which response by the nurse would be most appropriate?
(a) Give the client some tissues, and tell him it is okay to cry.
(b) Tell the client to stop crying and that every thing will be okay.
(c) Sort the client’s mail to distract the client.
(d) Change the subject.
Answer:
(a) Give the client some tissues, and tell him it is okay to cry.
Explanation:
The nurse would give the client a tissue and indicate that it is okay to cry to convey acceptance and empathy. He needs to know that it is natural to have tremendous feelings of loss and sadness. Telling the client to stop crying, busying oneself in the client’s room, and changing the subject are not helpful to the client because they ignore his needs and inhibit the expression of emotion.
Question 140.
The wife of an older adult who has been admitted to the hospital with kidney failure tells the nurse, “I know he doesn’t want to die in a hospital, but it’s so hard for me to take care of him at home.
He said he doesn’t want any more treatment, but I’m not ready to let him go. We have so many arrangements to decide before he dies.” Which statement by the nurse to the client’s wife would be most appropriate? Select all that apply.
(a) “He’s not going to die that soon judging by his current symptoms.”
(b) “What are your fears about your husband dying?”
(c) “I can imagine that it’s hard for you to care for him at home.”
(d) “What do you and your husband know about advance directives?”
(e) “We can discuss types of hospice and home care available.”
(f) “What kind of arrangements do you think need to be made before he dies?”
Answer:
(b) “What are your fears about your husband dying?”
(c) “I can imagine that it’s hard for you to care for him at home.”
(d) “What do you and your husband know about advance directives?”
(e) “We can discuss types of hospice and home care available.”
(f) “What kind of arrangements do you think need to be made before he dies?”
Explanation:
(b), (c), (d), (e),(f). With serious, chronic, and terminal illnesses, it is important to help clients and families address fears, difficulties with home care, advance directives, hospice and home care options, and final arrangements. Predicting the length of life for this client is not appropriate at admission.
Question 141.
A terminally ill client’s husband tells the nurse, “I wish we had taken that trip to Europe last year. We just kept putting it off, and now I'm furious that we didn’t go.” The nurse interprets the husband’s statement as indicating which stage of adaptation to dying?
(a) anger
(b) denial
(c) bargaining
(d) depression
Answer:
(a) anger
Explanation:
The client’s husband is experiencing anger, much of which stems from feelings of guilt about not taking the trip. During the stage of denial, the husband is more likely to deny the client’s diagnosis and prognosis. During the stage of bargaining, the husband would offer to do certain things in exchange for more time before the client dies. In the stage of depression, the husband is likely to make few or no comments and to act dejected.
Question 142.
Which philosophy should the nurse integrate into the plan of care for a client and family to help them best cope during the final stages of the client’s illness?
(a) living each day as it comes as fully as possible
(b) reliving the pleasant memories of days gone by
(c) expecting the worst and being grateful when it does not happen
(d) planning ahead for the remaining good times that will be spent together
Answer:
(a) living each day as it comes as fully as possible
Explanation:
When supporting the friends or family of a terminally ill client, it is best to focus on the present. This can be accomplished by living each day to its fullest. Friends and families also want to know what to expect and want someone to listen to them as they express grief over the approaching death. Focusing on the past can interfere with enjoying the present. Expecting the worst interferes with focusing on day-to-day positive experiences. Planning ahead is inappropriate because of uncertainty when the length of life is unknown.
Question 143.
A client who is in the end stages of cancer is increasingly upset about receiving chemotherapy. Which approach by the nurse would likely be most helpful in gaining the client’s cooperation?
(a) Tell the client how the treatment can be expected to help.
(b) Describe the probable effect that missing a treatment would have.
(c) Explain that being upset makes the treatment more difficult.
(d) Suggest having a massage during the treatment.
Answer:
(a) Tell the client how the treatment can be expected to help.
Explanation:
The best course of action when the client has outbursts concerning treatments is to explain how the treatment is expected to help. Describing the effect if the client misses a treatment is a negative approach and may be threatening to the client. Explaining the effects of being upset does not deal with the client’s feelings. Offering to arrange for a massage during the chemotherapy may be helpful, but it does not deal with the client’s immediate feelings.
Question 144.
A client suspects the end of life is near. However, others talk about only pleasant matters and maintain a persistently cheerful fagade. The nurse plans care for this client by recognizing that these behaviors will most likely cause the client to experience which feeling?
(a) relief
(b) isolation
(c) hope
(d) independence
Answer:
(b) isolation
Explanation:
Clients tend to experience isolation and loneliness when those around them are trying to hide or mask the truth. They are then left to face the realities of death alone. Clients do not experience relief or hopefulness when others are falsely cheer-ful. Independence is promoted by offering realistic choices about care at the end of life.
Question 145.
The young sister of a young adult client with leukemia asks, “Can you check my blood? When my sister got pneumonia, so did I. And I think I have this, too.” How should the nurse respond? Select all that apply.
(a) Ask the client’s health care provider to take a sample of the sister’s blood.
(b) Explain to the sister that leukemia is not a communicable disease.
(c) Discuss the sister’s concern with her parents.
(d) Tell the sister’s parents about a group for siblings of clients with terminal illness.
(e) Ask the sister about her concerns.
Answer:
(c) Discuss the sister’s concern with her parents.
(d) Tell the sister’s parents about a group for siblings of clients with terminal illness.
(e) Ask the sister about her concerns.
Explanation:
(c), (d), (e). Taking a blood sample is an unnecessary, invasive procedure that would not directly address the sister’s fear. Leukemia is not considered a communicable disease. The nurse should first determine the sister’s concerns, and then alert the parents to the sister’s concerns and also tell the parents about resources that are available to assist siblings to cope with a terminal illness in the family.
Question 146.
When talking with the nurse, the brother of a client with leukemia says, “We used to play pretty rough games together. Maybe some of the bruises he got when I tackled him caused this.” Which statement is the nurse’s best response?
(a) “Don’t feel guilty. You didn’t cause your brother’s illness.”
(b) “I can see you’re worried. Let’s talk about how people get leukemia.”
(c) “Here’s some information about leukemia for you to read.”
(d) “Lots of people worry about things like this. It’s not your fault.”
Answer:
(b) “I can see you’re worried. Let’s talk about how people get leukemia.”
Explanation:
A response that acknowledges the brother’s concern and provides him with information is most helpful. Therefore, telling the brother that the nurse sees that he is worried and then following this up with a discussion about leukemia is most appropriate. Providing reassurance or information without acknowledging the expressed concern is not as helpful as acknowledging the concern and providing the information. Although acknowledging his worry is appropriate, more importantly, the brother needs factual information about the disease.
Question 147.
A nurse is making follow-up phone calls to clients being treated for cancer. In which order of priority from first to last should the nurse return the calls? All options must be used.
(a) the client receiving chemotherapy who has a loss of appetite
(b) the client who underwent a mastectomy 2 weeks ago who called for information on the Reach for Recovery program
(c) the client receiving spinal radiation for bone cancer metastases who has urinary incontinence
(d) the client with colon cancer who has questions about a high-fiber diet
Answer:
(c) the client receiving spinal radiation for bone cancer metastases who has urinary incontinence
(a) the client receiving chemotherapy who has a loss of appetite
(d) the client with colon cancer who has questions about a high-fiber diet
(b) the client who underwent a mastectomy 2 weeks ago who called for information on the Reach for Recovery program
Explanation:
(c), (a), (d), (b). Using Maslow’s hierarchy of needs to set priorities, the nurse should first call the client with bone cancer metastases to the spine because this client is at risk for compression, damage, or severing of the spinal cord. The nurse should evaluate the client immediately for urinary incontinence, paralysis, difficulty ambulating, and possible weakness or loss of motor function.
The nurse should next call the client with loss of appetite to assess weight loss and suggest ways to increase the appetite. The client with colon cancer requires assistance with diet planning, also a physiologic need, but this client is not at high risk for weight loss. Lastly, the nurse should obtain information on Reach to Recovery and return the call to the client with a mastectomy. The needs of this client are the least urgent.
Question 148.
The nurse is making client rounds following shift report. Which client should the nurse assess first?
(a) a 38-year-old woman receiving internal radiation therapy for cervical cancer
(b) a 27-year-old man with leukemia hospitalized for induction of high-dose chemotherapy
(c) a 75-year-old man with metastatic prostate cancer with a pathologic fracture of the femur who is in pain
(d) a 23-year-old woman undergoing surgery for placement of a central venous catheter
Answer:
(c) a 75-year-old man with metastatic prostate cancer with a pathologic fracture of the femur who is in pain
Explanation:
The nurse should first assess the 75-year-old man with prostate cancer because of the client’s age, need for pain management, extended bed rest, and the potential for preexisting nutritional deficits. The nurse should plan to spend a focused but short time with the woman receiving internal radiation. The client who will receive chemotherapy will require more observation after receiving the medication. The nurse can assess the client who will have a central venous catheter after assuring the older client is comfortable.
Question 149.
The RN is administering intravenous chemotherapy to a client with cancer. Which precautions are necessary when administering chemotherapy? Select all that apply.
(a) taping all IV tubing connections
(b) wearing gloves when handling the client’s urine
(c) disposing of chemotherapy waste as hazardous material
(d) wearing a long-sleeved gown when administering chemotherapy
(e) disposing of sharps in a specifically labeled container.
Answer:
(b) wearing gloves when handling the client’s urine
(c) disposing of chemotherapy waste as hazardous material
(d) wearing a long-sleeved gown when administering chemotherapy
(e) disposing of sharps in a specifically labeled container.
Explanation:
(b), (c), (d), (e). Nurses preparing and administering chemotherapy wear gloves and a disposable, longsleeved gown. Antineoplastic agents are disposed of as hazardous material, and gloves are always worn when handling the excretions of clients who have received chemotherapy. Sharps must be disposed of in a sharps container labeled “chemotherapy items.” It is not appropriate to tape IV tubing connections; antineoplastic agents are administered using LuerLok fittings on all intravenous tubing to minimize the risk of exposure from needlestick injury.
Question 150.
During the intravenous administration of a chemotherapeutic vesicant drug, the nurse observes that there is a lack of blood return from the intravenous catheter. What should the nurse do first?
(a) Stop the administration of the drug.
(b) Reposition the client’s arm and continue with administration of the drug.
(c) Irrigate the catheter with normal saline.
(d) Continue to administer the drug and assess for edema at the IV site.
Answer:
(a) Stop the administration of the drug.
Explanation:
An intravenous catheter with no blood return is most likely occluded and not patent. A chemotherapeutic vesicant drug extravasates into the surrounding skin tissue and causes tissue necrosis. The nurse stops the administration of the drug immediately. Repositioning the arm does not improve patency. Irrigating the catheter may cause the medication to enter the tissue. It is inappropriate to wait and see if the arm becomes edematous because of the vesicant action of the drug.
Question 151.
The nurse is caring for a client with end-stage cancer whose health status is declining. A prescription is written by the attending health care provider (HCP) to withhold all fluid, but the health care team cannot locate a family member or guardian. The nurse requests an ethics consultation. Which information is true of an ethics consultation? Select all that apply.
(a) Persons requesting an ethics consultation may do so without intimidation or fear of reprisal.
(b) Ethics consultations may prevent poor outcomes in cases involving ethical problems.
(c) The recommendations of ethics consultants are advisory only.
(d) Requests for ethics consultations may only be made by the HCP or nurse.
(e) Ethics consultation is intended to provide legal advice on client care.
Answer:
(a) Persons requesting an ethics consultation may do so without intimidation or fear of reprisal.
(b) Ethics consultations may prevent poor outcomes in cases involving ethical problems.
(c) The recommendations of ethics consultants are advisory only.
Explanation:
(a), (b), (c). Ethics consultation seeks to facilitate communication and shared decision-making in client care. Ethics consultations also tend to increase knowledge of clinical ethics, improve client care, and prevent poor outcomes in cases involving ethical problems. Requests for ethics consultations can be made by any member of the health care team and by clients, family members, guardians, students, or others with a legitimate interest in the client. The recommendations of ethics consultants are advisory only; the ethics consultation process is intended to supplement and support existing departmental and institutional mechanisms for making decisions and resolving conflict in clinical practice.
Clinicians are encouraged to seek an ethics consultation when the client is incapacitated when no family member/s or guardian/s exists or can be found or when the client’s family members disagree about the ethically appropriate action to be taken. Ethics consultation is not intended or authorized to provide legal advice on client care. Persons requesting an ethics consultation may do so without intimidation or fear of reprisal.
Question 152.
The nurse manager on the oncology unit wants to improve documentation of the effectiveness of analgesia medication within 30 minutes after administration. What should the nurse manager do
first?
(a) Change the policy of documentation to 45 minutes.
(b) Consult the pharmacist.
(c) Consult the nurses on the evening shift where documentation of analgesia is the greatest problem.
(d) Complete a brief quality improvement study and chart audit to document the rate of adherence to the policy and the pattern of documentation over shifts.
Answer:
(d) Complete a brief quality improvement study and chart audit to document the rate of adherence to the policy and the pattern of documentation over shifts.
Explanation:
To determine the cause of this problem, a quality improvement study should be conducted along with a chart audit. Before implementing solutions to a problem, the precise issues in the hospital system must be observed and documented. Changing the time to chart from 30 to 45 minutes does not solve the problem. It is not the pharmacist’s role to provide consultation about documentation of drugs administered by nurses. Consulting the evening nurses may be helpful, but this is a systems issue of the entire unit and involves every registered nurse (RN) administering analgesia.
Question 153.
A registered nurse [RN) instructs the unlicensed assistive personnel (UAP) to check the urine intake and output (I&O) on clients on the oncology unit at the end of the 8-hour shift. It is important for the nurse to instruct the UAP to do what?
(a) Ask the clients if they are thirsty when calcu lating the I&O.
(b) Report back to the nurse immediately if any client has an output <240 mL.
(c) Document the I&O results on the medical records.
(d) Write the I&O results down for the nurse to give report to the next shift.
Answer:
(b) Report back to the nurse immediately if any client has an output <240 mL.
Explanation:
The RN is responsible for describing to the UAP when to report to the RN a result that indicates a potential client problem with dehydration. The RN must assess and interpret results but must also give concrete feedback to the UAP on what is an expected situation or a specific result to report back to the RN. Urine output should be at least 30 mL/h, or 240 mL, over the 8-hour shift.
Dehydrated clients may be thirsty, and the UAP can ask if the client is thirsty and offer water if permitted. However, because urine output is the critical indicator of dehydration, the UAP should document I&O and give results outside the normal range to the nurse. The nurse is specifically assessing dehydration and should request to receive this information from the UAP before it is charted and reported to the next shift.
Question 154.
An alert and oriented older adult female with metastatic lung cancer is admitted to the medical- surgical unit for treatment of heart failure. She was given 80 mg of furosemide in the emergency department. The nurse is instructing the unlicensed assistive personnel (UAP) to implement a nursing plan to manage potential incontinence. Which instruction will be most effective for this client?
(a) prescribing adult diapers for the client so she will not have to worry about incontinence
(b) requesting an indwelling urinary catheter to avoid incontinence
(c) padding the bed with extra absorbent linens
(d) placing a commode at the bedside and instructing the client in its use
Answer:
(d) placing a commode at the bedside and instructing the client in its use
Explanation:
A bedside commode should be near the client for easy, safe access. Measurement of urine output is also important in a client with heart failure. Putting diapers on an alert and oriented individual would be demeaning and inappropriate. Indwelling catheters are associated with increased risk of infection and are not a solution to possible incontinence. There is no reason to think that the client would not be able to use the bedside commode.
Question 155.
The nursing team on an oncology unit consists of a registered nurse (RN), a licensed practical/ vocational nurse (LPN/VN), and one unlicensed assistive personnel (UAP). Which client should be assigned to the RN?
(a) a 52-year-old client with lung cancer admit ted for acute dyspnea
(b) a 45-year-old client receiving tube feedings
(c) a 28-year-old client being evaluated for a bone marrow transplant
(d) a 65-year-old client diagnosed with endometrial cancer who underwent an abdominal hysterectomy 3 days ago
Answer:
(a) a 52-year-old client with lung cancer admit ted for acute dyspnea
Explanation:
Ongoing assessment by the RN is required to evaluate the client with dyspnea to monitor for potential deterioration of the respiratory status. If the RN is the care provider, the RN will have greater interaction with the individual client. The RN is responsible for assessment of all the clients. The other clients would not be considered unstable, and maintaining a patent airway is always the priority in providing care. Care for the other clients could be assigned safely, according to the abilities of the LPN/VN and UAP.
Question 156.
The nurse is to wear personal protective equipment (PPE) to administer a chemotherapeutic agent to the client. What guidelines should the nurse use for PPE use and care? Select all that apply.
(a) Understand the proper use and limitations of PPE.
(b) Use care in removing all items to reduce contamination.
(c) Ensure that PPE is made of materials that allow for air ventilation.
(d) Sanitize the hands with alcohol-based solution before putting gloves on and after removing gloves.
(e) Discard the PPE in containers for contaminated waste.
Answer:
(a) Understand the proper use and limitations of PPE.
(b) Use care in removing all items to reduce contamination.
(e) Discard the PPE in containers for contaminated waste.
Explanation:
(a), (b),(e). Employers should provide appropriate PPE to protect workers who handle hazardous drugs in the workplace. The following general guidelines apply to PPE use and care: select specific respirators and protective clothing based on an assessment of the potential exposure to hazardous drugs; understand proper use and limitations of any selected PPE to ensure that it functions properly; and use care in donning and removing all items to prevent damage to PPE and to reduce the spread of contamination.
The PPE must be constructed of materials that are appropriate for hazardous drug exposure. Hands must be thoroughly washed with soap and water both before donning and after removing gloves. Consider all PPE worn when handling hazardous drugs as being contaminated; contain and dispose of such PPE as contaminated waste.
Question 157.
The nurse should ensure that which item is placed when the client is to receive intravascular therapy for more than 6 days?
(a) short peripheral catheter
(b) central venous access in the femoral vein
(c) intravenous catheter insertion device
(d) peripherally inserted central catheter (PICC)
Answer:
(d) peripherally inserted central catheter (PICC)
Explanation:
When the duration of intravascular therapy is likely to be more than 6 days, a midline catheter or peripherally inserted central catheter (PICC) is preferred to a short peripheral catheter. In adult clients, use of the femoral vein for central venous access should be avoided. Steel needles should be avoided when administering fluids and medications that might cause tissue necrosis if extravasation occurs.