RN NCLEX Questions serve as a benchmark for assessing individual progress and readiness for the licensure exam.
NCLEX Biliary Tract Disorders Questions
Biliary Tract Disorders NCLEX Practice Questions
Question 1.
A client has undergone a laparoscopic cho-lecystectomy. Which instruction should the nurse include in the discharge teaching?
(a) Empty the bile bag daily.
(b) Breathe deeply into a paper bag when nauseated.
(c) Keep adhesive dressings in place for 6 weeks.
(d) Report bile-colored drainage from any incision.
Answer:
(d) Report bile-colored drainage from any incision.
Explanation:
There should be no bile-colored drainage coming from any of the incisions postoperatively. A laparoscopic cholecystectomy does not involve a bile bag. Breathing deeply into a paper bag will prevent a person from passing out due to hyperventilation; it does not alleviate nausea. If the adhesive dressings have not already fallen off, they are removed by the surgeon in 7 to 10 days, not 6 weeks.
Question 2.
A client with acute cholecystitis has severe pain. Which prescription will be most effective in relieving the pain?
(a) infusing normal saline solution at 100 mL/h
(b) administering morphine sulfate 10 mg IM every 3 to 4 hours
(c) receiving nothing by mouth (NPO)
(d) having a nasogastric tube connected to low intermittent suction
Answer:
(b) administering morphine sulfate 10 mg IM every 3 to 4 hours
Explanation:
The client is in severe pain, and the nurse should administer the morphine to relieve the pain. The client will receive IV fluids to maintain fluid and electrolyte balance, but that will not relieve the pain. The client may be NPO and have a nasogastric tube to promote gastric decompression to prevent further gallbladder stimulation, but these are not sufficient to manage the pain.
Question 3.
A client is admitted to the hospital with a diagnosis of cholecystitis. The client has severe abdominal pain and nausea and has vomited 120 mL. Based on these data, which nursing action would have the highest priority at this time?
(a) Manage anxiety.
(b) Restore fluid loss.
(c) Manage the pain.
(d) Replace nutritional loss.
Answer:
(c) Manage the pain.
Explanation:
The priority for nursing care at this time is to decrease the client’s severe abdominal pain. The pain, which is frequently accompanied by nausea and vomiting, is caused by biliary spasm. Opioid analgesics are given to relieve the severe pain and spasm of cholecystitis. Relief of pain may decrease nausea and vomiting and thereby decrease the client’s likelihood of developing further complications, such as severe fluid loss and inadequate nutrition. There are no data to suggest that the client is anxious.
Question 4.
A client’s stools are light gray in color. What additional information should the nurse obtain from the client? Select all that apply.
(a) intolerance to fatty foods
(b) fever
(c) jaundice
(d) respiratory distress
(e) pain at McBurney’s point
(f) bleeding ulcer
Answer:
(a) intolerance to fatty foods
(b) fever
(c) jaundice
Explanation:
(a), (b), (c). Bile is created in the liver, stored in the gallbladder, and released into the duodenum, giving stool its brown color. A bile duct obstruction can cause pale-colored stools. Other symptoms associated with cholelithiasis are right upper quadrant tenderness, fever from inflammation or infection, jaundice from elevated serum bilirubin levels, and nausea or right upper quadrant pain after a fatty meal. Pain at McBurney’s point lies between the umbilicus and right iliac crest and is associated with appendicitis. A bleeding ulcer produces black, tarry stools. Respiratory distress is not a symptom of cholelithiasis.
Question 5.
A client who has been scheduled to have a choledocholithotomy expresses anxiety about having surgery. Which nursing intervention would be the most appropriate to achieve the outcome of anxiety reduction?
(a) providing the client with information about what to expect postoperatively
(b) telling the client not to be afraid
(c) reassuring the client by saying that surgery is a common procedure
(d) stressing the importance of following the health care provider’s (HCP’s) instructions after surgery
Answer:
(a) providing the client with information about what to expect postoperatively
Explanation:
Providing information can help to answer the client’s questions and decrease anxiety. Fear of the unknown can increase anxiety. Telling the client not to be afraid, that the procedure is common, or to follow the HCP’s prescriptions will not necessarily decrease anxiety.
Question 6.
A client has an open cholecystectomy with bile duct exploration. Following surgery, the client has a T tube. What should the nurse do to determine the effectiveness of the T tube?
(a) Irrigate the tube with 20 mL of normal saline every 4 hours.
(b) Unclamp the T tube and empty the contents every day.
(c) Assess the color and amount of drainage every shift.
(d) Monitor the incision sites for bile drainage.
Answer:
(c) Assess the color and amount of drainage every shift.
Explanation:
A T tube is inserted in the common bile duct to maintain patency when there is a likelihood of edema. The tube remains in place until edema from the duct exploration subsides. The bile color should be gold to dark green, and the amount of drainage should be closely monitored to ensure tube patency. Irrigation is not routinely done, unless prescribed using a smaller volume of fluid. The T tube is not clamped in the early post-op period to allow for continuous drainage. An open cholecystectomy has one right subcostal incision, whereas a laparoscopic cholecystectomy has multiple small incisions.
Question 7.
At 0800, the nurse reviews the amount of T-tube drainage for a client who underwent an open cholecystectomy yesterday. After reviewing the output record (see chart), what should the nurse do next?
|
Time |
T-Tube |
|
1200 |
50 mL |
|
1600 |
60 mL |
|
2000 |
60 mL |
|
0000 |
70 mL |
|
0400 |
70 mL |
|
0800 |
10 mL |
(a) Report the 24-hour drainage amount at 1200.
(b) Clamp the T tube.
(c) Evaluate the tube for patency.
(d) Irrigate the T tube.
Answer:
(c) Evaluate the tube for patency.
Explanation:
The T tube should drain approximately 300 to 500 mL in the first 24 hours, and after 3 to 4 days the amount should decrease to <200 mL in 24 hours. With the sudden decrease in drainage at 0800, the nurse should immediately assess the tube for obstruction of flow that can be caused by kinks in the tube or the client lying on the tube. Drainage color must also be assessed for signs of bleeding. The tube should not be irrigated or clamped without a prescription.
Question 8.
A client who had a cholecystectomy has a T-tube for drainage. The nurse measures the amount of bile drainage from the T tube at the end of each shift. How should the nurse record the drainage?
(a) adding it to the client’s urine output
(b) charting it separately on the output record
(c) adding it to the amount of wound drainage
(d) subtracting it from the total intake for each day
Answer:
(b) charting it separately on the output record
Explanation:
T-tube bile drainage is recorded separately on the output record. Adding the T-tube drainage to the urine output or wound drainage makes it difficult to accurately determine the amounts of bile, urine, or drainage. The client’s total intake will be incorrect if drainage is subtracted from it.
Question 9.
The nurse is caring for a client who had an open cholecystectomy 24 hours ago. The client’s vital signs have been stable over the last 24 hours, with most recent temperature 98.6°F (37°C), blood pressure (BP) 118/76 mm Hg, respiratory rate (RR) 16 breaths/min, and heart rate (HR) 78 bpm, but these signs are now changing. Which set of vital signs indicates that the nurse should contact the health care provider (HCP)?
(a) temperature 101.8°F (38.8°C), BP 140/86 mm Hg, HR 94 bpm, RR 24 breaths/min
(b) temperature 100.7°F (38.2°C), BP 118/68 mm Hg, HR 84 bpm, RR 20 breaths/min
(c) temperature 99.5°F (37.5°C), BP 126/80 mm Hg, HR 58 bpm, RR 16 breaths/min
(d) temperature 97.5°F (36.4°C), BP 98/64 mm Hg, HR 98 bpm, RR 18 breaths/min
Answer:
(a) temperature 101.8°F (38.8°C), BP 140/86 mm Hg, HR 94 bpm, RR 24 breaths/min
Explanation:
This client is exhibiting signs of sepsis, and the nurse should notify the health care provider. The client has three signs indicating sepsis: temperature >101.CPF (38.3°C) (or <96.8°F [36°C]), HR >90 bpm, and RR >20 breaths/min. At least two of these variables are required to diagnose sepsis.
Question 10.
After a cholecystectomy, the client is to follow a low-fat diet. Which food would be most appropriate to include in a low-fat diet?
(a) cheese omelet with onions
(b) peanut butter on wheat toast
(c) ham salad sandwich made with mayonnaise
(d) roast beef sandwich with lettuce and tomato
Answer:
(d) roast beef sandwich with lettuce and tomato
Explanation:
Lean meats, such as beef, lamb, veal, and well-trimmed lean ham and pork, are low in fat. Rice, pasta, and vegetables are low in fat when not served with butter, cream, or sauces. Fruits are low in fat. The amount of fat allowed in a client’s diet after a cholecystectomy will depend on the client's ability to tolerate fat. Typically, the client does not require a special diet but is encouraged to avoid excessive fat intake. A cheese omelet and peanut butter have high fat content. Ham salad is high in fat from the fat in a mayonnaise-based salad dressing.
Question 11.
A client with cholecystitis has severe pain unrelieved by ibuprofen. The client feels nauseated. The nurse obtains the following vital signs: temperature 101.1°F (38.4°C); pulse 114 bpm; respirations 22 breaths/min; blood pressure 142/90 mm Hg. Using the SBAR (Situation-Background-Assessment- Recommendation) technique for communication, what should the nurse recommend to the health care provider for this client?
(a) a medication for severe pain
(b) a medication for increased temperature
(c) a medication for elevated blood pressure
(d) a medication for feelings of nausea
Answer:
(a) a medication for severe pain
Explanation:
The client has severe pain, and the nurse should contact the health care provider for pain medication. An opioid such as morphine is usually prescribed intravenously to manage the severe pain. Elevation of heart rate and blood pressure is likely due to the pain. The pain medication may also relieve the nausea.
Question 12.
The nurse prepares to administer promethazine 35 mg IM prescribed as needed for a client with cholecystitis who has severe nausea. The ampule label reads that the medication is available in 25 mg/mL. How many milliliters should the nurse administer? Record your answer using one decimal place.................. mL.
Answer:
1.4 mL.
The following formula is used to calculate the correct dosage:
35 mg/XmL = 25mg/1 mL
X = 1.4 mL
Question 13.
A client undergoes a laparoscopic cholecystectomy. Which instructions should the nurse give the client about a diet immediately after surgery?
(a) “You can’t eat or drink anything for 24 hours.”
(b) “You may resume your normal diet the day after your surgery.”
(c) “Start with liquids and see how you feel.”
(d) “You can progress from a liquid to a bland diet as tolerated.”
Answer:
(c) “Start with liquids and see how you feel.”
Explanation:
Immediately after surgery, the client can drink liquids. A light or regular diet can be resumed when the client can tolerate the liquids. There is no need for the client to remain on nothing-by-mouth status after surgery because peristaltic bowel activity should not be affected. The client will probably not be able to tolerate a full meal comfortably the day after surgery. There is no need for the client to stay on a bland diet after a laparoscopic cholecystectomy. The client should, however, avoid excessive fats.
Question 14.
Which discharge instruction would be appropriate for a client who has had a laparoscopic cholecystectomy and has sutures covered by a dressing?
(a) Avoid showering for 1 week after surgery.
(b) Return to work within 1 week.
(c) Leave dressing in place until seeing the sur geon at the postoperative visit.
(d) Use acetaminophen to control any fever.
Answer:
(c) Leave dressing in place until seeing the sur geon at the postoperative visit.
Explanation:
After a laparoscopic cholecystectomy when there are sutures covered by a dressing, the client should not remove dressings from the puncture sites but should wait until visiting the surgeon. The client may shower 48 hours after surgery. A client can return to work within 1 week, but only if approved by the surgeon and no strenuous activity is involved. The client should report any fever, which could be an indication of a complication.
Question 15.
A client who has had a laparoscopic chole-cystectomy has adhesive strips over the puncture sites. When preparing the client for discharge, which client statements indicate that the teaching has been successful? Select all that apply.
(a) “I can resume my normal diet when I feel ok.”
(b) “I need to avoid driving for about 4 weeks.”
(c) “I may experience some pain in my right shoulder.”
(d) “I should spend 2 to 3 days in bed before resuming activity.”
(e) “I can take a shower 2 days later.”
Answer:
(a) “I can resume my normal diet when I feel ok.”
(c) “I may experience some pain in my right shoulder.”
(e) “I can take a shower 2 days later.”
Explanation:
(a) , (c), (e). Following a laparoscopic cholecystectomy, the client can resume a normal diet as tolerated. The client may experience right shoulder pain from the gas that was used to inflate the abdomen during surgery. The client can take a shower 48 hours after the surgery. The adhesive strips will fall off in about 10 days. The client can resume driving within 3 to 4 days following surgery as long as the client is not taking pain medication. There is no need for the client to maintain bed rest in the days following surgery. Light exercise such as walking can be resumed immediately.
Question 16.
Following an emergency cholecystectomy, the client has a Jackson-Pratt drain with closed suction. After 4 hours, the drainage unit is full. What should the nurse do?
(a) Notify the surgeon.
(b) Remove the drain and suction unit.
(c) Check the dressing for bleeding.
(d) Empty the drainage unit.
Answer:
(d) Empty the drainage unit.
Explanation:
Portable suction units should be emptied and drained every shift or when full. It is normal for the unit to fill within the first hours after surgery; the nurse does not need to contact the surgeon. There should not be bleeding on the dressing if the drainage system is emptied when full. The drain should not be removed until prescribed by the health care provider (HCP).
Question 17.
The client who has been hospitalized with pancreatitis does not drink alcohol because of religious convictions. The client becomes upset when the health care provider (HCP) persists in asking about alcohol intake. What should the nurse tell the client about the reason for these questions?
(a) “There is a strong link between alcohol use and acute pancreatitis.”
(b) “Alcohol intake can interfere with the tests used to diagnose pancreatitis.”
(c) “Alcoholism is a major health problem, and all clients are questioned about alcohol intake.”
(d) “The health care provider must obtain the pertinent facts, regardless of religious beliefs.”
Answer:
(a) “There is a strong link between alcohol use and acute pancreatitis.”
Explanation:
Alcoholism is a major cause of acute pancreatitis in the United States and Canada. Because some clients are reluctant to discuss alcohol use, staff may inquire about it in several ways. Generally, alcohol intake does not interfere with the tests used to diagnose pancreatitis. Recent ingestion of large amounts of alcohol, however, may cause an increased serum amylase level.
Large amounts of ethyl and methyl alcohol may produce an elevated urinary amylase concentration. All clients are asked about alcohol and drug use on hospital admission, but this information is especially pertinent for clients with pancreatitis. HCPs JTJ do need to seek facts, but this can be done while respecting the client’s religious beliefs. Respecting religious beliefs is important in providing holistic client care.
Question 18.
A client with acute pancreatitis has a blood pressure of 88/40 mm Hg, heart rate of 128 bpm, res-pirations of 28 breaths/min, and Grey Turner’s sign. What prescription should the nurse implement first?
(a) Initiate intake/output record.
(b) Place an intravenous line.
(c) Position on the left side.
(d) Insert a nasogastric tube.
Answer:
(b) Place an intravenous line.
Explanation:
Grey Turner’s sign is a bluish discoloration in the flank area caused by retroperitoneal bleeding. The vital signs are showing hemodynamic instability. IV access should be obtained to provide immediate volume replacement. The urine output will provide information on the fluid status. A nasogastric tube is indicated for clients with uncontrolled nausea and vomiting or gastric distension. Repositioning the client may be considered for pain management once the client’s vital signs are stable.
Question 19.
On 1/16 at 0800, the nurse is caring for a client with acute pancreatitis and reviewing progress notes, (see notes) as listed: Which finding indicates that the desired outcome of the transfusion is obtained at this time?
|
Date |
time |
Progress Notes |
|
1/15 |
0800 |
Vittal sings are: temperature 37.4°C, heart rate, 138;Bp is 80/48; Pain is 9 on a 10-point scale; client is retless. |
|
1/15 |
1000 |
Discussed following lab Values with A. Smith,m MD: hematocrit is 27.6%, hemoglobin is 7.6 g/dl (76 g/l), platelet count is 245,000 mm3, and INR is 0.8 |
|
1/15 |
1100 |
PRBCs infused; no adverse reactions. |
(a) Blood pressure (BP) is 110/80 mm Hg.
(b) Pain is 4 on a 10-point scale.
(c) Hemoglobin is 12 g/dL.
(d) Platelet count is 144,000/mm3.
Answer:
(c) Hemoglobin is 12 g/dL.
Explanation:
Packed red blood cells (RBCs) are prescribed to improve the low hemoglobin level; therefore, the nurse assesses for an increase in hemoglobin. The PRBCs do not increase BP; colloid solutions are needed to increase the circulating blood volume and raise the BP. The client has acute pain and requires the use of analgesia to minimize the pain. The platelet count is within normal limits and is not affected by the infusion of PRBCs.
Question 20.
The nurse should monitor the client with acute pancreatitis for which complication?
(a) heart failure
(b) duodenal ulcer
(c) cirrhosis
(d) pneumonia
Answer:
(d) pneumonia
Explanation:
The client with acute pancreatitis is prone to complications associated with the respiratory system. Pneumonia, atelectasis, and pleural effusion are examples of respiratory complications that can develop as a result of pancreatic enzyme exudate. Pancreatitis does not cause heart failure, ulcer formation, or cirrhosis.
Question 21.
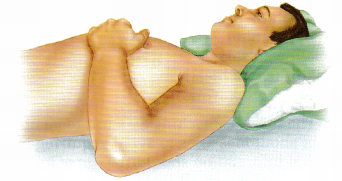
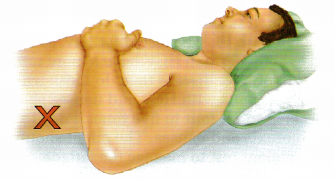
When the nurse is providing care for a client hospitalized with acute pancreatitis who has severe abdominal pain, which nursing interventions would be most appropriate for this client? Select all that apply.
(a) Place the client in a side-lying position.
(b) Administer morphine sulfate for pain as needed.
(c) Maintain the client on a high-calorie, high- protein diet.
(d) Monitor the client’s respiratory status.
(e) Obtain daily weights.
Answer:
(a) Place the client in a side-lying position.
(b) Administer morphine sulfate for pain as needed.
(d) Monitor the client’s respiratory status.
(e) Obtain daily weights.
Explanation:
(a), (b), (d), (e). The client with acute pancreatitis usually experiences severe abdominal pain. The client will likely receive an opioid such as morphine to treat the pain. Placing the client in a side-lying position relieves the tension on the abdominal area and promotes comfort. A semi Fowler’s position is also appropriate. The nurse should also monitor the client’s respiratory status because clients with pancreatitis are prone to develop respiratory complications. Daily weights are obtained to monitor the client’s nutritional and fluid volume status. During the acute phase of the illness while the client is experiencing pain, the pancreas is rested by withholding food and drink. When the diet is reintroduced, it is a high-carbohy-drate, low-fat, bland diet.
Question 22.
The nurse notes that a client with acute pancreatitis occasionally experiences muscle twitching and jerking. How should the nurse interpret the significance of these symptoms?
(a) The client may be developing hypocalcemia.
(b) The client is experiencing a reaction to meperidine.
(c) The client has a nutritional imbalance.
(d) The client needs a muscle relaxant to promote rest.
Answer:
(a) The client may be developing hypocalcemia.
Explanation:
Hypocalcemia develops in severe cases of acute pancreatitis. The exact cause is unknown. Signs and symptoms of hypocalcemia include jerk-ing and muscle twitching, numbness of lingers and lips, and irritability. Meperidine may cause tremors or seizures as an adverse effect, but not muscle twitching. Muscle twitching is not caused by a nutritional deficit, nor does it indicate that the client needs a muscle relaxant.
Question 23.
A client is receiving propantheline bromide in the management of acute pancreatitis. Which finding would indicate that the nurse should discuss withholding the medication with the health care provider?
(a) absent bowel sounds
(b) increased urine output
(c) diarrhea
(d) decreased heart rate
Answer:
(a) absent bowel sounds
Explanation:
Propantheline is an anticholinergic, antispasmodic medication that decreases vagal stimulation and pancreatic secretions. It is contraindicated in paralytic ileus; therefore, the nurse should be concerned with the absent bowel sounds. Side effects are urinary retention, constipation, and tachycardia.
Question 24.
Which dietary instruction would be appropriate for the nurse to give a client who is recovering from acute pancreatitis?
(a) Avoid crash dieting.
(b) Restrict carbohydrate intake.
(c) Eat six small meals a day.
(d) Decrease sodium in the diet.
Answer:
(a) Avoid crash dieting.
Explanation:
Crash dieting or bingeing may cause an acute attack of pancreatitis and should be avoided. Carbohydrate intake should be increased because carbohydrates are less stimulating to the pancreas. There is no need to maintain a dietary pattern of six meals a day; the client can eat whenever desired. There is no need to place the client on a sodium-restricted diet because pancreatitis does not promote fluid retention.
Question 25.
Pancreatic enzyme replacements are prescribed for the client with chronic pancreatitis.
When should the nurse instruct the client to take them to obtain the most therapeutic effect?
(a) three times daily between meals
(b) with each meal and snack
(c) in the morning and at bedtime
(d) every 4 hours, at specified times
Answer:
(b) with each meal and snack
Explanation:
In chronic pancreatitis, destruction of pancreatic tissue requires pancreatic enzyme replacement. Pancreatic enzymes are prescribed to facilitate the digestion of proteins and fats and should be taken in conjunction with every meal and snack. Specified hours or limited times for administration are ineffective because the enzymes must be taken in conjunction with food ingestion.
Question 26.
The client has chronic pancreatitis. What should the nurse teach the client to do to monitor the effectiveness of pancreatic enzyme replacement?
(a) Record daily fluid intake.
(b) Perform glucose fingerstick tests twice a day.
(c) Observe stools for steatorrhea.
(d) Test urine for ketones.
Answer:
(c) Observe stools for steatorrhea.
Explanation:
If the dosage and administration of pancreatic enzymes are adequate, the client’s stool will be relatively normal. Any increase in odor or fat content would indicate the need for dosage adjustment. Stable body weight would be another indirect indicator. Fluid intake does not affect enzyme replacement therapy. If diabetes has developed, the client will need to monitor glucose levels. However, glucose and ketone levels are not affected by pancreatic enzyme therapy and would not indicate effectiveness of the therapy.
Question 27.
The nurse is assessing a client with chronic hepatitis B who is receiving lamivudine. What information about the client is most important to communicate to the health care provider?
(a) a 3-kg weight gain over 2 days
(b) intermittent nausea
(c) a temperature of 99°F (37.2°C) orally
(d) constant fatigue
Answer:
(a) a 3-kg weight gain over 2 days
Explanation:
The fluid weight gain is of concern since the drug should be used with caution with impaired renal function. Dosage adjustment may be needed with renal insufficiency since the drug is excreted in the urine. Nausea, minor temperature elevation, and fatigue are symptoms that should be monitored, but are associated with hepatitis.
Question 28.
The nurse is assessing a client with hepatitis A and notices that the aspartate transaminase (AST) and alanine transaminase (ALT) lab values have increased. Which statement by the client indicates the need for further instruction by the nurse?
(a) “I require increased periods of rest.”
(b) “I follow a low-fat, high-carbohydrate diet.”
(c) "I eat dry toast to relieve my nausea.”
(d) "I take acetaminophen for arthritis pain.”
Answer:
(d) "I take acetaminophen for arthritis pain.”
Explanation:
Acetaminophen is toxic to the liver and should be avoided in a client with liver dysfunction. Increased periods of rest allow for liver regeneration. A low-fat, high-carbohydrate diet and dry toast to relieve nausea are appropriate.
Question 29.
A client plans to travel to a country where hepatitis B is common. What should the nurse advise the client about the most effective way to prevent the disease?
(a) Drink purified water.
(b) Avoid crowed, enclosed spaces.
(c) Complete the vaccination series.
(d) Observe safe sex practices.
Answer:
(c) Complete the vaccination series.
Explanation:
prevent infection. The client must complete the series of 3 or 4 injections over a period of time for the vaccine to be effective. Hepatitis B is considered a sexually transmitted disease, and the client also should observe safe sex practices, but being vaccinated is most effective. Poor sanitary conditions contribute to the spread of hepatitis A and E, but the client should also avoid drinking liquids that are not bottled. It is not necessary to avoid crowds or closed-in areas.
Question 30.
Which finding is normal for a client during the icteric phase of hepatitis A?
(a) tarry stools
(b) yellowed sclerae
(c) shortness of breath
(d) light, frothy urine
Answer:
(b) yellowed sclerae
Explanation:
Liver inflammation and obstruction block the normal flow of bile. Excess bilirubin turns the skin and sclerae yellow and the urine dark and frothy. Profound anorexia is also common. Tarry stools are indicative of gastrointestinal bleeding and would not be expected in hepatitis. Light- or clay-colored stools may occur in hepatitis owing to bile duct obstruction. Shortness of breath would be unexpected.
Question 31.
The nurse is teaching an adult recreational drug user about measures to avoid acquiring hepatitis A. What information should the nurse include in the instruction? Select all that apply.
(a) observing proper hand washing technique
(b) following safe syringe disposal procedures
(c) obtaining a vaccination
(d) wearing a mask when in crowds
(e) using caution with easting fresh fruits and vegetables
Answer:
(a) observing proper hand washing technique
(b) following safe syringe disposal procedures
(c) obtaining a vaccination
(e) using caution with easting fresh fruits and vegetables
Explanation:
(a), (b), (c), (e). The client is at risk for having hepatitis C because of recreational drug use. The main route of transmission for hepatitis A is the oral-fecal route; the disease can be prevented by good handwashing. The client should receive a vaccine for hepatitis A. The vaccine is administered in 2 doses 6 months apart. Percutaneous transmission is more common with hepatitis B, C, and D, but the client should follow safe needle and syringe precautions. Hepatitis A is not transmitted by droplet infection; the client does not need to wear a mask.
Question 32.
A client with chronic hepatitis C is experiencing nausea, anorexia, and fatigue. During the health history, the client states that he is homosexual, drinks one to two glasses of wine with dinner, is taking St. John’s wort for a “bit of depression,” and takes acetaminophen for frequent headaches. What should the nurse do? Select all that apply.
(a) Instruct the client that the wine with meals can be beneficial for cardiovascular health.
(b) Instruct the client to ask the health care provider (HCP) about taking any other medications as they may interact with medications the client is currently taking.
(c) Instruct the client to increase the protein in his diet and eat less frequently.
(d) Advise the client of the need for additional testing for HIV.
(e) Encourage the client to obtain sufficient rest.
Answer:
(b) Instruct the client to ask the health care provider (HCP) about taking any other medications as they may interact with medications the client is currently taking.
(d) Advise the client of the need for additional testing for HIV.
(e) Encourage the client to obtain sufficient rest.
Explanation:
(b), (d), (e). Clients with chronic hepatitis C should abstain from alcohol as it can speed cirrhosis and end-stage liver disease. Clients should also check with their HCPs Q before taking any nonprescription or prescription medications, or herbal supplements. It is also important that clients who are infected with HCV be tested for HIV, as clients who have both HIV and HCV have a more rapid progression of liver disease than do those who have HCV alone. Clients with HCV and nausea should be instructed to eat four to five times a day to help reduce anorexia and nausea. The client should obtain sufficient rest to manage the fatigue.
Question 33.
A client who is recovering from hepatitis A has fatigue and malaise. The client asks the nurse, “When will my strength return?” Which response by the nurse is most appropriate?
(a) “Your fatigue should be gone by now. We will evaluate you for a secondary infection.”
(b) “Your fatigue is an adverse effect of your drug therapy. It will disappear when your treatment regimen is complete.”
(c) “It is important for you to increase your activ ity level. That will help decrease your fatigue.”
(d) “It is normal for you to feel fatigued. The fatigue should go away in the next 2 to 4 months.”
Answer:
(d) “It is normal for you to feel fatigued. The fatigue should go away in the next 2 to 4 months.”
Explanation:
During the convalescent or posticteric stage of hepatitis, fatigue and malaise are the most common problems. These symptoms usually disappear within 2 to 4 months. Fatigue and malaise are not evidence of a secondary infection. Hepatitis A is not treated by drug therapy. It is important that the client continue to balance activity with periods of rest.
Question 34.
The nurse is caring for a client recently diagnosed with hepatitis C. In reviewing the client’s history, what information will be most helpful as the nurse develops a teaching plan? The client:
(a) has a history of exercise-induced asthma.
(b) is a scientist and is frequently exposed to multiple chemicals.
(c) traveled to Central America recently and ate uncooked vegetables.
(d) has a known history of sexually transmitted disease.
Answer:
(d) has a known history of sexually transmitted disease.
Explanation:
Although primarily bloodborne, unprotected sex with multiple partners and a history of sexually transmitted disease are risk factors for transmission of the hepatitis C virus. Other risk factors include blood transfusions, past treatment with chronic hemodialysis, being a child born to woman infected with hepatitis C virus, past/current illicit IV drug use, or needlestick injuries to health care workers. It is important for the nurse to be aware of the client’s history in order to help determine the client’s level of understanding of the disease, promote a healthy lifestyle, and discuss the role of viral transmission of the disease.
Question 35.
A client recently diagnosed with hepatitis C states: “Now that you know what’s wrong with me, you can just get me those new drugs to take care of it, right?” What should the nurse tell the client?
(a) “There are new antiviral drugs available that may make treatment more effective and help you tolerate it better.”
(b) “There are drugs to help with the symptoms, but once you have hepatitis C you will never be cured.”
(c) “The medicine currently used to treat hepa titis C is very expensive, and your insurance probably will not pay for it.”
(d) “If you continue to make the same lifestyle choices, the medicine will not make any difference.”
Answer:
(a) “There are new antiviral drugs available that may make treatment more effective and help you tolerate it better.”
Explanation:
The nurse should explain to the client that current therapy includes the use of antiviral agents which may be administered over a course of 8 to 12 weeks and usually cure the disease. Although the other answers choices may be true, it is not appropriate for the nurse to make judg-ments about a client’s health insurance or lifestyle choices.
Question 36.
The nurse is developing a teaching plan the client with viral hepatitis. What information should the nurse include in the plan?
(a) Obtain adequate bed rest.
(b) Increase fluid intake.
(c) Take antibiotic therapy as prescribed.
(d) Drink 8 oz (240 mL) of an electrolyte solution every day.
Answer:
(a) Obtain adequate bed rest.
Explanation:
Treatment of hepatitis consists primarily of bed rest with bathroom privileges. Bed rest is maintained during the acute phase to reduce metabolic demands on the liver, thus increasing its blood supply and promoting liver cell regeneration. When activity is gradually resumed, the client should be taught to rest before becoming overly tired. Although adequate fluid intake is important, it is not necessary to force fluids to treat hepatitis. Antibiotics are not used to treat hepatitis. Electrolyte imbalances are not typical of hepatitis.
Question 37.
When planning care for a client with hepatitis A, the nurse should review laboratory reports for which laboratory values?
(a) prolonged prothrombin time
(b) decreased blood glucose level
(c) elevated serum potassium level
(d) decreased serum calcium level
Answer:
(a) prolonged prothrombin time
Explanation:
The prothrombin time may be prolonged because of decreased absorption of vitamin K and decreased production of prothrombin by the liver. The client should be assessed carefully for bleeding tendencies. Blood glucose, serum potassium, and serum calcium levels are not affected by hepatitis.
Question 38.
The nurse is developing a teaching plan for the client with hepatitis A. What should the nurse tell the client to do?
(a) Limit caloric intake and reduce weight.
(b) Increase carbohydrates and protein in the diet.
(c) Avoid contact with others and sleep in a separate room.
(d) Intensify routine exercise and increase strength.
Answer:
(b) Increase carbohydrates and protein in the diet.
Explanation:
A low-fat, high-protein, high-carbohydrate diet is encouraged for a client with hepatitis to promote liver rejuvenation. Nutrition intake is important because clients may be anorexic and experience weight loss. Activity should be modified and adequate rest obtained to promote recovery. Social isolation should be avoided, and education on preventing transmission should be provided; the client does not need to sleep in a separate room.
Question 39.
The nurse develops a teaching plan for the client about how to prevent the transmission of hepatitis A. Which discharge instruction is appropriate for the client?
(a) Spray the house to eliminate infected insects.
(b) Tell family members to try to stay away from the client.
(c) Ask family members to wash their hands frequently.
(d) Disinfect all clothing and eating utensils.
Answer:
(c) Ask family members to wash their hands frequently.
Explanation:
The hepatitis A virus is transmitted via the fecal-oral route. It spreads through contaminated hands, water, and food, especially shellfish growing in contaminated water. Certain animal handlers are at risk for hepatitis A, particularly those handling primates. Frequent handwashing is probably the single most important preventive action. Insects do not transmit hepatitis A. Family members do not need to stay away from the client with hepatitis. It is not necessary to disinfect food and clothing.
Question 40.
The client with hepatitis A is experiencing fatigue, weakness, and a general feeling of malaise. The client tires rapidly during morning care. What is the most appropriate goal for this client?
(a) Increase mobility.
(b) Learn new self-care skills.
(c) Adapt to new levels of energy.
(d) Gradually increase activity tolerance.
Answer:
(d) Gradually increase activity tolerance.
Explanation:
The most appropriate goal for this client with hepatitis is to increase activity gradually as tolerated. Periods of alternating rest and activity should be included in the plan of care. There is no evidence that the client is physically immobile, is unable to provide self-care, or needs to adapt to new energy levels.
Question 41.
Interferon alfa-2b has been prescribed to treat a client with chronic hepatitis B. The nurse should assess the client for which common adverse effect?
(a) retinopathy
(b) constipation
(c) flulike symptoms
(d) hypoglycemia
Answer:
(c) flulike symptoms
Explanation:
Interferon alfa-2b most commonly causes flulike adverse effects, such as myalgia, arthralgia, headache, nausea, fever, and fatigue. Retinopathy is a potential adverse effect, but not a common one. Diarrhea may develop as an adverse effect. Clients are advised to administer the drug at bedtime and get adequate rest. Medications may be prescribed to treat the symptoms. The drug may also cause hematologic changes; therefore, laboratory tests such as a complete blood count and differential should be conducted monthly during drug therapy. Blood glucose laboratory values should be monitored for the development of hyperglycemia.
Question 42.
The nurse is preparing a community education program about preventing hepatitis B infection. Which information should be incorporated into the teaching plan?
(a) Hepatitis B is relatively uncommon among college students.
(b) Frequent ingestion of alcohol can predispose an individual to development of hepatitis B.
(c) Good personal hygiene habits are most effective at preventing the spread of hepatitis B.
(d) The use of a condom is advised for sexualintercourse.
Answer:
(d) The use of a condom is advised for sexualintercourse.
Explanation:
Hepatitis B is spread through exposure to blood or blood products and through high-risk sexual activity. Hepatitis B is considered to be a sexually transmitted disease. High-risk sexual activities include sex with multiple partners, unprotected sex with an infected individual, male homosexual activity, and sexual activity with IV drug users. College students are at high risk for development of hepatitis B and are encouraged to be immunized. Alcohol intake by itself does not predispose an individual to hepatitis B, but it can lead to high-risk behaviors such as unprotected sex. Good personal hygiene alone will not prevent the transmission of hepatitis B.
Question 43.
The nurse is establishing goals for the client with hepatitis A? Which goal is appropriate?
The client will:
(a) demonstrate a decrease in fluid retention related to ascites.
(b) verbalize the importance of reporting bleeding gums or bloody stools.
(c) limit use of alcohol to two to three drinks per week.
(d) restrict activity to within the home to prevent disease transmission.
Answer:
(b) verbalize the importance of reporting bleeding gums or bloody stools.
Explanation:
The client should be able to verbalize the importance of reporting any bleeding tendencies that could be the result of a prolonged prothrombin time. Ascites is not typically a clinical manifestation of hepatitis; it is associated with cirrhosis. Alcohol use should be eliminated for at least 1 year after the diagnosis of hepatitis to allow the liver time to fully recover. There is no need for a client to be restricted to the home because hepatitis is not spread through casual contact between individuals.
Question 44.
A client had a liver biopsy 1 hour ago. What should the nurse do first?
(a) Auscultate lung sounds.
(b) Check for fever.
(c) Obtain a CBC.
(d) Apply packing to the biopsy site.
Answer:
(a) Auscultate lung sounds.
Explanation:
immediately after the procedure, the nurse should determine diminished or absent lung sounds in the right lung. Although fever indicates infection, a rise in temperature is not seen immediately. A CBC is warranted if the vital signs and client symptoms indicate potential hemorrhage. The needle insertion site is covered with a pressure dressing; there is no need for a dressing requiring packing.
Question 45.
The nurse is assessing a client for ascites. Where does the nurse place the hands to percuss for the presence of fluid?
Answer:
The nurse places the client in supine position and percusses each flank for shifting dullness. If fluid is present, dullness is noted.
Question 46.
A client with cirrhosis is receiving lactulose. The nurse notes the client is more confused and has asterixis. What should the nurse do next?
(a) Assess for gastrointestinal (GI) bleeding.
(b) Withhold the lactulose.
(c) Increase protein in the diet.
(d) Monitor serum bilirubin levels.
Answer:
(a) Assess for gastrointestinal (GI) bleeding.
Explanation:
Clients with cirrhosis can develop hepatic encephalopathy caused by increased ammonia levels. Asterixis, a flapping tremor, is a characteristic symptom of increased ammonia levels. Bacterial action on increased protein in the bowel will increase ammonia levels and cause the encephalopathy to worsen. GI bleeding and protein consumed in the diet increase protein in the intestine and can elevate ammonia levels. Lactulose is given to reduce ammonia formation in the intestine and should not be held since neurological symptoms are worsening. Bilirubin is associated with jaundice.
Question 47.
The nurse is assessing a client with cirrhosis who has developed hepatic encephalopathy. The nurse should notify the health care provider of a decrease in which serum lab value that is a potential precipitating factor for hepatic encephalopathy?
(a) aldosterone
(b) creatinine
(c) potassium
(d) protein
Answer:
(c) potassium
Explanation:
Hypokalemia is a precipitating factor in hepatic encephalopathy. A decrease in creatinine results from muscle atrophy; an increase in creatinine would indicate renal insufficiency. With liver dysfunction, increased aldosterone levels are seen. A decrease in serum protein will decrease colloid osmotic pressure and promote edema.
Question 48.
A client has advanced cirrhosis of the liver. The client’s spouse asks the nurse why his abdomen is swollen, making it very difficult for him to fasten his pants. How should the nurse respond to provide the most accurate explanation of the disease process?
(a) “He must have been eating too many foods with salt in them. Salt pulls water with it.”
(b) “The swelling in his ankles must have moved up closer to his heart so the fluid circulates better.”
(c) “He must have forgotten to take his daily water pill.”
(d) “Blood is not able to flow readily through the liver now, and the liver cannot make protein to keep fluid inside the blood vessels.”
Answer:
(d) “Blood is not able to flow readily through the liver now, and the liver cannot make protein to keep fluid inside the blood vessels.”
Explanation:
Portal hypertension and hypoalbumin- emia as a result of cirrhosis cause a fluid shift into the peritoneal space causing ascites. In a cardiac or kidney problem, not cirrhosis, sodium can promote edema formation and subsequent decreased urine output. Edema does not migrate upward toward the heart to enhance its circulation. Although diuretics promote the excretion of excess fluid, occasionally forgetting or omitting a dose will not yield the ascites found in cirrhosis of the liver.
Question 49.
A nurse is developing a care plan for a client with hepatic encephalopathy. Which are goals for the care for this client? Select all that apply.
(a) Prevent constipation.
(b) Administer lactulose to reduce blood ammonia levels.
(c) Monitor coordination while walking.
(d) Check the pupil reaction.
(e) Provide food and fluids high in carbohydrate.
(f) Encourage physical activity.
Answer:
(a) Prevent constipation.
(b) Administer lactulose to reduce blood ammonia levels.
(c) Monitor coordination while walking.
(d) Check the pupil reaction.
(e) Provide food and fluids high in carbohydrate.
Explanation:
(a), (b), (c), (d), (e). Constipation leads to increased ammonia production. Lactulose is a hyperosmotic laxative that reduces blood ammonia by acidifying the colon contents, which retards diffusion of nonionic ammonia from the colon to the blood while promoting its migration from the blood to the colon. Hepatic encephalopathy is considered a toxic or metabolic condition that causes cerebral edema; it affects a person’s coordination and pupil reaction to light and accommodation. Food and fluids high in carbohydrates should be given because the liver is not synthesizing and storing glucose. Because exercise produces ammonia as a by-product of metabolism, physical activity should be limited, not encouraged.
Question 50.
The nurse is assessing a client who is in the early stages of cirrhosis of the liver. Which focused assessment is appropriate?
(a) peripheral edema
(b) ascites
(c) anorexia
(d) jaundice
Answer:
(c) anorexia
Explanation:
Early clinical manifestations of cirrhosis are subtle and usually include gastrointestinal symptoms, such as anorexia, nausea, vomiting, and changes in bowel patterns. These changes are caused by the liver’s altered ability to metabolize carbohydrates, proteins, and fats. Peripheral edema, ascites, and jaundice are later signs of liver failure and portal hypertension.
Question 51.
A client with cirrhosis begins to develop ascites. Spironolactone is prescribed to treat the ascites. The nurse should monitor the client closely for which drug-related adverse effect?
(a) constipation
(b) hyperkalemia
(c) irregular pulse
(d) dysuria
Answer:
(b) hyperkalemia
Explanation:
Spironolactone is a potassium-sparing diuretic; therefore, clients should be monitored closely for hyperkalemia. Other common adverse effects include abdominal cramping, diarrhea, dizziness, headache, and rash. Constipation and dysuria are not common adverse effects of spironolactone. An irregular pulse is not an adverse effect of spironolactone but could develop if serum potassium levels are not closely monitored.
Question 52.
What diet should be implemented for a client who is in the early stages of cirrhosis?
(a) high-calorie, high-carbohydrate
(b) high-protein, low-fat
(c) low-fat, low-protein
(d) high-carbohydrate, low-sodium
Answer:
(a) high-calorie, high-carbohydrate
Explanation:
For clients who have cirrhosis without complications, a high-calorie, high-carbohydrate diet is preferred to provide an adequate supply of nutrients. In the early stages of cirrhosis, there is no need to restrict fat, protein, or sodium.
Question 53.
A client with jaundice has pruritus and areas of irritation from scratching. What measures can the nurse suggest the client use to prevent skin breakdown? Select all that apply.
(a) Avoid lotions containing calamine.
(b) Add baking soda to the water in a tub bath.
(c) Keep nails short and clean.
(d) Rub the skin when it itches with knuckles instead of nails.
(e) Massage skin with alcohol.
(f) Increase sodium intake in diet.
Answer:
(b) Add baking soda to the water in a tub bath.
(c) Keep nails short and clean.
(d) Rub the skin when it itches with knuckles instead of nails.
Explanation:
(b), (c), (d). Baking soda baths can decrease pruritus. Keeping nails short and rubbing the area with knuckles can decrease breakdown when scratching. Calamine lotions help relieve itching. Alcohol will increase skin dryness. Sodium in the diet will increase edema and weaken skin integrity
Question 54.
Which health promotion activity should the nurse suggest that the client with cirrhosis add to the daily routine at home?
(a) Supplement the diet with daily multivitamins.
(b) Abstain from drinking alcohol.
(c) Take a sleeping pill at bedtime.
(d) Limit contact with other people whenever possible.
Answer:
(b) Abstain from drinking alcohol.
Explanation:
General health promotion measures include maintaining good nutrition, avoiding infection, and abstaining from alcohol. It is not necessary to take multivitamins if the client is obtaining adequate nutrition. Rest and sleep are essential, but an impaired liver may not be able to detoxify sedatives and barbiturates. Such drugs must be used cautiously, if at all, by clients with cirrhosis. The client does not need to limit contact with others but should exercise caution to stay away from ill people.
Question 55.
The nurse is reviewing the chart information for a client with increased ascites. The data include the following: temperature 98.9°F (37.2°C), heart rate 118 bpm, shallow respirations 26 breaths/min, blood pressure 128/76 mm Hg, and SpO2 89% on room air. What should the nurse do first?
(a) Assess heart sounds.
(b) Obtain a prescription for blood cultures.
(c) Prepare for a paracentesis.
(d) Raise the head of the bed.
Answer:
(d) Raise the head of the bed.
Explanation:
Elevating the head of the bed will allow for increased lung expansion by decreasing the ascites pressing on the diaphragm. The client requires reassessment. A paracentesis is reserved for symptomatic clients with ascites with impaired respiration or abdominal pain not responding to other measures such as sodium restriction and diuretics. There is no indication for blood cultures. Heart sounds are assessed with the routine physical assessment.
Question 56.
Which position would be appropriate for a client with severe ascites?
(a) Fowler’s
(b) side-lying
(c) reverse Trendelenburg
(d) Sims’
Answer:
(a) Fowler’s
Explanation:
Ascites can compromise the action of the diaphragm and increase the client’s risk of respiratory problems. Ascites also greatly increases the risk of skin breakdown. Frequent position changes are important, but the preferred position is Fowler’s. Placing the client in Fowler’s position helps facilitate the client’s breathing by relieving pressure on the diaphragm. The other positions do not relieve pressure on the diaphragm.
Question 57.
The nurse is caring for a client with esophageal varices. The nurse should discuss which laboratory report finding with the health care provider (HCP)?
(a) normal serum albumin
(b) decreased ammonia
(c) slightly decreased levels of calcium
(d) elevated PT/INR
Answer:
(d) elevated PT/INR
Explanation:
The client with esophageal varices is at even higher risk for bleeding with elevated PT/INR. The nurse and HCP collaborate to prevent bleeding. The other laboratory findings are not as life threatening. A decreased serum albumin can cause fluid to move into the interstitial tissues. Increased ammonia levels are toxic to the brain. Calcium loss is more common to pancreatitis.
Question 58.
A client with cirrhosis who has ascites receives 100 mL of 25% serum albumin IV. Which finding would best indicate that the albumin is having its desired effect?
(a) reduced ascites
(b) increased serum albumin level
(c) decreased anorexia
(d) increased ease of breathing
Answer:
(a) reduced ascites
Explanation:
Normal serum albumin is administered to reduce ascites. Hypoalbuminemia, a mechanism underlying ascites formation, results in decreased colloid osmotic pressure. Administering serum albumin increases the plasma colloid osmotic pressure, which causes fluid to flow from the tissue space into the plasma. Increased urine output is the best indication that the albumin is having the desired effect. An increased serum albumin level and increased ease of breathing may indirectly imply that the administration of albumin is effective in relieving the ascites. However, it is not as direct an indicator as increased urine output and reduced ascites. Anorexia is not affected by the administration of albumin.
Question 59.
A client with a Sengstaken-Blakemore tube has a sudden drop in SpO2 and an increase in respiratory rate to 40 breaths/min. What should the nurse do in order from first to last? All options must be used.
(a) Affirm airway obstruction by the tube.
(b) Remove the tube.
(c) Deflate the tube by cutting with bedside scissors.
(d) Apply oxygen via face mask.
Answer:
(a) Affirm airway obstruction by the tube.
(c) Deflate the tube by cutting with bedside scissors.
(b) Remove the tube.
(d) Apply oxygen via face mask.
Explanation:
(a), (c), (b), (d). The nurse should first assess the client to determine if the tube is obstructing the airway; assessment is done by assessing airflow. Once obstruction is established, the tube should be deflated and then quickly removed. A set of scissors should always be at the bedside to allow for emergency deflation of the balloon. Oxygen via face mask should then be applied once the tube is removed.
Question 60.
The health care provider instructs a client with alcohol-induced cirrhosis to stop drinking alcohol. The nurse should assess the client for which expected outcome?
(a) absence of delirium tremens
(b) having a balanced diet
(c) improved liver function
(d) reduced weight
Answer:
(c) improved liver function
Explanation:
The goal of abstinence from alcohol in clients with alcohol-induced cirrhosis is to improve the liver function; most clients have improved liver function when they abstain from alcohol. Clients with cirrhosis do not necessarily have delirium tremens. Abstaining from alcohol may allow the client to improve nutritional status, but additional dietary counseling may be needed to achieve that goal. Clients with cirrhosis may have weight gain from ascites, but this is managed with diuretics.
Question 61.
The nurse monitors a client with cirrhosis for the development of hepatic encephalopathy. Which would be an indication that hepatic encephalopathy is developing?
(a) decreased mental status
(b) elevated blood pressure
(c) decreased urine output
(d) labored respirations
Answer:
(a) decreased mental status
Explanation:
The client should be monitored closely for changes in mental status. Ammonia has a toxic effect on central nervous system tissue and produces an altered level of consciousness, marked by drowsiness and irritability. If this process is unchecked, the client may lapse into coma. Increasing ammonia levels are not detected by changes in blood pressure, urine output, or respirations.
Question 62.
A client’s serum ammonia level is elevated, and the health care provider prescribes 30 mL of lactulose. Which effect is common for this drug?
(a) increased urine output
(b) improved level of consciousness
(c) increased bowel movements
(d) nausea and vomiting
Answer:
(c) increased bowel movements
Explanation:
Lactulose increases intestinal motility, thereby trapping and expelling ammonia in the feces. An increase in the number of bowel movements is expected as an adverse effect. Lactulose does not affect urine output. Any improvements in mental status would be the result of increased ammonia elimination, not an adverse effect of the drug. Nausea and vomiting are not common adverse effects of lactulose.
Question 63.
A client is to be discharged with a prescription for lactulose. The nurse teaches the client how to administer this medication. Which statement would indicate that the client has understood the information?
(a) “I will take it with an antacid.”
(b) “I will mix it with apple juice.”
(c) “I will take it with a laxative.”
(d) “I will mix the crushed tablets in some gelatin.”
Answer:
(b) “I will mix it with apple juice.”
Explanation:
The taste of lactulose is a problem for some clients. Mixing it with fruit juice, water, or milk can make it more palatable. Lactulose should not be given with antacids, which may inhibit its action. Lactulose should not be taken with a laxative because increased stooling is an adverse effect of the drug and would be potentiated by using a laxative. Lactulose comes in the form of syrup for oral or rectal administration.
Question 64.
The nurse is providing discharge instructions for a client with cirrhosis. Which statement best indicates that the client has understood the teaching?
(a) “I should eat a high-protein, high-carbohy drate diet to provide energy.”
(b) “It is safer for me to take acetaminophen for pain instead of aspirin.”
(c) “I should avoid constipation to decrease chances of bleeding.”
(d) “If I get enough rest and follow my diet, it’s possible for my cirrhosis to be cured.”
Answer:
(c) “I should avoid constipation to decrease chances of bleeding.”
Explanation:
Clients with cirrhosis should be instructed to avoid constipation and straining at stool to prevent hemorrhage. The client with cirrhosis has bleeding tendencies because of the liver’s inability to produce clotting factors. A low-protein and high-carbohydrate diet is recommended. Clients with cirrhosis should not take acetaminophen, which is potentially hepatotoxic. Aspirin also should be avoided if esophageal varices are present. Cirrhosis is a chronic disease.
Question 65.
The nurse is preparing a client for a paracentesis. What should the nurse do?
(a) Have the client void immediately before the procedure.
(b) Place the client in a side-lying position.
(c) Initiate an IV line to administer sedatives.
(d) Place the client on nothing-by-mouth (NPO) status 6 hours before the procedure.
Answer:
(a) Have the client void immediately before the procedure.
Explanation:
Immediately before a paracentesis, the client should empty the bladder to prevent perforation. The client will be placed in a high Fowler’s position or seated on the side of the bed for the procedure. IV sedatives are not usually administered. The client does not need to be NPO.
Question 66.
A client with ascites and peripheral edema is at risk for impaired skin integrity. To prevent skin breakdown, what should the nurse do?
(a) Institute range-of-motion (ROM) exercise every 4 hours.
(b) Massage the abdomen once a shift.
(c) Use an alternating air pressure mattress.
(d) Elevate the lower extremities.
Answer:
(c) Use an alternating air pressure mattress.
Explanation:
Edematous tissue is easily traumatized and must receive meticulous care. An alternating air pressure mattress will help decrease pressure on the edematous tissue. ROM exercises are important to maintain joint function, but they do not necessarily prevent skin breakdown. When abdominal skin is stretched taut due to ascites, it must be cleaned very carefully. The abdomen should not be massaged. Elevation of the lower extremities promotes venous return and decreases swelling.
Question 67.
Which precautions should the health care team observe when caring for clients with hepatitis A?
(a) gowning when entering a client’s room
(b) wearing a mask when providing care
(c) assigning the client to a private room
(d) wearing gloves when giving direct care
Answer:
(d) wearing gloves when giving direct care
Explanation:
Contact precautions are recommended for clients with hepatitis A. This includes wearing gloves for direct care. A gown is not required unless substantial contact with the client is anticipated. It is not necessary to wear a mask. The client does not need a private room unless incontinent of stool.
Question 68.
After completing assessment rounds, which client should the nurse discuss with the health care provider (HCP) first?
(a) a client with cirrhosis who is depressed and has refused to eat for the past 2 days
(b) a client with stable vital signs that has been receiving IV ciprofloxacin following a cho-lecystectomy for 1 day and has developed a rash on the chest and arms
(c) a client with pancreatitis whose family requests to speak with the HCP regarding the treatment plan
(d) a client with hepatitis whose pulse was 84 bpm and regular and is now 118 bpm and irregular
Answer:
(d) a client with hepatitis whose pulse was 84 bpm and regular and is now 118 bpm and irregular
Explanation:
A change in a client’s baseline vital signs should be brought to the HCP’s attention immediately. In this case, the client’s heart rate has increased, and the rhythm appears to have changed; the HCP may prescribe an ECG to determine if treatment is necessary. The nurse should also have a complete set of current vital signs as well as a physical assessment before providing the HCP information using the SBAR format.
The nutritional as well as psychological needs of a client must be addressed but are not first priority. A rash that develops after a new antibiotic is started must be brought to the HCP attention; however, this client is stable and is not the first priority. The nurse is responsible to facilitate discussion between the client, the client’s family, and the HCP, but only after all of the immediate physical and psychological needs of all clients have been met.
Question 69.
The nurse’s assignment consists of four clients. From highest to lowest priority, in which order should the nurse assess the clients after receiving the morning report? All options must be used.
(a) the client with cirrhosis who became confused and disoriented during the night
(b) the client who is 1 day postoperative following a cholecystectomy and has a T tube inserted
(c) the client with acute pancreatitis who is requesting pain medication
(d) the client with hepatitis B who has questions about discharge instructions
Answer:
(a) the client with cirrhosis who became confused and disoriented during the night
(c) the client with acute pancreatitis who is requesting pain medication
(b) the client who is 1 day postoperative following a cholecystectomy and has a T tube inserted
(d) the client with hepatitis B who has questions about discharge instructions
Explanation:
(a), (c), (b), (d)The nurse should first assess the client with cirrhosis to ensure the client’s safety and assess the client for the onset of hepatic encephalopathy. The nurse should then assess the client with acute pancreatitis who is requesting pain medication and administer the needed medication. The nurse should next assess the client who underwent a cholecystectomy and is 1 day postoperative to make sure that the T tube is draining and that the client is performing postoperative breathing exercises. This client’s safety is not at risk, and the client is not reporting having pain. The nurse can speak last with the client with hepatitis B who has questions about discharge instructions because this client’s issues are not urgent.
Question 70.
The nurse should institute which measure to prevent transmission of the hepatitis C virus to health care personnel?
(a) administering hepatitis C vaccine to all health care personnel
(b) decreasing contact with blood and blood- contaminated fluids
(c) wearing gloves when emptying the bed pan
(d) wearing a gown and mask when providing direct care
Answer:
(b) decreasing contact with blood and blood-contaminated fluids
Explanation:
Hepatitis C is usually transmitted through blood exposure or needlesticks. A hepatitis C vaccine is currently under development, but it is not available for use. The first line of defense against hepatitis B is the hepatitis B vaccine. Hepatitis C is not transmitted through feces or urine. Wearing a gown and mask will not prevent transmission of the hepatitis C virus if the caregiver comes in contact with infected blood or needles.
Question 71.
The nurse is taking care of a client who has an IV infusion pump. The pump alarm rings. What should the nurse do in order from first to last? All options must be used.
(a) Silence the pump alarm.
(b) Determine if the infusion pump is plugged into an electrical outlet.
(c) Assess the client’s access site for infiltration or inflammation.
(d) Assess the tubing for hindrances to flow of solution.
Answer:
(a) Silence the pump alarm.
(c) Assess the client’s access site for infiltration or inflammation.
(d) Assess the tubing for hindrances to flow of solution.
(b) Determine if the infusion pump is plugged into an electrical outlet.
Explanation:
(a), (c), (d), (b). Silencing the alarm will eliminate a stress to the client and allow the nurse to focus on the task at hand. The nurse should then assess the access site to note if the needle is inserted in the vein or if there is tissue trauma, infiltration, or inflammation. Next, the nurse should check for kinks in the tubing. Finally, the nurse can plug the pump into the wall to allow the battery to become recharged.
Read More:
Urinary Tract Health Problems
Why You Should Be Eating Avocado During Pregnancy