NCLEX RN Practice Questions provide a simulated testing environment that helps students become familiar with the format and style of the actual exam.
NCLEX Antepartum Care Questions - NCLEX Questions on Antepartum Care
Antepartum Care NCLEX Practice Questions
Question 1.
A client has obtained levonorgestrel as emergency contraception. After unprotected intercourse, the client calls the clinic to ask questions about taking the contraceptives. The nurse realizes the client needs a further explanation when she makes which statement?
(a) “I can wait up to 4 days after intercourse to start taking these to prevent pregnancy.”
(b) “My boyfriend can buy levonorgestrel from the pharmacy if he is over 18 years old.”
(c) “The birth control works by preventing ovulation or fertilization of the egg.”
(d) “I may feel nauseated and have breast tenderness or a headache after using the contraceptive.”
Answer:
(a) “I can wait up to 4 days after intercourse to start taking these to prevent pregnancy.”
Explanation:
Levonorgestrel can reduce the chance of pregnancy if taken within 72 hours of unprotected intercourse, and then again 12 hours later. Waiting 4 days to take levonorgestrel reduces effectiveness. Males can purchase this contraceptive as long as they are over 18 years of age. Levonorgestrel works by preventing ovulation or fertilization depending on where a client is in the menstrual cycle. Common side effects include nausea, breast tenderness, vertigo, and stomach pain.
Question 2.
An antenatal G2, Tl, PO, AO, Ll client is discussing her postpartum plans for birth control with her health care provider (HCP). In analyzing the available choices, which factor has the greatest impact on her birth control options?
(a) satisfaction with prior methods
(b) preference of sexual partner
(c) breast- or bottle-feeding plan
(d) desire for another child in 2 years
Answer:
(c) breast- or bottle-feeding plan
Explanation:
Birth control plans are influenced primarily by whether the mother is breast- or bottle-feeding her infant. The maternal milk supply must be well established prior to the initiation of most hormonal birth control methods. Low-dose oral contraceptives would be the exception. Use of estrogen-/proges- throne-based pills and progesterone-only pills are commonly initiated from 4 to 6 weeks postpartum because the milk supply is well established by this time.
Prior experiences with birth control methods have an impact on the method chosen as do the preferences of the client’s partner; however, they are not the most influential factors. Desire to have another child in 2 years would make some methods, such as an IUD, less attractive but would still be secondary to the choice to breastfeed.
Question 3.
Which information would be important to include in the teaching plan for the client who wants more information on ovulation and fertility management?
(a) The ovum survives for 96 hours after ovulation, making conception possible during this time.
(b) The basal body temperature falls at least 0.2°F (0.17°C) after ovulation has occurred.
(c) Ovulation usually occurs on day 14, plus or minus 2 days, before the onset of the next menstrual cycle.
(d) Most women can tell they have ovulated because of severe pain and thick, scant cervical mucus.
Answer:
(c) Ovulation usually occurs on day 14, plus or minus 2 days, before the onset of the next menstrual cycle.
Explanation:
For a client with a typical menstrual cycle of 28 days, ovulation usually occurs on day 14, plus or minus 2 days, before the onset of the next menstrual cycle. Stated another way, the menstrual period begins about 2 weeks after ovulation has occurred. Ovulation does not usually occur during the menses component of the cycle when the uterine lining is being shed.
In most women, the ovum sur-vives for about 12 to 24 hours after ovulation, during which time conception is possible. The basal body temperature rises 0.5°F to 1.0°F (0.28°C to 0.56°C) when ovulation occurs. Although some women experience some pelvic discomfort during ovulation (mittelschmerz), severe or unusual pain is rare. After ovulation, the cervical mucus is thin and copious.
Question 4.
Which instructions about activities during menstruation would the nurse include when counseling an adolescent who has just begun to menstruate?
(a) Take a mild analgesic if needed for menstrual pain.
(b) Avoid cold foods if menstrual pain persists.
(c) Stop exercise while menstruating.
(d) Avoid tampons until you have had your periods for 1 year.
Answer:
(a) Take a mild analgesic if needed for menstrual pain.
Explanation:
The nurse should instruct the client to take a mild analgesic, such as ibuprofen, if menstrual pain or “cramps” are present. The client should also eat foods rich in iron and should continue moderate exercise during menstruation, which increases abdominal tone. Avoiding cold foods will not decrease dysmenorrhea. Use of pads or tampons is
a personal choice. There is no evidence that it is necessary to wait to use tampons.
Question 5.
After conducting a class for female adolescents about human reproduction, the nurse concludes teaching has been effective when a student makes which statement?
(a) “Under ideal conditions, sperm can reach the ovum in 15 to 30 minutes, resulting in pregnancy.”
(b) “I will not become pregnant if I abstain from intercourse during the last 14 days of my menstrual cycle.”
(c) “Sperms from a healthy male usually remain viable in the female reproductive tract for 96 hours.”
(d) “After an ovum is fertilized by a sperm, the ovum contains 21 pairs of chromosomes.”
Answer:
(a) “Under ideal conditions, sperm can reach the ovum in 15 to 30 minutes, resulting in pregnancy.”
Explanation:
Under ideal conditions, sperm can reach the ovum in 15 to 30 minutes. This is an important point to make with adolescents who may be sexually active. Many people believe that the time interval is much longer and that they can wait until after intercourse to take steps to prevent conception. Without protection, pregnancy and sexually transmitted diseases can occur. When using the abstinence or calendar method, the couple should abstain from intercourse on the days of the menstrual cycle when the woman is most likely to conceive.
Using a 28-day cycle as an example, a couple should abstain from coitus 3 to 4 days before ovulation (days 10 through 14) and 3 to 4 days after ovulation (days 15 through 18). Sperm from a healthy male can remain viable for 24 to 72 hours in the female reproductive tract. If the female client ovulates after coitus, there is a possibility that fertilization can occur. Before fertilization, the ovum and sperm each contain 23 chromosomes. After fertilization, the conceptus contains 46 chromosomes unless there is a chromosomal abnormality.
Question 6.
A 20-year-old nulligravid client expresses a desire to learn more about the symptothermal method of family planning. Which information would the nurse include in the teaching plan?
(a) This method has a 50% failure rate during the first year of use.
(b) Couples must abstain from coitus for 5 days after the menses.
(c) Cervical mucus is carefully monitored for changes.
(d) The male partner uses condoms for significant effectiveness.
Answer:
(c) Cervical mucus is carefully monitored for changes.
Explanation:
The symptothermal method is a natural method of fertility management that depends on knowing when ovulation has occurred. Because regular menstrual cycles can vary by 1 to 2 days in either direction, the symptothermal method requires daily basal body temperature assessments plus close monitoring of cervical mucus changes. The method relies on abstinence during the period of ovulation, which occurs approximately 14 days before the beginning of the next cycle.
Abstinence horn coitus for 5 days after menses is unnecessary because it is unlikely that ovulation will occur during this time period (days 1 through 10). Typically, the failure rate for this method is between 10% and 20%. Although a condom may increase the effectiveness of this method, most clients who choose natural methods are not interested in chemical or barrier types of family planning.
Question 7.
Before advising a 24-year-old client desiring oral contraceptives for family planning, the nurse would assess the client for which signs and symptoms?
(a) anemia
(b) hypertension
(c) dysmenorrhea
(d) acne vulgaris
Answer:
(b) hypertension
Explanation:
Before advising a client about oral contraceptives, the nurse needs to assess the client for signs and symptoms of hypertension. Clients who have hypertension, thrombophlebitis, obesity, or a family history of cerebral or cardiovascular accident are poor candidates for oral contraceptives. In addition, women who smoke, are older than 40 years of age, or have a history of pulmonary disease should be advised to use a different method. Iron deficiency anemia, dysmenorrhea, and acne are not contraindications for the use of oral contraceptives. Iron deficiency anemia is a common disorder in young women.
Oral contraceptives decrease the amount of menstrual flow and thus decrease the amount of iron lost through menses, thereby providing a beneficial effect when used by clients with anemia. Low-dose oral contraceptives to prevent ovulation may be effective in decreasing the severity of dysmenorrhea (painful menstruation). Dysmenorrhea is thought to be caused by the release of prostaglandins in response to tissue destruction during the ischemic phase of the menstrual cycle. Use of oral contraceptives commonly improves facial acne.
Question 8.
After instructing a 20-year-old nulligravid client about adverse effects of oral contraceptives, the nurse determines that further instruction is needed when the client states which as an adverse effect?
(a) weight gain
(b) nausea
(c) headache
(d) ovarian cancer
Answer:
(d) ovarian cancer
Explanation:
The nurse determines that the client needs further instruction when the client says that one of the adverse effects of oral contraceptive use is ovarian cancer. Some studies suggest that ovarian and endometrial cancers are reduced in women using oral contraceptives. Other adverse effects of oral contraceptives include weight gain, nausea, headache, breakthrough bleeding, and monilial infections. The most serious adverse effect is thrombophlebitis.
Question 9.
Which information would the nurse include in the teaching plan for a 32-year-old female client requesting information about using a diaphragm for family planning?
(a) Douching with an acidic solution after inter course is recommended.
(b) Diaphragms should not be used if the client develops acute cervicitis.
(c) The diaphragm should be washed in a weak solution of bleach and water.
(d) The diaphragm should be left in place for 2 hours after intercourse.
Answer:
(b) Diaphragms should not be used if the client develops acute cervicitis.
Explanation:
The teaching plan should include a caution that a diaphragm should not be used if the client develops acute cervicitis, possibly aggravated by contact with the rubber of the diaphragm. Some studies have also associated diaphragm use with increased incidence of urinary tract infections. Douching after use of a diaphragm and intercourse is not recommended because pregnancy could occur. The diaphragm should be inspected and washed with mild soap and water after each use.
A diaphragm should be left in place for at least 6 hours but no longer than 24 hours after intercourse. More spermicidal jelly or cream should be used if intercourse is repeated during this period.
Question 10.
After being examined and fitted for a diaphragm, a 24-year-old client receives instructions about its use. Which client statement indicates a need for further teaching?
(a) “I can continue to use the diaphragm for about 2 to 3 years if I keep it protected in the case.”
(b) “If I get pregnant, I will have to be refitted for another diaphragm after birth.”
(c) “Before inserting the diaphragm, I should coat the rim with contraceptive jelly.”
(d) “If I gain or lose 20 lb (9 kg), I can still use the same diaphragm.”
Answer:
(d) “If I gain or lose 20 lb (9 kg), I can still use the same diaphragm.”
Explanation:
The client would need additional instruc¬tions when she says that she can still use the same diaphragm if she gains or loses 20 lb (9 kg). Gaining or losing more than 15 lb (6.8 kg) can change the pelvic and vaginal contours to such a degree that the diaphragm will no longer protect the client against pregnancy. The diaphragm can be used for 2 to 3 years if it is cared for and well protected in its case. The client should be refitted for another diaphragm
Question 11.
A couple is inquiring about vasectomy as a permanent method of contraception. Which teaching statement would the nurse include in the teaching plan?
(a) “Another method of contraception is needed until the sperm count is 0.”
(b) “Vasectomy is easily reversed if children are desired in the future.”
(c) “Vasectomy is contraindicated in males with a prior history of cardiac disease.”
(d) “Vasectomy requires only a yearly follow-up once the procedure is completed.”
Answer:
(a) “Another method of contraception is needed until the sperm count is 0.”
Explanation:
Another method of contraception is needed until all sperm has been cleared from the body. The number of ejaculates for this to occur varies with the individual, and laboratory analysis is required to determine when that has been accomplished. Vasectomy is considered a permanent sterilization procedure and requires microsurgery for anastomosis of the vas deferens to be completed. Studies have shown that there is no connection between cardiac disease in males and vasectomy. There is no need for follow-up after verification that there is no sperm in the system.
Question 12.
A 39-year-old multigravid client asks the nurse for information about female sterilization with a tubal ligation. Which client statement indicates effective teaching?
(a) “My fallopian tubes will be tied off through a small abdominal incision.”
(b) “Reversal of a tubal ligation is easily done, with a pregnancy success rate of 80%.”
(c) “After this procedure, I must abstain from intercourse for at least 3 weeks.”
(d) “Both of my ovaries will be removed during the tubal ligation procedure.”
Answer:
(a) “My fallopian tubes will be tied off through a small abdominal incision.”
Explanation:
Tubal ligation, a female sterilization pro¬cedure, involves ligation (tying off) or cauterization of the fallopian tubes through a small abdominal incision (laparotomy). Reversal of a tubal ligation is not easily done, and the pregnancy success rate after reversal is about 30%. After a tubal ligation, the client may engage in intercourse 2 to 3 days after the procedure. The ovaries are not generally removed during a tubal ligation. An oophorectomy involves removal of one or both ovaries.
Question 13.
A 23-year-old nulliparous client visiting the clinic for a routine examination tells the nurse that she desires to use the basal body temperature method for family planning. What instructions should the nurse give the client?
(a) Check the cervical mucus to see if it is thick and sparse.
(b) Take her temperature at the same time every morning before getting out of bed.
(c) Document ovulation when her temperature decreases at least 1°F (0.56°C).
(d) Avoid coitus for 10 days after a slight rise in temperature.
Answer:
(b) Take her temperature at the same time every morning before getting out of bed.
Explanation:
The basal body temperature method requires that the client take her temperature each morning before getting out of bed, preferably at the same time each day before eating or any other activity. Just before the day of ovulation, the temperature falls by 0.5°F (0.28°C). At the time of ovulation, the temperature rises 0.4°F to 0.8°F (0.22°C to 0.44°C) because of increased progesterone secretion in response to the luteinizing hormone. The temperature remains higher for the rest of the menstrual cycle. The client should keep a diary of about 6 months of menstrual cycles to calculate “safe” days. There is no mucus for the first 3 or 4 days after menses, and then thick, sticky mucus begins to appear.
As estrogen increases, the mucus changes to clear, slippery, and stretchy. This condition, termed spinn- barkeit, is present during ovulation. After ovulation, the mucus decreases in amount and becomes thick and sticky again until menses. Because the ovum typically survives about 24 hours and sperm can survive up to 72 hours, couples must avoid coitus when the cervical mucus is copious and for about 3 to 4 days before and after ovulation to avoid a pregnancy.
Question 14.
A couple visiting the infertility clinic for the first time states that they have been trying to conceive for the past 2 years without success.
After a history and physical examination of both partners, what would be the most appropriate outcome for the couple to accomplish by the end of this visit?
(a) Choose an appropriate infertility treatment method.
(b) Acknowledge that only 50% of infertile couples achieve a pregnancy.
(c) Discuss alternative methods of having a family, such as adoption.
(d) Describe each of the potential causes and possible treatment modalities.
Answer:
(d) Describe each of the potential causes and possible treatment modalities.
Explanation:
By the end of the first visit, the couple should be able to identify potential causes and treatment modalities for infertility. If their evaluation shows that a treatment or procedure may help them to conceive, the couple must then decide how to proceed, considering all of the various treatments before selecting one. Treatments can be difficult, painful, or risky. The first visit is not the appropriate time to decide on a treatment plan because the couple needs time to adjust to the diagnosis of infertility, a crisis for most couples. Although the couple may be in a hurry for definitive therapy, a thorough assessment of both partners is necessary before a treatment plan can be initiated.
The success rate for achieving a pregnancy depends on both the cause and the effectiveness of the treatment, and in some cases, it may be only as high as 30%. The couple may desire information about alternatives to treatment, but insufficient data are available to suggest that a specific treatment modality may not be successful.
Suggesting that the couple consider adoption at this time may inappropriately imply that the couple has no other choice. If a specific therapy may result in a pregnancy, the couple should have time to consider their options. After a thorough evaluation, adoption may be considered by the couple as an alternative to the costly, time-consuming, and sometimes painful treatments for infertility.
Question 15.
A 20-year-old primigravid client tells the nurse that her mother had a friend who died from hemorrhage about 10 years ago during a vaginal birth. Which response would be most helpful?
(a) “Today’s modern technology has resulted in a low maternal mortality rate.”
(b) “Do not concern yourself with things that happened in the past.”
(c) “In North America, mothers seldom die in birth.”
(d) “What is it that concerns you about pregnancy, labor, or birth?”
Answer:
(d) “What is it that concerns you about pregnancy, labor, or birth?”
Explanation:
The client is verbalizing concerns about death during birth, thus providing the nurse with an opportunity to gather additional data. Asking the client about these concerns would be most helpful to determine the client’s knowledge base and to provide the nurse with the opportunity to answer any questions and clarify any misconceptions. Although the maternal mortality rate is low in the United States and Canada, maternal deaths do occur, even with modern technology.
Leading causes of maternal mortality in the United States and Canada include embolism, pregnancy-induced hypertension, hemorrhage, ectopic pregnancy, and infection. Telling the client not to concern herself about what has happened in the past is not useful. It only serves to discount the client’s concerns and block further therapeutic communication. Also, postponing or ignoring the client’s need for a discussion about complications of pregnancy may further increase the client’s anxiety.
Question 16.
A 19-year-old nulligravid client visiting the clinic for a routine examination asks the nurse about cervical mucus changes that occur during the menstrual cycle. Which information would the nurse expect to include in the client’s teaching plan?
(a) About midway through the menstrual cycle, cervical mucus is thick and sticky.
(b) During ovulation, the cervix remains dry without any mucus production.
(c) As ovulation approaches, cervical mucus is abundant and clear.
(d) Cervical mucus disappears immediately after ovulation, resuming with menses.
Answer:
(c) As ovulation approaches, cervical mucus is abundant and clear.
Explanation:
As ovulation approaches, cervical mucus is abundant and clear, resembling raw egg white. Ovulation generally occurs 14 days (±2 days) before the beginning of menses. During the luteal phase of the cycle, which occurs after ovulation, the cervical mucus is thick and sticky, making it difficult for sperm to pass. Changes in the cervical mucus are related to the influences of estrogen and progesterone. Cervical mucus is always present.
Question 17.
When instructing a client about the proper use of condoms for pregnancy prevention, the nurse should include which instruction to ensure maxi¬mum effectiveness?
(a) Place the condom over the erect penis before coitus.
(b) Withdraw the condom after coitus when the penis is flaccid.
(c) Ensure that the condom is pulled tightly over the tip of the penis before coitus.
(d) Obtain a prescription for a condom with nonoxynol
Answer:
(a) Place the condom over the erect penis before coitus.
Explanation:
To ensure maximum effectiveness, the condom should always be placed over the erect penis before coitus. Some couples find condom use objectionable because foreplay may have to be interrupted to apply the condom. The penis, covered by the condom, should be withdrawn before the penis becomes flaccid.
Otherwise, semen may escape from the condom, providing an opportunity for possible fertilization. Rather than having the condom pulled tightly over the penis before coitus, space should be left at the tip of the penis to allow the condom to hold the sperm. The client does not need a prescription for a condom with nonoxynol 9 because these are sold over the counter.
Question 18.
The nurse teaches a client about using medroxyprogesterone as a birth control method. Which client statement indicates effective teaching?
(a) “This method of family planning requires monthly injections.”
(b) “I should have my first injection during my menstrual cycle.”
(c) “One possible adverse effect is the absence of a menstrual period.”
(d) “This drug will be given by subcutaneous injections.”
Answer:
(c) “One possible adverse effect is the absence of a menstrual period.”
Explanation:
With medroxyprogesterone acetate, irregular menstrual cycles, and amenorrhea are common adverse effects. Other adverse effects include weight gain, breakthrough bleeding, headaches, and depression. This method requires deep intramuscular injections every 3 months. The first injection should occur within 5 days after menses.
Question 19.
Which instruction should the nurse include in the teaching plan for a 30-year-old multiparous client who will be using an intrauterine device (IUD) for family planning?
(a) Amenorrhea is a common adverse effect of IUDs.
(b) Additional conception protection will be needed.
(c) IUDs are more costly than other forms of contraception.
(d) Severe cramping may occur when the IUD is inserted.
Answer:
(d) Severe cramping may occur when the IUD is inserted.
Explanation:
Severe cramping and pain may occur as the device is passed through the internal cervical os. The insertion of the device is generally done when the client is having her menses because it is unlikely that she is pregnant at that time. Common adverse effects of IUDs are heavy menstrual bleeding and subsequent anemia, not amenorrhea. Uterine infection or ectopic pregnancy may occur.
The IUD has an effectiveness rate of 98%. Therefore, additional protection is not necessary to prevent pregnancy. IUDs generally are less costly than other forms of contraception because they do not require additional expense. Only one insertion is necessary, in comparison to daily doses of oral contraceptives or the need for spermicides in conjunction with diaphragm use.
Question 20.
Which information would the nurse include in a teaching plan about treatments for sexually transmitted infections?
(a) Acyclovir can be used to cure herpes genitalis.
(b) Chlamydia trachomatis infections are usually treated with penicillin.
(c) Ceftriaxone may be used to treat Neisseria gonorrhoeae infections.
(d) Metronidazole is used to treat condylomata acuminata.
Answer:
(c) Ceftriaxone may be used to treat Neisseria gonorrhoeae infections.
Explanation:
Ceftriaxone may be used to treat N. gonor- rhoeae infections and is commonly combined with doxycycline. Both the client and her partner should be treated if gonorrhea is present. Acyclovir can be used to treat herpes genitalis; however, the drug does not cure the disease. C. trachomatis infections are usually treated with antibiotics such as doxycycline or azithromycin. Metronidazole is used to treat trichomoniasis vaginitis, not condylomata acuminata (genital warts).
Question 21.
A couple is visiting the clinic because they have been unable to conceive a baby after 3 years of frequent coitus. The nurse determines that the couple needs further instruction when they identify which factor as a cause of male infertility?
(a) seminal fluid with an alkaline pH
(b) frequent exposure to heat sources
(c) abnormal hormonal stimulation
(d) immunologic factors
Answer:
(a) seminal fluid with an alkaline pH
Explanation:
The couple needs further instruction when they identify that one cause of male infertility is decreased sperm count due to seminal fluid that has an alkaline pH. A slightly alkaline pH is necessary to protect the sperm from the acidic secretions of the vagina and is a normal finding. An alkaline pH is not associated with decreased sperm count. However, seminal fluid that is abnormal in amount, consistency, or chemical composition suggests obstruction, inflammation, or infection, which can decrease sperm production.
The typical number of sperm produced during ejaculation is 400 million. Frequent exposure to heat sources, such as saunas and hot tubs, can decrease sperm production, as can abnormal hormonal stimulation. Immunologic factors produced by the man against his own sperm (autoantibodies) or by the woman can cause the sperm to clump or be unable to penetrate the ovum, thus contributing to infertility.
Question 22.
At a preconception visit, a 24-year-old client is found to have malformation of the uterus. The nurse uses the figure below to explain which type of uterine malformation?
(a) septate uterus
(b) bicornuate uterus
(c) double uterus
(d) uterus didelphys
Answer:
(b) bicornuate uterus
Explanation:
A bicornuate uterus has a “Y” shape and appears to be a double uterus but in fact has only one cervix. A septate uterus contains a septum that extends from the fundus to the cervix, thus dividing the uterus into two separate compartments. A double uterus has two uteri, each of which has a cervix. A uterus didelphys occurs when both uteri of a double uterus are fully formed.
Question 23.
A primigravid client at 15 weeks’ gestation has received teaching about concerning signs and symptoms to report following an amniocentesis. Which statement indicates that the client needs further teaching?
(a) “I need to call if I start to leak fluid from my vagina.”
(b) “If I start bleeding, I will need to call back.”
(c) “If my baby does not move, I need to call my health care provider.”
(d) “If I start running a fever, I should let the office know.”
Answer:
(c) “If my baby does not move, I need to call my health care provider.”
Explanation:
At 15 weeks’ gestation, a primipara will not feel the baby moving. Quickening typically occurs between 18 and 20 weeks’ gestation for a primipara and between 16 and 18 weeks’ gestation for a multipara. Leaking fluid from the vagina should not occur until labor begins and may indicate a rupture of the membranes. Bleeding and a fever are complications that warrant further evaluation and should be reported at any time during the pregnancy.
Question 24.
The nurse is caring for a client who is 12 weeks pregnant and speaks Spanish only. Which interventions should the nurse include in the plan of care at the client’s initial visit? Select all that apply.
(a) Provide brochures in the client’s native language.
(b) Refer the client to a high-risk clinic.
(c) Discuss differences with the dominant culture.
(d) Arrange for an interpreter for her appointments.
(e) Discuss contraception and options.
(f) Review nutritional preferences.
Answer:
(a) Provide brochures in the client’s native language.
(d) Arrange for an interpreter for her appointments.
(f) Review nutritional preferences.
Explanation:
(a), (d) (f) Providing culturally sensitive care includes providing printed material in the client’s native language. There is nothing to indicate that this client has a high-risk pregnancy. Discussing cultural differences is not a priority or important at the first visit. Clients need to have an interpreter for each prenatal visit to translate and interpret questions. Contraceptive options are not a priority for the first prenatal visit. Reviewing dietary intake and discussing nutrition are an important component of early prenatal care.
Question 25.
During a visit to the prenatal clinic, a pregnant client at 32 weeks’ gestation has heartburn. The client needs further instruction when she says she must do what to manage her heartburn?
(a) Avoid highly seasoned foods.
(b) Avoid lying down right after eating.
(c) Eat small, frequent meals.
(d) Consume liquids only between meals.
Answer:
(d) Consume liquids only between meals.
Explanation:
Consuming most liquids between meals rather than at the same time as eating is an excellent strategy to deter nausea and vomiting in pregnancy but does not relieve heartburn. During the third trimester, progesterone causes relaxation of the sphincter, and the pressure of the fetus against the stomach increases the potential of heartburn. Avoiding highly seasoned foods, remaining in an upright position after eating, and eating small, frequent meals are strategies to prevent heartburn.
Question 26.
The nurse is teaching a new prenatal client about her iron deficiency anemia during pregnancy. Which statement indicates that the client needs further instruction about her anemia?
(a) “I will need to take iron supplements now.”
(b) “I may have anemia because my family is of Asian descent.”
(c) “I am considered anemic if my hemoglobin is below 11 g/dL (110 g/L).”
(d) “The anemia increases the workload on my heart.”
Answer:
(b) “I may have anemia because my family is of Asian descent.”
Explanation:
Iron deficiency anemia is caused by insufficient iron stores in the body, poor iron content in the diet of the pregnant woman, or both. Other thalassemias and sickle cell anemia, rather than iron deficiency anemia, can be associated with ethnicity but occur primarily in clients of African or Mediterranean origin.
Because red blood cells increase by about 50% during pregnancy, many clients will need to take supplemental iron to avoid iron deficiency anemia. A pregnant client is considered anemic when the hemoglobin is below 11 mg/dL (110 g/dL). In most types of anemia, the heart must pump more often and harder to deliver oxygen to cells.
Question 27.
Following a positive pregnancy test, a client begins discussing the changes that will occur in the next several months with the nurse. The nurse should include which information about a change the client can anticipate in the first trimester?
(a) differentiating the self from the fetus
(b) enjoying the role of nurturer
(c) preparing for the reality of parenthood
(d) experiencing ambivalence about pregnancy
Answer:
(d) experiencing ambivalence about pregnancy
Explanation:
Many women in their first trimester feel ambivalent about being pregnant because of the significant life changes that occur for most women who have a child. Ambivalence can be expressed as a list of positive and negative consequences of having a child, consideration of financial and social impli-cations, and possible career changes.
During the second trimester, the infant becomes a separate individual to the mother. The mother will begin to enjoy the role of nurturer postpartum. During the third trimester, the mother begins to prepare for parenthood and all of the tasks that parenthood includes.
Question 28.
An antenatal primigravid client has just been informed that she is carrying twins. The plan of care includes educating the client concerning factors that put her at risk for problems during the pregnancy. The nurse realizes the client needs further instruction when she indicates carrying twins puts her at risk for which complication?
(a) preterm labor
(b) twin-to-twin transfusion
(c) anemia
(d) group B streptococcus
Answer:
(d) group B streptococcus
Explanation:
Group B streptococcus is a risk factor for all pregnant women and is not limited to those carrying twins. The multiple gestation client is at risk for preterm labor because uterine distention, a major factor initiating preterm labor, is more likely with a twin gestation. The normal uterus is only able to distend to a certain point, and when that point is reached, labor may be initiated. Twin-to-twin transfusion drains blood from one twin to the second and is a problem that may occur with multiple gestations.
The donor twin may become growth restricted and can have oligohydramnios, while the recipient twin may become polycythemic with polyhydramnios and develop heart failure. Anemia is a common problem with multiple gestation clients. The mother is commonly unable to consume enough protein, calcium, and iron to supply her needs and those of the fetuses. A maternal hemoglobin level below 11 mg/dL (110 g/L] is considered anemic.
Question 29.
A 30-year-old multigravid client has missed three periods and now visits the prenatal clinic because she assumes she is pregnant. She is experiencing enlargement of her abdomen, a positive preg¬nancy test, and changes in the pigmentation on her face and abdomen. These assessment findings reflect this woman is experiencing a cluster of which signs of pregnancy?
(a) positive
(b) probable
(c) presumptive
(d) diagnostic
Answer:
(b) probable
Explanation:
The plan of care should reflect that this woman is experiencing probable signs of pregnancy. She may be pregnant, but the signs and symptoms may have another etiology. An enlarging abdomen and a positive pregnancy test may also be caused by tumors, hydatidiform mole, or other disease processes as well as pregnancy. Changes in the pigmentation of the face may also be caused by oral contraceptive use.
Positive signs of pregnancy are considered diagnostic and include evident fetal heartbeat, fetal movement felt by a trained examiner, and visualization of the fetus with ultrasound confirmation. Presumptive signs are subjective and can have another etiology. These signs and symptoms include lack of menses, nausea, vomiting, fatigue, urinary frequency, and breast changes. The word “diagnostic” is not used to describe the condition of pregnancy.
Question 30.
When preparing a 20-year-old client for a serum pregnancy test, the nurse should include what information?
(a) The test has a high degree of accuracy within 1 week after ovulation.
(b) The test is identical in nature to an over the-counter home pregnancy test.
(c) A positive result is considered a presumptive sign of pregnancy.
(d) A urine sample is needed to obtain quicker
Answer:
(a) The test has a high degree of accuracy within 1 week after ovulation.
Explanation:
The serum pregnancy test measures human chorionic gonadotropin (hCG) in blood plasma and is highly accurate within 1 week after ovulation. The test is performed in a laboratory. Over-the-counter or home pregnancy tests are performed on urine and typically require higher levels of hCG to obtain a positive result. A positive pregnancy test is considered a probable sign of pregnancy. Certain conditions other than pregnancy, such as choriocarcinoma, can cause increased hCG levels.
Question 31.
After instructing a female client about the radioimmunoassay pregnancy test, the nurse determines that the client understands the instructions when the client states that which hormone is evaluated by this test?
(a) prolactin
(b) follicle-stimulating hormone
(c) luteinizing hormone
(d) human chorionic gonadotropin (hCG)
Answer:
(d) human chorionic gonadotropin (hCG)
Explanation:
The hormone analyzed in most pregnancy tests is hCG. In the pregnant woman, trace amounts of hCG appear in the serum as early as 24 to 48 hours after implantation owing to the trophoblast production of this hormone. Prolactin, follicle-stimulating hormone, and luteinizing hormone are not used to detect pregnancy. Prolactin is the hormone secreted by the pituitary gland to prepare the breasts for lactation. Follicle-stimulating hormone is involved in follicle maturation during the menstrual cycle. Luteinizing hormone is responsible for stimulating ovulation.
Question 32.
Using Nagele’s rule for a client whose last normal menstrual period began on May 10, the nurse determines that the client’s estimated date of birth is what date?
(a) January 13
(b) January 17
(c) February 13
(d) February 17
Answer:
(d) February 17
Explanation:
When using Nagele’s rule to determine the estimated date of birth, the nurse would count back 3 calendar months from the first day of the last menstrual period and add 7 days. This means the client’s estimated date is February 17.
Question 33.
After instructing a primigravid client about the functions of the placenta, the nurse determines that the client needs additional teaching when she says that which hormone is produced by the placenta?
(a) estrogen
(b) progesterone
(c) human chorionic gonadotropin (hCG)
(d) testosterone
Answer:
(d) testosterone
Explanation:
The placenta does not produce testosterone. Human placental lactogen, hCG, estrogen, and progesterone are hormones produced by the placenta during pregnancy. The hormone hCG stimulates the synthesis of estrogen and progesterone early in the pregnancy until the placenta can assume this role.
Estrogen results in uterine and breast enlargement. Progesterone aids in maintaining the endometrium, inhibiting uterine contractility, and developing the breasts for lactation. The placenta also produces some nutrients for the embryo and exchanges oxygen, nutrients, and waste products through the chorionic villi.
Question 34 .
The nurse assesses a woman at 24 weeks’ gestation and is unable to find the fetal heartbeat. The fetal heartbeat was heard at the client’s last visit 4 weeks ago. According to priority, the nurse should do the tasks in which order? All options must be used.
(a) Call the health care provider (HCP).
(b) Explain that the fetal heartbeat could not be found at this time.
(c) Obtain different equipment and recheck
(d) Ask the client if the baby is or has been moving.
Answer:
(d) Ask the client if the baby is or has been moving.
(c) Obtain different equipment and recheck
(b) Explain that the fetal heartbeat could not be found at this time.
Explanation:
(a), (b), (c), (d) While initially continuing to attempt to find the fetal heartbeat, the nurse can ask the client if the baby has been moving. This will give a quick idea of status. The next step would be to obtain different equipment and attempt to find the fetal heartbeat again.
A simple statement of fact that the nurse cannot find the heartbeat and is taking steps to rule out equipment error is appropriate. Calling the HCP (Dll would be the last step after it is determined that the baby does not have a heartbeat.
Question 35.
A primiparous client at 10 weeks’ gestation questions the nurse about the need for an ultra-sound. She states, “I feel fine, so why should I have the test?” The nurse should incorporate which state¬ments as the underlying reason for performing the ultrasound now? Select all that apply.
(a) “The test helps us view the gross anatomy of the fetus.”
(b) “We need to determine gestational age.”
(c) “The test will determine if the fetus is viable.”
(d) “We must determine fetal position.”
(e) “We must determine that there is a sufficient nutrient supply for the fetus.”
Answer:
(a) “The test helps us view the gross anatomy of the fetus.”
(b) “We need to determine gestational age.”
Explanation:
(a), (b), Although ultrasounds are not considered part of routine care, the ultrasound is able to confirm the pregnancy, identify the major anatomic features of the fetus and possible abnormalities, and determine the gestational age by measuring crown-to-rump length of the embryo during the first trimester. At this time, the ultrasound cannot confirm that the fetus is viable.
The ultrasound will provide information about fetal position; however, this information would be more important later in the pregnancy, not during the first trimester. The ultrasound would provide no information about nutrient supply for the fetus.
Question 36.
A 20-year-old married client with a positive pregnancy test states, “Is it really true? I cannot believe I am going to have a baby!” Which response by the nurse would be most appropriate at this time?
(a) “Would you like some booklets on the pregnancy experience?”
(b) “Yes, it is true. How does that make you feel?”
(c) “You should be delighted that you are pregnant.”
(d) “What concerns you about this pregnancy?”
Answer:
(b) “Yes, it is true. How does that make you feel?”
Explanation:
This client is expressing a feeling of surprise about having a baby. Therefore, the nurse’s best response would be to confirm the pregnancy, which is something that the client already suspects, and then ascertain how the client is feeling now that the suspicion is confirmed. Studies have shown that a common reaction to pregnancy is summarized as ambivalence or “someday, but not now.” Such feelings are normal and are experienced by many women early in pregnancy.
Offering a pamphlet on pregnancy does not respond to the client’s feelings. Telling the client that she should be delighted ignores, rather than addresses, the client’s feelings. Also, doing so imposes the nurse’s opinion on the client. Ambivalence is a common reaction to pregnancy. Telling the client that she should be delighted may lead to feelings of guilt. Asking about the client’s concerns is premature until the nurse determines the client’s overall feelings about the pregnancy.
Question 37.
A newly diagnosed pregnant client tells the nurse, “If I am going to have all of these discomforts, I am not sure I want to be pregnant!” The nurse interprets the client’s statement as an indication of which perception?
(a) fear of pregnancy outcome
(b) rejection of the pregnancy
(c) normal ambivalence
(d) limited self-care abilities
Answer:
(c) normal ambivalence
Explanation:
Women normally experience ambivalence when pregnancy is confirmed, even if the pregnancy was planned. Although the client’s culture may play a role in openly accepting the pregnancy, most new mothers who have been ambivalent initially accept the reality by the end of the first trimester. Ambivalence also may be expressed throughout the pregnancy; this is believed to be related to the amount of physical discomfort.
The nurse should become concerned and perhaps contact a social worker if the client expresses ambivalence in the third trimester. The client’s statement reflects ambivalence, not fear. There is no evidence to suggest or imply that the client is rejecting the fetus. The client’s statement reflects ambivalence about the pregnancy, not her ability to care for herself.
Question 38.
A client, approximately 11 weeks pregnant, and her husband are seen in the antepartal clinic. The client’s husband tells the nurse that he has been experiencing nausea and vomiting and fatigue along with his wife. The nurse interprets these findings as suggesting that the client’s husband is experiencing which complication?
(a) ptyalism
(b) mittelschmerz
(c) Couvade syndrome
(d) pica
Answer:
(c) Couvade syndrome
Explanation:
Couvade syndrome refers to the situation in which the expectant father experiences some of the discomforts of pregnancy along with the pregnant woman as a means of identifying with the pregnancy. Ptyalism is the term for excessive salivation. Mittelschmerz is the lower abdominal discomfort felt by some women during ovulation. Pica refers to an oral craving for substances such as clay or starch that some pregnant clients experience.
Question 39.
A primigravid client asks the nurse if she can continue to have a glass of wine with dinner during her pregnancy. Which statement would be the nurse’s best response?
(a) “The effects of alcohol on a fetus during pregnancy are unknown.”
(b) “You should limit your consumption to beer and wine.”
(c) “You should abstain from drinking alcoholic beverages.”
(d) “You may have 1 drink of 2oz of alcohol per day.”
Answer:
(c) “You should abstain from drinking alcoholic beverages.”
Explanation:
Maternal alcohol use may result in fetal alcohol syndrome, marked by mild-to-moderate mental retardation, physical growth retardation, central nervous system disorders, and feeding difficulties. Because there is no definitive answer as to how much alcohol can be safely consumed by a pregnant woman, it is recommended that pregnant clients be taught to abstain from drinking alcohol during pregnancy. Smoking and other medications also may affect the fetus.
Question 40.
Examination of a primigravid client having increased vaginal secretions since becoming pregnant reveals clear, highly acidic vaginal secretions. The client denies any perineal itching or burning. The nurse interprets these findings as a response related to which factor?
(a) a decrease in vaginal glycogen stores
(b) development of a sexually transmitted infection
(c) prevention of expulsion of the cervical mucus plug
(d) control of the growth of pathological bacteria
Answer:
(c) prevention of expulsion of the cervical mucus plug
Explanation:
An increase in clear, highly acidic vaginal secretions is a normal finding during pregnancy that aids in controlling the growth of pathologic bacteria. Vaginal secretions increase because of the influence of estrogen secretion and increased vaginal and cervical vascularity. The highly acidic nature of the vaginal secretions is caused by the action of Lactobacillus acidophilus, which increases the lactic acid content of the secretions.
The increased acidity helps to make the vagina resistant to bacterial growth. During pregnancy, estrogen secretion fosters a glycogen-rich environment. Unfortunately, this glycogen-rich, acidic environment fosters the development of yeast (Candida albicans) infections, manifested by itching, burning, and a cheese-like vaginal discharge.
If the client had a sexually transmitted infection, most likely she would have additional symptoms, such as lesions in the genital area or changes in color, consistency, or odor of the vaginal secretions. An increase in vaginal secretions does not help prevent expulsion of the mucus plug. The mucus plug is held in place by the cervix until the cervix becomes ripe.
Question 41.
When measuring the fundal height of a primigravid client at 20 weeks’ gestation, the nurse will locate the fundal height at which point?
(a) halfway between the client’s symphysis pubis and umbilicus
(b) at about the level of the client’s umbilicus
(c) between the client’s umbilicus and xiphoid process
(d) near the client’s xiphoid process and com pressing the diaphragm
Answer:
(b) at about the level of the client’s umbilicus
Explanation:
Measurement of the client’s fundal height is a gross estimate of fetal gestational age. At 20 weeks’ gestation, the fundal height should be at about the level of the client’s umbilicus. The fundus typically is over the symphysis pubis at 12 weeks. A fundal height measurement between these two areas would suggest a fetus with a gestational age between 12 and 20 weeks. The fundal height increases approximately 1 cm/week after 20 weeks’ gestation.
The fundus typically reaches the xiphoid process at approximately 36 weeks’ gestation. A fundal height between the umbilicus and the xiphoid process would suggest a fetus with a gestational age between 20 and 36 weeks. The fundus then commonly returns to about 4 cm below the xiphoid owing to lightening at 40 weeks. Additionally, pressure on the diaphragm occurs late in pregnancy. Therefore, a fundal height measurement near the xiphoid process with diaphragmatic compression suggests a fetus near the gestational age of 36 weeks or older.
Question 42.
A primigravida at 8 weeks’ gestation tells the nurse that she wants an amniocentesis because there is a history of hemophilia A in her family. The nurse informs the client that she will need to wait until she is at 15 weeks’ gestation for the amniocentesis. Which is the most appropriate rationale for the nurse’s statement regarding amniocentesis at 15 weeks’ gestation?
(a) Fetal development needs to be complete before testing.
(b) The volume of amniotic fluid needed for testing will be available by 15 weeks.
(c) Cells indicating hemophilia A are not produced until 15 weeks’ gestation.
(d) Performing an amniocentesis prior to 15 weeks’ gestation carries a greater infection rate.
Answer:
(b) The volume of amniotic fluid needed for testing will be available by 15 weeks.
Explanation:
The volume of fluid needed for amniocentesis is 15 mL, and this is usually available at 15 weeks’ gestation. Fetal development continues throughout the prenatal period. Cells necessary for testing for hemophilia A are available during the entire pregnancy but are not accessible by amniocentesis until 12 weeks’ gestation. Amniocentesis carries a slight risk of infection regardless of when the procedure is performed.
Question 43 .
After instructing a primigravid client about desired weight gain during pregnancy, the nurse determines that the teaching has been successful when the client makes which statement?
(a) “A total weight gain of approximately 20 lb (9 kg) is recommended.”
(b) “A weight gain of 6.6 lb (3 kg) in the second and third trimesters is considered normal.”
(c) “A weight gain of about 12 lb (5.5 kg) every trimester is recommended.”
(d) “Although it varies, a gain of 25 to 35 lb (11.4 to 14.5 kg) is about average.”
Answer:
(d) “Although it varies, a gain of 25 to 35 lb (11.4 to 14.5 kg) is about average.”
Explanation:
The National Academy of Sciences Institute of Medicine and Health Canada recommend that women gain 25 to 35 lb (11.5 to 14.5 kg) during pregnancy. The pattern of weight gain is as important as the total amount of weight gained. Underweight women and women carrying twins should have a greater weight gain. Typically, women should gain 3.5 lb (1.6 kg) during the first trimester and then 1 lb (0.45 kg)/week during the remainder of the pregnancy (24 weeks) for a total of about 27 to 28 lb (12.2 to 12.7 kg).
A weight gain of only 6.6 lb (3 kg) in the second and third trimesters is not normal because the client should be gaining about 1 lb (0.45 kg)/week, or 12 lb (5.4 kg) during the second and third trimesters. Gaining 12 lb (5.4 kg) during each trimester would total 36 lb (16.2 kg), which is slightly more than the recommended weight gain. In addition, nausea and vomiting during the first trimester can contribute to a lack of appetite and smaller weight gain during this trimester.
Question 44.
When developing a teaching plan for a client who is 8 weeks pregnant, the nurse would suggest what foods to meet the client’s need for increased folic acid? Select all that apply.
(a) spinach
(b) bananas
(c) seafood
(d) yogurt
(e) beans
Answer:
(a) spinach
(e) beans
Explanation:
Green, leafy vegetables, such as asparagus, spinach, brussels sprouts, and broccoli, are rich sources of folic acid. Beans, peas, and lentils are also good sources. The pregnant woman needs to eat foods high in folic acid to prevent folic acid deficits, which may result in neural tube defects in the newborn. A well-balanced diet must include whole grains, dairy products, and fresh fruits; however, bananas are rich in potassium, seafood is rich in iodine, and yogurt is rich in calcium, not folic acid.
Question 45.
The nurse instructs a primigravid client about the importance of sufficient vitamin A in her diet. The nurse knows that the instructions have been effective when the client indicates that she should include which foods in her diet?
(a) buttermilk and cheese
(b) strawberries and broccoli
(c) egg yolks and squash
(d) oranges and tomatoes
Answer:
(c) egg yolks and squash
Explanation:
Egg yolks and squash and other yellow vegetables are rich sources of vitamin A. Buttermilk and cheese are good sources of calcium. Strawberries, broccoli, citrus fruits (such as oranges), and tomatoes are good sources of vitamin C, not vitamin A.
Question 46.
The nurse is discussing dietary concerns with pregnant teens. Which choices are convenient for teens yet nutritious for both the mother and fetus? Select all that apply.
(a) milkshake or yogurt with fresh fruit or granola bar
(b) chicken nuggets with tater tots
(c) cheese pizza with spinach and mushroom topping
(d) peanut butter with crackers and a juice drink
(e) buttery light popcorn with diet cola
(f) cheeseburger, pickle, and ketchup
Answer:
(a) milkshake or yogurt with fresh fruit or granola bar
(c) cheese pizza with spinach and mushroom topping
(d) peanut butter with crackers and a juice drink
Explanation:
(a), (c), (d) Dairy products, fresh fruit, vegetables, and foods high in protein (like cheese and peanut butter) are excellent choices. Fried foods, such as chicken nuggets and tater tots, and foods such as cheeseburgers and buttered popcorn are high in fat; carbonated drinks such as diet colas, and foods such as pickles and ketchup contain large amounts of sodium. These foods can lead to an increase in ankle edema and promote weight gain from empty calories.
Question 47.
An antenatal client is discussing her anemia with the nurse in the prenatal clinic. After a discus¬sion about sources of iron to be incorporated into her daily meals, the nurse knows the client needs further instruction when she responds with which statement?
(a) “I can meet two goals when I drink milk lots of iron and meeting my calcium needs at the same time.”
(b) “Drinking coffee, tea, and sodas decreases the absorption of iron.”
(c) “I can increase the absorption of iron by drinking orange juice when I eat.”
(d) “Cream of wheat and molasses are excellent sources of iron.”
Answer:
(a) “I can meet two goals when I drink milk lots of iron and meeting my calcium needs at the same time.”
Explanation:
Milk contains a large amount of calcium but contains no iron. Coffee, tea, and caffeinated soft drinks inhibit the absorption of iron. The vitamin C found in orange juice enhances the absorption of iron. Cream of wheat (1 cup/10 mg iron) and molasses (1 tbsp/3 mg iron) are considered excellent sources of iron as they contain the indicated amounts of iron.
Question 48.
The nurse instructs a primigravid client to increase her intake of foods high in magnesium because of its role in which process?
(a) prevention of demineralization of the mother’s bones
(b) synthesis of proteins, nucleic acids, and fats
(c) amino acid metabolism
(d) synthesis of neural pathways in the fetus
Answer:
(b) synthesis of proteins, nucleic acids, and fats
Explanation:
Magnesium aids in the synthesis of protein, nucleic acids, proteins, and fats. It is important for cell growth and neuromuscular function. Magnesium also activates the enzymes for the metabolism of protein and energy. Calcium prevents demineralization of the mother’s bones. Vitamin B6 is important for amino acid metabolism. Folic acid assists in the development of neural pathways in the fetus.
Question 49.
A client is at 24 weeks’ gestation. The nurse is reviewing the report of laboratory tests as noted below.
Laboratory Results
|
Test |
Results |
|
1. Blood type |
1.A-positive |
|
2. Blood glucose |
2. 90 mg/dl(5 mmol/L) |
|
3. VDRL |
3. Positive |
|
4. Rubella tier |
4. Immune |
The nurse should report which results to the health care provider (HCP)?
(a) blood type
(b) VDRL
(c) blood glucose
(d) rubella titer
(e) hepatitis B
Answer:
(b) VDRL
Explanation:
The nurse reports the results of the VDRL to the HCP fffTIh The pregnant client must be treated for syphilis to prevent perinatal transmission of the disease. The rubella titer and blood sugar values are within normal range. The blood type is not a significant factor in this situation.
Question 50.
The prenatal client wants to know why the nurse is asking about her use of herbal supple¬ments. What is the nurse’s best response?
(a) “I need to assess your risk because most dietary supplements have not been tested in pregnant women, nursing mothers, or children.”
(b) “You may need additional screening because herbal supplements often contain other ingredients that may affect your care.”
(c) “Understanding the full picture of what herbal supplements you use to manage your health will help us better provide coordinated and safe care.”
(d) “Many herbal supplements change the way your body processes many medications and make them less ineffective.”
Answer:
(c) “Understanding the full picture of what herbal supplements you use to manage your health will help us better provide coordinated and safe care.”
Explanation:
Clients often do not tell providers about the use of complementary and alternative approaches because they fear they will be judged. By approaching care as a partnership, the nurse sets the stage for open communication. All other statements are true but begin the conversation in a way that suggests the client has done something wrong.
Question 51.
The nurse is reviewing a pregnant client’s immunization record. Which immuniza¬tions are contraindicated during pregnancy and are not updated at this time? Select all that apply.
(a) tetanus
(b) rubella
(c) mumps
(d) chickenpox
(e) live attenuated influenza vaccine
Answer:
(b) rubella
(c) mumps
(d) chickenpox
Explanation:
(b), (c), (d), (e) During pregnancy, live virus immunizations are not administered because of potential teratogenicity. These immunizations include chickenpox, rubella, mumps, smallpox, and live attenuated influenza vaccine. Vaccines containing killed viruses (tetanus, diphtheria, hepatitis B) may be administered, and in fact are recommended by the CDC if the immunizations are not up-to-date.
Question 52.
A 34-year-old multiparous client at 16 weeks’ gestation who received regular prenatal care for all of her previous pregnancies tells the nurse that she has already felt the baby move. How does the nurse interpret this finding?
(a) the possibility that the client is carrying twins
(b) unusual because most multiparous clients do not experience quickening until 30 weeks’ gestation
(c) evidence that the client’s estimated date of birth is probably off by a few weeks
(d) normal because multiparous clients can experience quickening between 14 and 20 weeks’ gestation
Answer:
(d) normal because multiparous clients can experience quickening between 14 and 20 weeks’ gestation
Explanation:
Although most multiparous women experience quickening at about Y7xh weeks’ gestation, some women may perceive it between 14 and 20 weeks’ gestation because they have been pregnant before and know what to expect. Detecting movement early does not suggest a twin pregnancy. If the multiparous client does not experience quickening by 20 weeks’ gestation, further investigation is warranted because the fetus may have died, the client has a hydatidiform mole, or the pregnancy dating is incorrect. There is no evidence that the client’s expected date of birth is erroneous.
Question 53.
A 17-year-old gravid client presents for her regularly scheduled 26-week prenatal visit. She appears disheveled, is wearing ill-fitting clothes, and does not make eye contact with the nurse. Which items should the nurse discuss with the client? Select all that apply.
(a) intimate partner violence
(b) substance abuse
(c) depression
(d) blood glucose screening
(e) hCG (human chorionic gonadotropin) levels
Answer:
(a) intimate partner violence
(b) substance abuse
(c) depression
(d) blood glucose screening
Explanation:
(a), (b), (c), (d) Anyone could be a victim of intimate partner violence. Health care workers should routinely assess women for intimate partner violence. Pregnant teens have increased risk for not finishing school, smoking, and substance abuse. It is possible that the client is depressed and her appearance and lack of eye contact are symptoms of her depression.
The nurse expects the blood glucose screening test to be prescribed between 24 and 28 weeks’ gestation to screen for gestational diabetes. hCG levels can identify the presence of a pregnancy or give information about an abnormal pregnancy. It would not be done at this time in a normal pregnancy.
Question 54.
When performing Leopold’s maneuvers, which action would the nurse ask the client to perform to ensure optimal comfort and accuracy?
(a) breathing deeply for 1 minute
(b) empting her bladder
(c) drinking a full glass of water
(d) lying on her left side
Answer:
(b) empting her bladder
Explanation:
Leopold’s maneuvers involve abdominal palpation. The client should empty her bladder before the nurse palpates the abdomen. Doing so increases the client’s comfort and makes palpation more accurate. Although breathing deeply may help to relax the client, it has no effect on the accuracy of the results of Leopold’s maneuvers. The client does not need to drink a full glass of water before the examination. The client should be lying in a supine position with the head slightly elevated for greater comfort and with the knees drawn up slightly.
Question 55.
The nurse performed Leopold’s maneuvers and determined that the fetal position is right occiput anterior (ROA). Identify the area where the nurse would place the Doppler to most easily hear fetal heart sounds
Answer:
Explanation:
Because the fetus is determined to be in an ROA, a vertex position, the convex portion of the fetus lying closest to the uterine wall would be located in the lower right quadrant of the abdomen. Placing the Doppler ultrasound over that area would produce the loudest fetal heart sounds.
Question 56.
The nurse is assessing fetal position for a 32-year-old client in her 8th month of pregnancy. As shown below, the fetus is in which position?
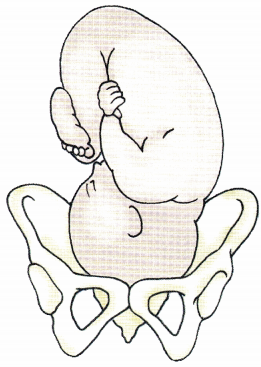
(a) left occipital transverse
(b) left occipital anterior
(c) right occipital transverse
(d) right occipital anterior
Answer:
(b) left occipital anterior
Explanation:
In the left occipital anterior lie, the occiput faces the left anterior segment of the woman’s pelvis. In the left occipital transverse lie, the occiput faces the woman’s left hip. In the right occipital transverse lie, the occiput faces the woman’s right hip. In the right occipital anterior lie, the occiput faces the right anterior segment of the woman’s pelvis.
Question 57.
Which statement by the nurse would be most appropriate when responding to a primigravid client who asks, “What should I do about this brown discoloration across my nose and cheeks?”
(a) “This usually disappears after birth.”
(b) “It is a sign of skin melanoma.”
(c) “The discoloration is due to dilated capillaries.”
(d) “It will fade if you use a prescribed cream.”
Answer:
(a) “This usually disappears after birth.”
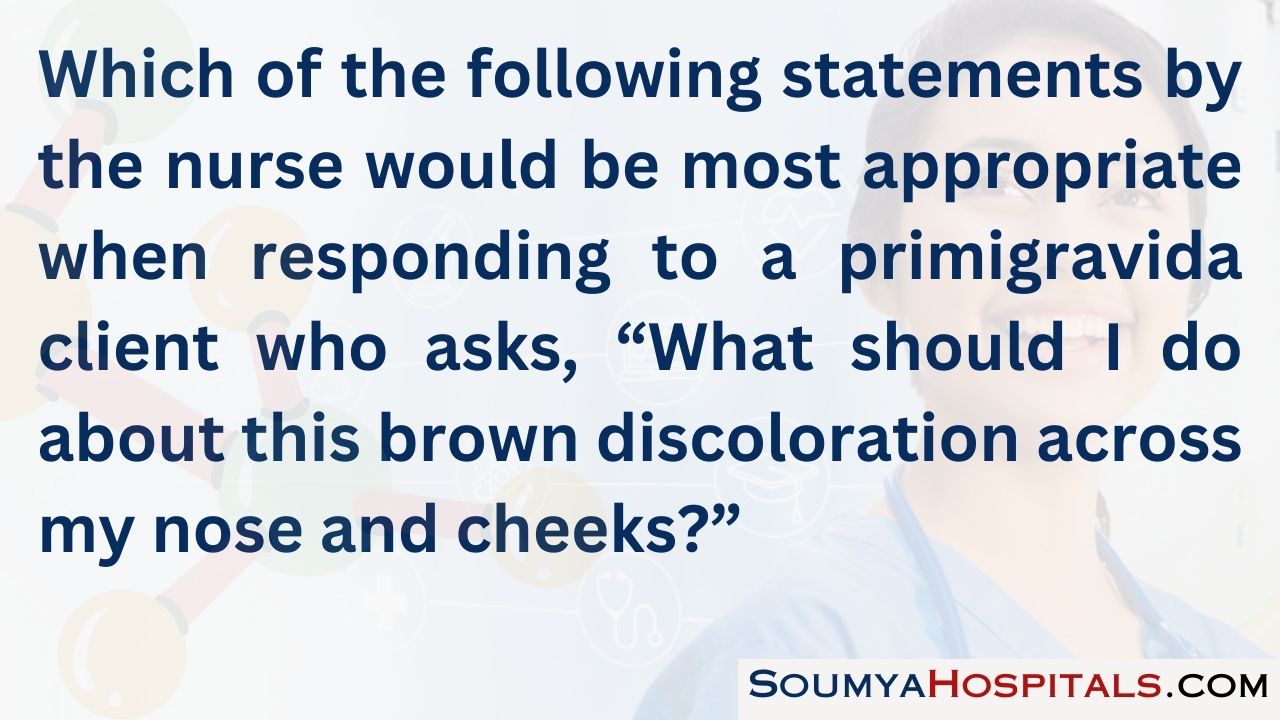
Explanation:
Discoloration on the face that commonly appears during pregnancy, called chloasma (mask of pregnancy), usually fades postpartum and is of no clinical significance. The client who is bothered by her appearance may be able to decrease its prominence with ordinary makeup. Chloasma is not a sign of skin melanoma. It is not caused by dilated capillaries. Rather, it results from increased secretion of melanocyte-stimulating hormones caused by estrogen and progesterone secretion. No treatment is necessary for this condition.
Question 58.
A 36-year-old primigravid client at 22 weeks’ gestation without any complications to date is being seen in the clinic for a routine visit. Why does the nurse need to assess the client’s fundal height?
(a) to determine the level of uterine activity
(b) to identify the need for increased weight gain
(c) to assess the fetal position
(d) to estimate the fetal growth
Answer:
(d) to estimate the fetal growth
Explanation:
Assessment of fundal height is a gross estimate of fetal growth. By 20 weeks’ gestation, the height of the fundus should be at the level of the umbilicus, after which it should increase 1 cm for each week of gestation until approximately 36 weeks’ gestation. Fundal height that is significantly different from that implied by the estimated gestational age warrants further evaluation (e.g., ultrasound examination) because it possibly indicates multiple pregnancy or fetal growth retardation.
Fundal height estimation will not determine uterine activity or a need for increased weight gain. Leopold’s maneuver will determine fetal position but is not typically done in the second trimester when the fetus is still freely moving.
Question 59.
After the nurse reviews the primary health care provider’s (HCP’s) explanation of amniocentesis with a multigravid client, which complication, if stated by the client, indicates that she needs more teaching about the procedure?
(a) risk of infection
(b) possible miscarriage
(c) risk of club foot
(d) fetal organ malformations
Answer:
(d) fetal organ malformations
Explanation:
There is little risk for fetal organ malformations from amniocentesis. One of the primary risks of amniocentesis is stimulation of the uterus and possible miscarriage. Other risks include hemorrhage from penetration of the placenta, infection of the amniotic fluid, and puncture of the fetus. Club foot has been associated with amniocentesis, especially when it is performed before 15 weeks.
Question 60.
A prenatal client wants to begin a yoga-based exercise class to keep her healthy during pregnancy. What information should the nurse include in the plan of care? Select all that apply.
(a) Drink plenty of water before, during, and after a workout.
(b) Take precaution to prevent overheating.
(c) Avoid jerky, high-impact motions.
(d) Modify any positions that put strain on the abdomen.
(e) Participate only classes specifically designed for pregnant clients.
Answer:
(a) Drink plenty of water before, during, and after a workout.
(b) Take precaution to prevent overheating.
(c) Avoid jerky, high-impact motions.
(d) Modify any positions that put strain on the abdomen.
Explanation:
(a), (b), (c), (d) Clients should keep well hydrated with any form of exercise. Dehydration can lead to dizziness and put the client at risk for falls. Later in pregnancy, dehydration can contribute to preterm labor. Becoming overheated can lead to dehydration. In the first trimester heat can act as a teratogen. Ligaments become more relaxed during pregnancy, making joints more mobile. High impact, quick movements can lead to injury.
Many yoga poses put pressure on the abdomen and would need to be modified as a pregnancy progresses. It is unnecessary to restrict participation to a prenatal yoga class only; however, the client should be advised to notify the instructor that she is pregnant and discuss if participating in that particular class is appropriate.
Question 61.
A primigravid client at 28 weeks’ gestation tells the nurse that she and her husband wish to drive to visit relatives who live several hours away. Which recommendation by the nurse would be best?
(a) “Try to avoid traveling anywhere in the car during your third trimester.”
(b) “Limit the time you spend in the car to a maximum of 4 to 5 hours.”
(c) “Taking the trip is okay if you stop every 1 to 2 hours and walk.”
(d) “Avoid wearing your seat belt in the car to prevent injury to the fetus.”
Answer:
(c) “Taking the trip is okay if you stop every 1 to 2 hours and walk.”
Explanation:
The client traveling by automobile should be advised to take intermittent breaks of 10 to 15 minutes, including walking, every 1 to 2 hours to stimulate the circulation, which becomes sluggish during long periods of sitting. Automobile travel is not contraindicated during pregnancy unless the client develops complications. There is no set maximum number of hours allowed. The pregnant client should always wear a seat belt when traveling by automobile. The client should be aware of the nearest health care facility in the city to which she is traveling.
Question 62.
The nurse teaches a client who is 18 weeks pregnant about seat belt safety. Identify the area that indicates that the client understands where the lap portion of the seat belt should be placed.
Answer:

Explanation:
Seat belt safety is important for pregnant women because proper use reduces maternal mortality in car accidents. Both lap and shoulder belts are to be used. The lap portion of the belt is placed snugly but comfortably to fit under the abdominal bulge. Wearing the lap belt over the abdomen could increase the risk of uterine rupture and fetal compli-cations due to belt tightening as the woman is propelled forward during an automobile accident. The shoulder belt is placed snugly across the shoulder, chest, and upper abdomen.
Question 63.
Which recommendation would be most helpful to suggest to a primigravid client at 37 weeks’ gestation who has leg cramps?
(a) Change positions frequently throughout the day.
(b) Alternately flex and extend the legs.
(c) Straighten the knees, and flex the toes toward the chin.
(d) Lie prone in bed with the legs elevated.
Answer:
(c) Straighten the knees, and flex the toes toward the chin.
Explanation:
Leg cramps are thought to result from excessive amounts of phosphorus absorbed from milk products. Straightening the knee and flexing the toes toward the chin is an effective measure to relieve leg cramps. Also, decreasing milk intake and supplementing with calcium lactate may help to reduce the cramping. Keeping the legs warm and elevating them are good preventive measures.
Changing positions frequently aids venous return but is not helpful in relieving leg cramps. Alternately flexing and extending the legs will not help to relieve the leg cramp. Lying prone in the bed is a difficult position for a client at 37 weeks’ gestation to achieve and maintain because of the increase in abdominal size and therefore is not considered helpful.
Question 64.
A nurse sees a pregnant woman showing signs of airway obstruction. When the nurse asks the woman if she needs help, the woman nods her head yes. Indicate the area where the nurse’s fist should be placed to effectively administer thrusts to clear the foreign body from the airway.
Answer:
Explanation:
The fist is placed against the middle of the woman’s sternum, with backward thrusts until the foreign body is expelled. The pressure from the backward thrusts causes compression of the ribs, further adding to the chest and lung pressure, thereby forcing the foreign body to move upward.
Question 65.
When performing Leopold’s maneuvers on a pri mi gravid client at 22 weeks’ gestation, the nurse performs the first maneuver to accomplish which action?
(a) Locate the fetal back and spine.
(b) Determine what is in the fundus.
(c) Determine whether the fetal head is at the pelvic inlet.
(d) Identify the degree of fetal descent and flexion.
Answer:
(b) Determine what is in the fundus.
Explanation:
In the first maneuver, which is done with the nurse facing the client’s head, both hands are used to palpate and determine which fetal body part (e.g., the head or buttocks) is in the fundus. This first maneuver helps to determine the presenting part of the fetus. In the second maneuver, also done with the nurse facing the client’s head, the palms of both hands are used to palpate the sides of the uterus and determine the location of the fetal back and spine.
In the third maneuver, one hand gently grasps the lower portion of the abdomen just above the symphysis pubis to determine whether the fetal head is at the pelvic inlet. The fourth maneuver, done with the nurse facing the client’s feet, determines the degree of fetal descent and flexion into the pelvis.
Question 66.
A primigravid adolescent client at approximately 15 weeks’ gestation is visiting the prenatal clinic to undergo maternal quad screening. What information should the nurse include in the teaching plan for this client?
(a) Ultrasonography usually accompanies maternal quad screen testing.
(b) Results are usually very accurate until 20 weeks’ gestation.
(c) A clean-catch midstream urine specimen is needed.
(d) Increased levels of alpha-fetoprotein are associated with neural tube defects.
Answer:
(d) Increased levels of alpha-fetoprotein are associated with neural tube defects.
Explanation:
Increased alpha-fetoprotein (AFP) is one of the four laboratory values in a maternal quad screen. The labs are human chorionic gonadotropin, estriol, and inhibinA. Increased AFP levels are associated with neural tube defects, such as spina bifida, anencephaly, and encephalocele. Ultrasonography is used to confirm a neural tube defect only when AFP levels are increased. Because AFP levels are usually highest at 15 to 18 weeks’ gestation, this is the optimum time for testing. Performing the test after this time leads to inaccurate results. The client’s blood, not urine, is used for the sample.
Question 67.
Which statement best identifies the rationale for why the nurse reinforces the need for continued prenatal care throughout the pregnancy with an adolescent primigravid client?
(a) Pregnant adolescents are at high risk for pregnancy-induced hypertension.
(b) Gestational diabetes during pregnancy commonly develops in adolescents.
(c) Adolescents need additional instruction related to common discomforts.
(d) The father of the baby is rarely involved in the pregnancy.
Answer:
(a) Pregnant adolescents are at high risk for pregnancy-induced hypertension.
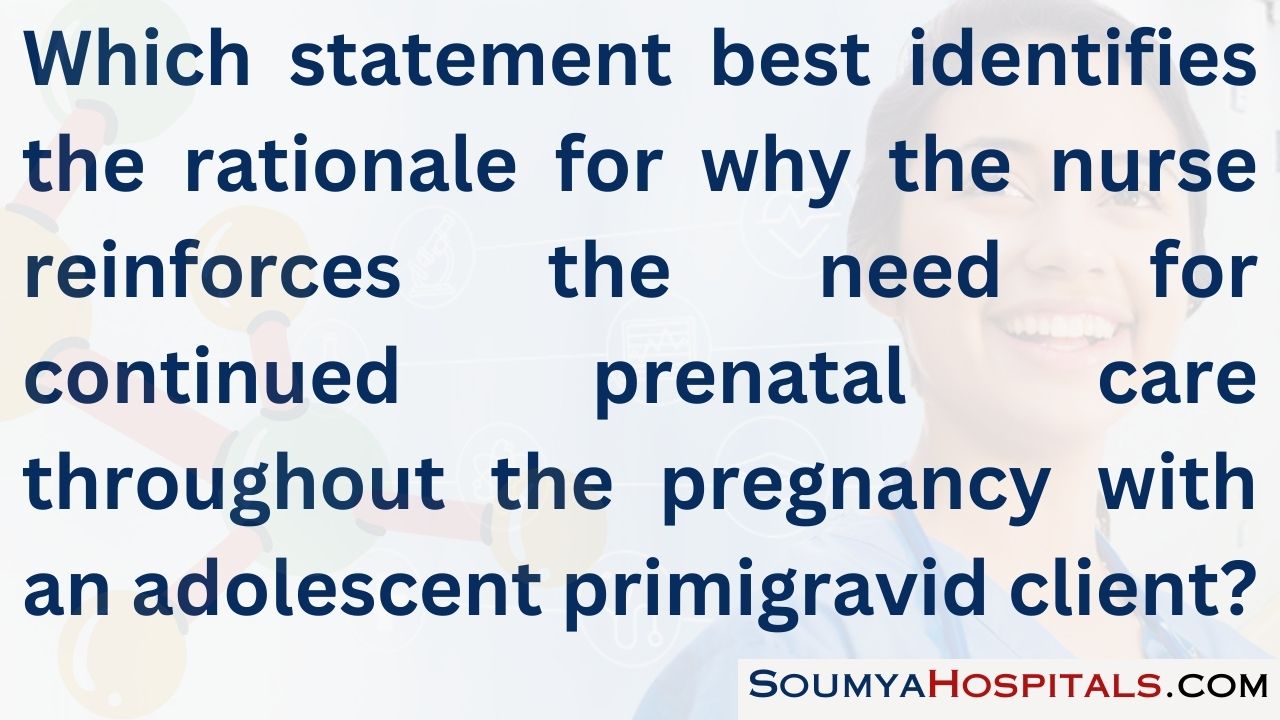
Explanation:
Prenatal care is commonly the most critical factor influencing pregnancy outcomes. This is especially true for adolescents because the most significant medical complication in pregnant adolescents is pregnancy-induced hypertension. Continued prenatal care helps to allow for early detection and prompt intervention should the complication arise. Other risks for adolescents include low-birth-weight infants, preterm labor, iron deficiency anemia, and cephalopelvic disproportion.
Gestational diabetes can occur with any pregnancy regardless of the age of the mother. Generally, all first-time mothers need instruction related to discomforts. Adolescent mothers have better nutrition when they attend group classes and are subject to peer pressure. No evidence demonstrates that most adolescents lack support systems. Fathers may aban-don mothers at any time during the pregnancy; other fathers, regardless of age, are supportive throughout the pregnancy.
Question 68.
Which information would be included in the teaching plan about pregnancy-related breast changes for a primigravid client?
(a) Growth of the milk ducts is greatest during the first 8 weeks of gestation.
(b) Enlargement of the breasts indicates adequate levels of progesterone.
(c) Colostrum is usually secreted by about the 16th week of gestation.
(d) Darkening of the areola occurs during the last month of pregnancy.
Answer:
(c) Colostrum is usually secreted by about the 16th week of gestation.
Explanation:
Colostrum is usually secreted by about the 16th week of gestation in preparation for breastfeeding. Growth of the milk ducts is greatest in the last trimester, not in the first 8 weeks of gestation. Enlargement of the breasts is usually caused by estrogen, not progesterone. Darkening of the areola can occur as early as the 6th week of gestation.
Question 69.
A primigravid client at 32 weeks’ gestation is enrolled in a breastfeeding class. Which statements indicate that the client understands the breastfeed¬ing education? Select all that apply.
(a) “My milk supply will be adequate since I have increased a whole bra size during pregnancy.”
(b) “I can hold my baby several different ways during feedings.”
(c) “If my infant latches on properly, I will not develop mastitis.”
(d) “If I breastfeed, my uterus will return to pre-pregnancy size more quickly.”
(e) “I need to feed my baby when I see feeding cues and not wait until she is crying.”
Answer:
(b) “I can hold my baby several different ways during feedings.”
(d) “If I breastfeed, my uterus will return to pre-pregnancy size more quickly.”
(e) “I need to feed my baby when I see feeding cues and not wait until she is crying.”
Explanation:
(b), (d), (e) Understanding of breastfeeding education is demonstrated by statements involving knowledge of the several positions available for comfortable breastfeeding, oxytocin release from the pituitary leading to a let-down reflex and uterine contractions for involution, and feeding cues helpful in successful breastfeeding (because waiting until the infant is hungry and crying is stressful). Breast size does not ensure successful breastfeeding. Mastitis is an infectious process and is not influenced by latching on.
Question 70.
When planning a class for primigravid clients about the common physiologic changes of pregnancy, the nurse should include which information in the teaching plan?
(a) The temperature decreases slightly early in pregnancy.
(b) Cardiac output increases by 25% to 50% during pregnancy.
(c) The circulating fibrinogen level decreases as much as 50% during pregnancy.
(d) The anterior pituitary gland secretes oxytocin late in pregnancy.
Answer:
(b) Cardiac output increases by 25% to 50% during pregnancy.
Explanation:
During pregnancy, the circulatory system undergoes tremendous changes. Cardiac output increases by 25% to 50%, and circulatory blood volume increases by about 30%. The client may experience transient hypotension and dizziness with sudden position changes. Early in pregnancy, there is a slight increase in the temperature, and clients may attribute this to a sinus infection or a cold. The client may feel warm, but this sensation is transient.
The level of circulating fibrinogen increases as much as 50% during pregnancy, probably because of increased estrogen. Any calf tenderness should be reported because it may indicate a clot. Late in pregnancy, the posterior pituitary gland secretes oxytocin. The client may experience painful Braxton Hicks contractions or early labor symptoms.
Question 71.
When teaching a primigravid client about the diagnostic tests used in pregnancy, the nurse should include which information?
(a) A fetal biophysical profile involves assessments of breathing movements, body move¬ments, tone, amniotic fluid volume, and fetal heart rate reactivity.
(b) Fetal heart rate increases during a nonstress test is an ominous sign and requires further evaluation with fetal echocardiography.
(c) Contraction stress testing, performed on most pregnant women, can be initiated as early as 16 weeks’ gestation.
(d) Percutaneous umbilical blood sampling uses a needle inserted through the vagina to obtain a sample.
Answer:
(a) A fetal biophysical profile involves assessments of breathing movements, body move¬ments, tone, amniotic fluid volume, and fetal heart rate reactivity.
Explanation:
The fetal biophysical profile includes fetal breathing movements, fetal body movements, tone, amniotic fluid volume, and fetal heart rate reactivity. Normal nonstress test findings include at least two qualifying accelerations in the fetal heart rate from baseline in 20 minutes. A contraction stress test or oxytocin challenge test should be performed only on women who are at risk for fetal distress during labor.
The contraction stress test is rarely performed before 28 weeks' gestation because of the possibility of initiating labor. Percutaneous umbilical cord sampling requires the insertion of a needle through the abdomen to obtain a fetal blood sample.
Question 72.
A client asks why she feels so much variability in fetal activity each day. The nurse explains that fetal movement is affected by which factors? Select all that apply.
(a) fetal sleep
(b) barometric pressure
(c) blood glucose
(d) time of day
(e) cigarette smoking
Answer:
(a) fetal sleep
(c) blood glucose
(d) time of day
(e) cigarette smoking
Explanation:
(a), (c), (d), (e) The fetus does go through sleep cycles, rendering it less likely to move while it is asleep. Blood glucose does cross the placenta and can affect fetal movement. Cigarette smoking causes carbon monoxide to cross the placenta, which reduces fetal oxygen. Pregnant women are more likely to notice fetal movement while they are sitting or lying down, and time of day often determines this. Most pregnant women notice fetal movement in the evening. Barometric pressure does not affect fetal activity in utero.
Question 73.
The nurse teaches a primigravid client how to do Kegel exercises. What does the nurse explain is the expected outcome of these exercises?
(a) reducing the risk of hemorrhoids
(b) alleviating lower back discomfort
(c) strengthening the perineal muscles
(d) strengthening the abdominal muscles
Answer:
(c) strengthening the perineal muscles
Explanation:
The purpose of Kegel exercises is to strengthen the perineal muscles in preparation for the labor process. These movements strengthen the pubococcygeal muscle, which surrounds the urinary meatus and vagina. No evidence is available to support the idea that these exercises reduce the risk of hemorrhoids, alleviate lower back discomfort, or strengthen the abdominal muscles.
Question 74.
During a routine clinic visit, a 25-year-old multigravid client who initiated prenatal care at 10 weeks’ gestation and is now in her third trimester states, “I’ve been having strange dreams about the baby. Last week I dreamed he was covered with hair.” What should the nurse tell the mother?
(a) “Dreams like the ones that you describe are very unusual. Please tell me more about them.”
(b) “Commonly when a mother has these dreams, she is trying to cope with becoming a parent.”
(c) “Dreams about the baby late in pregnancy usually mean that labor is about to begin soon.”
(d) “It is not uncommon to have dreams about the baby, particularly in the third trimester. ”
Answer:
(d) “It is not uncommon to have dreams about the baby, particularly in the third trimester. ”
Explanation:
During the third trimester, it is not uncommon for clients to have dreams or fantasies about the baby. Sometimes the dreams are about infants who are malformed or, in this example, covered with hair. There is no evidence to suggest that the client is trying to cope with becoming a parent. Having dreams about the baby does not mean that labor will begin soon.
Question 75.
A primigravid client at 36 weeks’ gestation tells the nurse that she has been experiencing insomnia for the past 2 weeks. Which suggestion would be most helpful?
(a) Practice relaxation techniques before bedtime.
(b) Drink a cup of hot chocolate before bedtime.
(c) Drink a small glass of wine with dinner.
(d) Exercise for 30 minutes just before bedtime.
Answer:
(a) Practice relaxation techniques before bedtime.
Explanation:
Insomnia in the later part of pregnancy is not uncommon because the client has difficulty getting into a position of comfort. This is further compounded by frequent nocturia. The best suggestion would be to advise the client to practice relaxation techniques before bedtime.
The client should avoid caffeine products such as chocolate and coffee before going to bed because caffeine is a stimulant. Alcohol consumption, regardless of the type or amount, should be avoided. Exercise is advised during the day, but it should be avoided before bedtime because exercise can stimulate the client and decrease the client’s ability to fall asleep.
Question 76.
Which client statement indicates a need for additional teaching about self-care during pregnancy?
(a) “I should use nonskid pads when I take a shower or bath.”
(b) “I should avoid using soap on my nipples to prevent drying.”
(c) “I should sit in a hot tub for 20 minutes to relax after working.”
(d) “I should avoid douching even if my vaginal secretions increase.”
Answer:
(c) “I should sit in a hot tub for 20 minutes to relax after working.”
Explanation:
The client needs further instruction when she says it is permissible to sit in a hot tub for 20 minutes to relax after working. Hot tubs and saunas should be avoided, particularly in the first trimester, because their use can lead to maternal hyperthermia, which is associated with fetal anomalies such as central nervous system defects. The client should use nonskid pads in the shower or bath to avoid slipping because the client’s center of gravity has shifted and she may fall.
The client should avoid using soap on the nipples to prevent removal of the natural protective oils. Douching is not recommended for pregnant women because it can destroy the normal flora and increase the client’s risk of infection.
Question 77.
A new antenatal G6, T4, P0, Al, L4 client attends her first prenatal visit with her partner. The nurse is assessing this couple’s psychological response to the pregnancy. Which finding requires the most immediate follow-up?
(a) The couple is concerned with financial changes this pregnancy causes.
(b) The couple expresses ambivalence about the current pregnancy.
(c) The father of the baby states that the pregnancy has changed the mother’s focus.
(d) The father of the baby is irritated that the mother is not like she was before pregnancy.
Answer:
(d) The father of the baby is irritated that the mother is not like she was before pregnancy.
Explanation:
Pregnancy creates changes in the mother and father. Being considerate, accepting changes, and being supportive of the current situation are considered acceptable responses by the father, rather than feeling irritation about these changes. Expressing concern over the financial changes of pregnancy and an expanded family is normal.
The first trimester involves the client and family feeling ambivalent about pregnancy and moving toward acceptance of the changes associated with pregnancy. Maternal acceptance of the pregnancy and a subsequent change in the mother’s focus are normal occurrences.
Question 78.
When preparing a prenatal class about endocrine changes that normally occur during pregnancy, the nurse should include information about which subject?
(a) Human placental lactogen maintains the corpus luteum.
(b) Progesterone is responsible for hyperpigmentation and vascular skin changes.
(c) Estrogen relaxes smooth muscle in the respiratory tract.
(d) The thyroid enlarges with an increase in basal metabolic rate.
Answer:
(d) The thyroid enlarges with an increase in basal metabolic rate.
Explanation:
Thyroid enlargement and increased basal body metabolism are common occurrences during pregnancy. Human placental lactogen enhances milk production. Estrogen is responsible for hyperpigmentation and vascular skin changes. Progesterone relaxes smooth muscle in the respiratory tract.
Question 79.
When developing a series of parent classes on fetal development, the nurse should include which feature as being developed by the end of the 3rd month (9 to 12 weeks)?
(a) external genitalia
(b) myelinization of nerves
(c) brown fat stores
(d) air ducts and alveoli
Answer:
(a) external genitalia
Explanation:
Although sex is not easily discerned at 9 to 12 weeks, external genitalia are developed at this period of fetal development. Myelinization of the nerves begins at about 20 weeks’ gestation. Brown fat stores develop at approximately 21 to 24 weeks. Air ducts and alveoli develop later in the gestational period, at approximately 25 to 28 weeks.
Question 80.
During a 2-hour birth preparation class focusing on the labor and birth process for primigravid clients, the nurse is describing the maneuvers that the fetus goes through during the labor process when the head is the presenting part. In which order do these maneuvers occur? All options must be used.
(a) engagement
(b) flexion
(c) descent
(e) internal rotation
Answer:
(a) engagement
(b) flexion
(c) descent
(e) internal rotation
Explanation:
(a), (b), (c), (d), Engagement refers to the fetus’ entering the true pelvis and occurs before descent in primiparas and concurrently in multiparous women. If the head is the presenting part, the normal maneuvers during labor and birth are (in order) descent, flexion, internal rotation, extension, external rotation, and expulsion. These maneuvers are called the cardinal movements. They occur as the fetal head passes through the maternal pelvis during the normal labor process.
Question 81.
A primigravid client in a preparation for parenting class asks how much blood is lost during an uncomplicated vaginal birth. What should the nurse tell the client?
(a) “The maximum blood loss considered within normal limits is 500 mL.”
(b) “The minimum blood loss considered within normal limits is 1,000 mL.”
(c) “Blood loss during birth is rarely estimated unless there is a hemorrhage.”
(d) “It would be very unusual if you lost more than 100 mL of blood during birth.”
Answer:
(a) “The maximum blood loss considered within normal limits is 500 mL.”
Explanation:
In a normal birth and for the first 24 hours postpartum, a total blood loss not exceeding 500 mL is considered normal. Blood loss during birth is almost always estimated because it provides a valuable indicator for possible hemorrhage. A blood loss of 1,000 mL is considered hemorrhage.
Question 82.
Which statement by a primigravid client about the amniotic fluid and sac indicates the need for further teaching?
(a) “The amniotic fluid helps to dilate the cervix once labor begins.”
(b) “Fetal nutrients are provided by the amniotic fluid.”
(c) “Amniotic fluid provides a cushion against impact of the maternal abdomen.”
(d) “The fetus is kept at a stable temperature by the amniotic fluid and sac.”
Answer:
(b) “Fetal nutrients are provided by the amniotic fluid.”
Explanation:
Although the amniotic fluid promotes normal prenatal development by allowing symmetric development, it does not provide the fetus with nutrients. Rather, nutrients are provided by the placenta. The amniotic fluid does help dilate the cervix once labor begins by pressure and gravity forces. The amniotic fluid helps to protect the fetus from injury by cushioning against impact of the maternal abdomen and allows room and buoyancy for fetal movement. The amniotic fluid and sac keep the fetus at a stable temperature by maintaining a neutral thermal environment.
Question 83.
During a birth preparation class, a primi gravid client at 36 weeks’ gestation tells the nurse, “My lower back has really been bothering me lately.” Which exercise would be most helpful?
(a) pelvic rocking
(b) deep breathing
(c) tailor sitting
(d) squatting
Answer:
(a) pelvic rocking
Explanation:
Pelvic rocking helps to relieve backache during pregnancy and early labor by making the spine more flexible. Deep breathing exercises assist with relaxation and pain relief during labor. Tailor sitting and squatting help stretch the perineal muscles in preparation for labor.
Question 84.
A client is experiencing pain during the first stage of labor. What should the nurse instruct the client to do to manage her pain? Select all that apply.
(a) Walk in the hospital room.
(b) Use slow chest breathing.
(c) Request pain medication on a regular basis.
(d) Lightly massage the abdomen.
(e) Sip ice water.
Answer:
(a) Walk in the hospital room.
(b) Use slow chest breathing.
(c) Request pain medication on a regular basis.
(d) Lightly massage the abdomen.
Explanation:
(a), (b), (d), Pain during the first stage of labor is primarily caused by hypoxia of the uterine and cervical muscle cells during contraction, stretching of the lower uterine segment, dilatation of the cervix and perineum, and pressure on adjacent structures. Ambulating will assist in increasing the circulation of blood to the area and relaxing the muscles. Slow chest breathing is appropriate during the first stage of labor to promote increased oxygenation as well as relaxation.
The woman or her coach can lightly massage the abdomen (effleurage) while using slow chest breathing. Chest breathing and massaging increase oxygenation and relaxation of uterine muscles. Pain medication is not used during the first stage of labor because most medications will slow labor; anesthesia may be considered during the second stage of labor. Sipping ice water, while helpful for maintaining hydration, will not be useful as a pain management strategy.
Question 85.
During a preparation for parenting class, one of the participants asks the nurse, “How will I know if I am really in labor?” What should the nurse tell the participant about true labor contractions?
(a) “Walking around helps to decrease true contractions.”
(b) “True labor contractions may disappear with ambulation, rest, or sleep.”
(c) “The duration and frequency of true labor contractions remain the same.”
(d) “True labor contractions are felt first in the lower back, then the abdomen."
Answer:
(d) “True labor contractions are felt first in the lower back, then the abdomen."
Explanation:
With true labor, the contractions are felt first in the lower back and then the abdomen. They gradually increase in frequency and duration and do not disappear with ambulation, rest, or sleep. In true labor, the cervix dilates and effaces. Walking tends to increase true contractions. False labor contractions disappear with ambulation, rest, or sleep. False labor contractions commonly remain the same in duration and frequency. Clients who are experiencing false labor may have pain, even though the contractions are not very effective.
Question 86.
After instructing participants in a birth education class about methods for coping with discomforts in the first stage of labor, the nurse determines that one of the pregnant clients needs further instruction when she says that she has been practicing which technique?
(a) biofeedback
(b) effleurage
(c) guided imagery
(d) pelvic tilt exercises
Answer:
(d) pelvic tilt exercises
Explanation:
Pelvic tilt exercises are useful to alleviate backache during pregnancy and labor but are not useful for the pain from contractions. Biofeedback (a conscious effort to control the response to pain), effleurage (light uterine massage), and guided imagery (focusing on a pleasant scene) are appropriate pain relief techniques to practice before labor begins. Various breathing exercises also can help to alleviate the discomfort from contraction pain.
Question 87.
After a preparation for parenting class session, a pregnant client tells the nurse that she has had some yellow-gray frothy vaginal discharge and local itching. What is the best advice for the nurse to give the client?
(a) Use an over-the-counter cream for yeast infections.
(b) Schedule an appointment at the clinic for an examination.
(c) Administer a vinegar douche under low pressure.
(d) Prepare for preterm labor and birth.
Answer:
(b) Schedule an appointment at the clinic for an examination.
Explanation:
Increased vaginal discharge is normal during pregnancy, but yellow-gray frothy discharge with local itching is associated with infection (e.g., Trichomonas vaginalis). The client’s symptoms must be further assessed by a health professional because the client needs treatment for this condition. T. vaginalis infection is commonly treated with metronidazole; however, this drug is not used in the first trimester.
In the first trimester, the typical treatment is topical clotrimazole. Although a yeast infection is associated with vaginal itching, the vaginal discharge is cheese-like. Furthermore, because the client may have a serious vaginal infection, over-the-counter medications are not advised until the client has been evaluated. Douching is not recommended during pregnancy because it would predispose the client to an ascending infection.
The client is not exhibiting signs and symptoms of preterm labor, such as contractions or leaking fluid. And although the client’s problems are suggestive of a T. vaginalis infection, which can lead to preterm labor and premature rupture of the membranes, further evaluation is needed to confirm the cause of the infection.
Question 88.
The topic of physiologic changes that occur during pregnancy is to be included in a parenting class for primigravid clients who are in their first half of pregnancy. Which topic would be important for the nurse to include in the teaching plan?
(a) decreased plasma volume
(b) increased risk for urinary tract infections
(c) increased peripheral vascular resistance
(d) increased hemoglobin levels
Answer:
(b) increased risk for urinary tract infections
Explanation:
During pregnancy, urinary tract infections are more common because of urinary stasis. Clients need instructions about increasing fluid volume intake. Plasma volume increases during pregnancy. The increase in plasma volume is more pronounced and occurs earlier than does the increase in red blood cell mass, possibly resulting in physiologic anemia. Peripheral vascular resistance decreases during pregnancy, providing a relatively stable blood pressure. Hemoglobin levels decrease during pregnancy even though there is an increase in blood volume.
Question 89.
A multigravid client at 32 weeks’ gestation has experienced hemolytic disease of the newborn in a previous pregnancy. The nurse should prepare the client for frequent antibody titer evaluations obtained from which source?
(a) placental blood
(b) amniotic fluid
(c) fetal blood
(d) maternal blood
Answer:
(d) maternal blood
Explanation:
For the Rh-negative client who may be pregnant with an Rh-positive fetus, an indirect Coombs test measures antibodies in the maternal blood. Titers should be performed monthly during the first and second trimesters and biweekly during the third trimester and the week before the due date.
Question 90.
Which diagnostic test would be the most important for a 40-year-old primigravid client to have in the second trimester of her pregnancy?
(a) beta strep screening
(b) chorionic villus sampling
(c) ultrasound testing
(d) quad screen
Answer:
(d) quad screen
Explanation:
A maternal quad screen testing is done to screen for genetic and neural tube abnormalities between the 15th and 18th weeks of gestation. The four tests included are an alpha fetoprotein (AFP), human chorionic gonadotropin, estriol, and inhibin- A. Abnormally high levels of AFP found in maternal serum may be indicative of neural tube defects such as anencephaly and spina bifida.
Low levels may indicate trisomy 21 (Down syndrome). Beta strep testing is done in the third trimester. Chorionic villus sampling is done as early as 10 weeks’ gestation to detect anomalies. Ultrasound testing may be done in the first trimester to determine fetal viability and in the third trimester to determine pelvic adequacy and fetal or placental position.
Question 91.
The nurse is caring for a client who has a history of gastric bypass surgery and is now being seen for her first prenatal visit. Which interventions should be included in the plan of care? Select all that apply.
(a) Take a prenatal vitamin with 400 meg of folic acid.
(b) Refer the client to a registered dietician.
(c) Draw glucose levels at each prenatal visit.
(d) Counsel her that she will most likely gain all of her weight back.
(e) Check urine at each visit for protein and glucose.
(f) Monitor with nonstress tests beginning at 20 weeks.
Answer:
(a) Take a prenatal vitamin with 400 meg of folic acid.
(b) Refer the client to a registered dietician.
(f) Monitor with nonstress tests beginning at 20 weeks.
Explanation:
(a), (b), (e) Prenatal care includes a general sup-plementation of 400 meg of folic acid, and clients with a history of gastric bypass should be referred to a dietician to determine adequate nutrient intake. All pregnant clients have their urine routinely checked for protein and sugar. There is no indication for checking glucose levels at each prenatal visit in clients who have undergone gastric bypass. Gastric bypass clients are not at risk of gaining all of their weight back. No evidence supports implementing nonstress tests at 20 weeks.
Question 92.
A client with a past medical history of ventricular septal defect repaired in infancy is seen at the prenatal clinic. She has dyspnea with exertion and is very tired. Her vital signs are oxygen saturation 98, pulse 80, respirations 20, blood pressure 116/72 mm Hg. She has +2 pedal edema and clear breath sounds. The nurse determines the client's symptoms indicate which cardiac functional classification?
(a) class I
(b) class II
(c) class III
(d) class IV
Answer:
(b) class II
Explanation:
According to both the New York Heart Association and the Canadian Cardiovascular Society, this client would fit under class II because she is symptomatic with increased activity (dyspnea with exertion). Class II clients have cardiac disease and a slight limitation in physical activity. When physical activity occurs, the client may experience angina, difficulty breathing, palpations, and fatigue. All of the client’s other symptoms are within normal limits.
Question 93.
A primigravid client has completed her first prenatal visit and blood work. Her laboratory test for the hepatitis B surface antigen (HBsAg) is positive. The nurse can advise the client that the plan of care for this newborn will include which interventions? Select all that apply.
(a) hepatitis B immune globulin at birth
(b) series of three hepatitis B vaccinations per recommended schedule
(c) hepatitis B screening when born
(d) isolation of infant during hospitalization
(e) universal precautions for mother and infant
(f) contraindication for breastfeeding
Answer:
(a) hepatitis B immune globulin at birth
(b) series of three hepatitis B vaccinations per recommended schedule
(f) contraindication for breastfeeding
Explanation:
(a), (b), (e) The test result indicates that the mother has an active hepatitis infection and is a carrier. Hepatitis B immune globulin at birth provides the infant with passive immunity against hepatitis B and serves as a prophylactic treatment. Additionally, the infant will be started on the vac-cine series of three injections. The infant should not be screened or isolated because the infant is already hepatitis B positive. As with all clients, universal precautions should be used and are sufficient to prevent transmission of the virus. Women who are positive for hepatitis B surface antigen are able to breastfeed.
Question 94.
A woman with asthma controlled through the consistent use of medication is now pregnant for the first time. Which client statement concern¬ing asthma during pregnancy indicates the need for further instruction?
(a) “I need to continue taking my asthma medication as prescribed.”
(b) “It is my goal to prevent or limit asthma attacks.”
(c) “During an asthma attack, oxygen needs to continue to be high for mother and fetus.”
(d) “Bronchodilators should be used only when necessary because of the risk they present to the fetus.”
Answer:
(d) “Bronchodilators should be used only when necessary because of the risk they present to the fetus.”
Explanation:
Asthma medications and bronchodilators should be continued during pregnancy as prescribed before the pregnancy began. The medications do not cause harm to the mother or fetus. Regular use of asthma medication will usually prevent asthma attacks. Prevention and limitation of an asthma attack is the goal of care for a client who is or is not pregnant and is the appropriate care strategy. During an asthma attack, oxygen needs continue as with any pregnant client, but the airways are edematous, decreasing perfusion. Asthma exacerbations during pregnancy may occur as a result of infrequent use of medication rather than as a result of the pregnancy.
Question 95.
A woman at 22 weeks’ gestation has right upper quadrant pain radiating to her back. She rates the pain as 9 on a scale of 1 to 10 and says that
it has occurred 2 times in the last week for about 4 hours at a time. She does not associate the pain with food. Which nursing measure is the highest priority for this client?
(a) Educate the client concerning changes occurring in the gallbladder as a result of pregnancy.
(b) Refer the client to her health care provider (HCP) for evaluation and treatment of the pain.
(c) Discuss nutritional strategies to decrease the possibility of heartburn.
(d) Support the client's use of acetaminophen to relieve pain.
Answer:
(b) Refer the client to her health care provider (HCP) for evaluation and treatment of the pain.
Explanation:
The nurse seeing this client should refer her to an HCP (EDI) for further evaluation of the pain. This referral would allow a more definitive diagnosis and medical interventions that may include surgery. Referral would occur because of her high pain rating as well as the other symptoms, which suggest gallbladder disease. During pregnancy, the gallblad-der is under the influence of progesterone, which is a smooth muscle relaxant. Because bile does not move through the system as quickly during pregnancy, bile stasis and gallstone formation can occur.
Although education should be a continuous strategy, with pain at this level, a brief explanation is most appropriate. Major emphasis should be placed on determining the cause and treating the pain. It is not appropriate for the nurse to diagnose pain at this level as heartburn. Discussing nutritional strategies to prevent heartburn are appropriate during pregnancy, but not in this situation. Acetaminophen is an acceptable medication to take during pregnancy but should not be used on a regular basis as it can mask other problems.
Question 96.
A client in the triage area who is at 19 weeks’ gestation states that she has not felt her baby move in the past week, and no fetal heart tones are found. While evaluating this client, the nurse identifies her as being at the highest risk for developing which problem?
(a) abruptio placentae
(b) HELLP syndrome
(c) disseminated intravascular coagulation
(d) threatened abortion
Answer:
(c) disseminated intravascular coagulation
Explanation:
A fetus that has died and is retained in utero places the mother at risk for disseminated intravascular coagulation (DIC) because the clotting factors within the maternal system are consumed when the nonviable fetus is retained. The longer the fetus is retained in utero, the greater the risk of DIC.
This client has no risk factors, history, or signs and symptoms that put her at risk for abruptio placentae such as sharp pain and “woody,” firm consistency of the abdomen. HELLP syndrome is a complication of preeclampsia that does not occur before 20 weeks’ gestation unless a molar pregnancy is present. There is no evidence that she is threatening to abort as she has no cramping or vaginal bleeding.
Question 97.
The nurse performs a routine prenatal assessment on a woman at 35 weeks’ gestation and finds vital signs: blood pressure 138/88 mm Hg, pulse 82/min, respirations 18/min, temperature 99.1°F (37.3°C). Which statement is most appropriate for the nurse to make at this time?
(a) “Your pulse is low. Do you exercise a lot?”
(b) “Your blood pressure is slightly high. I will check it again before you leave.”
(c) “You have a slight temperature. Do you feel hot?”
(d) “Your vital signs are all normal. I will document them on your medical record.”
Answer:
(b) “Your blood pressure is slightly high. I will check it again before you leave.”
Explanation:
A blood pressure reading of 138/88 mm Hg is nearing hypertension range and could be a sign of developing gestational hypertension. Conversely, the client may be experiencing “white coat” syndrome or could be anxious during the prenatal visit. In order to obtain an accurate blood pressure reading, the nurse should allow the woman to rest for a period of time and recheck the blood pressure in the same arm and while the woman is in the same position. This blood pressure is considered approaching high. All other vitals are within normal range.
Question 98.
A 40-year-old client at 8 weeks’ gestation has a 3-year-old child with Down syndrome. The nurse is discussing amniocentesis and chorionic villus sampling as genetic screening methods for the expected baby. The nurse is confident that the teaching has been understood when the client makes which statement?
(a) “Each test identifies a different part of the infant’s genetic makeup."
(b) “Chorionic villus sampling can be performed earlier in pregnancy.”
(c) “The test results take the same length of time to be completed.”
(d) “Amniocentesis is a more dangerous procedure for the fetus.”
Answer:
(b) “Chorionic villus sampling can be performed earlier in pregnancy.”
Explanation:
Chorionic villus sampling (CVS) can be performed from approximately 8 to 12 weeks’ gestation, while amniocentesis cannot be performed until between 11 weeks’ gestation and the end of the pregnancy. Eleven weeks’ gestation is the earliest possible time within the pregnancy to obtain a suf-ficient amount of amniotic fluid to sample. Because CVS takes a piece of membrane surrounding the infant, this procedure can be completed earlier in the pregnancy.
Amniocentesis and chorionic villus sampling identify the genetic makeup of the fetus in its entirety, rather than a portion of it. Laboratory analysis of chorionic villus sampling takes less time to complete. Both procedures place the fetus at risk, and postprocedure teaching asks the client to report the same complicating events (bleeding, cramping, fever, and fluid leakage from the vagina).
Question 99.
After conducting a presentation to a group of adolescent parents on the topic of adolescent pregnancy, the nurse determines that one of the parents needs further instruction when the parent says that adolescents are at greater risk for which complication?
(a) denial of the pregnancy
(b) low-birth-weight infant
(c) cephalopelvic disproportion
(d) congenital anomalies
Answer:
(d) congenital anomalies
Explanation:
Additional teaching is needed when the parent says that adolescents are at greater risk for congenital anomalies. Although adolescents are at greater risk for denial of the pregnancy, lack of prenatal care, low-birth-weight infant, cephalopelvic disproportion, anemia, nutritional deficits, and a higher maternal mortality rate, studies reveal that congenital anomalies are not more common in adolescent pregnancies.
Question 100.
A dilatation and curettage (D&C) are scheduled for a primigravid client admitted to the hospital at 10 weeks’ gestation with abdominal cramping, bright red vaginal spotting, and passage of some of the products of conception. The nurse should assess the client further for the expression of which feeling?
(a) ambivalence
(b) anxiety
(c) fear
(d) guilt
Answer:
(d) guilt
Explanation:
With a spontaneous abortion, many clients and their partners feel an acute sense of loss. Their grieving commonly includes feelings of guilt, which may be expressed as wondering whether the woman could have done something to prevent the loss. Anger, sadness, and disappointment are also common emotions after a pregnancy loss. Ambivalence, anxiety, and fear are not common emotions after a spontaneous abortion.
Question 101.
When providing care to a client who has undergone a dilatation and curettage (D&C) after a spontaneous abortion, the nurse administers hydroxyzine as prescribed. What is the expected outcome?
(a) absence of nausea
(b) minimized pain
(c) decreased uterine cramping
(d) improved uterine contractility
Answer:
(a) absence of nausea
Explanation:
Hydroxyzine has a tranquilizing effect and also decreases nausea and vomiting. It does not decrease fluid retention, reduce pain, decrease uterine cramping, or promote uterine contractility. One of the adverse effects of the medication is sleepiness. Ibuprofen may decrease pain from uterine cramping. Oxytocin may be used to increase uterine contractility.
Question 102.
On entering the room of a client who has undergone a dilatation and curettage (D&C) for a spontaneous abortion, the nurse finds the client crying. Which comment by the nurse would be most appropriate?
(a) “Are you having a great deal of uterine pain?”
(b) “Commonly spontaneous abortion means a defective embryo.”
(c) “I am truly sorry you lost your baby.”
(d) “It is important that you do not try to get pregnant too soon.”
Answer:
(c) “I am truly sorry you lost your baby.”
Explanation:
The death of a fetus at any time during pregnancy is a tragedy for most parents. After a spontaneous abortion, the client and family members can be expected to suffer from grief for several months or longer. When offering support, a simple statement such as “I am truly sorry you lost your baby” is most appropriate. Therapeutic communication techniques help the client and family understand the meaning of the loss, move less stressfully through the grief process, and share feelings.
Asking the client whether she is experiencing a great deal of uterine pain is inappropriate because this is a “yes-no" question and does not allow the client to express her feelings. Saying that the embryo was defective is inappropriate because this may lead the client to think that she contributed to the fetus’s demise.
This is not the appropriate time to discuss embryonic or fetal malformations. However, the nurse should explain to the client that this situation was not her fault. Telling the client that she should not get pregnant again too soon is not therapeutic and discounts the feelings of the expectant mother who had already begun to bond with the fetus.
Question 103.
A multigravid client who stands for long periods while working in a factory visits the prenatal clinic at 35 weeks’ gestation, stating, “The varicose veins in my legs have really been bothering me lately.” Which instruction would be most helpful?
(a) Perform slow contraction and relaxation of the feet and ankles twice daily.
(b) Take frequent rest periods with the legs elevated above the hips.
(c) Avoid support hoses that reach above the leg varicosities.
(d) Take a leave of absence from work to avoid prolonged standing.
Answer:
(b) Take frequent rest periods with the legs elevated above the hips.
Explanation:
The client with leg varicosities should take frequent rest periods with the legs elevated above the hips to promote venous circulation. The client should avoid constrictive clothing, but a support hose that reaches above the varicosities may help alleviate the pain.
Contracting and relaxing the feet and ankles twice daily is not helpful because it does not promote circulation. Taking a leave of absence from work may not be possible because of economic reasons. The client should try to rest with her legs elevated or walk around for a few minutes every 2 hours while on the job.
Question 104.
A primigravid client at 8 weeks’ gestation tells the nurse that since having had sexual relations with a new partner 2 weeks ago, she has noticed flu-like symptoms, enlarged lymph nodes, and clusters of vesicles in her vagina. The nurse refers the client to a primary health care provider (HCP) because the nurse suspects which sexually transmitted infection?
(a) gonorrhea
(b) Chlamydia trachomatis infection
(c) syphilis
(d) herpes genitalis
Answer:
(d) herpes genitalis
Explanation:
The client is reporting symptoms typically associated with herpes genitalis. Some women have no symptoms of gonorrhea. Others may experience vaginal itching and a thick, purulent vaginal discharge. C. trachomatis infection in women is commonly asymptomatic, but symptoms may include a yellowish discharge and painful urination. The first symptom of syphilis is a painless chancre.
Question 105.
The nurse is caring for a 24-year-old primigravid client scheduled for emergency surgery because of a probable ectopic pregnancy. What is the most important thing for the nurse to do?
(a) Prepare to witness an informed consent for surgery.
(b) Assess the client for massive external bleeding.
(c) Explain that the fallopian tube can be salvaged.
(d) Monitor the client for uterine contractions.
Answer:
(a) Prepare to witness an informed consent for surgery.
Explanation:
The client may need surgery to remove a ruptured fallopian tube where the pregnancy has occurred, and the nurse is usually responsible for witnessing the signature on the informed consent Oil. Typically, if bleeding is occurring, it is internal, and there is only scant vaginal bleeding with no discoloration. The nurse cannot determine whether the fallopian tube can be salvaged; this can be accomplished only during surgery.
If the tube has ruptured, it must be removed. If the tube has not ruptured, a linear salpingostomy may be done to salvage the tube for future pregnancies. With an ectopic pregnancy, although the client is experiencing abdominal pain, she is not having uterine contractions.
Question 106.
The nurse is reviewing results for clients who are having antenatal testing. The assessment data from which client warrant prompt notification of the health care provider (HCP) and a further plan of care?
(a) primigravida who reports fetal movement 6 times in 2 hours
(b) multigravida who had a positive oxytocin challenge test
(c) primigravida whose infant has a biophysical profile of 9
(d) multigravida whose infant has a moderate variability on a nonstress test
Answer:
(b) multigravida who had a positive oxytocin challenge test
Explanation:
Late decelerations during an oxytocin challenge test indicate that the infant is not receiving enough oxygen during contractions and is exhibiting signs of uteroplacental insufficiency. This client would need further medical intervention. Fetal movement 6 times in 2 hours is adequate in a healthy fetus, and a biophysical profile of 9 indicates that the risk of fetal asphyxia is rare.
A normal nonstress test report shows that the fetal heart rate is between 110 and 160 with moderate variability, with 2 fetal heart rate accelerations of 15 beats per minute above baseline and lasting for 15 seconds within a 20-minute period and no decelerations.
Question 107.
A client asks the nurse why taking folic acid is so important before and during pregnancy. What should the nurse tell the client?
(a) “Folic acid is important in preventing neural tube defects in newborns and preventing anemia in mothers.”
(b) “Eating foods with moderate amounts of folic acid helps regulate blood glucose levels.”
(c) “Folic acid consumption helps with the absorption of iron during pregnancy. ”
(d) “Folic acid is needed to promote blood clotting and collagen formation in the newborn.”
Answer:
(a) “Folic acid is important in preventing neural tube defects in newborns and preventing anemia in mothers.”
Explanation:
Folic acid supplementation is recommended to prevent neural tube defects and anemia in pregnancy. Deficiencies increase the risk of hemorrhage during birth as well as infection. The recommended dose prior to pregnancy is 400 meg/day; while breastfeeding and during pregnancy, the recommended dosage is 400 to 800 meg/day. Blood glucose levels are not regulated by the intake of folic acid. Vitamin C potentiates the absorption of iron and is also associated with blood clotting or collagen formation.
Question 108.
A nurse is assigned to the obstetrical triage area. When beginning the assignment, the nurse is given a report about four clients waiting to be seen. Place the clients in the order in which the nurse should see them. All options must be used.
(a) a primigravid client at 10 weeks’ gestation stating she is not feeling well with nausea and vomiting, urinary frequency, and fatigue
(b) a multiparous client at 32 weeks’ gestation asking for assistance with finding a new primary health care provider (HCP)
(c) a single mother at 4 months postpartum fearful of shaking her baby when he cries
(d) an antenatal client at 16 weeks’ gestation who has occasional sharp pain on her left side radiating from her symphysis to her fundus
Answer:
(c) a single mother at 4 months postpartum fearful of shaking her baby when he cries
(d) an antenatal client at 16 weeks’ gestation who has occasional sharp pain on her left side radiating from her symphysis to her fundus
(b) a multiparous client at 32 weeks’ gestation asking for assistance with finding a new primary health care provider (HCP)
Explanation:
(a), (b), (c), (d) The first client to be seen should be the postpartum mother who is fearful of shaking her infant. Postpartum depression is a disorder that may occur during the first year postpartum but peaks at 4 weeks postpartum, prior to menses, or upon weaning.
As a single mother, this client may not have support, a large factor putting women at risk. Other factors accentuating risk include prior depressive or bipolar illness and self-dissatisfaction. Second, the nurse should see the 16-week antenatal client, who is likely experiencing round ligament syndrome.
At this point in the pregnancy, the uterus is stretching into the abdomen causing this type of pain. The pain is on the wrong side to be attributed to appen-dicitis or gallbladder disease. Nursing interventions to ease the pain include a heating pad or bringing the legs toward the abdomen.
The nurse should next see the primigravid client who states she is not feeling well because she is exhibiting signs and symptoms of discomfort experienced by most women in the first trimester. The multiparous client at 32 weeks’ gestation is the lowest priority as she is physically well, while the other clients have physical and psychological problems. In most emergency department situations, she may not be seen by medical or nursing staff but would be given the names of HCPs © in the reception area.
Question 109.
The nurse is working in an ambulatory obstetrics setting. What are emphasized client safety procedures for this setting? Select all that apply.
(a) handwashing or antiseptic use when entering and leaving a room
(b) use of two client identifiers when initiating contact with a client
(c) use of same abbreviations as in the hospital setting
(d) conducting preprocedure verification asking for client name and procedure to be performed
(e) preventing infection by isolating anyone with nausea and vomiting
Answer:
(a) handwashing or antiseptic use when entering and leaving a room
(b) use of two client identifiers when initiating contact with a client
(c) use of same abbreviations as in the hospital setting
(d) conducting preprocedure verification asking for client name and procedure to be performed.
Explanation:
(a), (b), (c), (d) The same safety policies apply to both inpatient and outpatient settings and are adapted to the individual specialty. Handwashing and use of two client identifiers are standard procedures. Abbreviations that are used for inpatient are also used for outpatient as the same mistakes can occur in either setting with confusion in spelling or interpretation of letters and numbers.
Preprocedure verification with name and procedure is used in the operating room, inpatient, and in ambulatory settings regardless of the procedure. It is logical to place clients with obvious communicable diseases by themselves, but nausea and vomiting are a “normal” situation in early pregnancy and not contagious.
Must Read: