The CEN Study Guide are designed to reflect the types of scenarios and patient situations encountered in real-world nursing practice.
Wounds Emergencies CEN Study Guide
Wound Assessment and Management
- Skin is composed of 3 layers.
- The epidermis is the outermost layer of the skin. This waterproof layer contains no blood vessels and acts mainly to protect the body.
- Under the epidermis lies the dermis, which consists of dense connective tissue that allows skin to stretch and flex. The dermis is home to blood vessels, glands, and hair follicles.
- The hypodermis is a layer of fat below the dermis that stores energy (in the form of fat) and acts as a cushion for the body. The hypodermis is sometimes called the subcutaneous layer.
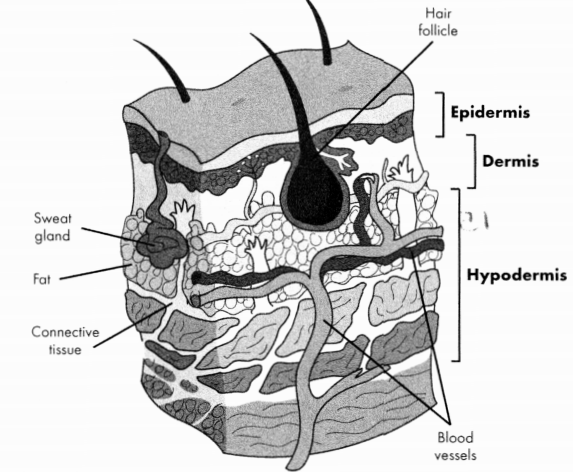
Figure 15.1. Anatomy of the Skin
General guidelines for wound care are outlined below.
- History and physical examination of wound:
- Should be done after patient is stable.
- Get vaccination history: Tetanus vaccination (DTaP, DT, Tdap, or Td) is required if patient has not been vaccinated within the last 5 years. Tetanus immunoglobulin (Tig) is required for unvaccinated patients with a high risk of wound infection.
- Include neurovascular assessment and examination of anatomy of a wound.
- X-rays as needed.
- Local anesthesia:
- Local anesthesia (injected or topical) should be administered before the wound is cleaned and closed.
- Common anesthetics include lidocaine (duration 1-2 hours), bupivacaine (duration 4-8 hours), and procaine (duration 15 - 45 minutes).
- Epinephrine may be added to anesthetic agents to increase the duration of effect.
- Wound cleaning:
- Irrigate with sterile water or normal saline to flush debris from wound.
- Remove foreign bodies.
- Debride nonviable tissue.
- Wound closure:
Methods of primary closure include sutures, staples, wound tape, and glue.
- Glue should not be used in high-tension areas (e.g., joints) or on mucous membranes.
- Staples should only be used in areas where scars will not be visible.
- Wound tape may be used for superficial wounds but may fall off when exposed to moisture.
Topical antibiotics may be applied after wound closure for wounds at high risk for infection.
- Wound dressing:
- gauze and non-adherent pads: used for dry, closed wounds
- wet-to-dry dressings: The innermost layer is wet and keeps wound bed moist
- transparent film: securement for IVs, moisture-retentive
- calcium alginate dressing: absorbs wound exudate
- hydrogel: promotes moisture within wound bed
- foam dressing: provides cushioning over bony prominences
TABLE 15.1. Types Of Wound Closure
|
Type |
Description |
|
Primary |
|
|
Secondary |
|
|
Tertiary |
|
Specific Wounds
TABLE 15.2. Diagnosis and Management of Trauma Wounds
|
Wound |
Management |
|
Avulsion full thickness injury in which skin Degloving injury |
|
|
Laceration a tear of the soft tissue; external Injection injury injection of substances (e.g., |
|
|
Missile injury damage from a projectile (e.g., |
|
|
Puncture wounds caused by an object entering |
|
Wound Infections
Pathophysiology
Trauma wounds are at high risk for infection because they are contaminated by debris and microorganisms. Surgical site infections may also require emergency care, particularly if the patient had a preexisting infection or there was spillage from the GI tract during surgery. If not treated properly wound infections prevent proper healing and may lead to complications including cellulitis, endocarditis, septicemia, and osteomyelitis.
Physical Examination
- fever
- pain, erythema, and edema around the wound
- purulent exudate from a wound
Diagnostic Tests
CBC with differential and cultures to identify an infectious organism
Management
- wound care, including drainage, debridement, and appropriate dressings
- incision and drainage of abscesses
- topical antibiotics for non-purulent, local infections
- oral antibiotics for purulent local infections
- IV antibiotics for systemic infections or high-risk patients