CEN Test Questions often come with detailed explanations to aid your understanding.
Toxicology And Substance Abuse CEN Practice Questions - CEN Questions on Toxicology And Substance Abuse
Question 1.
A patient presents to the emergency department after overdosing on an alpha-adrenergic antagonist medication. Which of the following assessment findings would the emergency nurse likely uncover?
(a) Warm, flushed skin
(b) Decreased respirations
(c) Elevated blood pressure
(d) Increased serum glucose
Answer:
(a) Warm, flushed skin
Rationale:
Warm and flushed skin is the most likely of the findings to be uncovered. Alpha-adrenergic antagonists would result in vasodilation (warm and flushed skin, hypotension), glycogenesis (decreased blood glucose), and dry skin. Alpha receptors of the sympathetic system do not affect the respiratory drive, which are controlled by the beta2 receptors, and this would make bradypnea an unlikely finding. Because vasodilation is a result of alpha-adrenergic antagonists, a finding of hypotension, rather than hypertension, would be more likely. And, finally, because this medication would cause glycogenesis, it is more likely for the patient to present with hypoglycemia as opposed to hyperglycemia.
Remember to keep it simple! Many (if not most) questions on the examination will fall back to the basics. Remember, in Toxicology the basics are the toxidromes. Take the time to really learn them. I promise it will be time VERY well spent!
Question 2.
A patient presents with an ingestion of an unknown substance. The emergency nurse notes the patient to have bradycardia, diminished bowel sounds, miosis, and cool, dry skin. Which of the following agents did the patient most likely ingest?
(a) Opioid
(b) Anticholinergic
(c) Sedative-hypnotic
(d) Sympathomimetic
Answer:
(a) Opioid
Rationale:
The opioid toxidrome includes bradycardia, constricted pupils (miosis), hypotension, hypothermia, diminished bowel sounds, bradypnea, and no change in diaphoresis; therefore, opioid would be the most likely choice in this scenario. Anticholinergics and sym- pathomimetics are known to have tachycardia, rather than bradycardia, mydriasis (dilated pupils) rather than miosis, and increased body temperature. Sedative-hypnotics are known to cause bradycardia, diminished bowel sounds, and cool, dry skin, but are not associated with miosis.
Question 3.
A patient arrives in the emergency department after a toxic ingestion of carbidopa/levodopa (Sinemet). Which of the following sets of symptoms would the emergency i nurse most likely observe in this patient on initial assessment?
(a) Tachycardia, miosis, flushed skin
(b) Dry mouth, absent bowel sounds, fever
(c) Increased urine output, hypertension, confusion
(d) Hallucinations, bradycardia, cool/clammy skin
Answer:
(b) Dry mouth, absent bowel sounds, fever
Rationale:
Dry mouth, absent bowel sounds, and fever are all symptoms consistent with toxicity from this medication. Carbidopa/levodopa (Sinemet) is a Parkinsonian drug and produces symptoms from the an-ticholinergic toxidrome. These symptoms often include tachycardia, dilated pupils (mydriasis), hypertension, hyperthermia, decreased or absent bowel sounds, and in-hibition of diaphoresis. Although tachycardia and flushed skin may be seen, mydriasis, rather than miosis, would be expected in this situation.
Hypertension and confusion (due to body temperatures over 41° C [105.8° F] causing denaturing of neurotransmitters and creating psychosis) may be expected; however, the blockade of muscarine binding sites inhibits fluid mobilization and would more likely decrease, rather than increase, urine production. The patient may have hallucinations, and would likely have tachycardia, rather than bradycardia, and hot and dry skin, rather than cool and clammy skin.
Many times the same basic content will be referenced in the questions in different ways. Notice how often the concept of toxidrome symptoms comes up. That is not a cheat, it is reality. Think about your practice and how often you see a patient and begin planning care around the symptoms displayed or the symptoms associated with the chief complaint. The examination is no different. So, again, I em-phasize, understand the basics and do not try to memorize all the individual drug effects; learn their class and the majority of the work is done!
Question 4.
The emergency nurse should prepare to administer which of the following medications to a patient with symptoms of organophosphate overdose?
(a) Glucagon (GlucaGen)
(b) Flumazenil (Romazicon)
(c) Physostigmine (Antilirium)
(d) Atropine sulfate (Atropine)
Answer:
(b) Flumazenil (Romazicon)
Rationale:
The antidote is an anticholinergic agent such as atropine, which is given in large doses. Organophosphate poisoning leads to cholinergic overstimulation. Physostigmine is a cholinergic agent and will worsen symptoms. Flumazenil reverses the sedative effects of benzodiazepines. Glucagon is the antidote for beta-adrenergic blockers.
Organophosphate poisoning is a cholinergic crisis that can happen with products such as bug spray. Think “wet” with cholinergic situations because all body fluids that can be secreted are in this situation. A good mnemonic to use for this is MUDDLES. This stands for Mz'osi's, and then increased Urination, Defecation, Diaphoresis, Lacrimation, Excitation, and Salivation. This happens with biochemical substances such as Sarin gas as well.
Question 5.
The emergency nurse suspects that an inebriated patient in the emergency department has ingested methanol after which of the following odors is notecl on the patient’s breath?
(a) Bitter almond
(b) Moth balls
(c) Formalin
(d) Garlic
Answer:
(c) Formalin
Rationale:
Formalin is a characteristic breath odor in methanol poisoning because formic acid is a metabo-lite of methanol. Several poisons may be indicated by the presence of associated breath odors. Bitter almond, for example, is characteristic of cyanide. The odor of moth balls is characteristic of camphor and naphthalene. Garlic is characteristic of arsenic, organophosphates, phosphorous, selenium, and thallium.
Another important key is to make a short list of exceptional findings or special cases. Know the basics of the toxidromes, and then tack on to that the handful of special findings such as, in this case, characteristic odors.
Question 6.
Emergency Medical Services personnel arrive in the emergency department with a patient with a depressed mental status and slowed respirations. They state that no pill bottles or needles were found at the scene, but they did find a white powdery substance and a pipe that the patient appeared to have been smoking. Which of the following additional symptoms should the emergency nurse anticipate assessing?
(a) Tachycardia
(b) Hot, dry skin
(c) Hypertension
(d) Pinpoint pupils
Answer:
(d) Pinpoint pupils
Rationale:
This patient shows signs of a possible opioid overdose, which includes the depressed mental state and decreased respiratory rate. Opioids, except for meperidine, cause pinpoint pupils. Other signs of opioid toxicity include bradycardia, hypotension, flushed cool skin, bradypnea, and decreased bowel sounds. Hypertension and tachycardia would not be anticipated in opioid overdose. Hot, dry skin is seen with an anticholinergic overdose, because the lack of diaphoresis in this specific toxicity leads to hyperthermia but would not be seen in opioid overdose.
Question 7.
A child is brought to the emergency department after ingesting oleander. The nurse should monitor the patient for:
(a) Drooling.
(b) Dysarthria.
(c) Bradycardia.
(d) Constipation.
Answer:
(c) Bradycardia.
Rationale:
Oleander is a plant that can produce cardiac glycoside effects. Symptoms of toxicity are similar to those of digoxin toxicity and include dysrhythmias (especially bradycardia), hyperkalemia, anorexia, nausea, vomiting, altered mental status, and visual dis-turbances. Dysarthria, drooling, and constipation are not associated with oleander toxicity.
After you have mastered the core content, such as tox-idromes in this case, try to learn examples of drugs or plants that produce these effects. Questions will often change it up by giving you a specific substance and you need to be able to determine the basic toxidrome it falls within. Other plants that cause digitalis-like symptoms are foxglove and lily of the valley.
Question 8.
Which of the following is the appropriate antidote for an ingestion of acetaminophen (Tylenol)?
(a) Succimer (Chemet)
(b) Deferoxamine mesylate (Desferal)
(c) Romazicon (flumazenil)
(d) N-Acetylcysteine (Mucomyst)
Answer:
(d) N-Acetylcysteine (Mucomyst)
Rationale:
The antidote for acetaminophen toxicity is N-acetylcysteine, which enhances conversion of toxic metabolites to nontoxic metabolites by providing the substance glutathione that works to clean up the metabolite NAPQI, which causes the liver damage. There are both oral and intravenous preparations of N-acetylcysteine. Mucomyst is the oral form and Acetadote is the intravenous form. Deferoxamine mesylate is the antidote for iron intoxication. Succimer is an antidote for lead poisoning, and flumazenil reverses the sedative effects of benzodiazepines.
Question 9.
Which of the following symptoms are considered among the first symptoms of iron toxicity?
(a) Fever over 101° F (38.3° C)
(b) Fecal impactions
(c) Coagulopathies
(d) Diarrhea
Answer:
(d) Diarrhea
Rationale:
The first phase of iron toxicity occurs within 0 to 2 hours after exposure and includes nausea, vomiting, abdominal pain, hematemesis, hemqtochezia (blood in the stool), and hypotension. Diarrhea, rather than constipation, would be associated with the first phase of iron toxicity. Fevers are not directly associated with iron toxicity, although they may be noted during the secondary phase because of dehydration. Coagulopathies are more associated with the acidosis of phase three of iron toxicity and not expected in the early phases.
The second phase of toxicity occurs within 2 and 48 hours of ingestion and is commonly a resolution of symptoms and perceived improvement in the condition, although the patient may have symptoms of dehydration that may include mild fevers. The third phase often takes 48 to 96 hours to appear and includes symptoms of metabolic acidosis, coagu-lopathies, hemorrhage, hypovolemic shock, hepatic failure, and renal failure.
Some questions rely on simple recall of facts, while others, like this one, ask you to know not just what happens, but when it happens in the progression of toxicity.
Remember, the goal is not to know everything before you enter the examination, but rather not to be thrown off or surprised by questions. Do not be sent into a tailspin during your examination. Take it slow. Learn the basics. Then challenge yourself to sharpen the knowledge you are gaining.
Question 10.
When assessing a patient with a suspected overdose of warfarin (Coumadin), the emergency nurse would anticipate which of the following?
(a) Purpura to skin
(b) Pain to posterior calf
(c) Elevated partial thromboplastin time (PTT)
(d) Decreased international normalized ratio (INR)
Answer:
(a) Purpura to skin
Rationale:
Purpura to the skin would be an expected finding in this patient because of the effect of warfarin (Coumadin) in inhibiting the recycling of vitamin K to its usable form. This reduction in functional vitamin K causes a reduction in vitamin K-dependent reactions that form the clotting factor of the extrinsic cascade: factor VII.
It also has a negative impact on nonspecific clotting factors of the common clotting pathway (factors II, IX, and X). The overall toxicity effect of this is a reduction in clotting ability and increased likelihood of bleeding episodes. Because this patient is likely to have bleeding episodes, pain to the posterior calf, a symptom often associated with deep vein thrombosis, is not likely to be seen. Factor VII is measured by the laboratory tests, prothrombin time (PT) and international normalized ratio (INR), rather than the partial thromboplastin time (PTT) test that measures the intrinsic factors (factors VIII, IX, XI, and! XII); therefore, an elevation in PTT is not a likely finding in this situation. Because warfarin (Coumadin) inhibits the creation of factor VII, an elevated INR would be anticipated rather than a decreased result.
"PHEW" That explanation was a bit intense! Sorry, I think my nerd showed a little on that one. In this review I do not want to dumb anything down and insult you, but I also know that not everyone appreciates the level of detail of patho-physiology that was presented there. I choose to see the best in you. I set the bar as high as I can and encourage you to reach for it. I know you will not always immediately get it, and that is perfectly okay. Just absorb as much as you can and challenge yourself to learn a little more each time. This is how we learn. We try-fail-adapt-overcome! Do not lose heart, you can do this. Remember what I told you earlier? You are AWESOME!
Question 11.
Tricyclic antidepressant overdoses have three main toxic features. These features are cardiotoxicity, adrenergic blocking, and:
(a) Anticoagulation.
(b) Anticholinergic effects.
(c) Sympathomimetic effects.
(d) Central nervous system excitation.
Answer:
(b) Anticholinergic effects.
Rationale:
The three effects associated with tricyclic antidepressant overdoses are cardiotoxicity (prolonged PR interval, widened QRS, prolonged QT interval, heart blocks, and asystole), adrenergic blocking leading to hypotension, and anticholinergic effects (dry skin and mouth with a depressed level of consciousness). There are no anticoagulation or sympathomimetic effects and the central nervous system is depressed rather than excited.
Question 12.
After chewing rhubarb leaves, a 3-year-old is brought to the emergency department. The emergency nurse should assess for which of the following conditions?
(a) Lethargy V
(b) Dysphagia
(c) Bradycardia
(d) Hypertension
Answer:
(b) Dysphagia
Rationale:
Dysphagia would be the most likely symptom in this scenario because rhubarb leaves contain oxalic acid, a toxin that irritates the mouth and throat. The acid may cause edema of the mouth and throat, dysphagia, and increased salivation. Systemic effects include hypocalcemia with calcium oxalate crystals in the urine. Lethargy may occur after ingestion of several plants, especially of the amygdalin-glycoside-cyanide category such as seeds of apples, pears, or apricots, but is not associated with ingestion of rhubarb leaves. Bradycardia is more often found after ingestion of plants that contain cardiac glycosides such as oleander, foxglove, or lily of the valley. Hypertension occurs after ingestion of plants that contain anticholinergic agents such as jimson weed rather than with rhubarb.
Question 13.
A patient presents to the emergency department after overdosing on levothyroxine (Synthroid). Among other symptoms, the patient has a core body temperature of 106.4° F (41.3° C). In addition to active external cooling methods, which of the following interventions would be optimal in this situation?
(a) Give acetaminophen (Tylenol) orally.
(b) Provide acetylsalicylic acid (Aspirin) rectally.
(c) Administer ketorolac (Toradol) intravenously.
(d) Instill Lugol iodine solution via nasogastric tube.
Answer:
(a) Give acetaminophen (Tylenol) orally.
Rationale:
Acetaminophen is the ideal choice because it will lower the set point without additional negative side effects. Hyperpyrexia caused by toxicity of thyroid hormone leads to uncontrolled hyperthermia and cellular breakdown, including clotting factor destruction. This is an acute life-threatening condition and must be addressed early. Thyroid hormone stimulates the hypothalamus’ temperature-regulating center known as the set point and, when the set point is high, prevents the body’s thermoregulatory function from cooling the body down. Antipyretic medications will directly lower this set point and allow the body to assist in dropping the emergent temperature.
Because the high temperature can destroy clotting factors, it is advised not to use nonsteroidal anti-inflammatory drugs (NSAIDs) to correct the fever because they may increase the risk of coagulopathies. In addition, salicylates, such as aspirin, can have detrimental effects of clotting ability and also create active metabolites that directly stimulate thyroid release from binding sites. Administering Lugol iodine solution is not incorrect, per se, but it will, at best, only decrease the further release of thyroid, and not do anything to actively stop the life-threatening problems harming the patient. Iodine solution must be given at least 1 hour after antithyroid medications such as methimazole or propylthiouracil (PTU). Therefore, reducing the temperature would be a higher priority.
Remember, not all high body temperatures are created equal! Patients can be hot due to inability to cool themselves (hyperpyrexia) or overproduction overexposure to heat (hyperthermia). Hyperpyrexia, when the set point is high, may be seen with metabolism-induced fevers (illness or inflammation cause set point to rise), increased hormones (hyperthyroidism or pregnancy hormone), or control malfunction (increased intracranial pressure or brain injury disrupts the hypothalamus’ ability to dissipate heat normally).
Hyperthermia, when heat overcomes the ability to cool, may be seen with high external temperatures (heat stroke) or high internal produc¬tion of heat (sympathomimetic toxicity). Although the problem (high body temperature) is the same for each of these, the treatment is dramatically different. Understanding the cause of the patient’s high body temperature is key to treatment.
Question 14.
Which of the following would be most likely noted by the emergency nurse in a patient with a known benzodiazepine overdose?
(a) Miosis
(b) Diarrhea
(c) Bradypnea
(d) Hyperthermia
Answer:
(c) Bradypnea
Rationale:
Benzodiazepines are within the sedative hypnotic toxidrome and have symptoms of bradycardia, hypotension, hypothermia, decreased bowel motility, and bradypnea. Constipation, rather than diarrhea, would be associated with benzodiazepine overdose. A decrease in body temperature, rather than hyperthermia, would be anticipated in this situation. Sedative-hypnotics are not normally associated with changes to pupil size.
Question 15.
Borborygmus would be associated with which of the following toxic overdoses?
(a) Cocaine
(b) Tincture of opium
(c) Donepezil (Aricept)
(d) Alprazolam (Xanax)
Answer:
(c) Donepezil (Aricept)
Rationale:
Donepezil (Aricept) is an example of a cholinergic medication and would be associated with increased bowel motility and diarrhea in a toxic over-dose. Borborygmus is the sound of air or fluid moving through the intestines and is commonly known as bowel sounds. Bowel motility, which would lead to increased borborygmus, is primarily governed by neurotransmitters of the parasympathetic nervous system. Cocaine, a member of the sympathomimetic toxidrome, has minimal effect on the gastrointestinal tract, although it may cause a decrease in motility. Opium, the namesake of the opioid class of medications, would cause a decrease in borborygmus. Alprazolam (Xanax) is a benzodiazepine and is associated with a decrease in bowel motility.
Question 16.
A 15-year-old presents to the emergency department with tachycardia; dry, flushed skin; confusion; and restlessness. The patient’s friends say that they were all at a party and ate some “stinkweed.” Recognizing this as jimson weed, which of the following interventions is NOT indicated in this scenario?
(a) Providing a cooling blanket
(b) Administering physostigmine
(c) Performing endotracheal intubation
(d) Administering IV crystalloid solution
Answer:
(c) Performing endotracheal intubation
Rationale:
Jimson weed is not known to cause airway compromise; therefore, endotracheal intubation is not normally indicated in these patients. Jimson weed is known to elicit anticholinergic properties when consumed. These symptoms may include tachycardia, dry skin, hyperthermia, psychosis and hallucinations, vasoconstriction, mydriasis (dilating pupils), increased blood sugar, and tachypnea.
Cooling measures, such as cooling blankets or cool cloths and cooled IV fluids, may be used to treat hyperthermia. Physostigmine is an acetylcholinesterase inhibitor and can, therefore, reverse the peripheral and central manifestations of anticholinergic excess; however, this medication can cause bradycardia and asystole along with other side effects. It must be given very slowly!
Anticholinergic manifestations that can be found with medications such as tricyclics can be remembered with the help of a mnemonic: blind as a bat, red as a beet, dry as a bone, mad as a hatter, hotter than Hades. This helps remind us of dilated pupils (blind as a bat), flushed skin (red as a beet), dry mucous membranes and urinary retention (dry as a bone), anxiety or other psychiatric symptoms (mad as a hatter), and hyperthermia (hotter than Hades): Remember that anticholinergics are “dry" and cholinergic issues are "wet. ”
Question 17.
On assessment of a patient with a suspected single-drug intentional overdose, the emergency nurse notes dilated pupils; hypoactive bowel sounds; and hot, dry, and flushed skin. Which of the following medications would be the most likely source of the overdose based on the symptoms present?
(a) Alprazolam (Xanax)
(b) Amitriptyline (Elavil)
(c) Methylphenidate (Ritalin)
(d) Morphine sulfate (Roxanol)
Answer:
(b) Amitriptyline (Elavil)
Rationale:
Based on this information and findings of this patient, the only medication that fits all criteria for this toxidrome is amitriptyline (Elavil). The four medications listed are from the toxidromes of sedatives (alprazolam), anticholinergics (amitriptyline), sympa- thomimetics (methylphenidate), and opioids (morphine sulfate). The symptoms for anticholinergics include tachycardia, dilated pupils (mydriasis), hypertension, hyperthermia, decreased bowel sounds, tachypnea, and dry skin.
The symptoms for opioids include bradycardia, constricted pupils (miosis), hypotension, hypothermia, decreased bowel sounds, bradypnea, and no effect on diaphoresis. The symptoms for sedatives include bradycardia, hypotension, hypothermia, decreased bowel sounds, bradypnea, and no effect on diaphoresis or pupil size. The symptoms for sympathomimetics include tachycardia, dilated pupils’(mydriasis), hyper-tension, hyperthermia, tachypnea, and diaphoresis, and bowel sounds may be hypoactive or hyperactive.
Remember, analysis questions always require you to bring a little extra to the table! There is nearly always some interpretation that you must do with the information in the question to understand what the answer choices are really indicating. This example, in my opinion, is one of the most straightforward in the analysis style. Here, the question presents you with symptoms you recognize as part of a specific toxidrome. You are then provided with specific medi-cations that you must identify as existing within one of the toxidromes as well. After that, it a simple enough task, to choose the correct choice with a matching toxidrome.
Question 18.
Following interventions for a pure beta2-cholinergic antagonist overdose, which of the following assessments would indicate treatment was successful?
(a) Increased heart rate
(b) Decreased respiratory rate
(c) Increased moisture to skin
(d) Decreased diastolic blood pressure
Answer:
(b) Decreased respiratory rate
Rationale:
If treatment was successful, decreased respiratory rate would be an expected outcome. A beta2-cholinergic antagonist, such as ipratropium (Atrovent), would block muscarine receptor sites of acetylcholine and result in unopposed sympathetic stimulation of the beta2-adrenergic receptors primarily in the lungs. Symptoms of the overdose would include tachypnea and bronchodilation if the medication is selective, as was the case in this scenario. In this sce-nario, we are not looking at the overdose, but rather at a resolution of the overdose symptoms.
Increased heart rate would not be expected, both because a decrease in sympathetic stimulation should occur and because with a pure beta2 agent the beta! receptors of the heart are not likely to be affected. Moisture to the skin and changes in diastolic blood pressure are associated with alpha-receptor activity rather than beta2 receptors and unlikely to be confirmation of successful treatment in this scenario.
Here is our first example of an evaluation-style question. These can be tricky if you do not understand the intention. In assessment questions, you are tasked to identify the problem on the basis of the assessment of the patient. After that, intervention questions ask you what do you do to fix identified problems. Evaluation questions make you determine whether your intervention worked.
So, the question may present a patient with a specific problem, but asks you something like “what indicates treatment was successful?" Be careful not to answer on the basis of symptoms of the condition presented, because if the treatment was successful, the patient will not have that anymore; instead, the patient will have symptoms opposite to that of the problem presented. Just read carefully and be sure to answer the question they asked you, not the question you WANTED them to ask you.
Question 19.
Which of the following beta2-adrenergic effects would the emergency nurse anticipate finding in an overdose of a medication in this class?
(a) Increased sweating
(b) Decreased heart rate
(c) Increased tidal volume
(d) Decreased blood sugar
Answer:
(c) Increased tidal volume
Rationale:
Because beta2 receptors are associated with lung function, the most likely symptom to be anticipated would be increased tidal volume. Adrenergic effects refer to the compensatory responses of the sympathetic system; commonly referred to as the flight- or-fight response. These effects are generated through specific receptor sites throughout the body and include alpha receptors and beta receptors. The beta receptors are differentiated into betaj, beta2, and beta3. The beta! receptors are almost entirely located in the heart and focus on stimulation of cardiac output such as increasing heart rate, contractility, and automaticity.
The beta2 receptors are almost, but not completely, located in the lungs and focus on increasing pulmonary function such as increased respiratory rate and bronchodilation, which increases tidal volume. The beta3 receptors are not completely understood, but have been found in the gallbladder, urinary bladder, and brown adipose tissue and appear to be associated with lipolysis (breakdown of fat for energy), thermogenesis, and bladder relaxation. Although increased sweating would be an adrenergic effect, it is not regulated by the beta2 recep-tors. Both decreased heart rate and decreased blood sugar are associated with the cholinergic (parasympa-thetic) system and would not be likely responses in this situation.
Just a little extra pathophysiology to help your understanding of the adrenergic system. Remember to take from these rationales what you need or can „ handle and then leave the rest for another time. Learning is a lifelong process ana will not be com-pleted in a single sitting.
Question 20.
A patient is brought to the emergency department after a suspected ovefdose. The patient has altered perceptions of reality^ shallow respirations, dysarthria, and ataxia. The emergency nurse suspects which of the following to be the causative substance?
(a) Phencyclidine (PCP)
(b) Cannabis (Marijuana)
(c) Gamma-hydroxybutyrate (GHB)
(d) Lysergic acid diethylamide (LSD)
Answer:
(c) Gamma-hydroxybutyrate (GHB)
Rationale:
Gamma-hydroxybutyrate (GHB) is a sedative/hypnotic which induces hallucinations and euphoria as well as more commonly associated sedation effects such as respiratory depression. Phencyclidine (PCP), cannabis (marijuana), and lysergic acid diethylamide (LSD) produce hallucinations and coordination impairment but act as stimulants, rather than as depressants on the respiratory drive.
Question 21.
A patient with a history of alcohol abuse comes to the emergency department 12 hours after last drinking complaining of nausea and palpitations. The patient is tremulous and reports feeling anxious. Which medication can the nurse anticipate being the first ordered in this scenario?
(a) Thiamine (vitamin BJ
(b) Lorazepam (Ativan)
(c) Phenytoin (Dilantin)
(d) Haloperidol (Haldol)
Answer:
(b) Lorazepam (Ativan)
Rationale:
Benzodiazepines such as lorazepam are first-line therapy for the treatment of acute withdrawal syndrome and the prevention and treatment of seizure activity and delirium tremens. Placebo-controlled trials have demonstrated that henytoin is ineffective for the secondary prevention of alcohol withdrawal seizures. In addition, phenytoin use has been attributed to respiratory depression in high doses or when combined with alcohol.
For the treatment of Wernicke’s encephalopathy and thiamine deficiency, the administration of thiamine is recommended; however, this would not be a first-line therapy. Haloperidol has also been used to control the psychiatric symptoms of alcohol withdrawal, including combativeness, delirium, and anxiousness. However, it has been shown to be significantly less effective than benzodiazepines in preventing delirium and can cause torsades de pointes because of prolongation of the QT interval.
Remember, certain words and phrases carry specific meaning on the examination. When you encounter words such as priority, primary, or initial interventions, it should lead you to think “Which will actively stop the dying process.” This is usually based on stopping the symptoms that are truly harming the patient. In the given example, we see that all four medications are appropriate for this patient, but only Ativan stopped the immediate life-threatening complication. I hope this helps!
Question 22.
The following rhythm strip is seen on the monitor of a patient who just arrived in the emergency department with a possible ingestion.
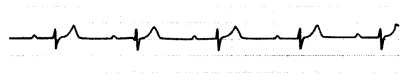
Which of the following medications most likely caused this rhythm change?
(a) Hydroxyzine (Vistaril)
(b) Nifedipine (Procardia)
(c) Nortriptyline (Aventyl)
(d) Ephedrine (Primatene)
Answer:
(b) Nifedipine (Procardia)
Rationale:
This rhythm strip demonstrates both a first-degree heart block and bradycardia. Calcium channel blockers such as nifedipine (Procardia) are known to cause heart blocks and bradycardia. Hydroxyzine (Vistaril) is an antihistamine drug and will cause tachycardia rather than bradycardia. Nortriptyline (Acentyl) is a tricyclic antidepressant and leads to several toxic cardiac effects including tachy- cardic dysrhythmias and arrest, but is not traditionally associated with heart blocks and bradycardia. Ephed- rine (Primatene) is a sympathomimetic and would cause an increased, rather than a decreased, heart rate and is not associated with heart blocks.
Remember that basic rhythm interpretation is fair game on the examination! Remember the five or so basic rhythms you need to know when you go to an ACLS or PALS course? Those are the same ones you need to know for this examination most of the time. Occasionally there will be a tougher rhythm that is very specific to an individual drug or condition, but such cases are the exceptions.
Question 23.
Two hours after taking an overdose of acetaminophen (Tylenol), a patient arrives in the emergency department. Based on the nomogram for acute ingestion, when can the emergency nurse expect to draw a blood acetaminophen level?
(a) Immediately
(b) In 1 hour
(c) In 2 hours
(d) In 4 hours
Answer:
(c) In 2 hours
Rationale:
Based on the nomogram for acute ingestion, serum acetaminophen levels should be drawn 4 hours after ingestion. Because the ingestion occurred 2 hours before arrival, the level should be drawn 2 hours after arrival to reach the 4-hour level. Levels drawn sooner or later would not reflect the peak acetaminophen level. An acetaminophen level greater than 150 g/mL 4 hours after ingestion indicates toxicity.
Question 24.
The emergency nurse knows that erethism, associated with mercury toxicity, primarily affects which of the following systems?
(a) Neurologic
(b) Genitourinary
(c) Cardiovascular
(d) Gastrointestinal
Answer:
(a) Neurologic
Rationale:
Erethism, also known as Mad Hatter Disease, is a neurologic complication of mercury toxicity. Symptoms associated with erethism include irritability, excitability, excessive shyness, and insomnia. Although acute or chronic symptoms of mercury toxicity may include other symptoms, the classic triad is tremors, gingivitis, and erethism. Erethism is not associated witiT the genitourinary, cardiovascular, or gastrointestinal systems.
Okay, I admit it! This was just me sneaking in a fun fact. Not sure it is the more relevant piece of information for the examination, but I did not know it and when I stumbled across it while researching this chapter, I wanted to share it. If you did not know it, do not feel bad; neither did I! But now you know that mercury poisoning causes neurologic manifestations! Just in case!
Question 25.
A child is brought to the emergency department after ingestion of prenatal vitamins. The child is noted to have symptoms consistent with an iron toxicity greater than 20 mg/kg and chelation therapy with deferoxamine (Desferal) is administered by continuous intravenous infusion. Which of the following symptoms would indicate the infusion should be discontirfued?
(a) Hypotension
(b) Hematochezia
(c) Return of yellow urine .
(d) Resolution of abdominal pain
Answer:
(c) Return of yellow urine .
Rationale:
Indication for discontinuation of deferox-amine therapy in iron toxicity is when urine color nor-malizes. The chelation process of deferoxamine on iron leads to a pink or orange-red urine. Therefore, once urine returns to a clear yellow color, the therapy is considered complete. Hypotension and hematochezia are symptoms of phase one of iron toxicity and would not be indicative of successful treatment. Likewise, resolution of abdominal pain is an expected event during the second phase of iron toxicity and would, therefore, not be a good indicator of completion of chelation therapy.
Iron toxicity often presents in three phases, each with its own set of symptoms. The first phase, often presenting within 0 to 2 hours of ingestion/exposure, is associated with hypotension, hematemesis (bloody emesis), hematochezia (bloody stool), and abdominal pain. The second phase, often presenting between 2 and 48 hours after ingestion, is associated with a resolution of gastrointestinal symptoms. The third phase, often seen approximately 48 to 96 hours after ingestion, is associated with metabolic acidosis, coagulopathy, hemorrhage, shock, and hepatic and renal failure. Some report this second phase as "in between phase one and two." Just remember there is a period of time where the patient seems to be “Okay. ”
Question 26.
A patient is brought to the emergency department 15 minutes after ingesting a full bottle of the tricyclic antidepressant amitriptyline (Elavil). Which of the following interventions would NOT be utilized in this scenario?
(a) Gastric lavage
(b) Syrup of ipecac
(c) Activated charcoal
(d) Electrocardiogram (ECG)
Answer:
(b) Syrup of ipecac
Rationale:
Syrup of ipecac is contraindicated in tricyclic antidepressant overdose. Because rapid deterioration with cardiovascular collapse and seizures can occur, inducing emesis may lead to airway compromise from aspiration. Gastric lavage could be ordered with endotracheal intubation with proper cuff inflation and mechanical ventilation. Administration of activated charcoal may be delayed. A baseline ECG may be ordered. The patient should be placed on a cardiac monitor because dysrhythmias and cardiac conduction delays are common.
Question 27.
Ingestion of the leaves of which of the following plants would be associated with buccal lesions and throat irritation?
(a) Coca
(b) Cannabis
(c) Potato plants
(d) Philodendron
Answer:
(d) Philodendron
Rationale:
Oxalic acid is a skin irritant contained in the leaves of several plants including dieffenbachia, philodendron, and rhubarb. Oxalic acid can cause blisters and ulcerations to the mucous membranes of the mouth and throat when chewed. This irritation can lead to throat swelling, dysphagia, and respiratory distress. Leaves of the coca plant will cause numbness and anesthesia to the mouth when chewed, but then lead to stimulant effects as they are absorbed in the body.
Cannabis leaves contain nearly 500 active chemicals including tetrahydrocannabinol (THC) and have little effect on the buccal cavity when chewed, but they are associated with alterations in perception, increased' appetite, and anxiety and several other mood-associated effects. Leaves of some potato plants have an anticholinergic effect including hyperthermia and hallucinations, dry skin, mental excitation, and tachycardia.
Although it is not always the most common situation we see in our practice, it is far from uncommon for patients to present with ingestions of nonphar- macologic agents such as plants or solutions. There is no chance that we will know every possible toxic substance out there, but see if you can add a few of them to your repertoire here and there.
Question 28.
During the past 3 hours, several adult patients have presented to the emergency department with similar symptoms, which include vomiting, severe diarrhea, and abdominal cramps. Each patient reports eating at the same restaurant the previous night with no other commonalities identified. Based on this information, the triage nurse suspects that these patients were exposed to which type of food poisoning?
(a) Botulism
(b) Listeriosis
(c) Salmonella
(d) Staphylococcal
Answer:
(c) Salmonella
Rationale:
Signs of Salmonella poisoning appear from 12 to 24 hours after the ingestion of contaminated food. Common foods contaminated with Salmonella include milk, custards and other egg dishes, salad dressings, sandwich fillings, polluted shellfish, and poultry. Staphylococcal symptoms appear suddenly 1 to 6 hours after exposure and include headache and fever. Listeriosis occurs 3 to 21 days after exposure, and, in addition to diarrhea, fever, and headache, it may result in pneumonia, meningitis, and endocarditis. Botulism does not usually cause diarrhea. The symptoms of botulism include bilateral facial weakness, dysphagia, eyelid ptosis (drooping), blurry vision, and pa¬ralysis as well as gastrointestional manifestations.
Question 29.
Urine alkalization is most likely to be considered in patients who overdose on which of the following types of medications?
(a) Sulfonylureas
(b) Cephalosporins
(c) Calcium channel blockers
(d) Phosphodiesterase inhibitors
Answer:
(a) Sulfonylureas
Rationale:
Alkalization of urine is considered effective for overdoses involving phenobarbital, sulfonylureas, form-aldehyde, and salicylates. Weak acids may become ion trapped and excreted in the urine when urine pH is increased with controlled administration of alkalizing agents. Alkalinizing the urine does not promote excretion of cephalosporins, calcium channel blockers, or phosphodiesterase inhibitors.
Question 30.
A patient with a long history of benzodiazepine use is brought to the emergency department for a reported overdose of approximately 35 tablets of lorazepam (Ativan). The patient is unresponsive and mildly cyanotic with the following vital signs:
Blood pressure 88/64 mm Hg Respirations 7 breaths/minute, shallow and regular Heart rate 52 beats/minute, strong and regular Pulse oximetry 86% on room air. The emergency nurse considers the following interventions. Which one would be the highest priority in this situation?
(a) Infuse 20 mL/kg isotonic crystalloid bolus.
(b) Administer flumazenil (Romazicon) IV push.
(c) Deliver ventilations at 14 breaths/minute.
(d) Initiate chest compressions at 100/minute.
Answer:
(c) Deliver ventilations at 14 breaths/minute.
Rationale:
Because of the phenomenon explained here, respiratory depression and arrest is the highest priority with an acute benzodiazepine overdose. Of the options presented, mechanical ventilations would be the highest priority because they are both ‘immediate and therapeutic, that is to say, the action directly stops the dying process in the patient. Benzodiazepines, such as lorazepam (Ativan), act as, agonists for the gamma-aminobutyric acid (GABA) receptor site and decrease neuronal excitability.
The primary effect of benzodiazepines is antianxiety and hypnotic effects; however, in higher doses, this increased resistance to nerve impulse conduction translates into a higher threshold of resistance to muscle firing as well. Therefore, benzodiazepines also are used to inhibit seizure activity by making muscles less able to contract because of an increased resistance threshold. In a toxic overdose setting, the antianxiety and hypnotic properties are not the primary concern, but rather the inhibition of muscle firing; specifically, in voluntary skeletal muscles, but with limited effect on vascular and cardiac smooth muscles.
Flumazenil V(Romazicon) is the antagonist for benzodiazepines and would act to reverse the effects of the drug within 1 to 3 minutes; however, there are multiple problems with choosing this as the first intervention in this situation. The obvious problem is that flumazenil would take 1 to 3 minutes to work, during which time the patient is still hypoventilated and hypoperfused; not optimal. Also, this patient is described as having chronic benzodiazepine use, which would impart tolerance to the medication.
Flumazenil is contraindicated in patients with chronic benzodiazepine use because of an increased risk of rebound sedation as well as of intractable seizure activity following rapid administra-tion of the reversal agent. In chronic tolerance cases, the recommended weaning of benzodiazepines with flumazenil is over the course of weeks to months and not recommended for rapid reversals. Chest compres-sions and intravenous fluid boluses are not incorrect in this situation, but they do not serve to correct the primary life-threatening problem, which is respiratory depression; therefore, they would not take precedence over ventilations.
Do not hate me for that one! I know it was probably frustrating. Let me explain a bit about why this type of question is so important and why it is an analysis-style question rather than intervention. Many times on the examination, you will be presented with four good choices! They are ■ sometimes all appropriate in the given situation. The question becomes not which one will I do, but which one will I do first to best provide therapeutic and immediate life-saving interventions.
As explained, there are multiple choices that are valid and if you stop at the first choice that is appropriate, you will get the question incorrect. When you see a question that has multiple “good" answers, ask yourself what is the crisis in this situation. That is, what is actually harming the patient and what will best correct that. It may be best because it is most readily available, targets the specific cause of harm in the patient, or does not create secondary complications. They are not always , easy, but they will show up both on the examination and in your emergency department!
Question 31.
Which of the following medications is most commonly used to treat anticholinergic delirium?
(a) Naloxone (Narcan)
(b) Lithium
(c) Physostigmine (Antilirium)
(d) Atropine
Answer:
(c) Physostigmine (Antilirium)
Rationale:
Physostigmine acts by interfering with the metabolism of acetylcholine; therefore, increasing the cholinergic effects of acetylcholine in the body and reversing anticholinergic delirium. Remember that physostigmine must be given slowly because of the side effects! Naloxone is used in opiate overdose. Lithium is - not used as an antidote in any scenario. Atropine is used in beta-adrenergic blocker, calcium channel blocker, and organophosphate and physostigmine poisonings.
Question 32.
A chronic alcoholic patient presents to the ED with ethanol intoxication. Which of the following laboratory results is most consistent with this scenario?
(a) Hyperkalemia
(b) Hyponatremia
(c) Hyperglycemia
(d) Hypomagnesemia
Answer:
(d) Hypomagnesemia
Rationale:
The most common cause of hypomagnesemia is alcoholism and is commonly associated with poor dietary intake, diarrhea-induced hypophosphatemia that drives down magnesium levels, and metabolic acidosis and magnesiuric effects which both lead to low levels of serum magnesium. Potassium levels are usually not elevated with chronic alcoholism. Alcohol is a known diuretic and is more likely to cause hypernatremia as opposed to hyponatremia. Because of liver damage and lack of glycogen stores, chronic alcoholics are more likely to be hypoglycemic than hyperglycemic.
Question 33.
A patient presents to the triage desk and complains of arthritis pain and tinnitus. The patient has been taking nonprescription medications for pain relief. Based on the chief complaints, the emergency nurse should ask about the use of which of the following medications?
(a) Naproxen (Aleve)
(b) Ibuprofen (Motrin)
(c) Acetaminophen (Tylenol)
(d) Acetylsalicylic acid (Aspirin)
Answer:
(d) Acetylsalicylic acid (Aspirin)
Rationale:
Tinnitus is the most common central nervous system sign of mild adlicylate toxicity. Patients taking medications that contain salicylates at doses prescribed for arthritis may develop mild toxicity (salicylism). Ibuprofen usually causes GI upset and blurred vision. Ac-etaminophen toxicity causes liver failure. Naproxen may cause Gl bleeding without other GI symptoms and may also mask infection.
Question 34.
While administering dimercaprol (British anti-Lewisite) to a patient, the emergency nurse knows which of the following is optimal regarding administration?
(a) Intramuscular injection
(b) Oral dose with 16 ounces of water
(c) Intravenous infusion over 60 minutes
(d) Rapid intravenous infusion over 5 minutes
Answer:
(a) Intramuscular injection
Rationale:
The only route that dimercaprol may be safely administered is via the intramuscular route. Di-mercaprol (British anti-Lewisite) is a chelating agent used to treat toxicity with select heavy metals including arsenic, lead, gold, and mercury. This medication is only effective in parenteral routes and is not effective orally. Dimercaprol is contraindicated in iron, selenium, silver, uranium, and cadmium toxicities because of the toxic complex that dimercaprol forms with these metals. Owing to the toxic interaction with iron, dimercaprol is contraindicated via the intravenous route, either slow or rapid infusion, because it chelates heme molecules in the red blood cells leading to life-threatening anemias in some cases.
Question 35.
A nondiabetic patient arrives in the emergency department after an intentional overdose of the biguanide antihyperglycemic agent metformin (Glucophage). The emergency nurse would anticipate which of the following finding if a toxic amount was taken?
(a) Bradycardia
(b) Hypoglycemia
(c) Metabolic acidosis
(d) Fruity odor to breath
Answer:
(c) Metabolic acidosis
Rationale:
Metabolic acidosis would be a more likely finding in this situation. The antidiabetic medication class of biguanide, of which metformin is a member, acts more prominently by inhibiting liver glucose production rather than, as other antidiabetic medications do, decreasing cellular resistance of insulin. Therefore, biguanides only drop blood sugar to the euglycemic threshold of the body and are not commonly
Question 36.
A patient who is actively hallucinating is brought to the emergency department by friends. They say that the patient used either D-lysergic acid diethylamide (LSD) or phencyclidine (PCP) at a concert. During triage, which assessment finding indicates that the patient may have ingested PCP?
(a) Paranoia
(b) Nystagmus
(c) Dilated pupils
(d) Altered mood
Answer:
(b) Nystagmus
Rationale:
Nystagmus would be the most compelling symptom presented to indicate PCP was ingested rather than LSD. Phencyclidine is an anesthetic with severe psychological effects. It blocks the reuptake of dopamine and directly affects the midbrain and thalamus. Bidirectional nystagmus and ataxia are common physical findings of PCP use. Dilated pupils are evidence of LSD ingestion. Paranoia and altered mood occur with both PCP and LSD ingestion.
Question 37.
For a patient with a suspected cholinergic agent exposure, which of the following symptoms would the emergency nurse consider the highest priority?
(a) Diaphoresis
(b) Tachycardia
(c) Flushed skin
(d) Constricted pupils
Answer:
(a) Diaphoresis
Rationale:
Diaphoresis would be the most concerning symptom in this situation because it indicates the level of toxicity of the cholinergic agent as well as having a primary impact on gas exchange through fluid produc-tion in the lungs. Cholinergic agents lead to symptoms of the parasympathetic system, which include vasodilation, decreased serum glucose, decreased cardiac function (including bradycardia, conduction blocks, and decreased contractility), bradypnea, and bronchoconstriction.
However, because of the relative strength imbalance between the adrenergic (sympathetic) receptors and the cholinergic (parasympathetic) receptors in the beta! and beta2 sites, lability in heart rate and respirations are often seen. In addition, with cholinergic toxicity, the effects of the muscarinic and nicotinic pathways, which have primary control over fluid mobilization in the body, we find, that excessive fluid production from all fluid-producing cells often occurs.
Tachycardia in this situation would be a sympathetic reflex as part of compensation and not directly life threatening. Flushed skin would indicate vasodilation, which may have a secondary impact on vascular resistance and blood pressure; but it would be a circulatory concern and would n3t take priority over the airway obstruction of fluid production. Constricted pupils would be a symptom of parasympathetic stimulation and expected in this situation, although they do not pose an immediate life-threatening concern.
Remember that cholinergic crises are “wet." All bodily fluids are sent into overdrive!
Question 38.
After an ingestion, a patient develops acute blindness and emergency treatment is provided. Ingestidh of which of the following would most likely be associated with this scenario?
(a) Hydraulic brake fluid
(b) Camping stove fuel
(c) Skin cleanser
(d) Mouthwash
Answer:
(b) Camping stove fuel
Rationale:
Visual disturbances and blindness are asso-ciated with toxicity of methanol. Methanol is found in several chemicals including windshield washer fluid, canned fuels, and alternative automobile fuel. Ethylene glycol, another alternative alcohol, leads to acidosis and renal failure. Ethylene glycol is often found in solvents and as an antifreeze agent in automotive fluids such as hydraulic brake fluid.
Isopropanol, the least toxic of the alternate alcohols, metabolizes quickly into acetone and, although toxic and able to cause profound central nervous system and respiratory depression, is lost in re-spiratory expressions rapidly and can be managed with supportive care. Isopropanol is found in disinfectants and skin cleansers.
Ethanol is safe for human consump-tion and is nontoxic in moderate doses. Ethanol, much like isopropanol, can be an effective solvent and is used in certain cleansers and tinctures. Owing to ethanol’s nontoxic nature, it is often found in products intended for internal use, such as mouthwash. If ingested in small amounts, it is unlikely to cause harm.
Another place to find methanol is moonshine!
Question 39.
A patient presents to the emergency department with a recent history of overuse of oral antacids. The emergency nurse would anticipate which of the following laboratory findings?
(a) Hyperkalemia and hypercalcemia
(b) Hypocalcemia and hypomagnesemia
(c) Hypercalcemia and hypophosphatemia
(d) Hypermagnesemia and hyperphosphatemia
Answer:
(c) Hypercalcemia and hypophosphatemia
Rationale:
The most likely findings would be hyper-calcemia and hypophosphatemia. Oral antacids are comprised of one of four primary active ingredients: alu-minum hydroxide, magnesium hydroxide, sodium bicar-bonate, and calcium carbonate. In most liquid antacids, such as Mylanta or Maalox, the active ingredient is aluminum hydroxide, which acts by deactivating the gastric enzyme pepsin and by increasing the mucosal lining of the stomach; but it has a side effect of binding to phosphates in the gastrointestinal tract and causing hypophosphatemia. The other common liquid antacid is milk of magnesium, which contains magnesium hydroxide.
Magnesium hydroxide works by binding in stomach acid to produce magnesium chloride, thereby reducing acid directly but also producing a biologically available magnesium compound in the process. The side effects of magnesium hydroxide are diarrhea and hypermagnesemia. One of the solid antacids containing sodium bicarbonate is Alka- Seltzer or baking soda and it acts by binding to gastric hydrochloric acid to reduce pH; but it has a side effect of producing sodium, which can be freely absorbed to elevate serum sodium levels.
The most common oral ant¬acid is calcium carbonate, such as in Turns, and this most potent usable antacid completely neutralizes available stomach acids. However, approximately one-third of the calcium gets absorbed into the bloodstream, causing el¬evations in serum calcium, and binds to phosphate ions, causing hypophosphatemia.
Therefore, regardless of the agent used, the following effects are common (number of agents that cause each is listed in parenthesis): metabolic alkalosis (4), hypercalcemia (2), hypophosphatemia (2), hypernatremia (1), hypermagnesemia (1) or hypomagne-semia (1), and hypokalemia (3). It is unlikely for this patient to have hyperkalemia because magnesium, calcium, and sodium bicarbonate all have a reducing effect on serum potassium levels. Hypercalcemia, rather than hypocalcemia, is a common effect. Although hypermagnesemia is possible, none of the agents are known to cause hyperphosphatemia but rather cause hypophosphatemia.
This was a fun fact for you. We all know the basics of antacids, but did you know how they each work? I cannot say I had a comprehensive understanding of them myself before I researched them extensively so do not feel a bit of shame if you did not either. Again, my goal is to raise the bar for you and push you to take your understanding to a new level.
Question 40.
A patient is treated for a cholinergic exposure. Which of the following manifestations would indicate successful treatment?
(a) Miosis
(b) Dry skin
(c) Tachycardia
(d) Hypotension
Answer:
(b) Dry skin
Rationale:
Drying of the skin would be an indication that the cholinergic toxicity effect has been resolved. This toxidrome often causes lability, as either elevated or de-creased heart rate, respirations, and blood pressure, and is not known to directly change body temperature. Miosis is a symptom of cholinergic exposure; therefore, its presence would not indicate successful treatment. Tachycardia and hypotension may be symptoms of cholinergic crisis; however, the treatment of cholinergic exposure would not intentionally create an abnormally high heart rate or an abnormallylow blood pressure. Tachycardia and hypotension in this case would indicate that patient was overtreated and a new problem, potentially anticholinergic crisis, was created.
Question 41.
A patient is being treated for an intentional overdose of metformin (Glucophage). Which of the following would indicate that treatment has been successfully completed?
(a) Venous pH of 7.29
(b) Blood glucose level of 60 mg/dL
(c) Lactate level of 1.1 mmol/L
(d) Urine output of 3.5 mL/kg/hour
Answer:
(c) Lactate level of 1.1 mmol/L
Rationale:
A lactate level of 1.1 mmol/L would be in the standard reference range and indicate the lactic acidosis caused by the toxicity has been resolved. Remember that biguanide antihyperglycemic agents, including metformin (Glucophage), act by inhibiting liver glucose production rather than, as other antidiabetic medications do, by decreasing cellular resistance of insulin. Therefore, biguanides only drop blood sugar to the euglycemic threshold of the body and are not commonly associated with hypoglycemic emergencies. They do, however, inhibit liver breakdown of lactate molecules and lead to metabolic lactic acidosis in overdoses.
A venous pH of 7.29 would indicate an acidotic state and would not indicate successful treatment in this situation. Because biguanide overdose is not normally associated with hypoglycemia, a blood glucose level of 60 mg/ dL would not necessarily indicate successful treatment. Although increased urine output may be present in a patient who is hyperglycemic, which is likely in a patient who has access to antidiabetic medications, it would be indicative of the condition of hyperglycemia, rather than the toxic effects of metformin (Glucophage) and would not be associated with effective treatment of the toxicity.
Question 42.
The emergency nurse expects a patient with hypotension, widened QRS complex tachycardia, dry, hot skin, respiratory depression, and decreased level of consciousness to have most likely overdosed on which of the following substances?
(a) Lorazepam (Ativan)
(b) Amitriptyline (Elavil)
(c) Carbidopa/levodopa (Sinemet)
(d) Benzoylmethylecgonine (cocaine)
Answer:
(b) Amitriptyline (Elavil)
Rationale:
Patients with toxicity from tricyclic anti-depressants may present with cardiotoxicity (wide- complex tachydysrhythmias), anticholinergic effects (hyperthermia, dry skin, tachycardia), and anti-ad-renergic effects (vasodilation, hypotension). Tricyclic antidepressants (modernly referred to as cyclic antide-pressants) have three primary effects that lead to unique symptoms in toxic exposures. The first two effects are due to an inhibition of norepinephrine and serotonin reuptake, which, in therapeutic levels, increases synaptic firing and stimulates elevations in mood, memory, and alertness.
At toxic levels, serotonin inhibits norepineph-rine release from adrenergic nerves leading to beta2- adrenergic blockade as well as generates increased levels of nitrous oxide from endothelial cells, which leads to alpha-adrenergic antagonist effects including severe va-sodilation and hypotension. The second mechanism seen in toxic tricyclic exposure is a reduction of sodium fast channels in cardiac myocytes, leading to delayed cardiac conduction and widening of QRS complexes. The third mechanism of action during toxicity is the blockade of cholinergic and histaminergic receptors, which manifests as the anticholinergic effects of lack of fluid mobilization (dry skin, dry mouth, and prevention of thermodissipa-tion effects of diaphoresis).
Have you seen the secret yet? The key to understanding toxicology is not in memorizing every possible presentation for every individual agent. It is knowing the toxidromes and the key features to each one. It is with this knowledge that Poison Centers are able to so effectively identify the probable toxic agents and recommend treatment. Fust yourself! Know the core content of the toxidromes and apply the presenting symptoms to that.
Question 43.
Signs and symptoms of cyanide exposure are best demonstrated by which of the following?
(a) Hallucinations, hypotension, tachycardia.
(b) Bradycardia, odor of bitter almonds, pH 7.62.
(c) Bradypnea, decreased mental status, Sp02 97%.
(d) Cyanosis, elevated serum lactate level, tachypnea.
Answer:
(c) Bradypnea, decreased mental status, Sp02 97%
Rationale:
Bradypnea, decreased mental status, and normal pulse oximetry would be expected in this situ-ation. Cyanide affects the body primarily by attaching to metalloenzymes found inside cells and inactivating them by preventing cytochrome oxidase. This blockade of a primary enzymatic reaction within cells prevents mito-chondria from performing oxidative phosphorylation and prevents it from performing aerobic cellular respiration.
This essential process forces affected cells into anaerobic metabolism and dramatically increases lactic acid production at the cellular level. It is this key feature that creates a set of very specific symptoms including hypotension, bradycardic dysrhythmias, respiratory depression/arrest, decreased mental status, seizure, and metabolic acidosis, but maintains an adequate serum oxygen level (because oxygen is carried by hemoglobin and stored on myoglobin but cannot be used by cells).
It is the relatively normal oxygen levels which create the clinical confusion, because they produce normal oxygen saturations and normal skin color (noncyanotic) while the patient has all the other signs or hypoxia. Tachycardia, serum alkalosis, and cyanosis would not be expected in cyanide exposure.
Question 44.
The emergency nurse may anticipate intravenous thiamine to be given for which of the following purposes?
(a) Treatment of Addison’s crisis
(b) Management of pernicious anemia
(c) Prevention of Wernicke’s encephalopathy
(d) Reducing the international normalized ratio (INR)
Answer:
(c) Prevention of Wernicke’s encephalopathy
Rationale:
Thiamine deficiency is known to contribute to Wernicke’s encephalopathy and Korsakoff’s syndrome; therefore, administration of thiamine is an expected treatment for both of these conditions. Addison’s crisis is caused by insufficient adrenal hormones and is treated with intravenous hydrocortisone (Solu-Cortef) or anothercorticosteroid. Pernicious anemia is caused by a deficiency of vitamin B12 and is treated with subcutaneous vitamin B12 injections, not thiamine which is vitamin Bj. Elevated inter¬national normalized ratio (INR) is treated with infusions of fresh frozen plasma and cryoprecipitate as well as vitamin K.
Question 45.
During initial care of a patient with acute lead toxicity, the emergency nurse knows that which of the following findings is most associated with this exposure?
(a) Serum pH 7.48
(b) Hemoglobin 8.2 g/dL
(c) Heart rate 36 beats/minute
(d) Respirations 10 breaths/minute
Answer:
(b) Hemoglobin 8.2 g/dL
Rationale:
A mild anemia, such as a hemoglobin level of 8.2 g/dL, may be likely with lead toxicity. Common symptoms of acute lead toxicity include neurologic changes (mood lability, tremors, concentration impairment, memory loss), renal failure, anemia, and gastrointestinal upset (diarrhea, vomiting, nausea, and anorexia). Metabolic acidosis, rather than alkalosis, would be expected because of renal failure and an increase in positive ions in the blood. Lead toxicity tends to create a stressed state in the body due to gastrointestinal losses and renal failure; therefore, tachycardia, rather than Bradycardia, and tachypnea, rather than bradypnea, would be more likely.
Question 46.
A comatose adult with a suspected barbiturate overdose is brought to the emergency department. If gastric lavage is ordered, which of the following would indicate correct performance of the intervention?
(a) Instill 300 mL of fluid.
(b) Insert an 18 French gastric tube.
(c) Administer activated charcoal before lavage.
(d) Place patient in a right lateral Trendelenburg position.
Answer:
(a) Instill 300 mL of fluid.
Rationale:
An adult receiving gastric lavage should have 200 to 300 mL of fluid instilled at a time. The fluid should then be removed by gravity or gentle suction. Larger amounts may cause the pyloric sphincter to open and force the toxins into the small intestine. Smaller amounts may not distend the stomach enough to open the rugae and be able to clear the pill fragments out of these folds. The patient should be placed in the left lat-eral Trendelenburg position. A large-bore gastric tube (22 to 36 French) should be used, with the average size for an adult being 32 to 36 French. Activated charcoal should be instilled after lavage has been completed; otherwise, it would be washed out during the lavage process.
Question 47.
The classic triad of symptoms associated with an opiate overdose is respiratory depression, central nervous system depression, and:
(a) Miosis.
(b) Diuresis.
(c) Tachycardia.
(d) Hyperthermia.
Answer:
(a) Miosis.
Rationale:
The classic triad of symptoms associated with an opiate overdose is respiratory depression, central nervous system depression, and miosis (constricted pupils). Alterations in urinary output, including diuresis, are not associated with opiate overdoses. Bradycardia, as opposed to tachycardia, and hypothermia, as opposed to hyperthermia, are associated with opiate overdoses.
Question 48.
A patient with a cocaine overdose presents to the emergency department with a temperature of 105.1°F (40.6° C). The emergency nurse anticipates which of the following interventions to be optimal in this situation?
(a) Insertion of rectal ibuprofen (Advil)
(b) Application of ice packs to the groin and axilla
(c) Administration of oral acetaminophen (Tylenol)
(d) Initiation of intravenous Dantrolene (dantrolene sodium)
Answer:
(b) Application of ice packs to the groin and axilla
Rationale:
Active external cooling methods, such asapplication of ice packs, are much more likely to be effective than pharmacologic interventions which fo-cus on reduction of the set point. Hyperthermia in sym-pathomimetic overdoses is driven primarily by excessive thermogenesis because of increased activity and muscle firing rather than through hyperpyrexia and endocrine activity. Administration of ibuprofen or acetaminophen is unlikely to be effective in reducing the temperature of this patient.
Dantrolene sodium, a postsynaptic muscle inhibitor, may be effective in blocking further tempera-ture generation by inhibiting muscle firing, although it will do little to reduce the current temperature and, therefore, would not take precedence over active cooling measures in this patient.
Dantrolene, which works on the skeletal muscles, can have some serious hepatotoxic side effects and is not usually the first line of defense for disease processes such as that listed in question 48. The most common reason to use this medication is in. a situation of malignant hyperthermia that is most often seen during surgery. However, be aware that the use of Succinylcholine (Anectine) can,also cause malignant hyperthermia!
Question 49.
While caring for a patient with carbon monoxide poisoning, which of the following is the most likely cause of the patient’s confusion?
(a) Airway obstruction
(b) Impaired gas exchange
(c) Oxygen delivery failure
(d) Arrested cellular metabolism
Answer:
(c) Oxygen delivery failure
Rationale:
The primary toxic effect of carbon monoxide (CO) is competitive binding to hemoglobin, which prevents the carrying and delivery of oxygen to cells; therefore, the primary cause of confusion would be oxygen delivery failure. Carbon monoxide has no direct impact on airway patency or gas exchange in the lung fields. Although there is some evidence that carbon mon-oxide may bind to cardiac myoglobin and have increased cardiovascular metabolism impairment, the toxicity much more directly retarding cellular metabolism is cyanide.
Once you have the pathophysiology of a toxicity in your grasp, you find that questions become a lot more straightforward. Take it slow and add what you can each time you get the opportunity. Ask questions when you see new or unfamiliar cases in your practice. Examples will always help you solidify your understanding!
Question 50.
During the treatment of a patient who drank antifreeze, which of the following would be an expected outcome?
(a) Declining serum methanol level
(b) Increasing serum ethanol level
(c) Rising potassium level
(d) Decreasing serum calcium, level
Answer:
(b) Increasing serum ethanol level
Rationale:
The most likely outcome in this situation would be rising ethanol levels. The dehydrogenase sites are saturated when ethanol levels are 100 mg/dL or above; therefore, increasing serum ethanol levels would be an expected outcome of therapy. Antifreeze contains ethylene glycol which, when metabolized by the liver, produces toxic metabolites. Medical therapy for ethylene glycol ingestion includes blocking the metabolism of the drug by saturating alcohol dehydrogenase sites with ethanol to prevent the production of toxic metabolites as well as administration of sodium bicarbonate for acidosis.
Ethylene glycol, rather than methanol, is a more common ingredient in antifreeze, so declining methanol levels would be less likely associated with this treatment; however, because treatment involves binding to the dehydrogenase sites, ttie levels of the alternate alcohol (ethylene glycol or methanol) should remain the same if treatment is successful. Ethylene glycol toxicity leads to hypocalcemia and hyperkalemia through chelation of calcium by oxalates and metabolic acidosis, respectively. Therefore, treatment of this toxicity should lead to in-creasing calcium levels and decreasing potassium levels.
Question 51.
A patient who ingested the tricyclic antidepressant doxepin (Sinequan) is brought to the emergency department. In addition to supportive measures, the nurse administers sodium bicarbonate IV push. Monitoring for which of the following would best indicate treatment had its intended effect?
(a) Acid-base status
(b) Neurologic status
(c) Respiratory status
(d) Cardiovascular status
Answer:
(d) Cardiovascular status
Rationale:
The primary effect of administering sodium bicarbonate is to reverse QRS prolongation and hypo-tension. The actual mechanism of action is not well understood, but it may inhibit binding of tricyclic an-tidepressants to the myocardial sodium channels. The toxic effects of tricyclic antidepressants include cardio- toxicity (prolongation of conduction leading to dysrhyth-mias and arrest), adrenergic blockade (alpha-receptor blockades leading to hypotension), and anticholinergic stimulation (including dry, flushed skin, hyperthermia, tachycardia).
Management of tricyclic antidepressant overdose is focused on reversing cardiotoxicity. Seizures may occur, but administration of benzodiazepines, rather than sodium bicarbonate, will suppress this symptom. The administration of sodium bicarbonate does not di-rectly affect respiratory status. Acid-base status should also be monitored, but effectiveness is based on cardiac response.
Question 52.
The emergency nurse administered activated charcoal with sorbitol to a patient. Which of the following would be cause for concern?
(a) Absent bowel sounds
(b) Three episodes of diarrhea
(c) Mean arterial pressure of 83 mm Hg
(d) Passage of copious dark stool
Answer:
(a) Absent bowel sounds
Rationale:
A contraindication to the administration of sorbitol is a bowel ileus because increasing lumen pressures proximal to a bowel obstruction exacerbates the risk of bowel perforation; therefore, absent bowel sounds would be a cause for concern in this situation. Sorbitol is a cathartic agent that may be added to activated charcoal to increase elimination of charcoal-bound toxins from the gastrointestinal tract. Sorbitol is a sugar-alcohol and is known to stimulate bowel motility by increasing intra-intestinal osmolality and drawing extra-intestinal fluids into the large intestine.
Episodes of diarrhea would be an expected outcome of sorbitol administration and not concerning with only the three episodes noted. Loss of fluid through the gastrointestinal tract is a concern and could lead to hy-potension; however, a mean arterial pressure of 83 mm Hg (potentially 110/70) is a normotensive value and not cause for alarm. The goal of activated charcoal with sor-bitol is to bind toxins with charcoal and increase their elimination in the stool; therefore, copious dark stool would be expected if this treatment was successful.
Question 53.
Which of the following would the emergency nurse expect to find in a patient with a known amphetamine overdose?
(a) Hypotension
(b) Tachycardia
(c) Hot, dry skin
(d) Constricted pupils
Answer:
(b) Tachycardia
Rationale:
Amphetamines are central nervous system stimulants that cause sympathetic stimulation, includ-ing hypertension, tachycardia, vasoconstriction, and hyperthermia. Hot, dry skin is seen with anticholinergic agents such as jimsonweed and tricyclic antidepressants. Pupils are dilated, not constricted, with amphetamine overdose.
Question 54.
Which of the following interventions is most likely to be effective in a patient who overdoses on a beta-adrenergic blocker?
(a) Glucagon
(b) Epinephrine
(c) Calcium gluconate
(d) Digoxin immune fab
Answer:
(a) Glucagon
Rationale:
Glucagon would be the most beneficial in-tervention because its primary activity on cells is to stimulate the production of cAMP; therefore, it will bypass the blockade applied by the beta-adrenergic blocking agent. Beta-adrenergic blockers decrease heart rate (negative chronotrope) and decrease systolic blood pressure (negative inotrope) by indirectly reducing the production of cyclic adenosine monophosphate (cAMP), which inhibits the influx of calcium into muscle cells via the L-type calcium channels.
Epinephrine would be less effective in this situation because the effect of the beta-adrenergic blocker is to specifically counter the function of catecholamines such as epinephrine. Calcium gluco-nate, although effective in calcium channel blocker over-dose, would not overcome the cAMP reduction which allows calcium to use the calcium channel to enter the cells and would therefore be less effective on a beta-"adrenergic blocker overdose. The digoxin immune fab is a specifically engineered molecule that binds to digoxin and renders it functionally inert but would have no effect on beta-adrenergic blocker overdoses.
Question 55.
After ingesting 10 mg of the antihypertensive drug clonidine (Catapres) in a suicide attempt, a patient is brought to the emergency department with a decreased level of consciousness. Following steps to secure the airway and obtain vascular access, the emergency nurse should anticipate administering:
(a) Naloxone.
(b) Calcium chloride.
(c) Magnesium sulfate.
(d) Sodium bicarbonate.
Answer:
(a) Naloxone.
Rationale:
Clonidine may stimulate the production of an opioid-like substance in high doses; therefore, the priority intervention of reversing the life-threatening depres¬sant effects of opioids would be anticipated. Clonidine is an imidazoline antihypertensive agent that stimulates alpha- adrenergic receptors in the central nervous system. Investigational uses include detoxification of opioid dependence. Calcium chloride, magnesium sulfate, and sodium bicarbonate would be neither indicated nor offer life-saving effect.
Question 56.
For which of the following exposures would charcoal hemoperfusion be indicated?
(a) Methanol
(b) Digitalis (Digoxin)
(c) Amitriptyline (Elavil)
(d) Coumadin (warfarin)
Answer:
(b) Digitalis (Digoxin)
Rationale:
Charcoal hemoperfusion is an extracorporeal technique by which blood is filtered through activated charcoal to remove toxins. Unfortunately, this process only works on a limited mumber of substances includ-ing digitalis, paraquat, phenobarbital, Tegretol, and theophylline. Methanol, amitriptyline, and Coumadin do not respond to charcoal hemoperfusion therapies. Char-coal hemoperfusion is different than hemodialysis. Alco-hol ingestions can be treated with hemodialysis.
There are several very important interventions, just as hemoperfusion, which have quite limited applications. Just because they are not universal does not mean they do not provide a valuable therapy. Knowing the limitations of an intervention can often be key!
Question 57.
An unresponsive patient is brought to the emergency department after a possible overdose. If the emergency nurse wants to determine whether the patient ingested an opioid rather than a sedative, which of the following would help make this determination?
(a) Bradycardia
(b) Hypertension
(c) Constricted pupils
(d) Absent bowel sounds
Answer:
(c) Constricted pupils
Rationale:
Constricted pupils would be a good assess-ment finding to help determine the likely ingestion was a narcotic and help the nurse provide definitive treatment promptly. The toxidrome for opioids and sedative-hypnotics are nearly identical in that they both cause bradycardia, hypotension, hypothermia, decreased bowel sounds, bradypnea, and have no change in skin moisture.
However, the difference between these two classes of medication is that opioids are known to cause constricted pupils, whereas sedative-hypnotics do not normally change pupil size. Bradycardia and absent bowel sounds are common with both types of ingestion and would not specifically assist with determining definitive treatment. Hypertension is not associated with either class of medication and would, therefore, not be anticipated.
Question 58.
A patient, after ingesting nightshade, is treated with physostigmine. Which of the following would indicate this treatment had its intended effect?
(a) Pupils dilate
(b) Heart rate increases
(c) Blood pressure rises
(d) Hallucinations subside
Answer:
(d) Hallucinations subside
Rationale:
Resolution of hallucinations would indicate a reversal of the anticholinergic effects and, therefore, successful treatment. Nightshade is known to have an-ticholinergic properties that may include tachycardia, dry skin, hyperthermia, psychosis and hallucinations, vaso-constriction, mydriasis (dilating pupils), increased blood sugar, and tachypnea.
Physostigmine is a cholinergic agent which can be used to counter the effects of anticholinergic toxicity. Increased heart rate, elevated blood pressure, and dilated pupils are all signs of an anticholinergic effect and these effects, therefore, would not indicate success in treatment.
Question 59.
Which of the following laboratory values is most consistent for a patient with an untreated acute salicylate overdose?
(a) A serum pH of 7.49
(b) A serum glucose of 150 mg/dL J
(c) A serum potassium of 2.9 mEq/L
(d) A serum creatinine level of 9.9 mg/dL
Answer:
(c) A serum potassium of 2.9 mEq/L
Rationale:
Salicylates create a direct stimulation of the beta2-adrenergic receptors, leading to respiratory alkalosis which, in turn, drives calcium and potassium losses in the urine as carbon dioxide is lost in the respiratory drive. Salicylates, such as Aspirin, are metabolized into salicylic acid and lead to, in overdoses, a profound metabolic acidosis.
The acidosis is exacerbated through three primary mechanisms: loss of bicarbonate, inability to excrete phosphoric and sulfuric acids, and stimulation of gluconeogenesis and ketoacid production. Low serum pH, rather than elevated, would be consistent in this untreated situation.
Hypoglycemia due to metabolism stimulation as oxidative phosphorylation is uncoupled by salicylate metabolites is more likely than elevated serum glucose. Although renal insufficiency may be seen, it is generally mild and would certainly not be anticipated to raise serum creatinine as high as 9.9 mg/dL.
Question 60.
When giving activated charcoal in small intermittent doses, the best explanation of the rationale for this method is that small doses:
(a) Increase the binding of toxins.
(b) Decrease the likelihood of bowel obstruction.
(c) Lessen the onset of electrolyte disturbances.
(d) Reduce the incidence of vomiting and aspiration.
Answer:
(d) Reduce the incidence of vomiting and aspiration.
Rationale:
Large quantities of activated charcoal, when given in a short period of time, are known to distend the stomach wall and stimulate gastric contraction and regurgitation. By giving smaller intermittent doses, this risk decreases. It is also easier for the patient to take in smaller doses. Giving smaller intermittent doses of activated charcoal does not reduce the risk of developing a bowel obstruction nor does it increase the binding ability of the charcoal. Activated charcoal is not associ¬ated with electrolyte disturbances regardless of the rate at which it is administered.
Do not forget the basics. It is not always the flashy interventions or therapies that show up on the ex-amination. Remembering your basic nursing interventions is vital for all certified emergency nurses!
Question 61.
When evaluating the effectiveness of treatment for organophosphate poisoning, the emergency nurse should prepare to administer additional antidote if a patient continues to display which of the following signs or symptoms?
(a) Tachycardia
(b) Hot, dry skin
(c) Pinpoint pupils
(d) Dry mucous membranes
Answer:
(c) Pinpoint pupils
Rationale:
If the nurse notes constricted pupils, adequate anticholinergic intervention has not been reached and subsequent dose(s) should be administered. Organophosphate agents act as cholinergic agonists and lead to symptoms which include vasodilation, decreased serum glucose, fluid production such as diaphoresis and brpnchorrhea, constricted pupils, bradycardia, and bradypnea.
Atropine, the antidote for organophosphate poisoning, is an anticholinergic agent and would counter the cholinergic (parasympathetic) symptoms of the exposure. Tachycardia hot, dry skin; and dry mucous membranes would all be expected findings of the successful treatment with the anticholinergic medication.
Question 62.
The following electrocardiogram is associated with which of the following overdoses? 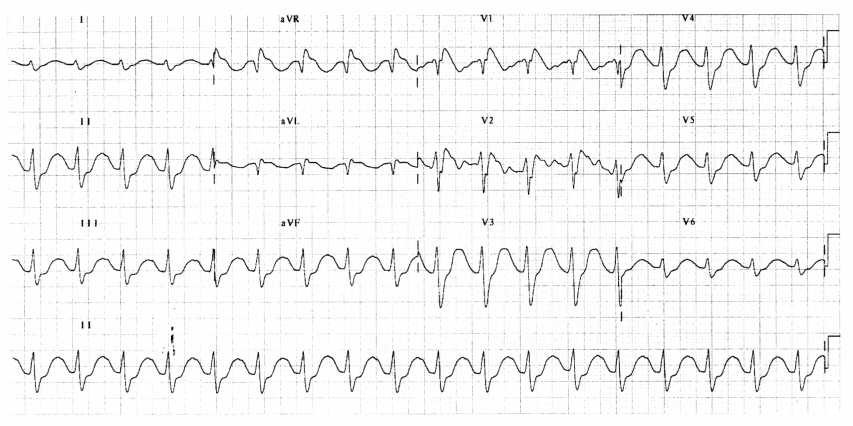
(a) Doxepin (Sinequan)
(b) Diltiazem (Cardizem)
(c) Propranolol (Inderal)
(d) Carvedilol (Coreg)
Answer:
(a) Doxepin (Sinequan)
Rationale:
Doxepin (Sinequan) is a tricyclic antide-pressant (TCA) and its toxicity is associated with these changes. Tricyclic antidepressants block voltagegated sodium channels causing electrocardiogram changes such as prolonged PR interval, widened QRS complexes, and prolonged QT intervals.
Diltiazem (Cardizem) is a calcium channel blocker and is associated with heart blocks and bradycardia which is not depicted in this strip. Propranolol (Inderal) and Carvedilol (Coreg) are a beta-adrenergic blockers and, similar to calcium channel blockers, leads to bradycardia and heart blocks.
Remember earlier I said there could be rhythms based on very specific conditions or toxicities? Here it is! TCAs have a specific pathophysiologic effect on sodium channels and create a very unique rhythm. Can you think of a few other examples? Like hyper¬kalemia? Hypomagnesemia?
Question 63.
A patient is brought to the emergency department after a possible cocaine overdose. Which of the following would the emergency nurse expect to note?
(a) Miosis
(b) Sudation
(c) Catatonia
(d) Borborygmus
Answer:
(b) Sudation
Rationale:
Sudation is another term for diaphoresis and would be the most likely symptom of those listened. Cocaine acts as a sympathomimetic agent and leads to stimulation of the adrenergic receptor sites. Symptoms may include vasoconstriction, hypertension, increased serum blood sugar, diaphoresis, dilation of the pupils, central nervous system stimulation or excitation, tachy-cardia, tachypnea, and decreased bowel motility.
Miosis, constriction of the pupils, is not associated with cocaine toxicity. Catatonia, a state of stupor or psychomotor im-mobility, is not an expected effect of sympathomimetic overdose. Borborygmus, or bowel sounds, would not be an expected finding but rather a lack of bowel sounds would be more likely noted in this case.
Remember your diagnostic terms and anatomy,and physiology definitions. Find ways to keep look-alike/ sound-alike terms clear. For instance, do you have trouble with miosis and mydriasis? Tryrthis: Miosis is the smaller word; the smaller word makes the smaller pupib Miosis is pupillary constriction. Mydriasis is the larger word; the larger word makes the larger pupils. Or the “D” in mydriasis stands for “dilation. ” Mydriasis is pupillary dilation.
Question 64.
A patient is unintentionally exposed to a large quantity of insecticide and brought to the emergency department for treatment. Which of the following sets of symptoms would be the most likely seen on assessment when the patient arrives?
(a) Urination, elevated serum pH, diarrhea
(b) Lacrimation, respiratory crackles, miosis 1
(c) Bradycardia, muscle cramping, dry cough
(d) Absent bowel sounds, drooling, defecation
Answer:
(b) Lacrimation, respiratory crackles, miosis 1
Rationale:
Lacrimation (tearing), respiratory crackles (due to stimulation of bronchial secretions), and miosis would all be symptoms consistent with this toxidrome. Insecticides commonly work by stimulating muscarinic and nicotinic pathways of the parasympathetic nervous system and, therefore, are associated with symptoms of the cholinergic toxidrome. The cholinergic toxidrome includes constricted pupils (miosis), increased bowel motility, and increased fluid production.
This toxidrome causes lability in heart rate, blood pressure, and respira-tion, which is to say it may produce high or low findings in each. Although urination and diarrhea would be ex-pected findings, acidosis, rather than elevated serum pH, would be more likely due to gas exchange obstruction from fluid production in lungs anti lactic acid production due to cellular hypoperfusion.
Bradycardia may be typi-cal in cholinergic exposures but muscle weakness, rather than cramping, and moist, rattling cough, rather than dry bradypnea, and decreased mental status.
Question 65.
Dimercaprol (British anti-Lewisite) is prescribed for a patient in the emergency department. The emergency nurse suspects the patient has which of the following presenting complaints?
(a) Exposure to anthrax
(b) Ingestion of mercury
(c) Inhalation of cyanide gas
(d) Consumption of ethylene glycol
Answer:
(b) Ingestion of mercury
Rationale:
Dimercaprol (British anti-Lewisite) is a chelating agent used to treat heavy metal exposures including arsenic, lead, gold, and mercury. Anthrax is a bacterial infection treated with long-course antibiotics such as ciprofloxacin or doxycycline and supportive care. Cyanide exposures are treated with hydroxocobalamin or with the classic cyanide kit which includes amyl nitrite, sodium nitrite, and sodium thiosulfate. Ethylene glycol is treated with ethanol to prevent liver metabolism of the alternate alcohol into toxic metabolites while treatments such as dialysis is implemented.
Cyanide treatment with amyl nitrite, sodium nitrite, and sodium thiosulfate consists of causing a low level of methemoglobinemia which is not a good‘ thing but better than cyanide poisoning! Cyanide likes methemoglobin much better and will bind with it to create cyanomethemoglobin. The sodium , thiosulfate then creates thiocyanate and it is then excreted in the urine. Utilizing hydroxycobalamin creates cyanocobalamin, which is then excreted also through the renal system.
Some significant side effects can occur when using hydroxycobalamin including hypertension, urine discoloration, and anaphylaxis and an inability to use with hemodialysis. It should also not be administered in the same line with medications such as diazepam (Valium), dopamine, or dobutamine. Another important note is that patients with smoke inhalation should not receive the sodium nitrite unless the carboxyhemoglobin level is verified as under 10%. Otherwise, it can extend the effects of the CO, which would decrease the oxygen-carrying
capacity of the patient’s blood.
Question 66.
A patient presents with an opioid overdose. Which of the following symptoms would be most likely uncovered by the emergency nurse?
(a) Diarrhea, dilated pupils, tachypnea
(b) Confusion, cool extremities, miosis
(c) Bradypnea, diaphoresis, thready pulses
(d) Bradycardia, hot and dry skin, hyperthermia
Answer:
(b) Confusion, cool extremities, miosis .
Rationale:
Symptoms of opioid toxicity include bra-dycardia, constricted pupils (miosis), hypotension, decreased body temperature, decreased bowel sounds, Diarrhea, cough would be more likely in this scenario. And, finally, dilated pupils, tachypnea, diaphoresis, thready pulses although drooling and defecation would be expected (associated with vasoconstriction), hot and dry skin, and symptoms, increased bowel motility, rather than absent hyperthermia would not be associated with a patient who bowel sounds, would be a more anticipated symptom.
Question 67.
A child is brought to the emergency department after accidentally dousing himself in lamp oil while attempting to drink it. After immediate decontamination, the emergency nurse knows that interventions for which system is the next highest priority?
(a) Pulmonary
(b) Neurologic
(c) Cardiovascular
(d) Gastrointestinal
Answer:
(a) Pulmonary
Rationale:
Pulmonary complications would be the highest priority for interventions after decontamination stopped continued exposure. Petroleum distillates, such as kerosene, lighter fluid, lamp oil, turpentine, and certain pesticides, pose a direct threat through ingestion, aspiration, and absorption through skin.
The most life-threatening complications normally occur from aspiration and pulmonary problems. In this situation, the child potentially drank and then was subsequently exposed to the petroleum distillate through skin absorption.
Complications to neurologic and cardiovascular systems would be possible but would result secondary to respiratory insufficiencies. The gastrointestinal tract may be altered, and problems may arise from exposure, but would not take priority over the pulmonary system.
Question 68.
Treatment is undertaken for a calcium channel blocker overdose. The emergency nurse knows that treatment has been effective if the patient’s:
(a) Heart rate decreases.
(b) Temperature decreases.
(c) Serum glucose increases.
(d) Blood pressure increases.
Answer:
(d) Blood pressure increases.
Rationale:
An increase in the patient’s blood pressure is an indication of successful treatment. Signs of calcium channel overdoses include hypotension (due to negative inotropic effects), bradycardia/heart blocks (due to negative chronotropic effects), decreased or altered level of consciousness (in response to both hypotension and bradycardia}, ' nausea, vomiting, and hyperglycemia (resulting from pancreatic L-type calcium channel blockage and resultant insulin resistance in the cells).
A decrease in the patient’s heart rate and an increase in the patient’s serum glucose levels all indicate that treatment is not working. The patient’s temperature does not usually change with either the overdose of calcium channel blockers or the treatment for it.
Question 69.
Which of the following substances is considered a sympathomimetic?
(a) Phencyclidine (PCP)
(b) Fentanyl (Sublimaze)
(c) Physostigmine (Antilirium)
(d) Gamma-hydroxybutyric acid (GHB)
Answer:
(a) Phencyclidine (PCP)
Rationale:
The example of a sympathomimetic is phen¬cyclidine (PCP). The sympathomimetic class of medica¬tions are substances commonly referred to as “uppers” and include street drugs such as methamphetamine or co¬caine, psychedelic agents such as phencyclidine (PCP) or D-lysergic acid diethylamide (LSD), and prescription medi¬cations such as albuterol, dopamine, or amitriptyline. Fen- tanyl is in the opioid class, physostigmlne belongs to the cholinergic class, and gamma-hydroxybutyric acid (GHB) falls into the sedative-hypnotic toxidrome as a barbiturate.
Question 70.
Which of the following findings is associated with successful treatment for a flunitrazepam (Rohypnol) overdose?
(a) Decrease in agitation
(b) Increase in heart rate
(c) Decrease in serum pH
(d) Increase in blood pressure
Answer:
(d) Increase in blood pressure
Rationale:
An increase in blood pressure would indicate successful treatment. Symptoms of flunitrazepam (Rohyp- nol) overdose include CNS depression (amnesia, confusion, unconsciousness) and hypotension. Because CNS depression is a side effect of this drug, a decrease in agitation is not an indication of successful treatment.
Depressed respiratory effort coupled with hypotension is likely to cause an acidosis with a low serum pH; therefore, a reduction in serum pH would not indicate effective treatment. Bradycardia is not a significant finding in this overdose; therefore, elevation in the heart rate is not associated with successful treatment.
Question 71.
A patient with an unknown single-drug overdose presents to the emergency department and is given a dose of naloxone (Narcan) to determine whether opioids are present. Which of the following findings would indicate opioids were the substance ingested?
(a) Drying of skin
(b) Dilated pupils
(c) Decreased heart rate
(d) Assisted ventilation
Answer:
(b) Dilated pupils
Rationale:
Reversal of opioid toxicity would likely cause the heart rate (o increase, pupil size to increase, blood pressure to rise, bowel sounds to increase, and respirations to increase. Moisture to the skin is not normally affected by opioids and would, therefore, not be expected to change when an opioid reversal agent is administered.
Bradycardia is a symptom of opioid toxic-ity; therefore, naloxone administration would not cause further bradycardia and not prove that opioids were the cause. Requiring assisted ventilations would be indicated if the patient became bradypneic or otherwise had in-terruption of ventilations; therefore, this would not be expected if opioid toxicity were removed following ad-ministration of naloxone (Narcan).
Remember that if Naloxone (Narcan) is going to work, it will occur within the first few minutes of administration. The patient will often awaken agitated and may require some strong arms to keep the person in the bed! The effects of Naloxone (Narcan) will last for about 20 to 90 minutes, after which the patient may require redosing.
Question 72.
Which of the following medications should the emergency nurse be prepared to administer to a patient with a toxic acetaminophen (Tylenol) level?
(a) Succimer (Chemet)
(b) Flumazenil (Romazicon)
(c) Deferoxamine (Desferal)
(d) Acetylcysteine (Acetadote)
Answer:
(d) Acetylcysteine (Acetadote)
Rationale:
It takes up to 24 hours for acetaminophen (Tylenol) to accumulate in the liver and cause liver damage; therefore, acetylcysteine (Mucomyst or Ac- etadote) can be given up to 24 hours after ingestion and still be effective. Although acetylcysteine (Mucomyst or Acetadote) should be given earlier, such as 2 or 4 hours after ingestion, it is still effective up to 24 hours later.
Acetylcysteine (Mucomyst) should not be given with charcoal, because charcoal will absorb acetylcysteine (Mucomyst) and prevent it from being absorbed into the body where it can effectively reduce acetaminophen (Tylenol) levels. Acetylcysteine (Mucomyst or Acetadote) should be given before liver enzymes elevate to prevent liver damage. Succimer (Chemet) is the chelating agent for lead poisoning. Flumazenil (Romazicon) is used to reverse the effects of benzodiazepines and Deferoxamine (Desferal) is the antidote for iron toxicity.
Question 73.
A patient is treated with deferoxamine (Desferal) following a drug toxicity. Which of the following would be the most likely agent involved in this situation?
(a) Prenatal vitamins
(b) Methamphetamine
(c) Nortriptyline (Aventyl)
(d) Nitroprusside (Nipride)
Answer:
(a) Prenatal vitamins
Rationale:
Deferoxamine (Desferal) is the antidote for iron. Prenatal vitamins are a common source of ele-mental iron. Methamphetamine, tricyclic antidepressants such as nortriptyline, and nitroprusside are not treated with deferoxamine.
Question 74.
Which of the following interventions would be the highest priority for an unresponsive patient with an overdose of the sulfonylurea agent glipizide?
(a) 20 mL/kg IV bolus of isotonic crystalloid
(b) Octreotide (Sandostatin) 80 mg IV bolus
(c) 25 g IV push of dextrose in 50 mL water
(d) 15 g of oral glucose solution (Glutose 15)
Answer:
(c) 25 g IV push of dextrose in 50 mL water
Rationale:
The highest priority intervention for this pa-tient would be to restore serum glucose with a bolus of IV dextrose solution. Sulfonylureas act by blocking potassium channels in pancreatic beta cells which results in additional insulin release. This excess insulin in the system can lead to life-threatening hypoglycemia in overdoses. Oral glucose would also meet this need, but it is contraindicated in a comatose patient because of the risk for aspiration.
In addition, the 15 g of dextrose would be much slower to reach the cells and would, therefore, not take precedence over IV dextrose. Intravenous fluid bolusing would be helpful in a patient with hyperglycemia and subsequent volume depletion, but it would not be a result from a patient overdosing on a sulfonylurea medication. Octreotide would be a reversal agent for sulfonylurea overdose because it would stop the pancreas from secreting insulin; however, the im¬mediate crisis in this situation is not the medication, but rather the hypoglycemic shock it has caused.
Another example of multiple “good” choices, but understanding the situation and underlying patho-physiology helps you see which one is the priority in this situation. Be sure to read all of the question and take everything into accouht when reading the stem of the question! The answers lie within!
Question 75.
A patient with an acute cyanide ingestion is brought to the emergency department by a private vehicle. Which of the following interventions takes the highest priority?
(a) Administer cyanide antidote.
(b) Perform gastric lavage.
(c) Give activated charcoal.
(d) Manage seizure activity.
Answer:
(a) Administer cyanide antidote.
Rationale:
The cyanide antidote should be administered before decontaminating the Cl tract or managing seizure activity. Because cyanide is rapidly absorbed and causes cellular hypoxia, reversing the hypoxia takes priority. One method of treating cyanide is administering the classic cyanide kit which contains an amyl nitrite inhaler or ampule that can be broken and placed in the oxygen mask and sodium nitrite, both of which create methemoglobin and attract cyanide away from the respiratory enzyme cytochrome oxidase.
Sodium thiosulfate is also used; it forms nontoxic thiocyanate and removes the cyanide from the body. Performing gastric lavage, giving activated charcoal, and managing seizures are not incorrect, but do not reverse the immediate life-threatening symptom of cellular hypoxia.
Amyl nitrite and sodium nitrite both do the same thing! Utilize the amyl nitrite first, which then buys the emergency nurse time to start an intravenous line. Once the line is established, remove the amyl nitrite before administering the sodium nitrite. A low level of methemoglobinemia is desired.
The reversal agent for methemoglobinemia is methylene blue. This is why this medication is also found in the cyanide kit. Symptoms of methemoglobinemia are the presence of cyanosis with no respiratory distress or relief with the administration of oxygen and blood draw that looks like chocolate.