The variety of CEN Study Guide available allows students to cover a wide range of topics and increase their knowledge base.
Respiratory Emergencies CEN Study Guide
Aspiration
Pathophysiologyca
Pulmonary aspiration is the entry of foreign bodies, or material from the mouth or gastrointestinal tract, into the upper and/or lower respiratory tract. Aspiration may lead to aspiration pneumonia, inflammation of lung tissue caused by infection or a reaction to the aspirated substances.
Risk Factors
- age > 65 years
- difficulty swallowing/neurological dysfunction
- intoxication/sedation/altered LOC
Physical Examination
- coughing or choking
- dyspnea
- fever
- abnormal lung sounds
- possible wheezing, rhonchi, or crackles
- diminished lung sounds in the lobe where the aspiration has settled
Diagnostic Tests
- CXR showing infiltrates after the aspiration
- WBC and blood cultures may show infection
Management
- manage airway
- oxygen and antibiotics as needed
Asthma
Pathophysiology
Asthma is a chronic obstructive pulmonary disease characterized by airway inflammation and bronchoconstriction. Asthma exacerbations may be triggered by allergens, infections, exercise, aspirin, and GERD. When the triggered response occurs, the airway becomes obstructed by a combination of bronchospasm, thick mucus, mucosal edema, and airway inflammation.
Status asthmaticus is a severe, progressively worsening asthma event that does not respond to bronchodilator therapy; the condition may develop into acute respiratory failure.
Physical Examination
- tachypnea and severe dyspnea
- bronchoconstriction
- expiratory wheeze (early stage); inspiratory and expiratory wheeze (late stage)
- wheezes may disappear with fatigue or if obstruction prevents wheezing
- increased use of accessory respiratory muscles
- decreased breath sounds in all lung fields (an ominous sign, as patient is not moving enough air)
- hypoxia (early); hypercapnia (late)
- tachycardia and hypertension
- pulsus paradoxus >20 mm Hg
- with progression of disease
- decreased cardiac output
- hypotension and bradycardia
- seizure
- coma
Diagnostic Tests
- peak expiratory flow rate (PEFR) showing 20% drop from expected response to treatment or baseline best effort
- ABG
- initial: respiratory alkalosis with hypoxemia
- worsening: respiratory acidosis with hypercapnia
- ECG may show peaked P wave and right-axis deviation
- CXR to rule out other underlying diseases (e,g., pneumonia, pneumothorax)
Management
- high-flow O2 to keep SpO2 >92%, or heliox to decrease airway resistance
- medications
- inhaled bronchodilators (beta 2 agonists)
- anticholinergics (synergistic effect with beta 2 agonists)
- corticosteroids
- mechanical ventilation required if patient is unresponsive to medication
Chronic Obstructive Pulmonary Disease (COPD)
Chronic obstructive pulmonary disease (COPD) is characterized by a breakdown in alveolar tissue (emphysema), chronic productive cough (chronic bronchitis), and long-term obstruction of the airways. The condition worsens over time.
COPD is characterized by low expiratory flow rates. Acute exacerbations of COPD are characterized by increased sputum production and hypoxia or hypercapnia, which may require emergent treatment.
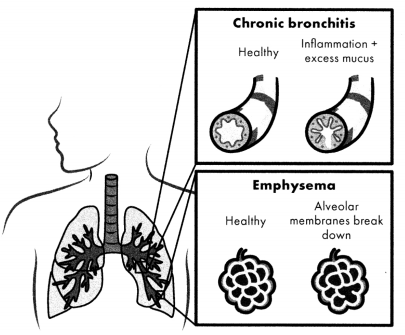
Figure 2.7. Chronic Obstructive Pulmonary Disease (COPD)
Risk Factors
- smoking (> 30 pack years [pack-years = packs per day x years])
- passive exposure to cigarette smoke
- exposure to inhaled chemicals or pollution
- severe childhood respiratory illness
Diagnosis
- chronic, productive cough
- dyspnea and wheezing
- prolonged expiration
- barrel chest (late sign)
- spirometry
- forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) used to measure airflow limitations
- FEV1/fVC less than 0.7 after bronchodilator administration generally diagnostic of COPD
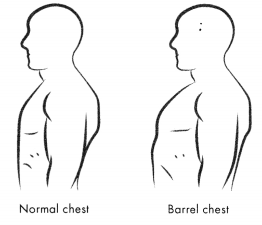
Figure 2.8. Barrel Chest
Management
- first-line management
- bronchodilators (not inhaled corticosteroids) such as short-acting beta-agonists (e.g., albuterol)
- anticholinergics: inhaled ipratropium
- administer oxygen
- cautious use of oxygen (titrated to SpO2 88- 92% or PaO2 of 60 mm Hg)
- monitor for hypercapnia when administering oxygen
- BiPaP if SpO2 does not improve
- chest physiotherapy and comfortable positioning
- teach smoking cessation at discharge
Respiratory Infections
Pneumonia is a lower respiratory tract infection that can be caused by bacteria, fungi, protozoa, or parasites. The infection causes inflammation in the alveoli and can cause them to fill with fluid.
- Diagnosis and treatment of community-acquired pneumonia (CAP), hospital-acquired pneumonia (HAP), and aspiration pneumonia are similar.
- Signs and symptoms include cough, dyspnea, hemoptysis, pleuritic chest pain, and fever. Abnormalities in affected lung/lobe include decreased lung sounds, inspiratory crackles, and dull percussion.
- CXR will show infiltrates; WBC and blood cultures will show infection.
- Management is antibiotics and oxygen as needed.
Croup is an upper airway obstruction caused by subglottic inflammation that results from viral illness (although rarely it can be caused by bacterial infection). The inflammation results in edema in the trachea and adjacent structures. Additionally, thick, tenacious mucus further obstructs the airway.
- Croup is associated with a barking cough and characteristic high-pitched stridor.
- Management may include oxygen, cool mist therapy, corticosteroids (dexamethasone), and nebulized racemic epinephrine.
Bronchitis is inflammation of the bronchi. Most cases (> 90%) are caused by a viral infection, but bronchitis can also result from bacterial infection or environmental irritants.
- Signs and symptoms may include a non-productive cough that evolves into a productive cough, sore throat, and congestion.
- Acute bronchitis will usually spontaneously resolve without intervention.
- Discharge instructions should include home symptom management (e.g., adequate hydration, use of humidifiers, and OTC antitussives)
- Fluids, antitussives, analgesics, or antibiotics may be administered.
Bronchiolitis is inflammation of the bronchioles, usually because of infection by RSV or human rhinovirus. The inflammation and congestion lead to a narrowing of the airway, resulting in dyspnea. Bronchiolitis is seen in children younger than 2 years and will usually spontaneously resolve.
Inhalation Injuries
Pathophysiology
Inhalation injuries fall into three categories differentiated by the mechanism of the injury.
- Exposure to asphyxiants such as carbon monoxide (CO) can cause injuries. In the case of CO poisoning, the CO displaces the oxygen on the hemoglobin molecule, leading to hypoxia and eventual death of tissue.
- Thermal or heat inhalation injuries can be caused by steam, heat from explosions, or the consumption of very hot liquids. The resulting edema and blistering of the airway mucosa lead to airway obstruction.
- Smoke exposure from fire or toxic gases causes damage to pulmonary
Risk Factors
- occupational exposure to asphyxiants or toxic gases
- proximity to fire
- intentional inhalation of toxic gases
Diagnosis
- depends on what irritant the patient is exposed to
- mucosal and pulmonary edema possible up to 48 hours after exposure
- general s/s of respiratory distress (e.g., dyspnea, wheezing, etc.)
- may be signs of injury at mouth, nose, or oral mucosa
Management
- manage airway
- intubate for burns in or around mouth
- oxygen as needed
- administer antidote available
- vigorous pulmonary hygiene with patient (including suctioning of airways, blow bottles, and nasotracheal suction)
Obstruction
Pathophysiology
Airway obstruction, or blockage of the upper airway, can be caused by a foreign body (e.g., teeth, food, marbles), the tongue, vomit, blood, or other secretions. Possible causes of airway obstruction include traumatic injuries to the face, edema in the airway, peritonsillar abscess, and burns to the airway. Small children may also place foreign bodies in their mouths or obstruct their airways with food.
Risk Factors
- age < 2 years and > 65 years
- upper airway burn or inhalation injury
- severe facial trauma
- seizures
- infections or inflammation of the upper airway
- difficulty swallowing
Diagnosis
- visually observed obstruction in the airway
- dyspnea or, gasping for air
- stridor
- excessive drooling in infants
- agitation or panic
- loss of consciousness, altered LOC, or respiratory arrest
Management
- inspect the airway
- suction out any visible foreign bodies
- reassess the patency of the airway
- if the airway is still obstructed, view with a laryngoscope
- if all else fails, cricothyrotomy to open the airway; suction mouth, and upper airway
Pleural Effusion
Pathophysiology
Pleural effusion is the buildup of fluid around the lungs in the pleural space. The fluid can displace lung tissue and inhibit adequate ventilation and lung expansion. There are two types ofpleural effusions.
- Transudative pleural effusions are fluid leakages caused by increased systemic pressure in the vessels or low serum protein levels. The most common causes of transudative pleural effusions are heart failure (due to increased pulmonary capillary pressure) or cirrhosis (currently believed to be the result of fluid movement from the peritoneal cavity to the thorax).
- Exudative pleural effusions are the result of changes in capillary permeability resulting in exudate. They have widely varying etiologies, including malignancy (especially lung cancer), pulmonary embolism, and infections.
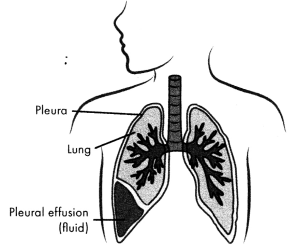
Figure 2.9. Pleural Effusion
Physical Examination
- dyspnea
- dullness upon percussion of the lung area
- asymmetrical chest expansion
- decreased breath sounds on affected side
- cough (dry or productive)
- pleuritic chest pain
Diagnostic Tests
- CXR showing white areas at the base of the lungs (unilaterally or bilaterally)
- CT scan to further diagnose the severity of the condition
- thoracentesis to determine the mechanism of effusion
Management
- stable, asymptomatic patients: monitoring and treatment of underlying condition
- symptomatic patients: drainage of excess pleural fluid (usually via thoracentesis)
- multiple thoracenteses necessary for reaccumulated fluid
- pleurodesis or indwelling pleural catheter for recurrent effusions
- medications based on underlying condition (e.g., diuretics, antibiotics)
Pneumothorax
Pathophysiology
Pneumothorax is the collection of air between the chest wall and the lung (pleural space). It can occur from blunt chest-wall injury, medical injury, underlying lung tissue disease, or hereditary factors. Pneumothorax is classified according to its underlying cause.
- Primary spontaneous pneumothorax (PSP) occurs spontaneously in the absence of lung disease and often presents with only minor symptoms.
- Secondary spontaneous pneumothorax (SSP) occurs in patients with an underlying lung disease and presents with more severe symptoms.
- Traumatic pneumothorax occurs when the chest wall is penetrated.
- Tension pneumothorax, the late progression of a pneumothorax, causes significant respiratory distress in the patient and requires immediate intervention for treatment.
Risk Factors
- for PSP: more common in men 20- 40 years old who are tall and underweight
- underlying lung tissue disease
- medical procedures
- blunt chest-wall injuries
- changes in atmospheric pressure smoking
Physical Examination
- sudden unilateral chest pain
- dyspnea
- tachycardia
- hypoxia and cyanosis
- hypotension
- tension pneumothorax:
- decreased breath sounds on the affected side
- increased percussion note
- tracheal deviation away from the side of the tension
- distended neck veins
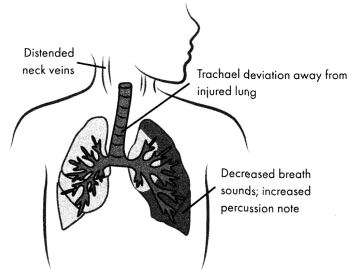
Figure 2.10. Physical Examination of Tension Pneumothorax
Diagnostic Tests
CXR will show lung tissue separated from the chest wall
Management
- pneumothorax < 15%: supplemental oxygen and monitoring
- pneumothorax > 15%: percutaneous needle aspiration of air from pleural space and insertion of chest tube
- emergent treatment of tension pneumothorax: immediate percutaneous placement of large-bore needle (insertion at second intercostal space mid-axillary line on affected side) and chest-tube insertion.
Noncardiac Pulmonary Edema
Pathophysiology
Noncardiac pulmonary edema (NPE) is when fluid collects in the alveoli of the lungs, but the condition is not due to heart failure. This fluid inhibits gas exchange.
Acute respiratory distress syndrome (ARDS) is a sudden and progressive form of noncardiogenic NPE in which the alveoli fill with fluid following damage to the pulmonary endothelium. ARDS is the systemic response to lung injury and is initiated by the inflammatory-immune system, which releases inflammatory mediators from the site of injury within 24- 48 hours. Inflammation causes alveoli to stiffen and collapse, resulting in NPE with refractory hypoxemia. Left- and right-sided heart failure may follow.
Risk Factors
- ARDS
- gastric aspiration, pneumonia
- toxic inhalation
- pulmonary contusion
- sepsis
- DIC
- pancreatitis
- fluid overload
- CNS injury (neurogenic pulmonary edema)
- removal of airway obstruction (post obstructive pulmonary edema)
- rapid increase in altitude (high-altitude pulmonary edema)
- reexpansion of the lung (reexpansion pulmonary edema)
Physical Examination
- tachycardia and hypotension
- tachypnea with increased accessory-muscle usage for work of breathing
- productive cough with frothy sputum (maybe pink)
- wheezes, crackles, and rhonchi
- progressive hypoxemia
- other signs and symptoms of heart failure
Diagnostic Tests
- CXR showing pulmonary infiltrates, ground-glass opacity, and an elevated diaphragm
- DecreasingP/Fratio
- <300 = mild ARDS
- <200 = moderate ARDS
- <100 = severe ARDS
- ABG findings
- refractory hypoxemia
- increasing hypercapnia
Management
- high-flow oxygen
- inhaled bronchodilator
- positive inotropic therapy and other vasoactive medications to maintain cardiac output
- mechanical ventilation required for severe ARDS
- set PEEP at lowest possible amount (10- 15 cm H2O)
- low VT (4-6 mL/kg) to reduce barotrauma and volutrauma
- permissive hypercapnia with arterial pH >7.20
- treat underlying condition
Pulmonary Embolus
Pathophysiology
A pulmonary embolus (PE) is a thromboembolic that occludes a pulmonary artery. The most common embolus is a blood clot caused by deep vein thrombosis (DVT), but fat emboli, tumor emboli, and amniotic fluid emboli can also reach the kings.
Damage to the lungs during PE follows several pathways. The occlusion increases pulmonary dead space and causes V/Qmismatch, resulting in pulmonary shunting and hypoxemia. PE may also trigger bronchoconstriction and disrupt surfactant functioning, resulting in atelectasis and worsening hypoxemia.
Pulmonary hypertension develops from both the mechanical obstruction (clot) and the release of an injury-site mediator that causes pulmonary vasoconstriction. These processes elevate pulmonary vascular resistance (PVR), which in turn increases right ventricular workload and eventually results in right ventricular failure. Left ventricular preload decreases, cardiac output drops, hypotension follows, and shock occurs.
Risk Factors
- trauma (high risk with fracture)
- surgery
- A-fib
- immobility
- hypercoagulability states
Physical Examination
- pleuritic chest pain
- tachycardia
- tachypnea and dyspnea
- hemoptysis
- increased pulmonary S2
- sudden onset
- increased PA pressures
- right-sided HF
Diagnostic Findings
- ABG showing low PaO2
- pulmonary angiogram: definitive diagnosis but with long study time
- V/Q scan (25%- 30% accuracy)
- spiral CT scan: a 30-second study with >90% sensitivity/specificity
- ultrasound for DVT in lower extremities
- 12-lead ECG
- tall, peaked T waves inII, III, aVF
- transient RBBB
- right-axis deviation
- D-dimer positive
- ETCO2 value >36 rules out PE with high reliability
Management
- supportive treatment for symptoms
- O2 therapy
- analgesics
- vasopressors to manage blood pressure
- IV fluid resuscitation
- IV anticoagulants once diagnosis is confirmed
- thrombolytics for unstable patients with no contraindications
Respiratory Trauma
Pathophysiology
Chest trauma, whether from blunt injury, sharp, invasive penetration, or thoracic surgical procedures, creates a wide range of respiratory complications.
|
Injury |
Pathophysiology |
Clinical Presentation |
|
Pulmonary |
Bruising of the parenchyma |
|
|
Rib fractures |
Commonly caused by |
|
|
Hemothorax |
Blood in the pleural space |
|
|
Tracheal |
Occurs when there is injury to the structure of the trachea. |
|
|
Ruptured |
Injury to the diaphragm |
|
|
Flail chest |
Multiple anterior and |
• paradoxical movement of the chest wall (flail segment moves inward during inspiration and outward during exhalation) |
Management
- pain management as needed (intercostal nerve blocks, thoracic epidural analgesia, opioids, or NSAIDs)
- small contusions: heal in 3- 5 days, often without treatment
- severe contusions: aggressive pulmonary care (e.g., ambulation, turning, incentive spirometry) and fluid management with possible mechanical ventilation
- hemothorax: chest-tube insertion or thoracotomy (if bleeding cannot be managed)
- tracheal perforation: maintain an airway and prepare for surgical repair
- ruptured diaphragm: prep patient for immediate surgical intervention
- flail chest: aggressive management with analgesics, pulmonary hygiene, and noninvasive positive pressure ventilation
Pulmonary Hypertension
Pathophysiology
Pulmonary hypertension, elevated blood pressure in the arteries to the lungs (> 20 mm Hg),' is caused by occlusions or narrowing of the arteries. Because blood cannot pass through the arteries, extra strain is placed on the heart, reducing its ability to pump effectively.
There is currently no cure for pulmonary hypertension; treatment is focused on reducing symptoms through medications.
Risk Factors
- can be idiopathic
- hereditary
- chronic conditions (e.g., lupus, liver disease, HIV)
- stimulant drug use (e.g., cocaine, methamphetamines)
Physical Examination
- dyspnea
- signs of right-ventricular failure
Diagnostic Tests
- CXR may show enlarged arteries or ventricles
- CT scan of the chest may show pulmonary hypertension
- echocardiogram necessary to ascertain pressures within the pulmonary arteries
Management
emergent management: oxygen and medications (vasodilators, diuretics, and/or anticoagulants)
Read More
