Free CEN Study Guide cover various areas, such as pharmacology, medical-surgical nursing, pediatric care, and mental health.
Neurological Emergencies CEN Study Guide
Neurological Disorders
TABLE 3.3. Diagnosis and Management of Neurological Disorders
|
Disorder Alzheimer's disease |
Diagnosis |
Management |
|
a cognitive deterioration caused |
loss of short-term |
supportive treatment for symptoms |
|
Disorder |
progressive asymmetrical weakness: can affect both upper and lower extremities difficulty swallowing, walking, or speaking muscle cramps |
Supportive treatment for symptons respiratory support high risk of aspiration |
|
Multiple sclerosis |
paresthesia weakness of at least |
corticosteroids for inflammation baclofen (Lioresal) ortizanidine |
|
Muscular dystrophy (MD) a genetic disorder in which a mutation in the recessive |
first noted at 2 – 3 years of age steady progression of weakness limb flexion and contraction |
prednisone or deflazacort |
|
Disorder |
weakened eye muscles |
IV fluids |
|
Guillain-Barre |
neuropathy |
Analgesics IV immunoglobulins treatment of dysrhythmias respiratory support |
Headaches
TABLE B.4. Diagnosis and Management of Headaches
|
Condition |
Management |
|
Cluster headaches characterized by intense unilateral pain in the periorbital or temporal area, with ipsilateral autonomic symptoms |
usually resolves within 30 minutes to 1 hour 100% oxygen via non-rebreather triptans (e.g., sumatriptan) |
|
Migraine a neurovascular condition caused by neurological changes that result in vasoconstriction or vasodila tion of the intracranial vessels intense or debilitating headache (typically unilat eral) lasting from 4 hours to several days accompanied by nausea, vomiting, and sensitivity |
analgesics (NSAIDs) triptans (e.g., sumatriptan) dihydroergotamine antiemetics limit sensory triggers and apply ice packs to painful |
|
Temporal arteritis |
glucocorticoids (e.g., prednisone, methylprednisolone): early intervention to prevent permanent |
|
Tension headaches headaches characterized by generalized mild |
NSAIDs |
Increased Intracranial Pressure
Pathophysiology
Intracranial pressure (ICP) is the pressure within the intracranial compartment (the area enclosed by the cranium). A normal adult cranium encloses a fixed volume of around 1500 mL divided between brain tissue (80% of volume), CSF (10%), and blood (10%). Since the cranium does not expand or otherwise move, insults to brain tissue that increase intracranial volume will increase.
Normal ICP is 5 - 15 mm Hg. An ICP >20 mm Hg is a neurological emergency that requires immediate treatment.
When ICP increases, immediate interventions must be implemented to maintain cerebral perfusion pressure (CPP), the net pressure gradient that drives oxygen delivery to brain tissue. CPP is defined as the difference between MAP and ICP (i.e., MAP - ICP), and should be maintained at 50- 70 mm Hg.
Risk Factors
- trauma (TBI, brain contusion)
- mass displacement of brain tissue by tumor, hematoma, or abscess
- hypoxic-ischemic brain injury
- intracranial hemorrhage
- increased CSF production (meningitis)
- blockages to CSF flow/reabsorption (hydrocephalus, meningeal disease)
- seizures
- hyperthermia (core temperature > 37.5°C)
Physical Examination
- change in LOC
- headache
- vomiting
- Cushing's triad
- irritability
- photophobia
- lethargy and impaired/slowed decision-making
Diagnostic Tests
- ICP > 20 mm tfg
- abnormal ICP waveform
- An elevated tidal wave (P2) indicates reduced intracranial compliance and increased ICP.
- A single wave with a lack of distinct peaks indicates a critical increase in ICP that requires immediate intervention.
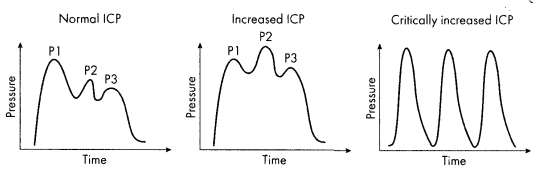
PI = Percussion wove P2 = Tidal wave P3 ~ Dicrotic notch
Figure 3.6. ICP Waveform
Management
- hyperosmolar/hypertonic fluid therapy
- mannitol 20%
- loop diuretics (assess for hypokalemia)
- hypertonic saline
- patient positioning: elevate HOB 30- 35° with midline head alignment, and avoid hip flexion
- maintain normal body temperature
- limit activities that may raise ICP, including coughing, sneezing, vomiting, suctioning, PEEP, restraint use, and the Valsalva maneuver
- stabilize blood glucose: maintain blood glucose <140 mg/dL
- decrease environmental stimuli, and minimize nursing care
- higher-level interventions for refractory ICP: mechanical ventilation, IV opioids, sedation, and decompressive craniotomy
Meningitis
Pathophysiology
Meningitis, an acute inflammation of the meninges, is caused by bacterial, viral, or fungal pathogens that invade the subarachnoid space. The infection triggers WBC accumulation and tissue damage, leading to swelling and purulent exudate within the cranium.
Viral infection is the most common cause of meningitis. Bacterial meningitis is a medical emergency because of the rapidity of deterioration and the high mortality rate.
Physical Examination
- headache
- nuchal rigidity
- positive Brudzinski’s and Kernig’s signs
- fever
- altered mental status
- rash
- photophobia
Diagnostic Tests
- lumbar puncture to confirm
- CSF finding for viral meningitis: elevated protein and lymphocytes; clear fluid
- CSF finding for bacterial meningitis: very elevated protein, elevated WBCs and neutrophils, low glucose, cloudy fluid
Management
- standard and droplet isolation precautions until a specific cause is determined
- empirical lIV antibiotic therapy
- corticosteroids
- antivirals (as appropriate)
- monitor for sepsis, increased ICP, and SIADFI/DI
Seizure Disorders
Seizure disorders are caused by abnormal electrical discharges in the brain. During a seizure, brain neurons abnormally or excessively fire because the membrane potential is altered in a way that makes those neurons hypersensitive to stimuli. Seizures may be focal (limited to one part of the, brain) or generalized.
Status epilepticus is a medical emergency in which seizure activity continues or recurs for more than 5 minutes.It has a high mortality rate (20- 30%) and requires immediate intervention.
Risk Factors
- trauma
- drug toxicity or withdrawal
- fluid or electrolyte imbalances
- hypoglycemia
- hypoxic-ischemic events
- cerebral edema
- sepsis
- tumors
Physical Examination
- convulsive: tonic-clonic (grand mal) seizure
- tonic phase: loss of consciousness, rigidity of extremities, dilated pupils.
- clonic phase: rhythmic shaking, violent alternating contraction/ relaxation, tachycardia, mouth-frothing
- postictal: impaired mental status and focal neurological deficits (Todd paralysis common)
- status epilepticus: seizure activity lasting longer than 5 minutes or repeat seizures with no regaining of consciousness between
Management
- manage ABCs
- prevent injury
- roll the patient on the left side to avoid aspiration
- loosen clothes around the neck
- lace a pillow under the patient’s head and remove objects near the head
- finger-stick blood glucose: administer 50 mL D50WIV push if blood glucose <60 mg/dL
- prompt pharmacological treatment
- first-line drup:IV lorazepam,IV diazepam, or IM midazolam
- second-line drugs (after 20 minutes of nonresponse to treatment): IV fosphenytoin, IV valproates, or IV levetiracetam
Stroke (Hemorrhagic)
Pathophysiology
A hemorrhagic stroke, the disruption of CBF, is caused by bleeding. The resulting hypoxia rapidly leads to brain cell death, and the excess blood in the cranium also increases ICP, increasing the risk of brain herniation. Bleeding may be caused by the spontaneous rupture of a blood vessel, head trauma, a brain mass, or uncontrolled anticoagulation conditions. The hemorrhage is classified by location as intracerebral or subarachnoid.
An intracerebral hemorrhage (ICH) is arterial bleeding directly into cerebral tissue. An ICH is most commonly caused by hypertensive rupture of a cerebral artery that has become damaged over time by atherosclerosis. The burst of blood from such a break in the artery causes a hematoma in the brain tissue around the rupture site. Patients with anICH often present to EMS as unconscious and require immediate intubation for ventilatory support.
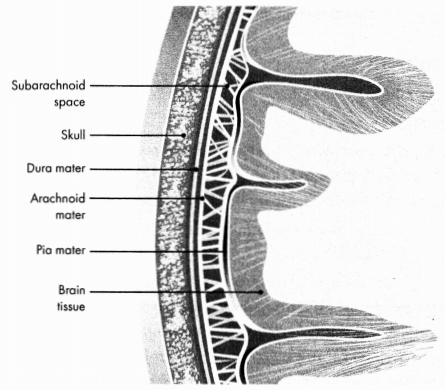
Figure 3.7. Anatomy of the Subarachnoid Space
A subarachnoid hemorrhage (SAH) is bleeding into the subarachnoid space. About 85% of spontaneous SAHs are due to the rupture of a saccular cerebral aneurysm, most commonly located at the circle of Willis. When age-related or long-term hypertension places stress on the weakened arterial blood vessel, the dome of the outpouching aneurysm thins and ruptures.
Risk Factors
- hypertension
- arteriovenous malformation (AVM)
- smoking
- diabetes
- A-fib
Diagnosis
TABLE 3.5. Diagnosis of Hemorrhagic Stroke
|
|
Intracerebral |
Subarachnoid hemorrhage |
|
Physical |
acute onset of |
abrupt onset of pain, often described as "the |
|
Diagnostic |
priority (interpreted in < 45 minutes): noncontrast CT |
noncontrast CT scan: blood visualized in CT angiogram to locate cause of hemorrhage (for surgical intervention) Hunt and Hess Grading Scale
|
Management
- priority goal: management of ABCs and reduction of BP
- intubation and mechanical ventilation usually necessary for ICH
- moderate BP reduction to reduce bleeding
- MAP = 110- 130 mm Hg
- CPP > 70 mm Hg
- vasopressor therapy after fluid replacement ifSBP <90 mm Hg
- treat increased ICP (per above)
- reverse or stabilize anticoagulation state
- management of seizures (possibly with prophylactic medication)
- DVT prophylaxis
- surgical intervention based on location of bleed and neurological condition
Stroke (Ischemic)
Pathophysiology
During an ischemic stroke, blood flow to the brain is interrupted because of either a thrombotic or an embolic clot. Regardless of etiology, loss of CBF leads to hypoperfusion of brain cells, ischemic injury to a focal area, and brain death if anoxia is sustained.
A transient ischemic attack (TIA), a sudden, brief neurological deficit resulting from brain ischemia, does not cause permanent damage or infarction. Symptoms depend on the area of the brain affected. Most TIAs last less than 5 minutes and are resolved within hour. A majority are caused by emboli in the carotid or vertebral arteries.
Risk Factors
- atherosclerosis or carotid artery disease
- history of A-Fib
- hypertension
- abdominal obesity
- diabetes
- sickle cell disease
- vasculitis
- tobacco use
- cocaine and amphetamine usage
Physical Examination
- sudden onset of severe headache
- focal neurological signs determined by location and size of the area of ischemia (lesion)
- facial drooping, usually on one side
- numbness, paralysis, or weakness on one side of the body
- arm drift
- slurred speech or inability to speak
- confusion
- vision changes
- dizziness or loss of balance control.
Diagnostic Tests
- priority (interpreted in < 45 minutes); non-contrast CT scan of head to differentiate ischemic from hemorrhagic stroke
- bedside glucose check to rule out hypoglycemia as cause of the symptoms
- National Institute of Health Stroke Scale (NIHSS)
- LOC
- eye deviation (CN HI, IV, VI)
- visual field loss (tests hemianopia and extinction)
- facial palsy
- motor arm (drift)
- motor leg (drift)
- limb ataxia (tests for unilateral cerebellar lesion)
- sensory
- best language (tests for comprehension/aphasia)
- dysarthria (tests for speech ability)
- extinction and inattention (tests for visual/spatial “neglect")
Management
- IV or intra-arterial fibrinolytic therapy (alteplase)
- dosage: 0.9 mg/kg to a maximum of90 mg; first 10% as IV bolus dose over 1 minute, with remaining 90% given as IV infusion over 1 hour
- must be initiated within 3 hours from “last seen normal"; time window expanded to 4.5 hours for eligible patients (<80 years old, no history of diabetes/stroke, NIHSS score <25)
- hypertensive patients: BP should be lowered to <185/110 with anti-hypertensive medication before administration
- aspirin administered >24 hours after alteplase administration
- monitor for side effects, including bleeding, angioedema, ICH, pulmonary edema, DVT, seizure, and sepsis
- mechanical thrombectomy for fibrinolytic-ineligible patients or fibrinolytic-eligible patients with high likelihood of stroke due to LVO; may be done in conjunction with tenecteplase administration
- cardiac monitoring for post-reperfusion dysrhythmias
- regular neurological checks and monitor ICP
- maintain normal body temperature
- maintain blood glucose of140- 180 mL/dL (do not administer D5W)
- supplemental O2 for saturation below 94%
- DVT prophylaxis
Head and Spinal Cord Trauma
ACUTE SPINAL CORD INJURIES
- Spinal cord injuries (SCIs) are injuries to the vertebral column.
- The primary injury is caused by trauma, including compression, hyperextension, contusion, or shearing.
- Secondary injuries are caused by resulting physiological processes such as hypoxia and ischemia; they may lead to neurological dysfunction that presents hours or days after the initial trauma.
- SCIs may be complete (meaning all sensory and motor function is lost below the level of injury) or incomplete (meaning some sensory and motor function is retained).
- The location and severity of sensory/motor loss depends on the type of injury.
- Anterior spinal cord syndrome occurs when the blood flow to the anterior spinal artery is disrupted, resulting in ischemia in the spinal cord and complete loss of motor and sensory function below the lesion.
- Brown-S6quard syndrome is an SCI caused by complete cord hemitransection, typically at the cervical level. Symptoms include ipsilateral motor loss below the lesion and contralateral loss of sensation of pain and temperature.
- Cauda equina syndrome is an SCI typically caused by compression of, or damage to, the cauda equina, the nerve bundle that innervates the lower limbs and pelvic organs, most notably the bladder. Symptoms include sensory loss in the lower extremities, bowel and bladder dysfunction, numbness in saddle area, and loss of reflexes in upper extremities.
- Central cord syndrome is caused by spinal cord compression and edema, both ofwhich cause the lateral corticospinal tract white matter to deteriorate. Symptoms include greater motor function loss in the upper extremities than in the lower extremities and paresthesia in the upper extremities.
- Respiratory compromise due to SCI is determined by lesion level.
TABLE 3.6. Respiratory Compromise in SCIs
|
Level of Lesion |
Description |
|
C1 or C2 (high cervical lesions) |
|
|
C3-C6 |
|
|
T2 - T4 (high thoracic lesions) |
|
|
Below T4-T10 |
|
|
T11 |
|
- Management of SCIs
- goals of management: prevent life-threatening complications, maximize organ system functions, prevent secondary spinal cord damage, and address neurological deficits
- immediate spinal cord stabilization (tongs, halo traction braces, kinetic therapy beds, body casts)
- methylprednisolone (bolus followed by 24- 48 hour infusion)
- monitor for, and treat, cardiac and respiratory complications (both common in SCIs)
- temperature stabilization
- urinary catheterization (to avoid bladder distension)
- Autonomic dysreflexia is the overstimulation of the autonomic nervous system after SCIs above the T6 level. A sympathetic stimulation to the lower portion of the body leads to vasoconstriction below the area of injury and vasodilation above the injury, resulting in bradycardia and hypertension. If left untreated, cardiac status quickly deteriorates, and MI or stroke may occur.
- Symptoms: flushing and sweating above the level of injury; cold, clammy skin below the level of injury; bradycardia; sudden, severe headache; hypertension
- Management: anti-hypertensives; elevate HOB to 90°; have patient empty bladder and bowel; remove tight, restrictive clothing.
Traumatic Brain Injuries
- Traumatic brain injury (TUI) results from a blunt or penetrating blow to the head or from a blast injury.
- Primary injuries are caused by mechanical forces and can cause skull fractures, brain contusions and concussions, lacerations, hemorrhages, hematomas, or damage to white brain matter.
- Secondary injuries occur days or weeks after the TBI event as a result of neurochemical cascades leading to chronic inflammation and vascular changes in the brain.
- The goal of the management of TBI is to maintain CPP and decrease secondary injury to the brain.
- The level of care for skull fractures depends on the type and severity of fracture.
- Nondisplaced fractures generally do well with conservative treatment.
- No treatment is usually required for a linear fracture, especially as the dura mater usually remains intact in adults.
- Surgical decompression for a depressed fracture is necessary only when the depression is greater than the thickness of the skull (if the depression is >6 mm).
- Basilar skull fractures require critical care monitoring and intervention.
- Basilar skull fractures affect the floor of the skull.
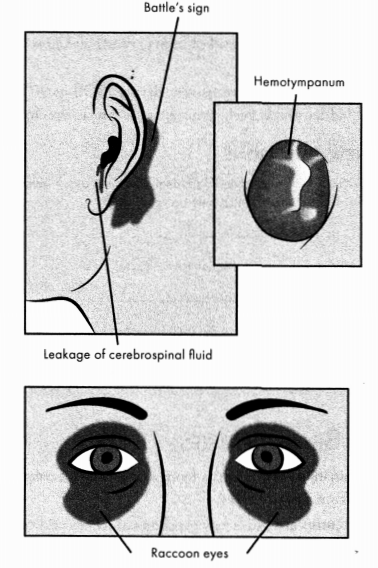
Figure 3.8. Physical Examination of Basilar Skull Fracture
- may cause rupture of meninges, resulting in pneumocephalus
- likely injury to CNI, III, VII, and VIII
- associated spinal cord injury common
- signs and symptoms: Battle signs, raccoon eyes, otorrhea, and rhinorrhea
- management: manage ABCs; manage ICP, hemorrhage, and meningeal injury (as described above); avoid and oral tube, oral
- suctioning, and positive-pressure support
- Diffuse axonal injury (DAI) is a shearing injury that occurs during rapid acceleration-deceleration or rotational acceleration. These forces can shear axons in the brain and cause the death of the brain cells to which they were connected. Sufficient force will disconnect the cerebral hemisphere from the reticular activating system.
- signs and symptoms: coma (GCS <8), decorticate or decerebrate posturing, cerebral edema, increased ICP, temperature elevation
- management: manage ABCs; supportive treatment for symptoms; reduce secondary injury
- An epidural hematoma (EDH) is a traumatic collection of blood between the dura mater and the skull, usually because of a temporal- or parietalregion skull fracture that causes a laceration of the middle meningeal artery.
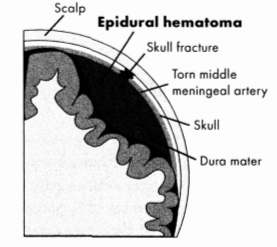
Figure 3.9. Epidural Hematoma
- EDH is a neurosurgical emergency: a rapidly expanding hematoma will increase ICP and quickly progress to uncal herniation of brain tissue.
- Diagnosis: unconsciousness followed by lucid interval with continued deterioration; agitation and confusion; nausea and vomiting; headache; ipsilateral pupil dilation; Cushing's triad; CT. scan or MRI
- Management: manage ABCs; craniotomy or trephination for hematoma evacuation
- A subdural hematoma (SDH) is low-pressure venous bleeding between the dura mater and the arachnoid space. SDH is generally caused either by trauma or by anticoagulation therapy.
- SDH is categorized as acute, subacute, or chronic, based on the rate of bleed, symptom appearance, and rebleeding subsequent to the initial trauma/event.
- Diagnosis: progressive decrease in LOC; headache; confusion; contralateral hemiparesis; increased ICP; ipsilateral pupil dilation; CT scan or MRI
- Management: manage ABCs; craniotomy or trephination for hematoma evacuation
Neurogenic Shock
Pathophysiology
Neurogenic shock is a form of distributive shock caused by an injury or trauma to the spinal cord, typically above T6. The injury causes a decrease in sympathetic tone, leading to vasodilation and rapid onset of hypotension. The resulting decrease in SVR causes blood to pool in the lower extremities, and cardiac output is greatly reduced. Bradycardia occurs because of unopposed vagal tone exacerbated by hypoxia and suctioning (common in spinal injury patients).
Unless rapidly recognized and treated, multisystem organ failure occurs with very high mortality. This shock state may persist for more than a month from the injury event.
Physical Examination
- hemodynamic triad: rapid onset of hypotension, bradycardia, hypothermia
- wide pulse pressure
- skin warm, flushed, and dry
- priapism
Diagnostic Tests
spinal X-ray, CT scan, or MRI to diagnose spinal cord injury
Management
- first-line treatment: IV fluids
- vasopressors and/or inotropes if hypotension persists
- atropine (for bradycardia)
- spine immobilization
Read More