Analyzing your answers to CEN Practice Questions can provide valuable insights.
Neurologic Emergencies CEN Practice Questions - CEN Questions on Neurologic Emergencies
Question 1.
A patient is brought into the emergency department after a spinal cord injury. He is unable to move below the level of the injury. An indwelling urinary catheter is inserted because:
(a) the bladder is areflexic.
(b) the patient is unable to ambulate.
(c) voluntary reflex bladder emptying occurs.
(d) hematuria may be present.
Answer:
(a) the bladder is areflexic.
Rationale:
After a spinal cord injury, the bladder will lose nerve innervation to sense when the bladder is full. The bladder becomes areflexic, which is why many spinal cord-injured patients require straight catheterization or an indwelling urinary catheter. A patient who is unable to ambulate may still be able to urinate. Voluntary reflex bladder emptying may occur at the time of the initial injury to the spinal column, especially if the bladder is full upon injury or trauma but is not a reason to insert a urinary catheter. Hematuria is not always present in a spinal column injury patient and may indicate a urologic injury.
Question 2.
A patient arrives via EMS in full tonic-clonic seizures. His airway is patent and suction is at the bedside. The patient’s phenytoin (Dilantin) level is 3 pg/mL. Normal is 10 to 20 pg/mL. The emergency nurse is ready to infuse phenytoin (Dilantin) 1 g (1,000 mg) via intravenous (IV) line. The emergency nurse should infuse this medication in:
(a) Dextrose 5 % in water as quickly as possible.
(b) 3% normal saline at 75 mL/minute.
(c) 0.9% normal saline at 50 mL/minute.
(d) lactated ringer’s solution at 100 mL/minute
Answer:
(a) Dextrose 5 % in water as quickly as possible.
Rationale:
Phenytoin (Dilantin) must be mixed in normal saline and administered via an intravenous pump at no greater than 50 mg/minute. It can also be mixed in lactated ringer’s solution, but the rate of the infusion is too fast in this option. If phenytoin (Dilantin) is mixed in dextrose, it will crystalize and render the medication and fluid unable to administer.
Never give phenytoin (Dilantin) rapid IV push because it can drop the blood pressure, increase drowsiness, and may cause cardiac dysrhythmias. It would be inappropriate to mix 3% normal saline as this would not routinely be given unless there was an issue with possible head injury or severe hyponatremia and it is not an appropriate diluent for Phenytoin (Dilantin).
Administering phenytoin (Dilantin) often requires a slower rate than the recommended 50 mg/minute because of the pain that it causes the patient. Remember to check with the patient as they may not offer that it is extremely painful. Fosphenytoin (Cerebyx) can be given faster—at 150 mg/minute, and is not venous irritating/painful, so, it is a good alternative for the phenytoin (Dilantin). Both medications must be monitored for hypotension and cardiac dysrhythmias.
Question 3.
A patient presents to the emergency department complaining of pain in her jaw. The emergency nurse notes facial drooping to the corner of the mouth on the left side. Which of the following cranial nerves (CN) is affected?
(a) Cranial nerve VI (Abducens)
(b) Cranial nerve VIII (Acoustic)
(c) Cranial nerve V (Trigeminal)
(d) Cranial nerve III (Oculomotor)
Answer:
(c) Cranial nerve V (Trigeminal)
Rationale:
Cranial nerve V (Trigeminal) deals with facial, cheek, and chin movement. Cranial nerve III (Oculomotor) constricts the pupil and is responsible for helping with eyeball movement. Cranial nerve VI (Abducens) rotates the eyeball outward, and cranial nerve VIII (Acoustic) deals with hearing and balance.
|
Cranial Nerves Mnemonic and Functions |
|||
|
On |
I |
Olfactory |
Smell |
|
Old |
II |
Optic |
Visual acuity, count fingers, and dark vs. light |
|
Olympus |
III |
Oculomotor |
Constricts pupil, opens eyelid, extraocular eye movements (EOMs) |
|
Towering |
IV |
Trochlear |
Look down and outward (EOMs) |
|
Tops |
V |
Trigeminal |
Forehead, cheek, and chin movement and sensation, jaw movement |
|
A |
VI |
Abducens |
Rotates eyeball outward (EOMs) |
|
Fin |
VII |
Facial |
Smile, closes the eyelid, raising eyebrows, facial movement, tears, and saliva production |
|
And |
VIII |
Acoustic (vestibulocochlear) |
Hearing and balance |
|
German |
IX |
Glossopharyngeal |
Swallow and gag reflex |
|
Viewed |
X |
Vagus |
Swallowing, parasympathetic responses of heart, lungs, and abdominal viscera |
|
Some |
XI |
Spinal accessory |
Shoulder shrug and head turning |
|
Hops |
XII |
Hypoglossal |
Tongue movement, speech, and swallowing |
Question 4.
A provider has just asked the patient “How many fingers do you see?” This question is assessing which of the following cranial nerves?
(a) Cranial nerve II (Optic)
(b) Cranial nerve III (Oculomotor)
(c) Cranial nerve IV (Trochlear)
(d) Cranial nerve VI (Abducens)
Answer:
(a) Cranial nerve II (Optic)
Rationale:
Cranial nerve II, the Optic nerve, assesses visual acuity, dark versus light, and the counting of fingers. Cranial nerve III, Oculomotor, gives the eye the ability to constrict the pupils, move the eyeball, and open the eyelid. Cranial nerve IV, Trochlear, allows the eye to look downward and outward and cranial nerve VI, Abducens, assists the eyeball to rotate outward.
The cranial nerves that move the eyeball are CN III, CN IV, and CN VI (Oculomotor, Trochlear, and Abducens). These nerves are responsible for the muscles that innervate the globe. A mnemonic to help remember this is: “3,4,6 makes my eyes do tricks!” PS—Remember this one! You might need to recall it for the test!
Question 5.
During a neurologic examination, the patient is unable to raise his eyebrows or close his eyes tightly against resistance. Which of the following cranial nerves might be damaged?
(a) Cranial nerve II (Optic)
(b) Cranial nerve V (Trigeminal)
(c) Cranial nerve VII (Facial)
(d) Cranial nerve XII (Hypoglossal)
Answer:
(c) Cranial nerve VII (Facial)
Rationale:
The Facial nerve, CN VII, controls facial expression and taste in the anterior two-thirds of the tongue. This nerve has five branches and the temporal branch allows the patient to raise their eyebrows and close their eyes. The other branches are the zygomatic, buccal, mandibular, and cervical. CN II, the Optic nerve, allows the patient to have vision, perceive light, and con-strict the pupil. CN V, the Trigeminal nerve, controls jaw movement and facial sensation. CN XII, the Hypoglossal nerve, controls tongue movement.
Cranial nerves V (Trigeminal),and VII (Facial) should be assessed when dealing with trigeminal neuralgia and Bell’s palsy, CVA, or possible TIA. Bell's palsy is usually manifested by unilateral facial paralysis, inability to close one eye or move facial muscles, drooling, and pain behind the ear. The extremities are not affected. Trigeminal neuralgia is manifested as sudden, severe pains associated with one of the branches of CN V. At times, a "tic" or muscle spasm accompanies the pain. Usually a computed tomography (CT) is performed to rule out stroke.
Question 6.
An 8-month-old presents with a hematoma on his head. According to developmental milestones, which of the following is the most likely explanation for the hematoma?
(a) He fell off a slide while playing.
(b) He fell while pulling up to a standing position.
(c) He climbed out of his crib.
(d) He bumped into a coffee table while walking.
Answer:
(b) He fell while pulling up to a standing position.
Rationale:
Developmental milestones for 7 to 12 months old include pulling themselves up to a standing position and then cruising along a stationary item depending on emerging or advanced skill level. An 8-month-old cannot climb a slide and does not possess the fine motor dexterity, tp climb out of a crib unassisted or walk independently.
Question 7.
A 13-year-old presents with a laceration to the occiput after a fall with numbness and tingling to the extremities. Which of the following is the priority nursing intervention?
(a) Assess the airway while maintaining cervical spine immobilization.
(b) Insert two large-bore IVs and administer a normal saline bolus.
(c) Apply a pressure dressing and obtain a type and crossmatch.
(d) Place the patient on a cardiac monitor and pulse oximetry.
Answer:
(a) Assess the airway while maintaining cervical spine immobilization.
Rationale:
Assessment of the pediatric trauma patient should always begin with inspecting the airway and maintaining cervical spine stabilization. With a presentation of numbness and tingling in the extremities, the patient is at great risk for spinal cord injury. Although intravenous access may be important, there is nothing to indicate that this patient is in need of a normal saline bolus nor is it the first priority for this patient. The dressing may also be necessary, but again there is nothing that indicates the bleeding is uncontrolled requiring blood replacement. The cardiac monitor and pulse oximetry are good care options, but the airway and cervical spine issues are the highest priority.
Question 8.
A 4-month-old presents with decreased feeding and increased somnolence. He has had two episodes of vomiting in the last 3 hours. Vital signs are as follows:
Blood pressure—108/38 mm Hg Pulse—66 beats/mimjte Respirations—30 breaths/minute Temperature—97.0° F (36.1° C)
Which of the following is the most likely cause of these symptoms?
(a) Dehydration
(b) Increased intracranial pressure
(c) Autonomic dysreflexia
(d) Increased intra-abdominal pressure
Answer:
(b) Increased intracranial pressure
Rationale:
Increased intracranial pressure produces ob-servable signs and symptoms depending on the stage of increased pressure. Early signs include headache, nausea and vomiting, altered level of consciousness, and drowsi-ness. Late signs include increased systolic blood pressure, bradycardia, widening pulse pressures, and dilated nonreactive pupils. Hypothermia, bradycardia, and a widened pulse pressure are indicative of increased intracranial pressure. Two episodes of vomiting in 3 hours should not cause these symptoms. Autonomic dysreflexia is a hypertensive emergency and occurs in patients who have a history of spinal cord injuries. There is no indication in the stem of the question to indicate increased intra-abdominal pressure.
Neurologic Signs of Early versus Late Intracranial Pressure (ICP)
Early Signs of Increased ICP
- Restlessness or altered level of consciousness
- Nausea and vomiting (can be with or without nausea)
- Headache
- Amnesia
- Behavioral changes that progress to confusion drowsiness, or impaired judgment
Cushing's Triad - Very LATE Sign of Increased ICP
- Increased systolic BP with widening pulse pressure
- Profound bradycardia
- Abnormal respirations
Other Late Signs of Increased ICP
- Dilated nonreactive pupils
- Unresponsiveness
- Abnormal posturing (flexion, extension, or flaccidity)
Herniation
- Increasing ICP causes herniation ("shift") of brain tissue
- Etiology can be many, that is, tumor, bleeding, and swelling
- All other signs and symptoms of herniation are usually present to some degree
- Altered level of consciousness (LOC), posturing, and vital sign changes
- Uncal herniation—dilated pupils unilaterally or bilaterally
- Central herniation—bilateral constricted pupils
Question 9.
A 5-week-old is brought in by his parents for concern of fever and being inconsolable at home. Upon assessment, the emergency nurse notes that the infant is irritable, exhibits a high-pitched cry, has areas of purpura on his extremities, and has a rectal temperature of 102.0° F (38.9° C). Which of the following are these signs and symptoms most consistent with?
(a) Henoch-Schonlein purpura
(b) Meningococcemia
(c) Idiopathic thrombocytopenic purpura
(d) Kawasaki disease
Answer:
(b) Meningococcemia
Rationale:
Meningococcemia is a potentially life- or limb-threatening clinical entity in which the organism Neisseria meningitidis gains access to the bloodstream. It is characterized by rapid onset of petechiae and purpuric lesions and is spread by oral or nasal droplets. Additional signs and symptoms include irritability, fever/temperature instability, bleeding from puncture sites, tachycardia, poor perfusion, hypotension, gangrene, and tissue necrosis (late). Henoch-Schonlein purpura (HSP) is a disease of the skin, mucous membranes, and sometimes other organs that most commonly affects children following an infectious process such as a throat infection. Palpable purpura (small, raised areas of bleeding underneath the skin), joint pain, and abdominal pain can occur. Chronic kidney disease can follow this disease process. Idiopathic thrombocytopenic purpura (ITP) is a disorder affecting both children and adults that can lead to easy or excessive bruising and bleeding. The bleeding results from unusually low levels of platelets and the cells that help blood clot.
Children often develop ITP after a viral infection and usually recover fully without treatment. In adults, the disorder is often long term. Depending on the level of platelets, manifestations can range from minimal to potentially fatal with internal bleeding. Kawasaki disease affects children and includes fever, rash, swelling of the hands and feet, irritation and redness of the whites of the eyes, and swollen lymph glands in the neck with irritation and inflammation of the mouth, lips, and throat. The effects of Kawasaki disease are rarely serious. The acute phase of the condition commonly lasts 10 to 14 days or more. Most children recover fully. In some cases, Kawasaki disease can lead to long-term heart complications.
Question 10.
A patient presents to the triage desk 20 hours after a motorcycle crash without a helmet. The emergency nurse notes bruising to the mastoid process and periorbital ecchymosis. Which of the following types of head injury is most likely?
(a) Epidural hematoma
(b) Subdural hematoma
(c) Depressed skull fracture
(d) Basilar skull fracture
Answer:
(d) Basilar skull fracture
Rationale:
Battle’s sign (mastoid bruising) and raccoon eyes (periorbital ecchymosis) are signs of a basilar skull fracture and indicates that blood may be leaking into the periorbital and mastoid spaces. These signs do not usually present until 12 to 24 hours after the initial injury to the base of the skull. Epidural hematoma is usually caused by an arterial bleed between the skull and the dura mater because of laceration of the middle meningeal artery with a direct blow to the head. Unconsciousness followed by a lucid period and then rapid change to a decreased level of consciousness are landmark signs of this problem. Subdural hematomas occur more frequently and are characterized by bleeding in the subdural space between the dura mater and arachnoid. Classic presentation results in a venous bleed with loss of consciousness, fixed and dilated pupils with immediate surgical intervention often required. A de-pressed skull fracture would be indicated by a depression in the integrity of the skull with soft tissue injury.
This is an excellent example of reading the question very closely for small clues. The major clue here is that the patient arrived “20 hours after a motorcycle crash without a helmet. ” That points to the answer of basilar skull fracture with the presenting manifestations.
Question 11.
Which of the following patients is most at risk for a diagnosis of encephalitis?
(a) A 16-year-old with nuchal rigidity and a headache. He has not had a tetanus immunization since his childhood immunizations.
(b) A 4-year-old with nuchal rigidity and a headache. She is behind in her immunization schedule and is recovering from chicken pox.
(c) An 8-year-old with a recent history of a viral illness and has been being medicated with aspirin for fever control.
(d) A 9-year-old with a recent history of a viral illness diagnosed as measles. No medication has been used in this child.
Answer:
(d) A 9-year-old with a recent history of a viral illness diagnosed as measles. No medication has been used in this child.
Rationale:
Acute encephalitis (inflammation of the brain parenchyma) can be caused by bacterial, viral, or parasitic infections and can be seen in children with systemic infectious childhood illnesses such as measles. It occurs more often in children less than 10 years of age. Children who take aspirin with a viral illness are at increased risk of presenting with Reye’s syndrome. Reye’s syndrome is rarely seen today because education of the risk of using aspirin products during viral illnesses has been greatly appreciated. Any child with fever and nuchal rigidity should be placed on droplet precautions until a diagnostic lumbar puncture (LP) can be completed to rule out meningitis. Immunization history is not relevant in these situations.
Question 12.
A young adult presents to the emergency department complaining of numbness and paresthesia of her hands and feet, as well as lower leg muscle weakness. She works as a child care provider and had a recent viral illness. Which of the following disease processes is the highest probability for this patient?
(a) Myasthenia gravis
(b) Guillain-Barre syndrome
(c) Botulism poisoning
(d) Organophosphate poisoning
Answer:
(b) Guillain-Barre syndrome
Rationale:
Guillain-Barre syndrome is an acute idiopathic poly-neuropathic disorder affecting the motor component of the peripheral nerves. It affects people between the age of 16 and 30 years of age and over 50% of those affected have had a recent viral illness. Classic presentation is ascending, bilateral weakqess progressing from the extremities upward and inward. Myasthenia gravis is a chronic autoimmune disorder caused by a defect in neuromuscular transmission occurring more frequently in women also between the ages of 20 and 30 years of age.
Ocular dysfunction is the most common initial symptom ptosis (eyelid drooping), diplopia with sustained directional gaze, and difficulty keeping the eye closed, BoTulism poisoning presents after ingestion, inhalation, or wound contamination with botulism toxin. Patient presentation includes symmetrical descending flaccid paralysis with ptosis and blurred vision, which then progresses to flaccid paralysis and respiratory distress. Organophosphate poisoning is an acetylcholinesterase inhibitor disrupting and blocking the effects of acetylcholinesterase. Presentation includes skeletal muscle twitching, cramping, flaccid paralysis, tachycardia, pinpoint pupils (miosis), diaphoresis, hypersecretion of the salivary glands, lacrimal glands, sweat, and bronchial glands, nausea, vomiting, and diarrhea.
Organophosphate poisoning occurs with bug sprays and also with sarin gas. This is a cholinergic crisis that is “wet. ” A mnemonic to help remember the manifestations of this process are:
SLUDGEM
Salivation and increased secretions
Lacrimation
Urinary incontinence
Defecation incontinence (diarrhea)
Gastroesophageal effects (nausea, vomiting, and
diarrhea)
Miosis (pinpoint pupils)
Question 13.
Four patients with the complaint of headache present to the triage desk within minutes of each other. Which of the following statements made by these patients would indicate the most emergent situation?
(a) “I have a throbbing headache that’s been coming on for several days. Can you turn off the lights?”
(b) “This terrible headache hit me so quick while I was watching TV. It’s getting worse and now I’m throwing up.”
(c) “1 have a really bad headache and my neck hurts. I’ve been so stressed lately.”
(d) “I tripped over a rug and have a laceration on my head. It bled a lot and sure hurts.”
Answer:
(b) “This terrible headache hit me so quick while I was watching TV. It’s getting worse and now I’m throwing up.”
Rationale:
The timing of onset of symptoms with progressing severity of symptoms should be considered higher acuity. A patient with sudden onset of headache and vomiting should be considered high priority as this may be indicative of pathophysiologic events such as herniation or subarathnoid hemorrhage. A throbbing headache with photophobia is indicative of a classic migraine. A bad headache in the occipital/neck area may also be indicative of a migraine or a tension type of headache. Head lacerations usually bleed quite a bit because of the vascularity of the head. This option indicated that the bleeding had stopped at this time.
From a triage standpoint, always consider a sudden onset—especially one that is like a “thunderbolt”— and pain of highest intensity, to be a possibility for grave consequences.
Question 14.
Which of the following are typical signs of increased intracranial pressure?
(a) Decreased pulse rate and decreased respiratory rate
(b) Numbness of fingers and decreased temperature
(c) Increased pulse rate and decreased blood pressure
(d) Decreased mentation and increased respiratory rate
Answer:
(a) Decreased pulse rate and decreased respiratory rate
Rationale:
Cushing’s triad/response is a late sign of increased intracranial pressure and includes: reflex bradycardia, high systolic or widened pulse pressure and breathing abnormalities, which can result in a decreased respiratory effort. Numbness of the fingers and decreased temperature are not associated with increased intracranial pressure. A decreased level of consciousness (mentation) would occur in increased intracranial pressure but not the increased respiratory rate.
The response to increase in blood pressure when intracranial pressure is increasing occurs automatically to maintain cerebral perfusion pressure (CPP). It is a response to the formula, CPP = MAP - ICP. MAP is mean arterial pressure and ICP is intracranial pressure. The body must maintain a cerebral perfusion pressure of at least 60 mm Hg in order to perfuse the brain. The blood pressure increases to maintain the CPP when intracranial pressure is increased.
Question 15.
A patient suffered a thoracic-level spinal injury from a diving accident. To initiate cardiopulmonary resuscitation (CPR) at the poolside, which of the following measures would be most important?
(a) Hyperextend the neck to clear the airway before mouth-to-mouth resuscitation.
(b) Administer CPR in a prone position.
(c) Do not administer CPR after a head injury.
(d) Elevate the mandible with a jaw thrust to assess airway with the head in a neutral position.
Answer:
(d) Elevate the mandible with a jaw thrust to assess airway with the head in a neutral position.
Rationale:
Initiating CPR starts with opening the airway. Jaw thrust is the most effective way to open the airway in a patient with a suspected spinal cord injury. CPR cannot be effectively administered in a prone position, and many patients with a catastrophic head injury in association with a spinal injury who present in cardiopulmonary arrest may require CPR. Cervical spine injury should be considered until proven otherwise thus hyperextending the neck would not be recommended.
Question 16.
A paraplegic patient presents to the emergency department complaining of a headache. He is noted to be flushed and is sweating profusely. Which of the following should be the first action for this patient?
(a) Apply compression stockings.
(b) Lower his head to increase cerebral circulation.
(c) Massage lower extremities to cause vasodilation.
(d) Assess for a bjpcked urinary catheter.
Answer:
(d) Assess for a bjpcked urinary catheter.
Rationale:
This patient is demonstrating manifestations of autonomic dysreflexia. This is the sudden onset of an abnormal sympathetic nervous system response to a noxious stimuli such as a full bladder, full rectum, or pressure on an ulcer. The symptoms include bradycardia, hypertension, headache, flushing, and exces-' sive sweating. Emergency treatment involves raising the head of the bed and loosening any constricting clothing.
If compression stockings are present on the patient, they should be removed to encourage venous pooling. The most important intervention for this response is to resolve the offending stimulus. Assess for G-I or G-U-related situations. Often irrigation of a urinary catheter or unkinking the tubing may relieve the sympathetic response. Enemas or removal of an impaction may be necessary. Antihypertensives can be given, but the hypertension will not resolve until the stimulus has been removed.
Question 17.
Which of the following would be the first intervention when assisting a patient experiencing a tonic-clonic seizure?
(a) Place a tongue blade between the patient’s teeth.
(b) Restrain the patient from all movements to avoid injury.
(c) Turn the patient onto their side and observe them.
(d) Protect the patient from hitting their arms against close objects.
Answer:
(c) Turn the patient onto their side and observe them.
Rationale:
The most important measure to take when assisting a person who is actively seizing is to ensure airway patency and prevent further injury. The patient should be rolled onto their” side to facilitate drainage of secretions from the airway. The extremities and head should be protected from injury, but the patient should be turned first. Motor activity should be monitored and length of time of the seizure activity should be noted. Placing a tongue blade or mouth block may cause more injury. Restraining the patient is not appropriate
Many times, there seems to be two appropriate an-swers for the question. Always choose the one that has to do with airway!
Question 18.
Which of the following would be the primary nursing goal when caring for a 4-year-old with meningitis?
(a) Increase stimulation opportunities to prevent coma.
(b) Provide an opportunity for therapeutic play.
(c) Reduce the pain related to nuchal rigidity.
(d) Place a urinary catheter to monitor urine output.
Answer:
(c) Reduce the pain related to nuchal rigidity.
Rationale:
In addition to treating infection and minimizing exposures, pain management is a high priority. Minimizing pain contributes to reducing increased metabolism, glucose utilization, and intracranial pressure. You would not want to increase stimulation to the child because this will increase metabolic demands and glucose needs. Measuring urine output is important but a urinary catheter should not be placed unless it is absolutely necessary due to the potential of introducing another focus of infection.
Question 19.
A 1-year-old girl has experienced a febrile seizure. Which of the following statements made by the parents would indicate that they understood the discharge instructions regarding temperature control?
(a) “We will use alcohol baths if her temperature gets too high.”
(b) “We will keep her temperature down with tepid sponge baths and acetaminophen (Tylenol).”
(c) “We will give her the phenobarbital when the temperature is above 101° F (38.3° C).”
(d) “We will use ice baths if her temperature goes up and we cannot get it to come down.”
Answer:
(b) “We will keep her temperature down with tepid sponge baths and acetaminophen (Tylenol).”
Rationale:
Between 25% and 30% of children who have suffered a febrile seizure may have reoccurrences. Keeping the temperature from increasing rapidly may contribute to the prevention of febrile seizures. Tepid sponge bath, administering antipyretics, and increasing fluid intake during febrile illnesses are key to preventing febrile seizures. An ice bath is too cool to bring the temperature down and the temperature should be brought down slowly by using tepid water between 60° F and 100° F (16° C to 38° C). Alcohol baths was an accepted form of temperature control in years past, but it was then realized that the alcohol could be absorbed through the skin, causing alcohol poisoning. Phenobarbital does not affect temperature.
Question 20.
A patient presents with a known history of migraine headaches. The emergency nurse prepares for which of the following treatment regimens?
(a) IV fluid bolus, antiemetic, and Morphine
(b) IV fluid bolus, hydromorphone (Dilaudid), and antiemetic
(c) Antihistamine, antiemetic, and IV fluid bolus
(d) Antihistamine, Nitroglycerin sublingual, and IV fluid bolus
Answer:
(c) Antihistamine, antiemetic, and IV fluid bolus
Rationale:
Over 23 million patients suffer from migraine headaches. Current treatment standards for patients with migraine headaches include providing hydration (oral or intravenous), antiemetics (ondansetron hydrochloride [Zofran]), and/or antihistamines (intravenous diphenhydramine or Benadryl), and NSAIDS [Ibuprofen, Motrin]). Narcotic analgesics should be avoided because of the possibility of a rebound headache and addiction. Nitroglycerin sublingual should be avoided because of the vasodilatory affect, which can increase the intensity of the headache.
Question 21.
When asking health history questions about the child admitted with Reye’s syndrome, which of the following would be considered a common finding?
(a) Parental administration of acetaminophen for fever
(b) Recent streptococcal infection
(c) Recent sickle cell crisis
(d) Recent influenza illness with aspirin administration
Answer:
(d) Recent influenza illness with aspirin administration
Rationale:
The characteristic presentation of a child with Reye’s syndrome is use of salicylates during a viral illness, followed by mental status change and evidence of fatty deposits in the liver. Sickle cell crisis is often triggered by stress, illness, extreme changes in temperature (cold weather), or infection, but is not associated with Reye’s syndrome. Acetaminophen (Tylenol) use or bacterial streptococcal infection has not been linked to Reye’s syndrome. Influenza-like illnesses or viral conditions should be treated with antipyretics such as acetaminophen or Tylenol.
Early manifestations of Reye’s syndrome are lethargy and vomiting, which is associated with encephalopathy. These symptoms usually occur within the first 2 days of the illness.
Question 22.
An infant with a high-pitched cry, irritability, and fever is being prepped for a lumbar puncture (LP). Which of the following is an appropriate position for this patient during this procedure?
(a) Lateral with knees to chest and chin to chest
(b) Lateral with legs extended and arms above the head
(c) Placing the patient in the prone position
(d) Placing the patient in the supine position
Answer:
(a) Lateral with knees to chest and chin to chest
Rationale:
Optimal positioning for a lumbar puncture in an infant is sitting upright or on their side with knees flexed and chin to chest. Older children or adults may be sitting on the side of the bed, leaning over a bedside table. A prone position is not appropriate and the supine position would not provide access to the spinal area. The child or infant would have to be in a curled position in order to access the proper location for needle insertion.
Remember that all children and infants should be monitored very closely during this procedure because of the positioning. Watch respirations and' pulse oximetry.
Question 23.
A patient with suspected bacterial meningitis had a lumbar puncture (LP) with cerebral spinal fluid (CSF) sent to the laboratory for evaluation. The emergency nurse would suspect which of the following laboratory values?
(a) Increased WBC, increased protein, and decreased glucose
(b) Increased WBC, increased protein, and increased glucose
(c) Decreased WBC, decreased protein, and increased glucose
(d) Decreased WBC, decreased protein, and decreased glucose
Answer:
(a) Increased WBC, increased protein, and decreased glucose
Rationale:
Characteristics of CSF with bacterial meningitis include elevated WBC, elevated protein, decreased glucose, and positive gram stain with turbid or cloudy CSF. Bacterial meningitis can be fatal in 50% of patients. Common agents include Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae, or group B streptococci, and Listeria monocytogenes.
|
Type of Meningitis |
CSF Pressure |
Protein |
Glucose |
WBC |
|
Bacterial |
↑ Elevated |
↑ Elevated |
↓ Decreased |
↑ Increased (>1,000 cells/pL) |
|
Viral |
Normal (may be mildly increased) |
↓ Decreased |
Normal |
↑ Increased (10-1,000 cells/pL) |
Question 24.
A patient presents with hemiplegia that started 1 hour before arrival. A computed tomography (CT) scan of the head is negative and the physician has ordered administration of tissue plasminogen activator (TPA/ Activase). The emergency nurse knows that which of the following is the maximum dose of TPA?
(a) 80 mg
(b) 90 mg
(c) 120 mg
(d) No maximum, because the dosage is based on weight.
Answer:
(b) 90 mg
Rationale:
TPA is administered as a weight-based dose of 0.9 mg/kg, but with a maximum dose of 90 mg in the patient presenting with a stroke. TPA is the only thrombolytic approved for use in stroke patients.
Be cautious with computer-generated ordering and medication screens. Near misses have occurred because of wrong orders being “clicked” and pharmacy errors regarding placing a “stop” on the dose at 90 mg!
Question 25.
Receptive aphasia results from damage to which area of the brain?
(a) Parietal lobe
(b) Occipital lobe
(c) Temporal lobe
(d) Frontal lobe
Answer:
(c) Temporal lobe
Rationale:
The temporal lobe contains the auditory as-sociation area. If this area is damaged in the dominant hemisphere, the patient hears words but does not know their meaning. It is also associated with memory.
Damage to the parietal lobe affects the patient’s ability to identify special relationships with the environment. This has to do with sensory information that is obtained through the sense of touch. It also is a focus for the sensation of pain. When damaged, the occipital lobe affects visual associations; therefore, the patient can visualize objects but cannot identify them. The frontal lobe acts as the center for the ability to reason and express the spoken word, to understand right from wrong, cognition, and socialization skills.
Question 26.
During neurosurgical evaluation of an unresponsive patient, the physician evaluates the oculocephalic reflex (doll’s eye phenomenon). When the head is rotated to the left, the patient’s eyes also move to the left. What does this finding indicate?
(a) No abnormality
(b) Damage to Cranial Nerve I (Olfactory)
(c) Damage to the fovea
(d) A lesion on the brain stem
Answer:
(d) A lesion on the brain stem
Rationale:
Evaluation of brain stem function can be done in an unconscious patient by testing the oculo- cephalic reflex. When the patient’s head is rotated, the eyes should move in a direction opposite to the head movement. Brain stem damage is indicated if the eyes move in the same direction as head movement. Cranial nerve I is the olfactory nerve; damage to this nerve results in the inability to identify odors. The fovea is the center of the retina’s macula, the area of greatest visual acuity.
Evaluation of this reflex is contraindicated in a patient with suspected cervical spine injury or who has not had the cervical spine cleared.
Assessment Technique for the Oculocephatic Reflex
1. Briskly rotate the head from side to side, or
2. Briskly flex and extend the neck
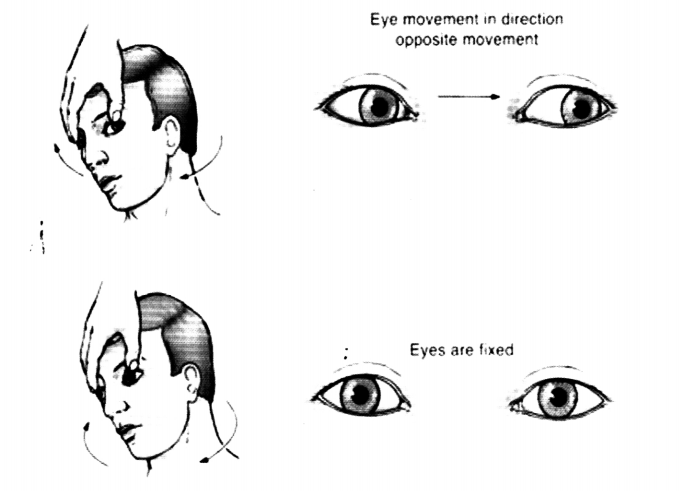
Findings
- When the head is rotated, the eyes should move in the ovecton opposite to the head movement top (If the head is rotated to the left, the eyes appear to move to the right) Alternative method When the neck is hexed, the eyes appear to look upward, when the neck is extended, the eyes look downward
- When the dolls eye reflex is absent, the eyes do not move in the sockets and thus fofiow the directon of passive rotation
Loss of the ocuiocephasc reflex in the comatose patient indicates a leson at the pontine- m«SKam level of the brainstem
Reprinted with permission from Hickey, J. (2013). Clinical practice of neurological & neurosurgical nursing (7th ed.). Philadelphia, PA: Wolters Kluwer Health.
Question 27.
Which of the following would be the primary intervention for a patient complaining of headache and neck pain and does not recall events leading up to his arrival in the emergency department? On arrival, the patient has a Glasgow Coma Scale of 14. A hematoma is palpated from the occipital to the frontal skull areas.
(a) Perform a complete head-to-toe assessment.
(b) Apply cervical immobilization.
(c) Administer opioid analgesics for complaints of pain.
(d) Obtain a specimen to determine blood alcohol level.
Answer:
(b) Apply cervical immobilization.
Rationale:
Immobilization of the head and neck reduces the risk of further damage to the cervical spine. This patient arrived with a large hematoma to his head, which indicates some type of trauma. All patients with suspected head and neck trauma should be immobilized until all seven cervical vertebrae are cleared by radiograph visualization or computed tomography (CT). A complete head-to-toe assessment (secondary survey) should be performed after CT (computed tomography) scan or radiologic examination. Airway, breathing, and circulation are assessed as the cervical spine is immobilized, and the patient is evaluated for potential life-threatening injuries (primary survey).
Administering opioid analgesics to a patient with altered mental status or head injuries is not a primary intervention because opioids can increase respiratory depression and hypotension in patients with head injury. Obtaining a specimen for blood alcohol level helps determine the amount of alcohol the patient has consumed and its possible relationship with the patient’s level of consciousness. Although this is useful information, it is not a primary intervention.
Question 28.
Thirty minutes after a patient is admitted to the emergency department, the emergency nurse performs a repeat neurologic examination. The patient does not follow commands, but after several attempts by the nurse to apply noxious stimuli, he opens his eyes and moves the nurse’s hand. The patient utters a one-word response to the nurse. Which of the following is the correct Glasgow Coma Scale for this patient?
(a) 5
(b) 7
(c) 10
(d) 12
Answer:
(c) 10
Rationale:
This patient is given 5 points for purposeful movement to pain (motor), 3 points for inappropriate words (verbal), and 2 points for eye opening in response to painful stimuli. The total score is 10. Remember! The lowest score on a Glasgow Coma Scale is 3—not 0! Highest potential scoring is 15.
Reprinted with permission from Leonard, L. S. (2017). The Washington manual of emergency medicine (1st ed.). Phila-delphia, PA: Wolters Kluwer Health.
Question 29.
Which of the following signs and symptoms would indicate the presence of a spinal cord injury?
(a) Hypertension with tachycardia
(b) Numbness and tingling in the extremities
(c) Cloudy cerebrospinal fluid (CSF)
(d) Presence of exophthalmos
Answer:
(b) Numbness and tingling in the extremities
Rationale:
A patient with possible spinal cord injury typically complains of numbness and tingling in the extremities or an inability to detect sensation. Bradycardia and hypotension would be expected with spinal cord injury not hypertension and tachycardia. Cloudy CSF is associated with bacterial infections such as meningitis. Exophthalmos is an abnormal protrusion of the eyeball associated with orbital tumors, thyroid disorders, and orbital cellulitis.
Question 30.
Which of the following conditions indicates an ovoid-shaped pupil?
(a) Traumatic orbital injury
(b) Intracranial hypertension
(c) History of cataract surgery
(d) Pontine hemorrhage
Answer:
(b) Intracranial hypertension
Rationale:
An ovoid pupil is the midpoint between a normally round pupil and a fully dilated and fixed pupil and is a sign of increased intracranial pressure.
Traumatic orbital injury results in a jagged-appearing pupil or a tear-drop-shaped pupil as with a globe rupture.
A keyhole-shaped pupil is common in patients who have had an iridectomy as part of cataract surgery. A pontine hemorrhage causes the pupils to be pinpoint.
Question 31.
A patient receiving pharmacologic medications for combativeness associated with a head injury responds to noxious stimuli only. Which of the following scores on the Ramsay Score for Sedation (RASS) would be documented?
(a) 1
(b) 3
(c) 5
(d) 15
Answer:
(c) 5
Rationale:
The modified Ramsay Score for Sedation (RASS) measures the level of sedation achieved with pharmacologic agents. A Ramsay score of 5 suggests that the patient responds only to noxious stimuli. A patient who is anxious, agitated, or restless has a Ramsay score of 1. A patient who is cooperative, tranquil, and oriented has a score of 2. A patient who responds to voice and verbal commands has a Ramsay score of 3. A patient who responds to gentle shaking scores a 4. A patient who shows no response to noxious stimuli is considered a 6 on the scale. The scale ranges from 1 to 6 only.
Question 32.
In an adult patient with head injuries, which of the following medications can be administered before sedating the patient with succinylcholine (Anectine)?
(a) Atropine
(b) Ketamine (Ketalar)
(c) Lidocaine (Xylocaine)
(d) Meperidine (Demerol)
Answer:
(c) Lidocaine (Xylocaine)
Rationale:
Succinylcholine is a neuromuscular-blocking agent that can increase intracranial pressure (ICP) in a patient with head injuries. Administering 1 mg/kg of lido- caine provides ICP control. Atropine is the prpmedication of choice for children receiving succinylcholine because it decreases the bradycardia that occurs with succinylcholine administration. Ketamine and meperidine are contraindicated in a patient with head injuries because they increase ICP.
There is some controversy regarding the use of li- docaine as a pretreatment because of inconsistent studies. It is an accepted practice.
Question 33.
Which of the following assessment findings would be associated with a patient with an intracranial pressure (ICP) reading of 35 mm Hg?
(a) Narrowed pulse pressure
(b) Hypothermia
(c) Cheyne-Stokes respirations
(d) Kussmaul’s respirations
Answer:
(c) Cheyne-Stokes respirations
Rationale:
Normal ICP should be less than 0 to 20 mm Hg. Widening pulse pressure, hyperthermia, and Cheyne- Stokes respirations are signs of increased ICP. Kussmaul’s respirations are associated with diabetic ketoacidosis.
Different books may provide different numbers on normal values such as intracranial pressure readings. One book may document it as 0 to 20, whereas another will state 0 to 15. They are usually close together and neither are necessarily incorrect.
Question 34.
Which of the following interventions will decrease elevated intracranial pressure (ICP)?
(a) Frequent suctioning of the airway
(b) Administering morphine for pain
(c) Maintaining the patient in trendelenburg position
(d) Administering mannitol (Osmitrol)
Answer:
(d) Administering mannitol (Osmitrol)
Rationale:
Mannitol is an osmotic diuretic that decreases intracranial pressure (ICP). Suctioning the patient’s airway should be minimized to prevent increased ICP. Morphine should be used cautiously in a patient with a head injury or increased ICP because the drug’s respiratory depressant effects are considerably enhanced in these situations. A patient with a head injury should have his head elevated 30 degrees to promote venous drainage. Placing a patient in trendelenburg position obstructs venous return from the brain and increases ICP.
Question 35.
Which of the following is NOT an early symptom of multiple sclerosis (MS)?
(a) Diplopia
(b) Scotomas
(c) Weakness
(d) Paralysis
Answer:
(d) Paralysis
Rationale:
Paralysis is a late symptom of multiple sclerosis (MS). The earliest clinical signs of MS may be vague, such as weakness, numbness, or tingling in limbs; visual blurring; or urinary changes. Motor symptoms initially present as weakness and then progress to paralysis. Diplopia (double vision) or scotoma (area of depressed vision in the visual field) may also present early in the disease.
Multiple sclerosis is a disease process that affects the myelin sheath of the central nervous system. Guillain-Barre syndrome affects the myelin sheath of the peripheral nervous system.
Question 36.
A patient is brought to the emergency department by ambulance with a chief complaint of lethargy. Two days before the patient was in a high-speed motor vehicle accident and refused care. Since that time, she has complained of headaches and drowsiness. Her friend states that it has now become difficult to wake her up. Assessment reveals a right pupil that is fixed and dilated with papilledema present. The Glasgow Coma Scale score is 8. Which of the following types of injury does this patient exhibit?
(a) Subdural hematoma
(b) Epidural hematoma
(c) Diffuse axonal injury
(d) Postconcussion syndrome
Answer:
(a) Subdural hematoma
Rationale:
A subdural hematoma, occurring between the dura mater and the arachnoid layer of the meninges, is bleeding that causes direct pressure to the surface of the brain. Signs and symptoms appear within 48 hours (acute) and can be delayed as long as several months (chronic). Symptoms of an epidural hematoma include a history of momentary loss of consciousness followed by a lucid period after which the patient’s mental status deteriorates rapidly due to the presence of bleeding from the middle meningeal artery. The clinical manifestations of a diffuse axonal injury are immediate and prolonged coma with decorticate or decerebrate posturing. Manifestations of postconcussion syndrome include headache, dizziness, irritability, poor judgment, and insomnia.
When patients arrive in the ED with a headache, always ask if they have fallen and hit their head within the past 2 to 3 months. The term “chronic subdural hematoma” occurs at later dates as the vessels bleed a little at a time. Hvo patients who are at increased risk for this are the geriatric patient and the alcoholic because of their smaller brain mass (atrophy occurs with both of these) and their tendency to fall. Those on blood thinners are at even higher risk. Think of these things when assessing patients at either the triage area or as the primary nurse.
Question 37.
Which of the following areas of the brain controls the respiratory and cardiac systems?
(a) Medulla
(b) Frontal lobe
(c) Diencephalon
(d) Hypothalamus
Answer:
(a) Medulla
Rationale:
The medulla controls the arterioles, the blood pressure, and the rate and depth of respirations. Severe injury to this area generally results in death. The medulla also controls yawning, coughing, vomiting, and hiccoughing. The frontal lobe of the cerebrum controls personality, judgment, thought, and logic. The diencephalon contains the thalamus, which is the sensory pathway between the spinal cord and the cortex of the brain. The hypothalamus regulates body temperature, appetite, and sleep.
Question 38.
Which of the following is a potential complication when utilizing succinylcholine (Anectine) for rapid sequence intubation (RSI) in a patient diagnosed with Guillan-Barre?
(a) Hypernatremia
(b) Hyperkalemia
(c) Hypokalemia
(d) Hyponatremia
Answer:
(b) Hyperkalemia
Rationale:
Hyperkalemia can occur if succinylcholine (Anectine) is used for the induction of rapid sequence intubation in the patient with Guillain-Barre and in the later stages of those with spinal cord injuries, bums, and strokes. The uptake of acetylcholine at the neuromuscular junction is increased in these disease processes as well as the medication, succinylcholine. This allows for the release of potassium and can cause a fatal hyperkalemia. Those patients who have disease processes that lend toward increased potassium levels can also be at risk, such as renal failure, large crush injuries, or even digitalis toxicity. Sodium is not affected by this medication and disease processes.
Question 39.
Which of the following head injuries results in a collection of blood between the skull and the dura mater?
(a) Subdural hematoma
(b) Subarachnoid hemorrhage
(c) Epidural hematoma
(d) Contusion
Answer:
(c) Epidural hematoma
Rationale:
An epidural hematoma results from blood collecting between the skull and the dura mater. A subdural hematoma is commonly caused by trauma or violent shaking (shaken baby syndrome) and results in a collection of venous blood between the dura mater and the arachnoid mater. A subarachnoid hemorrhage is a collection of blood between the pia mater and the arachnoid membrane.
A contusion is a bruise on the surface of the brain.
Question 40.
A mother brings her 1-year-old child, who fell down the stairs 2 hours ago, to the emergency department. The child is dirty and wearing clothing that is inappropriate for the cold weather. The child cries when the head and neck are palpated. Bruises at various stages of healing are noted on the buttocks and back. As the physician enters the room, the child begins seizing. This child should be evaluated for which of the following conditions?
(a) Coagulation disorder
(b) Meningitis
(c) Subdural hematoma
(d) Leukemia
Answer:
(c) Subdural hematoma
Rationale:
This child has classic signs of a traumatic head injury such as subdural hematoma, which is caused by venous bleeding between the dura and the arachnoid layers. This injury is frequently associated with child abuse. A patient with a history of coagulation or hematologic disorders may present with ecchymosis, petechiae (in platelet disorders), or purpura. Meningitis is associated with lethargy, irritability, fever, seizures, and headache. Petechiae and purpura are present in meningococcemia.
When assessing any patient, the history, psychological findings, and patient’s overall appearance must also be considered to determine whether the signs and symptoms are consistent with the patient/caregiver's history. Remember that we need to focus on the “chief complaint, ” but we also must look at our patients holistically!
Question 41.
A patient with a diagnosis of ischemic stroke is being prepped for the initiation of tissue plasminogen activator (TPA). The patient is on the cardiac monitor. Oxygen has been applied at 2 L/nasal cannula. Labetalol (Normodyne) 5 mg intravenous was administered. A light, warm blanket has been applied. Which of the following would indicate that proper interventions have been completed that allow for the administration of this medication?
(a) Pulse rate of 120 beats/minute
(b) Blood pressure of 168/98 mm Hg
(c) Pulse oximetry reading of 94%
(d) Temperature of 98.6° F (37° C)
Answer:
(b) Blood pressure of 168/98 mm Hg
Rationale:
According to the stroke guidelines for care, a systolic blood pressure above 180 mm Hg requires treatment before the initiation of TPA. Labetalol (Nor- modyne) was given before with a blood pressure now of 168/98 mm Hg, which demonstrates that the Labetalol (Normodyne) was successful in lowering the systolic pressure below 185 mm Hg. A systolic blood pressure that remains above 185 mm Hg is a contraindication to TPA initiation. Acceptable pressures are systolic below 185 mm Hg and diastolic below 110 mm Hg.
Uncontrolled hypertension increases the risk of intracranial bleeding. Tachycardia would not necessarily contraindicate the administration unless it was associated with bleeding/hypovolemia. The pulse oximetry reading and temperature are not included in the criteria, although it is recommended to supplement for Sa02 below 94%. Hyperthermia can increase the morbidity rate, but in this scenario, the temperature is normal and a light, warm blanket was applied for patient comfort.
Other exclusion criteria are head trauma, previous recent stroke or intracranial bleed, and laboratory tests that indicate bleeding potential (platelets, international normalized ratio [INR], protime). Other considerations include resolving symptoms, recent surgery, recent gastrointestinal hemorrhage, recent myocardial infarction, and seizure at onset of event.
Question 42.
Which of the following would be an ominous sign in a 1-year-old child with a possible neck injury?
(a) Heart rate of 60 beats/minute
(b) Respiratory rate of 30 breaths/minute
(c) Capillary refill time of 3 seconds
(d) Positive Babinski’s reflex
Answer:
(a) Heart rate of 60 beats/minute
Rationale:
The normal heart rate for a 1-year-old child ranges from 90 to 120 beats/minute. Bradycardia is a sign of increasing intracranial pressure. Normally, respirations for a child of this age range from 20 to 30 breaths/minute. Capillary refill time less than or equal to 3 seconds is a normal finding. For children below the age of 2, a positive Babinski’s reflex is a normal finding.
Question 43.
While caring for a patient with a ventriculostomy, the emergency nurse notices that the intracranial pressure (ICP) reading is 30 mm Hg. The emergency nurse assesses the patient and the ICP monitor and determines that the drain is open. Which of the following would be the appropriate immediate intervention for this patient?
(a) Move the head from a rotated position to the midline.
(b) Lower the head of the bed to the Trendelenburg position.
(c) Close the stopcock on the ventriculostomy.
(d) Elevate the head of the bed to high Fowler’s position.
Answer:
(a) Move the head from a rotated position to the midline.
Rationale:
A rotated head position will prevent venous outflow via the jugular veins and contribute to increased intracranial pressure (ICP). The head of the bed should be maintained at 30 degrees, and hyperextension, flexion, and rotation of the head should be avoided. Placing the patient in Trendelenburg position by lowering the head of the bed would increase the pressure on the brain. Closing the stopcock on the ventriculostomy causes the ICP to rise because there is no longer an outlet for the cerebrospinal fluid (CSF).
Question 44.
A patient involved in a 20-foot fall sustains a fracture with spinal cord transection at the level of C6. This injury will result in which of the following findings?
(a) Quadriplegia with diaphragmatic breathing and gross arm movements
(b) Quadriplegia with total loss of respiratory function
(c) Paraplegia with variable loss of intercostal and abdominal muscle use
(d) Paraplegia with loss of bowel and bladder function
Answer:
(a) Quadriplegia with diaphragmatic breathing and gross arm movements
Rationale:
A patient with an injury at C6 will have quadriplegia with diaphragmatic breathing and gross motor arm movements. The patient may also suffer from hypotension and an atonic bladder. An injury at level C2 results in total loss of respiratory function and - movement from the shoulders down. Paraplegia with loss of portions of intercostal and abdominal muscles is indicative of injury at Tj to L2. An injury below L2 results in mixed motor sensory loss and bowel and bladder dysfunction.
Question 45.
All of the following can be used fdr blood pressure control for the cerebral vascular accident (CVA) patient EXCEPT:
(a) Nicardipine (Cardene)
(b) Nitroprusside (Nipride)
(c) Labetalol (Normodyne)
(d) Cardizem (Diltiazem)
Answer:
(d) Cardizem (Diltiazem)
Rationale:
Cardizem is typically used to treat tachycardia, such as that associated with atrial fibrillation with a rapid ventricular rate. Nicardipine (Gardene), nitroprusside (Nipride) and labetalol (Normodyne) are all agents used to reduce blood pressure in ischemic stroke.
Question 46.
Which of the following statements made by a patient being discharged with a new prescription for phenytoin (Dilantin) indicates that the patient understands their instructions?
(a) “I know that if I miss a routine dose I cannot easily make it up.”
(b) “I am glad to know that I won’t have to have routine lab tests.”
(c) “I am aware that if I stop taking this medication I am at risk for status epilepticus.”
(d) “It’s good that I don’t have to worry about a bunch of adverse effects from this drug.”
Answer:
(c) “I am aware that if I stop taking this medication I am at risk for status epilepticus.”
Rationale:
One of the most common causes of seizures in a patient taking phenytoin (Dilantin) is discontinuation of the medication. Because of the slow absorption of phenytoin from the GI tract, daily drug routines can be easily adjusted when a dose is missed. The patient also needs to be made aware of possible adverse effects of his medications. Phenytoin is metabolized in the liver, and both the inactive metabolites and unchanged drug are excreted in the urine. Because phenytoin has many hematopoietic adverse effects, blood work (including complete blood count, liver, and renal function studies) should be obtained on a regular basis. Serum levels should also be monitored because serum concentrations increase disproportionately to dosing regimens.
Question 47.
Which of the following would be the priority action if an ischemic stroke patient receiving tissue plasminogen activator (TPA) infusion begins to vomit bright red blood?
(a) Notify the physician.
(b) Place a nasogastric tube.
(c) Decrease the infusion.
(d) Stop the infusion.
Answer:
(d) Stop the infusion.
Rationale:
Tissue plasminogen activator (TPA) is a fibrinolytic medication that decreases the patient’s ability to clot. The infusion should be stopped immediately. While a patient is receiving TPA, all invasive procedures should be avoided because of the increased risk of bleeding; therefore, a nasogastric tube should not be placed. The physician should be notified, but'the priority is to stop the infusion.
When administering TPA, a bolus of 10% of the total dose is given IV push and then the infusion is provided over 1 hour.
Question 48.
Which of the following is NOT a clinical manifestation of Parkinson’s disease?
(a) Shuffling gait
(b) Bradykinesia
(c) Rigidity
(d) Alopecia
Answer:
(d) Alopecia
Rationale:
Alopecia (hair loss) is not a manifestation of Parkinson’s disease. The symptom that typically characterizes this disease is a faint tremor that slowly progresses in intensity. As the patient’s muscle tone becomes more rigid, the gait takes on a shuffling appearance. The patient’s face is masklike, and his/her speech is slow and monotone. Movements are slow (bradykinesia). It is common for the patient to develop dysphagia and drooling. The patient’s judgment becomes impaired even though actual intelligence remains unaffected.
Question 49.
Which of the following medications is commonly used to treat the symptoms of Parkinson’s disease?
(a) Pramipexole (Mirapex)
(b) Reserpine (Serpalan)
(c) Haloperidol (Haldol)
(d) Valproic acid (Depakote)
Answer:
(a) Pramipexole (Mirapex)
Rationale:
Pramipexole (Mirapex) is a dopamine agonist. It activates dopamine receptors, which mimic or copy the function of dopamine in the brain. Reserpine (Serpalan) is used for hypertension, some psychiatric disorders, and tardive dyskinesia. Haloperidol (Haldol) is used in the treatment of schizophrenia. Valproic acid (Depakote) is an antiseizure medication that can cause tremors.
The use of dopamine-blocking drugs has been linked to pharmacologically induced parkinsonism. Dopamine and acetylcholine are neurotransmitters that act on the input nuclei to the basal ganglia. When dopamine (an inhibitor) is reduced, acetylcholine (an excitatory neurotransmitter) becomes predominant and precipitates tremor.
Question 50.
The National Institutes for Health Stroke Scale (NIHSS) can be linked to outcomes. Which of the following indicates the meaning of the higher scoring?
(a) Better outcome
(b) Better orientation
(c) Increased risk factors
(d) Poorer outcome
Answer:
(d) Poorer outcome
Rationale:
The higher the score, the more deficits are present, which indicates a worse outcome for the patient. A score of 0 would indicate no deficits present for a patient with a normal examination. The NIHSS assesses the patient’s level of consciousness, orientation, response to commands, gaze, visual fields, facial movement, motor function, limb ataxia, sensation, language, articulation, and extinction.
Question 51.
A 28-year-old woman comes to the emergency department with blurred vision and drooping of the right eyelid. She also complains of intermittent episodes of muscle weakness and states that at times her neck does not feel strong enough to support her head. She tires when eating and takes frequent breaks during a meal. Several times, she has had to close her mouth using her hand because “the muscles in my face feel so weak. ” Which of the following is the probable diagnosis for this patient?
(a) Myasthenia gravis
(b) Bell’s palsy
(c) Trigeminal neuralgia
(d) Glioblastoma
Answer:
(a) Myasthenia gravis
Rationale:
The primary symptom of myasthenia gravis is weakness of voluntary muscles, especially those of the face. This weakness may temporarily improve with short periods of rest. Myasthenia gravis affects two to three times more women than men until age 40. This disease may result from a defect at the myoneural junction. Bell’s palsy is an inflammatory reaction involving the facial nerve presenting as ipsilateral facial paresis. This patient also has blurred vision and difficulty eating, which would not indicate Bell’s palsy. Trigeminal neuralgia is characterized by sudden episodes of ipsilateral facial pain. Glioblastomas are intracranial tumors that present with symptoms of increased intracranial pressure and focal deficits.
Question 52.
Which of the following tests is frequently used to diagnose myasthenia gravis?
(a) Lumbar puncture
(b) Tensilon test
(c) Allen’s test
(d) Magnetic resonance imaging (MRI)
Answer:
(b) Tensilon test
Rationale:
In the Tensilon test, edrophonium (Tensilon) is administered by intravenous infusion to a patient exhibiting signs of muscle weakness. Significant im-provement, lasting approximately 4 to 5 minutes, in the patient’s muscle tone indicates a positive diagnosis for myasthenia gravis. A lumbar puncture (LP) is frequently performed to assist in diagnosing meningitis. An Allen’s test is performed to evaluate the circulatory function of the ulnar artery before obtaining arterial blood gases (ABG) to verify collateral circulation before accessing the radial artery. An MRI is effective in detecting degenerative central nervous system diseases, malignant tumors, and oxygen-deprived tissue, but none of these findings are associated with myasthenia gravis.
Question 53.
Which of the following medications is NOT used to reduce the spasticity or pain associated with multiple sclerosis (MS)?
(a) Diazepam (Valium)
(b) Baclofen (Lioresal)
(c) Gabapentin (Neurontin)
(d) Cyclophosphamide (Cytoxan)
Answer:
(d) Cyclophosphamide (Cytoxan)
Rationale:
Cytoxan is a chemotherapeutic agent used to slow growth of cancer cells and interfere with their spread throughout the body. Diazepam, baclofen, and gabapentin are associated with the medical management of patients with multiple sclerosis (MS). Diazepam and baclofen are primarily effective in decreasing the spasms and stiffness associated with the disease, whereas gabapentin relieves pain as well as spasticity.
Question 54.
Alzheimer’s disease is characterized by profound impairment of cognitive functions. Which of the following is the cause of this disorder?
(a) Destruction of motor cells in the pyramidal tracts
(b) Metabolic disorder involving the adrenal glands
(c) Cerebral atrophy and cellular degeneration
(d) Degeneration of the basal ganglia
Answer:
(c) Cerebral atrophy and cellular degeneration
Rationale:
Alzheimer’s disease is a neurologic and degenerative disorder resulting from cerebral atrophy and cellular degeneration. Predominating symptoms are mental status changes, increased anxiety, forgetfulness, and eventually, the inability to recognize significant others and perform activities of daily living. Destruction of motor cells in the anterior gray horns and pyramidal tracts can result in the symptoms associated with amyotrophic lateral sclerosis. Metabolic disorders may cause altered cognitive function but can be reversed by correction of the underlying problem. Degeneration of the basal ganglia is usually associated with Parkinson’s disease.
Question 55.
An emergency nurse is caring for a patient who has suffered a closed head injury and has elevated intracranial pressure (ICP). Which of the following guidelines should the nurse follow when maintaining the patency of the endotracheal tube?
(a) Suction every 2 hours
(b) Instill normal saline before suctioning
(c) Lower the head of the bed before suctioning
(d) Suction only when necessary
Answer:
(d) Suction only when necessary
Rationale:
Suctioning should occur only when necessary and should be done quickly with less than 10 seconds at a time. Suctioning will cause coughing, which increases both intrathoracic and intracranial pressure. Suctioning should not occur every 2 hours but should be performed in case of elevated peak pressures or visible secretions accompanied by respiratory assessments that support the need. The instillation of normal saline before suctioning increases ventilator-associated pneumonia. Lowering the head of the bed will elevate the ICP. The head of the bed should be maintained at 30 degrees.
Question 56.
A patient with complaints of seeing “zigzagging lines” in her visual field after waking this morning presents to the emergency department. She now complains of a right temporal headache accompanied by nausea and photosensitivity. Based on these symptoms, the patient is evaluated for which of the following conditions?
(a) Sinusitis
(b) Meningitis
(c) Migraine headache
(d) Trigeminal neuralgia
Answer:
(c) Migraine headache
Rationale:
This patient is experiencing a migraine headache. Vision changes such as “zig-zag lines,” a unilateral headache, nausea, and photosensitivity are common manifestations of this type of headache. Sinusitis is described as pain or pressure over the maxillary or frontal sinus areas. The pain can be reproduced by palpation. Meningitis presents with symptoms of fever, headache, severe neck discomfort, and irritability. Typically, there’s an altered level of consciousness. Trigeminal neuralgia is characterized by ipsilateral facial pain from the side of the mouth to the ear, eye, or nostril on the same side.
Migraines are more prevalent in women than men, and there can be a familial tendency. Migraines are divided into three phases: aura (vision disturbances, confusion, paresthesia), which precedes the headache and lasts from 15 to 30 minutes; headache, characterized by a throbbing pain that usually begins as unilateral and can progress to bilateral accompanied by nausea or vomiting; and pos headache, noted by scalp tenderness and muscular aching of the neck.
Question 57.
Which of the following medications is utilized as preventative treatment for migraine headache?
(a) Propranolol (Inderal)
(b) Ondansetron (Zofran)
(c) Codeine
(d) Diphenhydramine (Benadryl)
Answer:
(a) Propranolol (Inderal)
Rationale:
Propranolol (Inderal), a beta-blocker, is one of the most commonly prescribed drugs for the prevention of migraines. Ondansetron (Zofran) is an antiemetic used to control the nausea and vomiting associated with a migraine headache. Codeine can be given for the pain of a full-blown migraine. Diphenhydramine (Benadryl) is useful in treating cluster headaches and can be used in the treatment of migraine headaches, but not the prevention.
Question 58.
A patient is prescribed ergotamine (Cafergot) for treatment of her headache. This medication has a cumulative effect that increases the risk of drug overdose. Clinical manifestations of ergotamine overdose (ergotism) include which of the following symptoms?
(a) Diplopia
(b) Hypotension
(c) Numbness
(d) Ataxic gait
Answer:
(c) Numbness
Rationale:
Symptoms of ergotamine overdose occur in response to intense vasoconstriction, which can produce signs and symptoms of peripheral vascular ischemia. In addition to numbness and tingling of fingers and toes, the patient may experience muscle pain and weakness, gangrene, and hypertension as well as dysrhythmias and myocardial infarction. Diplopia and ataxia are not associated with ergotamine tartrate overdose.
Question 59.
A patient arrives by ambulance for evaluation of seizure activity after falling on the ground while engaged in an argument with his employer. He is screaming and violently flinging his extremities. No evidence of incontinence or tongue biting is present. Prehospital providers state that this episode has lasted for 40 minutes. Based on this information, this patient is most likely to be diagnosed with which of the following conditions?
(a) Pseudoseizures
(b) Absence (petit mal) seizures
(c) Tonic-clonic (grand mal) seizures
(d) Focal seizures
Answer:
(a) Pseudoseizures
Rationale:
Emotional upset usually precedes a pseudoseizure, which generally lasts longer than a true seizure. In a true seizure, the patient may scream at the onset of the event but repetitive, consistent movement of the extremities is ongoing. Absence, or petit mal, seizures are manifested by an absence of consciousness for 5 to 10 seconds. Tonic- clonic (grand mal) seizures present with the following pattern: aura, cry, loss of consciousness, fall, tonic-clonic movement, and incontinence. Focal seizures involve one area of the body (which varies from patient to patient) and are not associated with an altered mental state.
Remember that patients do not have to have a loss of consciousness in order to manifest a seizure!
Question 60.
Temporary periods of cerebral ischemia may result in symptoms associated with which of the following conditions?
(a) Transient ischemic attacks (TIAs)
(b) Hypercapneic encephalopathy
(c) Disequilibrium1 syndrome
(d) Transtentorial herniation
Answer:
(a) Transient ischemic attacks (TIAs)
Rationale:
Transient ischemic attacks (TIAs) are temporary episodes of neurologic dysfunction in response to brief episodes of cerebral ischemia. Most commonly, a TIA presents as weakness of the lower face and upper and lower extremities (either right or left sided) as well as dysphagia, which may occur multiple times during the day. Between each attack, neurologic findings are normal. Hypercapneic encephalopathy is seen in patients with problems associated with chronic respiratory acidosis. Disequilibrium syndrome is an acute complication of peritoneal dialysis or hemodialysis. Transtentorial herniation occurs as a result of downward pressure from edema in the parietal or frontal lobes.
Question 61.
Which of the following medications is used to treat an acute cerebrovascular accident (stroke)?
(a) Tissue Plasminogen Activator (TPA)
(b) Tenecteplase (TNK)
(c) Reteplase (Retevase)
(d) Streptokinase (Streptase)
Answer:
(a) Tissue Plasminogen Activator (TPA)
Rationale:
Thrombolytics are part of a drug therapy that dissolves clots by fibrinolysis. Tissue plasminogen activator (Activase) is the only approved thrombolytic for use in acute ischemic stroke. Studies are in progress regarding the use of Tenecteplase (TNK) in acute stroke but are not approved at this time.
Thrombolytics are utilized within the 3-hour time period as recognized by the American Heart Association and for a select group of individuals within a 4.5-hour time period. Also remember that thrombolytic therapy should be started within 60 minutes of arrival to the ED (door to needle).
Question 62.
Which of the following responses from a new emergency nurse on an orientation test would indicate knowledge of the neurologic problem related to difficulty in transforming sound into patterns of understandable speech?
(a) Receptive aphasia
(b) Dysphagia
(c) Expressive aphasia
(d) Apraxia
Answer:
(c) Expressive aphasia
Rationale:
The new emergency nurse would provide the correct response if she/he stated that expressive aphasia is represented by the inability to speak words even though the patient is able to comprehend the spoken word. This is indicative of stroke syndromes on the left side of the brain (right-sided hemiplegia). Receptive aphasia is an impaired ability to understand spoken words. Dysphagia refers to difficulty in swallowing, which occurs when injury affects the vertebrobasilar region. Apraxia is the inability to perform a learned movement, such as using a comb, brushing one’s teeth, or waving goodbye.
Question 63.
The emergency nurse is discharging a patient with a probable diagnosis of Alzheimer’s versus dementia. Which of the following statements made by the family indicates an understanding of the explanations provided to them?
(a) “We understand that hallucinations and delusions are not as common as with other forms of dementia.”
(b) “We know that he is losing his mental abilities and this will interfere with his daily activities and social interactions.”
(c) “We are glad to know that there are medications out there that we will discuss with his doctor that will cure him.”
(d) “We understand that this disease called Alzheimer’s is not very common for dementia patients. ”
Answer:
(b) “We know that he is losing his mental abilities and this will interfere with his daily activities and social interactions.”
Rationale:
Alzheimer’s disease is a type of dementia. Generally, dementia is defined as a decline in thinking, reasoning, and/or remembering. People with Alzheimer’s disease have difficulty carrying out daily tasks they have performed routinely and independently throughout their lives and they can have difficulty with social interactions. Alzheimer’s disease accounts for 60% to 80% of all cases of dementia. This terminal, progressive brain disorder has no known cause or cure. Hallucinations and delusions can occur later in the disease process for these patients.
Question 64.
Which of the following is one of the most malignant and rapidly growing forms of brain tumor?
(a) Astrocytoma
(b) Meningioma
(c) Neuroma
(d) Glioblastoma
Answer:
(d) Glioblastoma
Rationale:
The glioblastoma and medulloblastoma are two of the most malignant and rapidly growing brain tumors. They are difficult to excise and can cause death within months. An astrocytoma is a slower-growing form of glioma. A meningioma is benign and frequently encapsulated. A neuroma is an extremely slow-growing tumor that arises from any of the cranial nerves.
Question 65.
Children below the age of 8 years are most likely to injure which portion of the vertebral column?
(a) Q to C7
(b) C1 to C3
(c) C5 to C6
(d) C7 exclusively
Answer:
(b) C1 to C3
Rationale:
When a young child is placed in a safety restraint seat facing the front of the car, the risk of cervical fracture at the to C3 level increases because of the fulcrum effect as the child’s head whips forward in an accident. For several reasons, a child’s cervical spine is more susceptible to injury than an adult. The other options are more common injuries in older children and adults.
Spinal Anatomical and Physiologic Changes in Children
- The vertebral bodies of children are wedged anteriorly and tend to slide forward with flexion.
- The neck ligaments of children are more lax.
- The neck muscles of children are weaker.
- The upper cervical spine facets of children are flatter.
SCIWORA stands for Spinal Cord Injury Without Radiographic Abnormality that is found in children only. This is under some regrouping at this time since with magnetic resonance imaging (MRI) we can actually determine some of these injuries. If you see it on the test, the answer is usually that an MRI is necessary to identify this disorder. The child may complain of neurologic deficits that were present but are now absent. The cfiild must be “packaged” and sent to a facility that dan provide MRI imaging. Do not discount children’s complaints of these deficits!
Question 66.
Which of the following is an important anatomical consideration for an infant regarding the potential of hypovolemia related to head and neck trauma?
(a) Open suture lines
(b) Lax neck muscles
(c) Large head
(d) Short trachea
Answer:
(a) Open suture lines
Rationale:
An infant’s open suture lines can allow for a greater amount of bleeding into the head and can actually bleed significantly enough to cause hypovolemia with hypotension and a shock state. The lax neck muscles, large head, and short trachea do not impact the potential for blood loss in an infant.
A child with a subdural hematoma exhibits bulging fontanels because the sutures separate as intracranial pressure (ICP) increases. Always check fontanels when assessing an infant.
Question 67.
Clinical symptoms of autonomic dysreflexia include headache, profuse sweating, piloerection (gooseflesh), hypertension, and bradycardia. This syndrome occurs in patients with injuries at or above which of the following levels?
(a) S5
(b) L1
(c) T6
(d) T12
Answer:
(c) T6
Rationale:
Autonomic dysreflexia is associated with spinal cord injuries at or above the T6 level. Autonomic dysreflexia occurs in the postacute phase when reflex activity has returned. A massive vasoconstriction creates a dangerous hypertensive situation.
Question 68.
A patient is being treated in the emergency department after a high-speed motor vehicle crash. He is complaining of pain to his lower thoracic spine area and is paralyzed from the waist down. He is noted to have hypotension. Computed tomography (CT) demonstrates a fracture at T9. Which of the following is the most probable reason for his hypotension?
(a) Neurogenic shock
(b) Hypovolemic shock
(c) Septic shock
(d) Spinal shock
Answer:
(b) Hypovolemic shock
Rationale:
Neurogenic shock occurs with fractures at T6 or above. This patient’s most likely cause of shock is hypovolemic, which must be discovered thorough examination and testing for etiologies within the chest and abdomen. Because of his paralysis from the T9 fracture, he will not be able to feel discomfort in either of these areas. It is therefore important to recognize these principles and not assume that the hypotension derives from the lower thoracic spinal area. Septic shock would not appear this early and is associated with infectious disease processes. Spinal shock revolves around a temporary cessation of feeling and motor power below the level of the lesion. This can happen immedi-ately after the event or may appear several days later. This also impacts bowel and bladder functions. Hypotension is not a part of spinal shock.
Remember that with neurogenic shock, hypotension will be present with bradycardia—not tachycardia!
Question 69.
Which of the following is the most common manifestation of central cord syndrome?
(a) Quadriplegia
(b) Priapism
(c) Upper extremity paralysis
(d) Poikilothermia
Answer:
(c) Upper extremity paralysis
Rationale:
Central cord syndrome, which usually occurs with a hyperextension injury or bleeding into the central canal, causes upper extremity loss of sensation and/or paralysis. The lower extremities are either not involved or are minimally involved. Priapism (sustained erection) and poikilothermia (inability to regulate temperature control) occur with complete spinal cord injuries, not an incomplete one such as central cord syndrome.
Brown-Sequard spinal cord injury is another incomplete spinal cord injury that involves hemisection of the cord in the anterior-posterior plane and occurs most often secondary to knife or gunshot wounds. This leaves the patient with paralysis on one side and paresthesia on the opposite side.
Question 70.
Which of the following types of medications would be prescribed for a patient diagnosed with temporal arteritis?
(a) Steroids
(b) Anticonvulsants
(c) Muscle relaxants
(d) Antihistamines
Answer:
(a) Steroids
Rationale:
Oral steroids are an effective treatment for temporal arteritis because it is a vasculitis. If any visual deficits are noted, steroids should be administered intravenously. Anticonvulsants, muscle relaxants, and antihistamines will not be effective or necessary.
Patients with temporal arteritis will have pain and tenderness to the temporal area. An erythrocyte sedimentation rate (ESR) may be done and would reveal an ESR value greater than 80. The definitive diagnosis is made by temporal artery biopsy.
Question 71.
Which of the following symptoms is associated with a cluster headache?
(a) Tearing
(b) Fever
(c) Aphasia
(d) Epistaxis
Answer:
(a) Tearing
Rationale:
A cluster headache is characterized by pain episodes that are grouped or clustered together for a few days or a few weeks with long periods of remission. The headache is described as causing unilateral pain behind the eyes or near the temples. Associated symptoms include tearing, rhinorrhea, nasal congestion, and Horner’s syndrome. Fever, aphasia, and epi- staxis are not associated with cluster headaches.
Homer’s syndrome is a rare process that includes a combination of miosis, ptosis, and anhidrosis (lack of sweating) to one side of the face involving one eye.
Question 72.
A patient presents to the triage desk and states, “This is the worst headache of my life.” The patient is well known by the staff with a past history of migraine headaches and hypertension. He is vomiting on arrival. He requests to have thej lights off in his room, and on assessment, the emergency nurse notes that his speech is abnormal. The patient is rubbing the back of his neck and he states that it “just hurts so much when I move my head down.” All of the following make this person high risk for a catastrophic event EXCEPT:
(a) intensity of the headache.
(b) pain to the posterior neck area.
(c) history of migraine headaches.
(d) speech abnormalities.
Answer:
(c) history of migraine headaches.
Rationale:
This patient is most likely experiencing a subarachnoid hemorrhage. The history of migraine headaches is not a risk factor for this catastrophic diagnosis. Patients with subarachnoid hemorrhage often state that the headache is the most severe they have ever had. This is also a process that is a sudden onset. Often patients with cerebral aneurysms are asymptomatic until the time of bleeding.
At the time of rupture, blood is forced into the subarachnoid space, causing symptoms of meningeal irritation, which would cause pain in the back of the neck when the head is moved in a forward (chin to chest) direction (nuchal rigidity). Other manifestations include nausea, vomiting, aphasia or other speech difficulties, photosensitivity, hypertension, and bradycardia. Other risk factors for this diagnosis are cocaine and amphetamine use and disease processes such as Marfan’s syndrome and sickle cell disease.
Remember that all patients, even those who frequent our doors, are at risk for devastating events. No matter how many times patients have been treated, each one deserves to be heard and should be assessed based on their present complaint! Also, patients with a pending subarachnoid hemorrhage may have atypical headaches for the 2 weeks before mpture. Often, the first symptom is syncope and coma!
Question 73.
When evaluating parameters, which of the following would have the most negative impact on a patient with a closed head injury?
(a) Blood pressure—90/42 mm Hg
(b) Cerebral perfusion pressure—85 mm Hg
(c) Urine output—48 mL in 1 hour
(d) Serum osmolality—280 mOsm
Answer:
(a) Blood pressure—90/42 mm Hg
Rationale:
One episode of hypotension, which drops the mean arterial pressure (MAP) below 70 mm Hg, can have devastating effects. The MAP should be maintained between 70 and 90 mm Hg. A blood pressure of 90/42 mm Hg creates an MAP of 58 mm Hg. In a head injured patient, the cerebral perfusion pressure (CPP) should remain above 70 mm Hg. This is the end result of the formula, CPP = MAP - ICP. The patient in this question is within normal limits for a patient with head injury. To obtain this number, an intracranial catheter must be in place. Maintaining the serum osmolality below 320 mOsm is recommended, which is noted in this question. Urine output of 48 mL/hour is adequate output.
Although it is accepted to allow “permissive hypo-tension” in patient’s suffering from hypovolemic shock, it is not permitted in the head injured patient. This will increase the patient’s mortality and morbidity significantly!
Question 74.
A patient with a ventriculostomy in place is noted to have an increasing intracranial pressure. Which of the following corrections would help remedy this situation?
(a) Turn the head to the right.
(b) Place the patient supine.
(c) Remove C-Collar on neck.
(d) Increase activity in the room.
Answer:
(c) Remove C-Collar on neck.
Rationale:
C-Collars can actually increase intracranial pressure (ICP). It is important to remove them as soon as possible once the C-spine has been appropriately cleared. This will help reduce the increasing intracranial pressure. Maintaining the head in midline position, elevating the head of the bed to 30 degrees, and keeping the room quiet and dark are all ways to help keep intracranial pressure down. Other interventions that can assist in reducing ICP are to provide pafn and sedating medications and administer osmotic diuretics. Hyperventilation should only be used as a short, temporary measure when the ICP is known to be elevated. Prophylactic hyperventilation is no longer performed.
Question 75.
Which of the following is the earliest indicator of change in a patient’s neurologic status?
(a) Pupillary reaction
(b) Motor response
(c) Capillary refill
(d) Level of consciousness (LOC)
Answer:
(d) Level of consciousness (LOC)
Rationale:
The earliest indicator of neurologic status is the level of consciousness (LOC). A patient who exhibits altered mental status or decreased consciousness should be reevaluated. Changes in the reaction and shape of pupils are late indicators of neurologic problems. Motor response appears as a delayed sign of neurologic status change. Capillary refill is an indicator of circulatory status.