Working through CEN Study Guide can boost confidence and reduce test anxiety by building familiarity and competence.
Gastrointestinal Emergencies CEN Study Guide
Acute Abdomen
Acute abdomen is sudden, severe abdominal pain. The physical examination of patients with acute abdomen should focus on pain location, history of GI symptoms, and palpation to assess for rigidity or guarding. Cardiovascular, genitourinary, and obstetrical conditions should also be considered when assessing acute abdomen.
TABLE 4.3 Causes of Acute Abdomen
|
Condition |
Pathophysiology |
Symptoms |
|
Abdominal aortic |
widening of |
sharp, severe pain in the chest, back, abdomen, or flank; rapid, weak, or |
|
Appendicitis |
inflammation of the appendix |
RLQ pain: rebound tenderness; |
|
Cholecystitis |
inflammation of the gallbladder |
colicky RUO pain, which can |
|
Kidney stones Discussed in detail |
blockage in the urethra leading to |
unilateral flank pain (can be |
|
Pancreatitis |
inflammation of the pancreas |
LUQ pain that may radiate to the back or shoulder; distension of abdomen |
|
Peptic ulcer |
erosion of the stomach by |
upper abdomen and back pain; heartburn |
|
Ruptured ectopic pregnancy Discussed in detail in Ch. 7 |
rupture of the fallopian tube due to ectopic |
vaginal bleeding, abdominal pain, cessation of pregnancy s/s |
|
Ruptured ovarian |
rupture of cyst in the ovary |
sudden, severe, unilateral pelvic pain |
Appendicitis
Pathophysiology
Appendicitis is inflammation of the appendix. Obstruction of the appendiceal lumen results in a decrease in blood supply which can lead to necrosis and perforation.
Risk Factors
- more common in males under 30
- inflammatory bowel disease (e.g., Crohn’s disease or ulcerative colitis)
Physical Examination
- abdominal pain
- dull, steady periumbilical pain
- RLQ pain that worsens with movement
- pain in RLQ at McBurney’s point
- positive Rovsing’s sign and Psoas sign
- fever
- anorexia
- nausea and vomiting
- rebound tenderness
- abdominal rigidity
Diagnostic Tests
- CT scan, the most precise exam to diagnosis appendicitis
- WBCs may be elevated
Management
- surgical intervention required: keep the patient NPO and prep for surgery
- analgesics and antiemetics as needed
- antibiotics
Peritonitis
Pathophysiology
Peritonitis is inflammation of the peritoneum (the lining of the abdominal cavity). There are several common causes of peritonitis.
- Perforation peritonitis occurs when the perforation of an organ allows the contents to spill into the peritoneal cavity, causing infection.
- Spontaneous bacterial peritonitis (SBP) is an infection of ascitic fluid in patients with cirrhosis. Mortality is high, and prompt intervention is required to prevent sepsis.
- Peritonitis is a common complication of peritoneal dialysis and is usually caused by contaminated equipment.
Physical Examination
- diffuse pain
- usually worsens with movement
- relieved by flexing the knees or bending right hip
- rigid abdomen
- guarding of the abdomen and rebound tenderness
- fever
- ileus
Diagnostic Tests
- CT scan or acute abdominal series
- positive Markle test
- CBC and liver function tests
- possible paracentesis for fluid analysis
Management
- antibiotics (IV or intraperitoneal)
- analgesics and antiemetics as needed
- monitor for sepsis and follow facility sepsis protocols
Bowel Obstruction and Perforation
Pathophysiology
A bowel obstruction occurs when normal flow through the bowel is disrupted. Mechanical obstructions are physical barriers in the bowel. The most common mechanical obstructions in the small bowel are adhesions, hernias, and volvulus (twisting of the bowels). The most common obstruction in the large bowel are tumors.
Paralytic ileus is the impairment of peristalsis in the absence of mechanical obstruction. It is most common in postoperative patients and can also be caused by endocrine disorders or medications (e.g., opioids).
Increased pressure proximal to the obstruction can lead to perforation of the bowel wall. Other common causes of bowel perforation include surgery, abdominal trauma, and neoplasm (in large bowel).
Physical Examination
- nausea and vomiting
- diarrhea
- distended and firm abdomen
- abdominal pain (cramping and colicky)
- unable to pass flatus
- high-pitched bowel sounds (early); absent bowel sounds (late)
- tympanic percussion
- pain, often sudden onset (perforation)
Diagnostic Tests
- increased WBCs
- elevated BUN and decreased electrolytes from dehydration/vomiting
- abdominal X-ray may show dilated bowel loops
- CT scan to diagnose
Management
- bowel rest (NPO) or nutritional support distal to obstruction
- fluid resuscitation
- bowel decompression via tube (NG or Miller-Abbott) with low, intermittent suction for patients with severe vomiting or abdominal distention
- antibiotics as needed
- surgical intervention for obstructions that do not resolve within 48 hours
- surgical closure of perforation
Cyclic Vomiting Syndrome
Pathophysiology
Cyclic vomiting syndrome (CVS) is characterized by a recurrent period of severe nausea and vomiting followed by periods of normal health. The etiology of CVS is unknown, but it has been linked to migraines, autonomic dysfunction, food sensitivities, and chronic cannabis use. It can occur in children and adults but is more common in children.
Physical Examination
- recurring vomiting that continues for hours or days (longer episodes more common in adults)
- episodes usually have patient-specific pattern (e.g., triggers, time of onset)
- prodrome: nausea, epigastric pain, headache
Management
- IV fluids
- antiemetic (usually IV ondansetron)
- sumatriptan or aprepitant may be given during prodrome or within first hour of symptom onset
Bleeding
UPPER Gl BLEEDING
Pathophysiology
An upper Gl bleed is bleeding that occurs between the esophagus and duodenum. Bleeding may be severe and require immediate hemodynamic management.
The etiology of upper Gl bleed varies.
- Peptic ulcers and esophagitis (secondary to GERD) are the most common causes of upper Gl bleeding.
- Esophageal varices occur when veins in the esophagus rupture because of portal hypertension (usually caused by hepatic cirrhosis). Bleeding may be severe and is likely to recur.
- Esophageal perforation or rupture may be iatrogenic, secondary to trauma, or caused by the severe effort of vomiting (Boerhaave syndrome).
- Mallory-Weiss tears occur at the gastroesophageal junction and result from forceful vomiting.
- NSAIDs and chronic gastritis can cause or worsen upper Gl bleeding.
Physical Examination
- hematemesis (may be in nasogastric aspirate) or coffee-ground emesis
- hematochezia (if hemorrhaging)
- upper abdominal pain
- melena
- signs and symptoms of hypovolemia (after significant blood loss)
Diagnostic Tests
- decreased HgB, Hct, and platelets
- longer PT and aPTT
- electrolyte imbalances (due to hypovolemia)
- elevated BUN and BUN-creatinine ratio
- positive hemoccult
- diagnosed via appropriate endoscopy or angiogram (EGD to locate source of bleeding)
Management
- O2 therapy
- manage hemodynamic status: IV fluids, blood products, and management of coagulopathies
- medications to constrict vasculature: vasopressin, octreotide, and beta blockers
- endoscopic or surgical repair if bleeding persists
- esophageal varices: endoscopic variceal band ligation (EVL) or esophageal balloon tamponade (e.g., Sengstaken-Blakemore tube)
- PPI to prevent post-procedure ulcers
LOWER Gl BLEEDING
Pathophysiology
A lower Gl bleed is any bleeding that occurs below the duodenum. Lower Gl bleeds occur less frequently than do upper Gl bleeds, are typically less emergent, and may stop on their own.
Risk Factors
- disease of the colon (e.g„ diverticulitis, IBD, colitis)
- colon polyps, cancer, or tumors
- abscess or inflammation of rectum
- hemorrhoids
- anal fissures
Physical Examination
- hematochezia
- melena
- bleeding from rectum
- abdominal or chest pain
- signs and symptoms of hypovolemia (after significant blood loss)
Diagnostic'Tests
- positive hemoccult
- decreased HgB and Hct
- PT and a PTT may be longer
- diagnosed via appropriate endoscopy, CT scan, or angiogram
Management
- manage hemodynamic status: IV fluids, blood products, and management of coagulopathies
- gastric lavage via NG tube
- endoscopic or surgical repair if bleeding persists
Cholecystitis
Pathophysiology
Cholecystitis, acute or chronic inflammation of the gallbladder, usually results from an impacted stone in the neck of the gallbladder or in the cystic duct. Cholelithiasis is the presence of gallstones in the gallbladder.
Risk Factors
- the 5 Fs for cholecystitis:
- fair (more prevalent in the Caucasian population)
- fat (BMI > 30)
- female (occurs more often in females than in males)
- fertile (one or more children) or pregnant
- forty (age over 40)
Physical Examination
- RUQpain, which can radiate to back or right shoulder; common after eating a high-fat meal
- colicky pain?
- positive Murphys sign
- nausea and vomiting
- flatulence
- jaundice if obstruction is significant
- atypical symptoms in older patients and patients with type 2 diabetes: confusion, lack of pain
Diagnostic Tests
ultrasound or CT scan
Management
- IV crystalloid
- antiemetic and analgesics as needed
- definitive treatment is cholecystectomy
Cirrhosis
Hepatic (liver) failure can be acute (onset <26 weeks) or chronic. Common causes of acute liver failure (also called fulminate hepatitis) include acetaminophen overdose and viral hepatitis; the most common cause of chronic liver failure is alcohol abuse.
Liver failure leads to dysfunction in multiple organ systems.
- Hepatic encephalopathy is impaired cognitive function caused by increased serum ammonia (NH3) levels. Increased NH3 levels may also cause neuromuscular symptoms, including asterixis and bradykinesia.
- Coagulopathies are caused by impaired synthesis of clotting factors in liver tissue.
- Jaundice is caused by hyperbilirubinemia.
- Acute kidney injury occurs in approximately 50% of patients with liver failure. (The mechanism is unknown.)
- Infections and sepsis develop secondary to decreased and defective WBCs.
- Metabolic imbalances may include hypokalemia, hyponatremia, and hypoglycemia.
- Lowered peripheral vascular resistance decreases BP and increases HR.
Chronic liver failure leads to cirrhosis the development of fibrotic tissue in the liver. Cirrhosis in the liver increases resistance in the portal vein, causing portal hypertension. Common conditions that occur secondary to portal hypertension include esophageal varices, ascites, and splenomegaly.
Physical Examination
- cognitive changes or motor dysfunction
- jaundice
- petechiae or purpura
- spider angiomas
- ascites
- RUQpain
- palmar erythema
- nausea and vomiting
Diagnostic Tests
- elevated AST, ALT, and/or bilirubin
- elevated NH3 levels
- decreased protein, albumin, and fibrinogen
- decreased WBCs, HgB, Hct, and platelets
- longer PT and PTT, and increased INR
- CT scan or MRI may show fibrosis of liver
Management
- IV fluid resuscitation
- lactulose and neomycin to reduce ammonia levels
- diuretics for ascites
- prophylactic treatment for stress ulcers
- monitor ICP
- tight glucose control for nonalcoholic fatty liver disease
- shunt to reduce portal hypertension
Diverticulitis
Pathophysiology
Diverticulitis is inflammation of the diverticula (small outpouchings in the GI tract, usually in the sigmoid colon). The inflammation is usually caused by obstruction of diverticula by fecal material or undigested food. It may lead to infection, necrosis, or perforation.
Risk Factors
age (more common in elderly patients)
Physical Examination
- LLQabdominal pain
- rebound tenderness
- abdominal distention
- anorexia
- nausea and vomiting
- fever
- change in bowel habits (diarrhea or constipation)
- hematochezia
Diagnostic Tests
- CBC may show increased WBCs
- CT scan of abdomen to diagnose or rule out perforation
- Electrolyte monitoring for imbalances
Management
- IV fluids
- keep patient NPO
- anticholinergics (to reduce spasms in colon)
- analgesics as needed
- patient education
- stool softeners
- a liquid diet followed by a low-fiber diet until the inflammation is reduced, then a high-fiber diet to prevent straining
Esophageal varices
- Causes- Decompensated liver failure can cause portal hypertension. Portal pressure surpasses that of the inferior vena cava, and blood is directed through venous collaterals in the esophagus, stomach fundus and rectum. These varices can rupture and cause severe upper GI bleeding.
- Clinical features- Indicators of upper GI bleeding include sudden and intense episodes of painless vomiting of blood (hematemesis). The complications include hypovolemic shock and hepatic encephalopathy.
- Treatment.
- Immediate resuscitation involves airway management, IV fluids, blood products and vasopressors as needed.
- Endoscopic banding.
- Sclerotherapy.
- IV octreotide administration.
- Sengstpken-Blakemore tube for mechanical compression.
- Transjugular intrahepatic portosystemic shunts for persistent bleeding.
Foreign Bodies in the Gl System
Pathophysiology
A foreign body is any object that enters the GI system either intentionally or accidently. Foreign bodies within the GI system typically present as partial or full obstructions of the esophagus, although objects may also pass to other GI organs. These objects can cause damage, including tears, infection, and obstruction, to the GI system.
Physical Examination
- drooling or difficulty swallowing
- feeling of something “stuck” in throat
- subcutaneous emphysema present if esophageal perforation
Diagnostic Tests
chest or neck X-rays to diagnose
Management
- maintain airway
- glucagon to promote smooth muscle relaxation
- endoscopy or surgery to remove objects that don’t pass on their
- emergent removal required
- magnets anywhere in the GI tract
- sharp objects or batteries in the esophagus
Hepatitis
Pathophysiology
Hepatitis is inflammation of the liver. It can be caused by a systemic viral infection, autoimmune conditions, or by certain medications.
Physical Examination
- clay-colored stools
- dark urine (foamy)
- jaundice
- steatorrhea (excess fat in stool)
- flulike symptoms
- abdominal pain
Diagnostic Tests
- elevated liver enzymes (AST and ALT)
- elevated alkaline phosphatase
- elevated ammonia
- low albumin
Management
- manage symptoms of liver failure (detailed in the section Cirrhosis)
- treatment of underlying cause (e.g., antivirals, glucocorticoids)
TABLE 4.4. Types of Viral Hepatitis
|
Type |
Route of Transmission |
Prevention and Treatment |
|
A |
Fecal/oral |
Vaccine available |
|
B |
Blood/body fluids |
Generally mild and requires only supportive |
|
C |
Blood/body fluids |
Chronic infection may lead to liver failure |
|
D |
Blood/body fluids |
Occurs simultaneously with hepatitis B |
|
E |
Fecal/oral |
No vaccine available |
Intussusception
Pathophysiology
Intussusception is a mechanical bowel obstruction caused when a loop of the large intestine telescopes within itself. This condition can cut off the blood supply, causing perforation, infection, and bowel ischemia. It usually occurs within the first 3 years of life and is more prevalent in males.
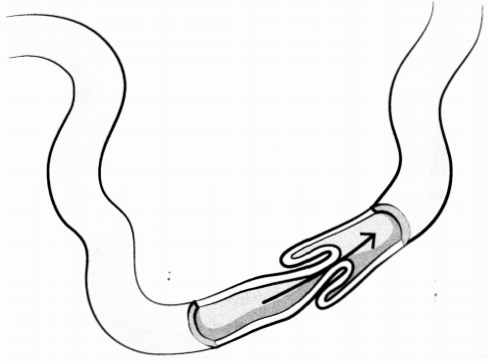
Figure 4.2. Intussusception
Physical Examination
- red currant-jelly-like stool
- sausage-shaped abdominal mass
- colicky pain
- inconsolable crying
- absence of stools
Diagnostic Tests
abdominal X-rays to confirm diagnosis
Management
- keep patient NPO
- a stable patient: hydrostatic or pneumatic enema
- unstable patients: surgery
Obstructions
1. Causes- The common culprits are hernias, tumors and adhesions. Other triggers include foreign body impaction, volvulus, fecal impaction and intussusception.
2. Clinical features- Clinically, these obstructions manifest as abdominal cramps and vomiting. Ifthere’s a complete obstruction, it can cause severe constipation that is known as obstipation. On the other hand, a partial obstruction can cause diarrhea. Usually, hyperactive bowel sounds are observed, but if these sounds are absent, it might indicate peritonitis. In more severe cases, the patient might go into shock. Obstructions in the large intestine generally present milder symptoms, which can include constipation, vomiting, abdominal cramps, and in some cases, palpable masses.
3. Treatment.
This is a surgical emergency that necessitates:
A. NPO (Nothing by Mouth) status.
B. Nasogastric suction.
C. IV fluid and electrolyte replacement.
D. Fluid input-output measurement.
E. The use of IV antibiotics.
F. The definitive treatment involves surgical exploration, resection and anastomosis as necessary.
Pancreatitis
Pathophysiology
Pancreatitis is caused by the release of digestive enzymes into the tissues of the pancreas. The condition causes autodigestion, inflammation, tissue destruction, and injuny to adjacent structures and organs. Pancreatitis can be acute or chronic, butt its onset is usually sudden.
The tissue damage caused by pancreatitis increases capillary permeability, resulting in fluid shifts into interstitial spaces that cause edema and systemic inflammatory responses (e.g., ARDS); Inflammation may also limit diaphragm movement and cause atelectasis. Severe damage to the pancreas may cause retroperitoneal bleeding.
Risk Factors
BAD HITS
- ciliary (e.g., gallstones blocking pancreatic duct)
- alcohol
- lirugs (thiazide diuretics, sulfa drugs, pentamidine, antiretrovirals)
- hypertriglyceridemia/hypercalcemia
- idiopathic causes
- trauma
- scorpion sting or surgery (recent ERCP or abdominal surgery)
Physical Examination
- steady, severe pain abdominal pain; usually in the LUQ and may radiate to the back or shoulder
- guarding
- nausea and vomiting
- decreased bowel sounds
- steatorrhea
- fever
- tachycardia and hypotension
- dyspnea
- Cullen sign
- Grey Turner sign
Diagnostic Tests
- elevated amylase and lipase
- hypocalcemia
- decreased total protein
- hypoglycemia
- elevated Hct, BUN, and CRP
- increased WBCs
- imaging (MRI or CT scan with contrast) to diagnose
Management
fluid resuscitation, including electrolyte replacement.
pain management (usually opioids) and antiemetics.
endoscopic retrograde cholangiopancreatography (ERCP) for gallstones and bile duct inflammation.
monitor for respiratory complications, including ARDS and atelectasis.
Gastrointestinal Trauma
Pathophysiology
Gl trauma can be caused by a penetrating injury such as a gunshot or knife wound or can be caused by blunt trauma from a motor vehicle injury or a fall.
TABLE 4.5. Diagnosis of Gl Trauma
|
Organ |
Physical |
Diagnostic Tests and Findings |
|
Spleen |
LUQ pain (referred to |
CT scan or FAST exam |
|
Liver |
RUQ pain (referred to |
CT scan may show |
|
Pancreas |
Epigastric pain |
CT for diagnosis |
|
Stomach |
Hematemesis |
Free air on chest X-ray |
Management
- manage hypovolemia and monitor for hypovolemic shock
- surgery required for penetration injuries and unstable patients
Read More