The ultimate goal of engaging with CEN Study Guide is to solidify nursing competence, pass the licensure exam, and embark on a successful nursing career.
Environmental Emergencies CEN Study Guide
Burns
Pathophysiology
Burns are trauma to the skin or underlying tissue caused by heat, radiation, electricity, or chemical exposure. The heat causes protein denaturation of the cells that leads to coagulative necrosis, platelet aggregation, and vessel constriction. The inflammatory response to the injury creates a fluid shift that can result in hypovolemia and reduced cardiac output (“burn shock”). Damage to large areas of skin also puts patients at risk of hypothermia.
Burns are classified by depth as first-degree, second-degree, and third-degree.
- Superficial (first degree): Damage is limited to the epidermis and does not result in blisters (e.g., sunburn).
- Partial-Thickness (second degree): Damage includes the dermis and epidermis accompanied by severe pain.
- Full-Thickness (third degree): All layers of the skin are damaged and there is likely underlying tissue damage. The patient may not feel pain in areas of significant nerve damage.
Burns are described by the total body surface area (TBSA) involved. TBSA is calculated by assigning a numerical value to the areas that are burned; the rule of 9s is the most commonly used method.
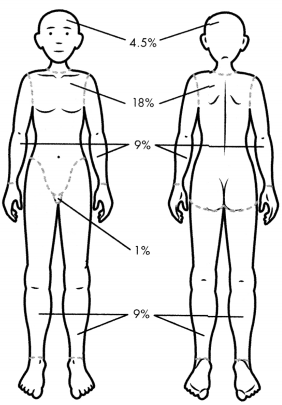
Fig: Rule of 9s for Calculating Total Body Surface Area (TBSA) of Bums
Physical Examination
- Superficial (first degree): Damage is limited to the epidermis and does not result in blisters (e.g., sunburn).
- Partial-Thickness (second degree): Damage includes the dermis and epidermis accompanied by severe pain.
- Full-Thickness (third degree): All layers of the skin are damaged and there is likely underlying tissue damage. The patient may not feel pain in areas of significant nerve damage.
Diagnostic Tests
- Labs to monitor for hypovolemia, electrolyte imbalances, metabolic acidosis, and renal dysfunction.
- ABGs and carboxyhemoglobin to monitor pulmonary function.
Management
Priority: ABCs and IV access for fluids
- Look for signs of airway compromise (e.g., burns to the face, soot in the nose or mouth, singed nasal hair, or coughing due to smoke inhalation).
- Edema may develop quickly and obstruct the airway.
- Remove hot jewelry and clothing.
- Cool burns with cool water or saline-soaked gauze.
- Calculate TBSA (used to correct hypovolemia).
IV lactatecj Rimer’s per Parkland formula:
- 4 ml x TBSA (%) x body weight (kg).
- Give 50% in first 8 hours; then 50% in next 16 hours.
- Formula time starts at the time the burn happens.
- Expected urine output is 0.5 - 1.0 ml/kg/hr in adults and 1.0 - 1.5 ml/kg/hr in children < 30 kg.
- Analgesics
- Clean wounds and apply sterile dressing.
- Topical antibiotic (e.g., silver sulfadiazine).
- Escharotomy to remove constricting areas of eschar as needed.
- Full-thickness burns require hospitalization for excision and grafting.
Chemical Exposure
Pathophysiology
Chemical burns result from contact with acids (e.g., hydrofluoric acid), alkalis (e.g., ammonia, cement), or organic compounds (e.g., phenol, gasoline). The injury will depend on the how the patient was exposed, what chemical they were exposed to, and the length of time of the exposure. Chemicals will continue to cause tissue damage as long as they have been removed, so early decontamination is critical.
Chemical burns may take several days for to slough, making them difficult to assess their severity. They should be assumed to be partial- or full-thickness during acute care.
The safety data sheets (SDS) (formally known as material safety data sheets [MSDS]) for a chemical agent will include information on toxicology, first aid, and exposure control.
Management
Consult poison control and/or SDS.
Decontaminate the affected areas
- Remove patient's clothing.
- Brush off dry chemicals.
Irrigate burn with water.
Fluid resuscitation and wound care (as described in "Burns” above)
Hydrofluoric acid
- Administration of calcium gluconate (topically, subcutaneously, or intravenously).
- Monitor for dysrhythmias and electrolyte imbalances.
Phenol: swab affected area with polyethylene glycol (PEG) and irrigate with water.
Electrical Injuries
Pathophysiology
Generated electrical energy causes external and internal injury from the electrical current running through the body. Injuries will vary depending on the intensity of the current, voltage, resistance, the length of time exposed, entry and exit locations, and the tissue and organs affected by the electrical current. Generated electrical injury can result in skin burns, damage to internal organs or tissue, respiratory arrest, or cardiac arrhythmias/arrest.
Physical Examination
- Burns at the entry and exit points with a clean line of demarcation.
- Involuntary muscular contractions
- Dyspnea
- Seizures, confusion, or loss of consciousness
- Paralysis
- Dysrhythmias
- Signs and symptoms of rhabdomyolysis or compartment syndrome in severe cases.
Management
- Priority: ABCs
- Follows ALS protocols for respiratory/cardiac arrest.
IV fluids
- Standard burn fluid-resuscitation protocols are not used as there is usually more damage than is seen on surface burns.
- IV fluid treatment goal is to maintain urine output of 75 - 100 ml/hr.
- Analgesics
- Monitor cardiac and kidney function.
- Head-to-toe assessment for injuries secondary to falls.
Envenomation Emergencies
Pathophysiology
Most animal bites or stings do not require emergency care and can be managed with OTC analgesics. However, emergent care may be required for exposure to lethal venom or for anaphylaxis.
Table: Diagnosis and Management of Envenomation Emergencies
|
Animal |
Physical Examination |
Treatment and Management |
|
Snake |
varies depending on snake species general s/s: nausea and vomiting, tachycardia, diaphoresis coagulation abnormalities weakness and lethargy confusion |
ABCs |
|
Spider |
brown spider bites: delayed pain; ecchymosis and erythema; central blood-filled lesion that ruptures, leaving an ulcer widow spider bites: immediate pain; muscle cramping and weakness; diaphoresis; hypertension; tachycardia |
wound care analgesics excision of brown spider bite opioids and benzodiazepines for symptomatic widow bites antivenom for widow bites only in patients at high risk for severe systemic response |
|
Scorpion |
immediate pain |
supportive treatment for s/s antivenom only for patients with severe symptoms |
|
Bee, Wasp, Hornet, or Fire Ant |
immediate pain, burning, and itching |
remove stinger if still in place ice, antihistamines, or NSAIDs for pain |
Submersion Injury
Pathophysiology
A submersion injury is a respiratory injury or impairment that occurs as a result of being submerged in a substance (usually water, but it can be other liquids or solids like grain). The respiratory impairment resulting from submersion leads to hypoxemia, which in turn can lead to organ failure. Common complications include dysrhythmias, ARDS, and cerebral edema.
Physical Examination
- Change in LOC
- Cool, clammy, pale skin
- Wheezing or crackles
- Signs and symptoms of respiratory failure
Diagnostic Tests
ABG shows metabolic acidosis
Management
- Follow ALS protocols for respiratory/cardiac arrest.
- Priority: treatment of hypoxemia.
- Start patient on 100% oxygen; titrate down based on serial ABG results.
- Intubation and mechanical ventilation may be needed.
- Nebulized bronchodilators to relieve bronchospasms or wheezing.
- Manage hypothermia (See “Temperature-Related Emergencies” next).
Temperature-Related Emergencies
HYPOTHERMIA
Pathophysiology
Hypothermia occurs when core body temperature drops below 35°C (95°F), causing a reduction in metabolic rate and in respiratory, cardiac, and neurological functions. When body temperature drops below 30°C (86°F), thermoregulation ceases.
During hypothermia, diuresis and systemic fluid leakage into the interstitial space can lead to hypovolemia. Vasoconstriction due to the cold can mask this hypovolemia. When the patient is rewarmed and the vessels dilate, the patient will go into shock or cardiac arrest if the fluid volume is not replaced.
Physical Examination
- Mild hypothermia: 32 - 35°C (90 - 95°F)
- Moderate hypothermia: 28 - 32°C (82 - 90°F)
- Severe hypothermia: < 28°C (82°F)
- Intense shivering that lasts until core body temperature drops below 31°C (87.8°F)
- Lethargy, clumsiness, confusion, agitation, or hallucinations
- Hypotension
Diagnostic Tests
- Decreased cardiac function.
- Initial bradycardia and slow A-fib, then V-fib or asystole.
- ECG: will read as injury due to myocardial infarction, but will show a J wave or Osborn wave.
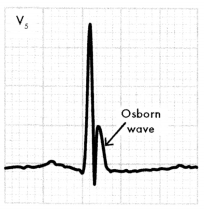
Fig: Osborn or J Wave
Management
- First line: prevent further heat loss by removing wet/cold clothing and insulating patient.
- Mild hypothermia: passively rewarm patients at a rate of 1°C per hour with an insulated blanket and warmed fluids.
- Severe hypothermia: active core warming.
- Inhalation: oxygen at 40°C - 45°C (104°F - 113°F) delivered via oxygen mask or ET tube.
- Infusion: IV fluids or blood products at 40°C - 42°C (104°F - 107.6°F).
- Lavage: closed thoracic lavage through 2 thoracic tubes at 40°C - 45°C (104°F - 113°F).
- Extracorporeal core rewarming (ECR): not often performed as it requires a specialist and prearranged protocol.
- Fluid resuscitation: 1 - 2 L (for adults) or 20 ml/kg (for pediatrics) of 0.9% saline solution heated to 40°C - 42°C (104°F - 107.6°F) via IV.
- CPR for V-fib or asystole: defibrillation once body temperature > 30°C (86°F).
Local Cold-Related Emergencies
Frostbite is injury to the dermis and underlying tissue due to cold. The exposure to cold leads to cellular damage, impairment of the vascular system, and an inflammatory response.
- Symptoms (early stage): cold and white skin; numbness, tingling, or throbbing in affected area.
- Symptoms (mild stage): skin hard or frozen to the touch; skin red and blistered when warmed and thawed.
- Symptoms (severe stage): blue, blotchy, or white skin; black necrotic areas; blood-filled blisters as skin warms; damage to underlying tissue.
Immersion foot is an injury that results from prolonged exposure to a cold and wet environment of a limb that had little or no mobility. The limb will be numb, cold, pale, clammy, and swollen. Severe cases may present with ulcers, eschar, or muscle atrophy.
Management of frostbite and immersion foot
- Rewarm Affected Area Until It Is Red In Color: Warm Water, Heated To 104°F - 108°F (40°C - 42°C), In A Basin Or Bath.
- Analgesics (Pain During Rewarming May Be Severe).
- Wound Care As Necessary, Including Debridement.
Chilblains are an Inflammatory Response That Occurs In The Skin And Small Blood Vessels After Repeated Exposure To Cold But Not Freezing Temperatures. It Is Most Common In Women, Underweight Patients, And Patients With Raynaud's Disease.
- Symptoms: Red Or Purple Bumps On The Skin That Can Be Painful Or Swollen; Complaints Of Itchy Feeling; Blistering Or Ulceration (Severe Case).
- Management: passive rewarming of affected area; topical corticosteroids; daily nifedipine for recurrent chilblains.
Heat-Related Injuries
Heat cramps (exercise-associated muscle cramps) occur when exercise or physical exertion leads to a profuse loss of fluids and sodium through sweating. The resulting hyponatremia causes muscle cramps.
- Diagnosis: sudden onset of severe spasmodic muscle cramps in extremities; may progress to carpopedal spasms, which can incapacitate the hands or the feet.
- Management: keep patient cool; oral fluids (solution of 1 L of water with 10 g of sodium or commercial sports drinks); IV fluids if patient cannot tolerate fluids by mouth (1 - 2 L of 0.9% saline solution); stretch the affected muscle (firm, passive stretching).
Heat exhaustion occurs when the body is exposed to high temperatures, leading to dehydration. It is not a result of deficits in thermoregulation or the central nervous system.
- Diagnosis: temperature elevated but < 104°F (40°C); diaphoresis; dizziness and weakness; tachycardia; hypertension; headache; nausea and vomiting; syncope.
- Management: cool with ice packs; oral fluids (solution of 1 L of water with 10 g of sodium or commercial sports drinks); IV fluids if patient cannot tolerate fluids by mouth (1 - 2 L of 0.9% saline solution).
Heat stroke (classic or exertional) results when the compensatory measures for ridding the body of excess heat fail, leading to an increased core temperature. Complications can include rhabdomyolysis, DIC, and acute kidney injury.
- Diagnosis: temperature > 104°F (40°C); tachycardia and tachypnea; confusion or delirium; seizures; labs show organ dysfunction.
- Management: cool rapidly with ice bath or ice yacks to 102°F (38.9°C); aggressive fluid resuscitation; electrolytes as needed; management of complications (e.g., platelets, benzodiazepines).
Animal Bites
- The most common cause of animal bites are domesticated dogs and cats, but bites may also come from wild animals such as bats, raccoons, and skunks.
- Animal bites can cause punctures, lacerations, fractures, and crush injuries.
- Wounds caused by animal bites are also at high risk for infection.
- Management: wound care, antibiotics for high-risk bite wounds, immunizations as indicated.
- High-risk bite wounds include: cat and human bites, bites to the hand or foot, puncture wounds, damage to deep structures, and wounds to immunocompromised patients.
Rabies is a virus that causes encephalitis. It is carried in the saliva of infected animals and is transmitted during animal bites.
- Management of animal bite: clean wound with soap and water or BZK wipes; rabies vaccine and rabies immune globulin (RIG); once rabies has advanced, there is no curative treatment.
- Diagnosis of rabies: fatigue; fever; headache; confusion; agitation; hallucinations; insomnia; excessive salivation; hydrophobia; ascending paralysis; positive fluorescence antibody test from biopsy of skin near the nape of neck.
Related Posts: