CEN Study Guide covers a wide range of nursing specialties, including obstetrics, geriatrics, community health, and psychiatric nursing.
Communicable Diseases CEN Study Guide
Clostridium difficile (C. Difficile)
Pathophysiology
Clostridium difficile (commonly called C. diff) is an acute bacterial infection in the intestine most commonly seen after antibiotic use. The antibiotics disrupt the normal intestinal flora, allowing; the antibiotic-resistant C. diff spores to proliferate in the intestines. The bacterium releases a toxin that causes the intestine to produce yellow-white plaques on the intestinal lining. The C. diff infection can produce inflammation in the intestines, resulting in toxic colitis (toxic megacolon) or pseudomembranous colitis, and may also lead to perforation and sepsis.
Transmission and Precautions
- Fecal to oral transmission
- Use contact precautions
- Do not use foams and gels (they will not kill the spores)
- Environmental cleanse of a 1:10 bleach-to-water solution
Physical Examination
- Foul-smelling diarrhea 5-10 days after start of antibiotic.
- Signs and symptoms of toxic colitis: tenesmus, rectal bleeding, abdominal distension and tenderness.
Diagnostic Tests
- Enzyme immunoassay (EIA): most commonly run diagnostic test
- PCR test on the stool specimen: most sensitive and specific diagnostic test
Management
Antibiotic-induced C. diff: stop current use of antibiotics if possible
Oral antibiotics; IV if oral antibiotics cannot be tolerated
- Vancomycin (Vancocin)
- Fidaxomicin (Dificid)
- Metronidazole (Flagyl)
Vaccine-Preventable Diseases
CHICKENPOX
Pathophysiology
Chicken pox (varicella-zoster virus) is a viral infection that infects the conjunctiva or the mucous membranes of the upper respiratory tract. The infection then spreads, causing the hallmark rash of small, itchy, fluid-filled blisters all over the body.
Transmissions and Precautions
- Person to person through direct contact or airborne droplets
- Airborne, droplet, and contact precautions
Physical Examination
- Itchy rash that forms small fluid-filled blisters that eventually scab
- Mild headache
- Moderate fever
- Fatigue
Diagnostic Tests
- Varicella titer test on a blood sample
- Tzanck test performed on a swab sample of the lesion area
Management
- Supportive care for symptoms (systemic antihistamines, colloidal oatmeal baths)
- Antivirals in severe cases
DIPHTHERIA
Pathophysiology
Diphtheria is an infection caused by the bacterium Corynebacterium diphtheriae. The bacterium enters through the pharynx or the skin and releases a toxin that causes inflammation and necrosis.
Transmissions and Precautions
- Person to person through respiratory droplets (pharyngeal infection)
- Person to person skin contact (skin infection)
- Droplet, contact precautions
Physical Examination
- White or gray glossy exudate in the back of the throat
- Mild sore throat and hoarseness
- Serosanguinous or purulent discharge
- Difficulty swallowing or getting food stuck in throat
- Visibly swollen neck (bull neck)
- Stridor
- Low-grade fever
- Skin infection: non-specific symptoms
Diagnostic Tests
positive culture from swab
Management
- Diphtheria antitoxin (IM or IV)
- Antibiotics (penicillin, erythromycin)
- Clean skin infection with soap and water
- Diphtheria vaccination after recovery
MEASLES
Pathophysiology
Measles is an acute, highly contagious infection caused by a paramyxovirus. The virus enters through the upper respiratory tract or conjunctiva and spreads systemically through the lymph nodes, triggering a systemic inflammatory response. Infants, elderly patients, and immunocompromised patients are more likely to experience serious complications such as pneumonia and encephalitis.
Transmissions and Precautions
- Person to person through respiratory droplets that can live in the air or on hard surfaces for up to 2 hours
- Airborne, droplet, and contact precautions
Physical Examination
- Fever
- Cough
- Runny nose and conjunctivitis
- Sore throat
- Koplik spots
- Red, blotchy rash (usually starts on the face and spreads cephatocaudally)
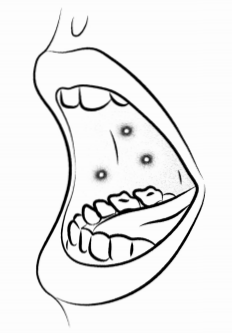
Figure: Koplik spots
Diagnostic Tests
Positive PCR or serum measles IgM antibody
Management
- Vitamin A
- Antivirals (ribavirin) for high-risk patients
- Supportive care for symptoms
- Prophylaxis for high-risk contacts (MMR vaccine or immune globulin)
MUMPS
Pathophysiology
Mumps is an acute infection caused by a paramyxovirus. The virus causes an inflammatory response that results in swelling of the salivary glands (usually the parotid glands). Possible complications include epididymo-orchitis, meningitis, encephalitis, and hearing loss.
Transmissions and Precautions
- Person to person through respiratory droplets in close proximity
- Droplet precautions
Physical Examination
- Fever
- Salivary gland edema
- Parotitis
- Pain when chewing or swallowing
- Swelling in submandibular glands or tongue
Diagnostic Tests
Positive serum IgM or PCR
Management
Supportive care for symptoms (acetaminophen, warm/cold packs for swelling)
PERTUSSIS
Pathophysiology
Pertussis (whooping cough) is an infection caused by the bacterium Bordetella pertussis that causes a mucopurulent sanguineous exudate that can compromise the respiratory tract.
Transmissions and Precautions
- Person to person through respiratory droplets in close proximity
- Droplet precautions
Physical Examination
Paroxysmal or spasmodic cough (“whoop”) that ends in a prolonged, high-pitched inspiration
Diagnostic Tests
PCR on nasal or throat swab
Management
- Antibiotics (erythromycin, azithromycin)
- Supportive, care for symptoms, including suctioning
Influenza
Pathophysiology
Influenza (flu) is a group of contagious viruses that cause respiratory symptoms and fever. Four types of human influenza viruses have been identified (A, B, C, and D); only types A and B cause severe illness in people. Flu is a common seasonal illness that tends to be more widespread during the fall and winter. However, infection may occur at any time of the year.
Symptoms of flu typically appear suddenly and can range from mild to life-threatening. For most people, flu is a self-limiting infection that does not require emergent care. High-risk patients may develop severe complications, including pneumonia, sepsis, myositis, seizure, and encephalopathy.
Risk factors for severe flu complications include:
- Age of < 2 years or > 65 years
- Being immunocompromised
- Pregnancy
- Asthma or chronic lung disease
- Diabetes
- Obesity
- Heart, liver, kidney, or metabolic disorders
Transmissions and Precautions
- Transmission through mucous membrane contact and respiratory droplets
- Contact and droplet precautions
Physical Examination
- Fever
- Headache
- Myalgia
- Nonproductive cough
- Sore throat
- Nausea and vomiting
Diagnostic Tests
Rapid influenza diagnostic test or molecular assay (more reliable)
Management
Pharmacological management of symptoms
- Antipyretics
- Cough suppressant
- Antiemetics
- Antiviral drugs administered to high-risk patients and patients with symptom onset of < 48 hours previous
- Monitor for and manage complications
- Isolate until symptoms resolve or at least 24 hours after fever has gone
|
Drug |
Notes |
|
Oseltamivir |
recommended for ages 2 years and older may cause nausea and vomiting |
|
Zanamivir |
for ages 7 and older risk of bronchospasm |
|
Peramivir |
approved for ages 2 and older may cause diarrhea |
|
Baloxavir |
for ages 12 and older |
Multi-Drug Resistant Organisms
Methicillin-resistant Staphylococcus aureus (MRSA) is a bacterial infection caused by a strain of Staphylococcus (“staph”) that is resistant to many of the antibiotics normally used to treat staph infections, including the beta-lactate agents ampicillin, amoxicillin, methicillin, penicillin, and cephalosporin.
Diagnosis: red area on the skin; swelling; pain; warm to the touch; pus or drainage from bumps on skin; fever; positive culture of MRSA bacterium
Management: antibiotics (trimethoprim, sulfamethoxazole, clindamycin linezolid)
Vancomycin-resistant enterococci (VRE) is a bacterial infection caused by strains of enterococci bacteria that are resistant to vancomycin.
- Diagnosis: s/s of wound infection, pneumonia, UTI, meningitis, or sepsis; culture and sensitivity
- Management (general): antibiotics (amoxicillin, ampicillin, gentamicin, penicillin, piperacillin, streptomycin)
- Management (skin infections): daptomycin, linezolid, tedizolid, tigecycline
- Management (intra-abdominal infections): piperacillin-tazobactam, imipenem, meropenem
Tuberculosis
Pathophysiology
Tuberculosis (TB) is a chronic, progressive bacterial infection of the lungs. There is an initial asymptomatic infection followed by a period of latency that may develop into active disease. Active TB produces granulomatous necrosis, more commonly known as lesions. The rupturing of the lesions in the pleural space can cause empyema, bronchopleural fistulas, or a pneumothorax.
Transmission and Precautions
- Person to person through respiratory droplets
- Airborne precautions
Physical Examination
- Prolonged productive cough
- Fever and fatigue
- Night sweats
- Hemoptysis
- Dyspnea
Diagnostic Tests
- TB skin test (Mantoux skin test)
- CXR showing multinodular infiltrate near the clavicle
Management
- Supportive treatment for symptoms
- 2 months of treatment with: isoniazid (INH), rifampin (RIF), pyrazinamide (PZA), ethambutol (EMB)
- After 2 months of treatment, PZA and EMB discontinued after 2 months; INH and RIF continue for another 4-7 months
Hemorrhagic Fevers
Pathophysiology
Viral hemorrhagic fevers (VHFs) are caused by several distinct groups of RNA viruses with the potential to cause severe, emergent disease. Hemorrhagic fevers are rare in the US and are usually diagnosed in travelers returning from areas where the viruses are endemic. Symptoms will develop within 1 to 3 weeks of exposure.
|
Virus |
Endemic in |
|
Crimean-Congo Hemorrhagic Fever (CCHF) |
sub-Saharan Africa, the Middle East, Eastern Europe, Central Asia, and the Balkans |
|
Dengue Fever |
Central and South America, India, and Southeast Asia |
|
Ebola |
sub-Saharan Africa |
|
Lassa |
West Africa |
|
Marburg |
sub-Saharan Africa |
|
Yellow Fever |
tropical areas of Africa and South America |
Transmission and Precautions
- Person-to-person transmission through contact with bodily fluids or mucous membranes
- Patients with suspected VHF infection should be isolated
- PPE: gown, mask, face shield, and gloves required
Physical Examination
Most common presentation
- High fever
- Myalgia
- Abdominal pain
- Vomiting or diarrhea
- Bleeding or hemorrhage
Hantavirus pulmonary syndrome (HPS): abrupt-onset VHF symptoms followed by respiratory distress
Hemorrhagic fever with renal syndrome (HFRS)
- Early symptoms include facial flushing, eye irritation and redness and petechiae rash
- Late symptoms are hypovolemic shock and acute kidney failure that causes extreme fluid overload
Management
- Treatment for VHFs is supportive (e.g., antipyretics, fluid replacement)
- No antiviral treatment is available for most VHFs
Read More:
