Analyzing your answers to CEN Practice Questions can provide valuable insights.
BCEN Practice Test 7 with Rationale
Question 1.
The ED nurse is caring for a patient with a subdural hematoma sustained in an automobile accident. The patient currently has an ICP of 22 mmHg. Which of the following would NOT be an appropriate intervention?
(a) BMP and CBC
(b) lumbar puncture
(c) mechanical ventilation
(d) Foley catheter placement
Answer:
(b) lumbar puncture
Rationale: Lumbar punctures are contraindicated for patients with increased ICP because of the risk of brain shift caused by the sudden release of CSF pressure. Severe brain shift can result in permanent damage. BMP and CBC labs are routinely monitored in patients with increased ICP. Mechanical ventilation and Foley catheter placement are commonly ordered for patients with increased ICP.
Objective: Neurological Emergencies
Subobjective: Increased Intracranial Pressure (ICP)
Question 2.
Which of the following substances is contraindicated for an 80-year-old patient with acute heart failure?
(a) dopamine
(b) adrenaline
(c) digoxin
(d) dobutamine
Answer:
(c) digoxin
Rationale: Adrenaline, dopamine, digoxin, and dobutamine are all positive inotropes and can be helpful in the management of heart failure. However, digoxin is not recommended in the treatment of acute heart failure in an. 80-year-old patient as elderly patients are more susceptible to digoxin toxicity.
Objective: Cardiovascular Emergencies
Subobjective: Heart Failure
Question 3.
Which observation in a patient with abdominal aortic aneurysm indicates the need for immediate treatment?
(a) complaints of yellow-tinted vision
(b) hemoptysis
(c) urinary output of 75 mL/hr per urinary catheter
(d) complaints of sudden and severe back pain and dyspnea
Answer:
(d) complaints of sudden and severe back pain and dyspnea
Rationale: Sudden back pain and dyspnea indicate rupture of the aneurysm, which is an emergency. The nurse should notify the health care provider, monitor neurological and vital signs, and remain with the patient. Yellow-tinted vision is a finding of digitalis toxicity. Hemoptysis a sign of pulmonary edema. Urinary output of 75 ml/hr is normal.
Objective: Cardiovascular Emergencies
Subobjective: Aneurysm/Dissection
Question 4.
The nurse is evaluating patients for risk of heparin-induced thrombocytopenia (HIT). Which patient is at greatest risk for HIT, based on the nurse's assessment?
(a) a male patient who just completed a 1-week course of heparin
(b) a male patient taking enoxaparin for management of unstable angina
(c) a female patient receiving heparin for postsurgical thromboprophylaxis
(d) a female patient taking enoxaparin to prevent clots following a mild myocardial infarction
Answer:
(c) a female patient receiving heparin for postsurgical thromboprophylaxis
Rationale: Increased risk factors for heparin-induced thrombocytopenia (HIT) include being female and heparin use for postsurgical thromboprophylaxis. HIT is more common in patients who have been on unfractionated heparin or who have used heparin for longer than 1 week. Enoxaparin is a low-molecular-weight heparin, which carries a lower risk of causing HIT. It is often prescribed for patients with unstable angina to help increase blood flow through the heart.
Objective: Cardiovascular Emergencies
Subobjective: Thromboembolic Disease
Question 5.
During cardiac assessment of a patient with pericarditis, the nurse should expect to hear
(a) mitral regurgitation.
(b) S3 gallop.
(c) S4 gallop.
(d) pericardial friction rub.
Answer:
(d) pericardial friction rub.
Rationale: A pericardial friction rub is heard in pericarditis due to the inflammation of the pericardial layers rubbing together. Mitral regurgitation does not occur in pericarditis. An S3 gallop is heard in heart failure. S4 gallop is heard in cardiomyopathies and congenital heart disease.
Objective: Cardiovascular Emergencies
Subobjective: Pericarditis
Question 6.
Complications resulting from an untreated/undertreated high-velocity injection injury may be minimized by j
(a) educating the patient to return if signs of infection appear.
(b) administering prophylactic antibiotics.
(c) obtaining a surgical consultation and exploration.
(d) immobilizing the extremity involved.
Answer:
(c) obtaining a surgical consultation and exploration.
Rationale: High-velocity injection injuries damage underlying tissue and often result in necrosis and compartment syndrome and may require amputation. Obtaining a surgical consultation and exploration minimizes the risk of long-term complications. While administering prophylactic antibiotics, providing patient education, and immobilizing the affected extremity are correct nursing interventions, they alone will not minimize the risk for complications.
Objective: Wound
Subobjective: Injection Injuries
Question 7.
A patient arrives in the ED with midsternal chest pain radiating down the left arm and left jaw. He slumps to the floor and is unresponsive, pulseless, and apneic. High-quality compressions are started, and the patient's ECG shows the following rhythm. What is the priority nursing intervention?
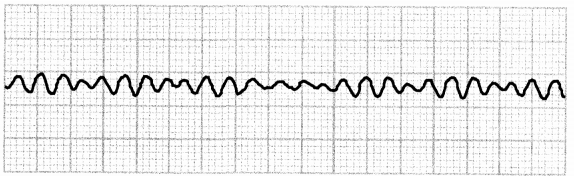
(a) administer a fluid bolus of 1L normal saline
(b) defibrillate with 200 J
(c) administer 1 mg epinephrine IV
(d) insert an advanced airway
Answer:
(b) defibrillate with 200 J
Rationale: The patient is in V-fib and is pulseless. After CPR is started, the next priority intervention is defibrillation. Epinephrine should not be administered until after defibrillation. Inserting an advanced airway may be indicated but is not the priority. A fluid bolus is not a priority for a patient in V-fib.
Objective: Cardiovascular Emergencies
Subobjective: Cardiopulmonary Arrest
Question 8.
A patient comes to the ED complaining of intermittent nausea and vomiting for the past month. She states that she has pain in the abdomen that is relieved by eating. She began having diarrhea the day before. Medical history shows that the patient takes naproxen daily for arthritis. The nurse should assess for
(a) obesity.
(b) appendicitis.
(c) hypertension.
(d) gastritis.
Answer:
(d) gastritis.
Rationale: The patient has signs and symptoms of gastritis. Pain relievers such as naproxen can inflame the lining of the stomach and lead to gastritis. Tobacco use, radiation, and viral or bacterial infection are also risk factors. Obesity, appendicitis, and hypertension are not associated with naproxen.
Objective: Gastrointestinal Emergencies
Subobjective: Gastritis
Question 9.
An infant's parents bring him to the ED because of bloody, mucous stools. The child cries constantly and pulls his knees up to his chest. Which of the following findings would be the most critical?
(a) vomiting
(b) diarrhea
(c) abdominal swelling
(d) a lump in the abdomen
Answer:
(c) abdominal swelling
Rationale: The infant has signs of intussusception, in which part of the intestine telescopes into another area of the intestine. Abdominal swelling in a child with intussusception is a sign of peritonitis, which can be life-threatening. Vomiting, diarrhea, and a lump in the abdomen are expected findings in a child with intussusception.
Objective: Gastrointestinal Emergencies
Subobjective: Intussusception
Question 10.
A patient with abdominal pain and possible appendicitis wants to leave the ED. What should the nurse do next?
(a) Inform the patient he will be involuntarily committed to the hospital if he tries to leave.
(b) Inform the physician of the patient's wish to leave.
(c) Warn the patient he will die if he leaves the department.
(d) Give the patient directions to the exit.
Answer:
(b) Inform the physician of the patient's wish to leave.
Rationale: The physician will counsel the patient on the risks associated with leaving against medical advice (AMA). Whenever possible, the patient should be counseled by the physician, sign AMA paperwork, and then leave the department. A patient with appendicitis will not be involuntarily committed. It is not appropriate to tell a patient he will die if he leaves, although he should be informed of possible negative consequences. The patient should speak with the physician before he tries to leave.
Objective: Professional Issues
Subobjective: Patient (Discharge Planning)
Question 11.
The current American Heart Association (AHA) guidelines for CPR on an adult patient with 2 rescuers is
(a) 30 compressions: 2 ventilations.
(b) 15 compressions: 2 ventilations.
(c) 30 compressions: 1 ventilation.
(d) 15 compressions: 1 ventilation.
Answer:
(a) 30 compressions : 2 ventilations.
Rationale: Current 2015 guidelines for CPR from the AHA is 30 compressions to 2 ventilations for adult patients with 2 rescuers.
Objective: Cardiovascular Emergencies
Subobjective: Cardiopulmonary Arrest
Question 12.
A patient in the ED is diagnosed with a right ventricular infarction with hypotension. The nurse should prepare to administer which of the following to treat the hypotension?
(a) normal saline fluid boluses 1 to 2 L
(b) dopamine (Intropine) at 10 mcg/kg/min
(c) D5W fluid boluses titrate 3 L
(d) furosemide drip at 20 mg/hr
Answer:
(a) normal saline fluid boluses 1 to 2 L
Rationale: Fluid boluses of 1 to 2 L normal saline should be used to treat hypotension. The patient is dehydrated at the cellular level and needs fluid resuscitation. Furosemide is used as a diuretic and would further dehydrate the patient, exacerbating the issue. Inotropes such as dopamine are used to promote cardiac contractility and will not hydrate the patient. D5W is not indicated because it is not an isotonic solution that will add to the systemic fluid volume.
Objective: Cardiac Emergencies
Subobjective: Acute Coronary Syndromes
Question 13.
Which lab results confirm a diagnosis of carbon monoxide toxicity in a nonsmoking adult?
(a) COHb 0.8%
(b) COHb 8%
(c) PaCO2 38
(d) PaCO2 41
Answer:
(b) COHb 8%
Rationale: An elevated carboxyhemoglobin (COHb) level of 2% or higher for nonsmokers and 10% or higher for smokers strongly supports a diagnosis of carbon monoxide poisoning. COHb may be measured with a fingertip pulse CO-oximeter or by serum lab values. PaCO2 measurements remain normal (38-42).
Objective: Environmental
Subobjective: Chemical Exposure
Question 14.
A 43-year-old female patient comes to the ED with complaints of vaginal discharge with itching and burning. The nurse notes a non-odorous white discharge that resembles cottage cheese. The nurse should prepare to treat the patient for which of the following?
(a) bacterial vaginosis
(b) trichomoniasis vaginitis
(c) Candida vulvovaginitis
(d) Neisseria gonorrhoeae
Answer:
(c) Candida vulvovaginitis
Rationale: A non-odorous white "cottage cheese" appearing vaginal discharge, describes Candida vulvovaginitis. Bacterial vaginosis presents with thin white, gray, or green discharge and a fishy odor. Trichomoniasis vaginitis typically presents with thin discharge and itching or burning of the genital area. Neisseria gonorrhoeae usually does not cause any symptoms but may have dysuria and thin discharge.
Objective: Gynecological
Subobjective: Infection
Question 15.
An 82-year-old patient presents to triage with a complaint of diarrhea for the past 3 days. She tells the triage nurse that she is on her third day of antibiotics. Which precautions should the nurse implement?
(a) airborne precautions
(b) contact precautions
(c) droplet precautions
(d) contact and droplet precautions
Answer:
(b) contact precautions
Rationale: The nurse should place the patient on contact precautions with concern for C. difficile. The other levels of precautions are not appropriate based on the information presented.
Objective: Communicable Diseases
Subobjective: C. Difficile
Question 16.
A 20-year-old female patient comes to the ED complaining of a green-gray frothy malodorous vaginal discharge and vaginal itching. The wet prep shows only WBCs. The nurse should prepare to assess for
(a) trichomoniasis.
(b) bacterial vaginosis.
(c) herpes simplex virus.
(d) chlamydia.
Answer:
(a) trichomoniasis.
Rationale: A greenish-gray frothy malodorous vaginal discharge and itching are signs and symptoms of trichomoniasis. Bacterial vaginosis would present with a thin discharge and presence of clue cells on the wet prep. Herpes would most likely present with lesions upon inspection. Chlamydia would not cause frothy discharge.
Objective: Gynecological
Subobjective: Infection
Question 17.
The nurse is performing an abdominal assessment on a patient with suspected heart failure. The patient asks the nurse the reason for assessing the abdomen. Which of the following would be the best response from the nurse?
(a) "Sometimes the medications used in heart failure will cause stomach upset."
(b) "Hepatomegaly, or an enlarged liver, is common in heart failure."
(c) "I am checking to see if you are constipated."
(d) "Heart failure can lead to appendicitis."
Answer:
(b) "Hepatomegaly, or an enlarged liver, is common in heart failure."
Rationale: Hepatomegaly is seen in patients with right-sided heart failure due to vascular engorgement. Heart failure does not lead to appendicitis. Constipation is not directly a result of heart failure and therefore is not a priority assessment consideration. Stomach upset is a common side effect of many medications but is not a cause for focused or priority assessment.
Objective: Cardiac Emergencies
Subobjective: Heart Failure
Question 18.
When trying to find a piece of glass in the soft tissue of the lateral thigh, which assessment technique should the nurse avoid?
(a) deep tissue palpation
(b) visual inspection
(c) palpation of distal pulses
(d) CSM of extremity
Answer:
(a) deep tissue palpation
Rationale: Deep tissue palpation should be avoided to minimize the risk of injury to •' the nurse and to prevent advancement of the foreign body deeper into the tissue structure.
Objective: Wound
Subobjective: Foreign Bodies
Question 19.
A patient's cardiac monitor shows the rhythm below. He is awake and alert but is pale and confused. His blood pressure reads 64/40 mm Hg. What is the priority nursing intervention for this patient?
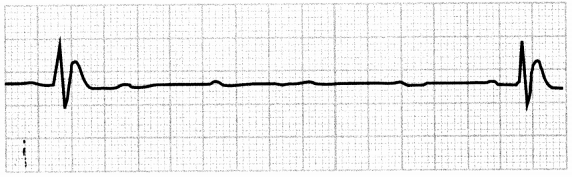
(a) defibrillate at 200 J
(b) prepare for transcutaneous pacing
(c) administer epinephrine 1 mg
(d) begin CPR
Answer:
(b) prepare for transcutaneous pacing
Rationale: The patient is unstable in a third-degree or complete heart block, so transcutaneous pacing is indicated.
Objective: Cardiovascular Emergencies
Subobjective: Dysrhythmias
Question 20.
A patient who is 28 weeks pregnant presents to the ED with a malodorous vaginal discharge, a temperature of 102.3°F (39°C), and no complaints of uterine contractions. These signs and symptoms are most indicative of which of the following?
(a) septic spontaneous abortion
(b) ectopic pregnancy
(c) missed abortion
(d) abdominal trauma
Answer:
(a) septic spontaneous abortion
Rationale: The patient's symptoms are signs of a septic abortion. An ectopic pregnancy typically presents with vaginal bleeding and pain without fever. A missed abortion may have no other symptoms except a brown discharge. The symptoms are not indicative of abdominal trauma.
Objective: Obstetrical
Question 21.
Which of the following lab values should the nurse expect to order for a patient receiving IV heparin therapy for a pulmonary embolism?
(a) hematocrit
(b) HDL and LDL
(c) PT and PTT
(d) troponin level
Answer:
(c) PT and PTT
Rationale: PT (prothrombin time) and PTT (partial thromboplastin time) are blood tests that monitor effectiveness of anticoagulant therapy. Hematocrit measures packed RBCs and is not a specific study of anticoagulant effectiveness. HDL and LDL are components of cholesterol measurement. Troponin levels measure myocardial muscle injury.
Objective: Respiratory Emergencies
Subobjective: Pulmonary Embolism
Question 22.
A patient is being treated for rapidly evolving disseminated intravascular coagulation (DIC) in the ED. Which of the following lab values would the nurse expect?
(a) increased hemoglobin
(b) decreased D-dimer
(c) increased platelets
(d) decreased fibrinogen
Answer:
(d) decreased fibrinogen
Rationale: The patient who is diagnosed with disseminated intravascular coagulation (DIC) has both a clotting and bleeding problem. Increased PT/PTT, elevated D-dimer levels, decreased platelets, decreased hemoglobin, and a decreased fibrinogen level are all expected lab values for this patient.
Objective: Medical Emergencies
Subobjective: Blood Dyscrasias
Question 23.
The nurse is caring for a patient with Guillain-Barre syndrome who is at risk for autonomic dysfunction. The nurse should monitor the patient for
(a) trigeminy.
(b) heart block.
(c) atrial flutter.
(d) tachycardia.
Answer:
(b) heart block.
Rationale: Symptoms of autonomic dysfunction include
heart block, bradycardia, hypertension, hypotension, and orthostatic hypotension. Deficits in CN X (vagus nerve) contribute to the development of autonomic dysfunction. Trigeminy, atrial flutter, and tachycardia are not symptoms of autonomic dysfunction.
Objective: Neurological Emergencies
Subobjective: Guillain-Barre Syndrome
Question 24.
Which of the following procedures can be performed under procedural sedation in the ED?
(a) perimortem cesarean section
(b) synchronized cardioversion
(c) dilatation and curettage
(d) open fracture reduction
Answer:
(b) synchronized cardioversion
Rationale: Procedural sedation is appropriate for synchronized cardioversion. A perimortem cesarean section is typically done emergently. Open fracture reductions should occur in the operating room, as should dilatation and curettage.
Objective: Professional Issues
Subobjective: Patient (Pain Management and Procedural Sedation)
Question 25.
A nurse notes crackles while assessing lung sounds in a child with pneumonia. How would the nurse classify this respiratory disorder?
(a) upper airway disorder
(b) lower airway disorder
(c) lung tissue disorder
(d) disordered control of breathing
Answer:
(c) lung tissue disorder
Rationale: Lung tissue disorders include pneumonia and pulmonary edema. Examples of lower airway disorders are bronchiolitis and asthma. An upper airway disorder would be croup, anaphylaxis, or foreign body obstruction. Disordered control of breathing means an irregular, slow breathing pattern with a neurological component, such as a seizure.
Objective: Respiratory Emergencies
Subobjective: Infections
Question 26.
The ECG in the exhibit supports the diagnosis of
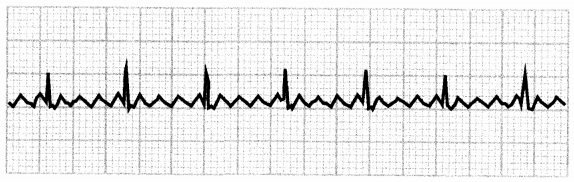
(a) atrial flutter.
(b) atrial fibrillation.
(c) torsades de pointes.
(d) ventricular fibrillation.
Answer:
(a) atrial flutter.
Rationale: In atrial flutter, there are no discernible P waves, and a distinct sawtooth wave pattern is present. The atrial rate is regular, and the PR interval is not measurable. In atrial fibrillation, the rhythm would be very irregular with coarse, asynchronous waves. Torsades de pointes, or "twisting of the points," is characterized by QRS complexes that twist around the baseline and is a form of polymorphic ventricular tachycardia. It may resolve spontaneously or progress to ventricular fibrillation, which is emergent, as the ventricles are unable to pump any blood due to disorganized electrical activity. Untreated, it quickly leads to cardiac arrest.
Objective: Cardiovascular Emergencies
Subobjective: Dysrhythmias
Question 27.
A patient who was playing basketball outside all day has been drinking only water to stay hydrated. He suddenly became confused, complained of a headache, and collapsed. The nurse should suspect
(a) hyperkalemia.
(b) hyponatremia.
(c) hypernatremia.
(d) hypokalemia.
Answer:
(b) hyponatremia.
Rationale: The patient has been playing sports, sweating and replacing lost fluid with only water, which can cause hyponatremia. A loss of sodium will cause neurological effects such as confusion, seizures, and coma. The symptoms are not indicative of a potassium imbalance. Hyperkalemia would cause thirst and nausea/vomiting.
Objective: Medical Emergencies
Subobjective: Electrolyte/Fluid Imbalance
Question 28.
Which of the following medications should a nurse anticipate administering to an 18-month-old patient with a barking cough first?
(a) epinephrine 0.01 mg/kg IV stat
(b) nebulized epinephrine breathing treatment
(c) albuterol breathing treatment
(d) dexamethasone PO or IV
Answer:
(b) nebulized epinephrine breathing treatment
Rationale: A barking cough is a symptom of croup, and nebulized epinephrine is the treatment of choice. IV epinephrine is not indicated in croup; it is more often used in anaphylaxis and resuscitation efforts. Albuterol has a primary effect on lower lung structures and will not improve symptoms of croup. Dexamethasone is indicated for croup but is not the priority intervention.
Objective: Respiratory Emergencies
Subobjective: Infections
Question 29.
Classic signs of Bell's palsy include
(a) facial droop, dysphagia, dysarthria.
(b) facial droop, confusion, ataxia.
(c) hemiparalysis, photophobia, headache.
(d) tinnitus, nausea, vertigo.
Answer:
(a) facial droop, dysphagia, dysarthria.
Rationale: Bell's palsy is caused by an inflammation of the seventh cranial nerve and presents with facial paralysis and weakness.
Objective: Maxillofacial
Subobjective: Facial Nerve Disorders
Question 30.
Which of the following is most likely to be found in a patient with left-sided heart failure?
(a) jugular vein distention
(b) crackles
(c) hepatomegaly
(d) ascites
Answer:
(b) crackles
Rationale: Left-sided heart failure manifestations include pulmonary symptoms such as crackles and dyspnea. Right-sided heart failure causes systemic congestion, leading to hepatomegaly, dependent edema, jugular vein distention, and ascites.
Objective: Cardiovascular Emergencies
Subobjective: Heart Failure
Question 31.
Localized pain and edema associated with systemic fever and left shift differential may be indicative of
(a) foreign body infection of surgical hardware.
(b) superficial foreign body.
(c) buckle fracture.
(d) Achilles tendon rupture.
Answer:
(a) foreign body infection of surgical hardware.
Rationale: Foreign body infections and cellulitis of surgical hardware sites present with local pain and systemic infectious indicators such as fever, edema, warmth, and elevated WBCs with left shift in neutrophils.
Objective: Orthopedic
Subobjective: Foreign Bodies
Question 32.
The most common site of injection injuries is
(a) the second digit of the nondominant hand.
(b) the first digit of the nondominant hand.
(c) the second digit of the dominant hand.
(d) the first digit of the dominant hand.
Answer:
(a) the second digit of the nondominant hand.
Rationale: The second digit of the nondominant hand is the most common site, as these types of injuries are usually self-inflicted.
Objective: Wound
Subobjective: Injection Injuries
Question 33.
A 12-year-old patient is brought to the ED after falling 15 feet out of a tree. She is complaining of severe pain in the right side of the chest and severe dyspnea. Upon auscultation, the nurse notes absent breath sounds on the right and should suspect
(a) pneumothorax.
(b) foreign body lodged in the right side of the chest.
(c) hematoma.
(d) pleural effusion.
Answer:
(a) pneumothorax.
Rationale: Absent or decreased breath sounds are present in a pneumothorax. A nurse would be able to visualize a foreign body on the right side of chest while doing the initial assessment. Hematoma and pleural effusion are both associated with decreased breath sounds, not with absent sounds.
Objective: Respiratory Emergencies
Subobjective: Pneumothorax
Question 34.
A patient with a subarachnoid hemorrhage from a fall at home arrives at the ED. When reviewing the medical orders, which medication order should prompt the nurse to notify the health care provider?
(a) warfarin
(b) morphine
(c) nimodipine
(d) a stool softener
Answer:
(a) warfarin
Rationale: Warfarin is an anticoagulant commonly prescribed for patients with A-fib. Any anticoagulant must be given cautiously to patients with subarachnoid hemorrhage due to the increased risk of bleeding. Morphine is commonly prescribed for pain, and nimodipine is given to treat or prevent cerebral vasospasm. Stool softeners are given to reduce the need to strain during a bowel movement.
Objective: Neurological Emergencies
Subobjective: Trauma
Question 35.
Which symptom, identified by the patient, is the most common and consistent with a myocardial infarction?
(a) palpitations
(b) lower extremity edema
(c) feeling of pressure in the chest
(d) nausea
Answer:
(c) feeling of pressure in the chest
Rationale: An uncomfortable feeling of pressure, squeezing, fullness, or pain in the center of the chest is the predominant symptom of a myocardial infarction (Ml), particularly in women. Palpitations indicate a dysrhythmia. Edefna in the lower extremities is a later sign of cardiac failure. A feeling of nausea is not common with Ml.
Objective: Cardiovascular Emergencies
Subobjective: Acute Coronary Syndrome
Question 36.
A patient arrives to the ED with a grossly deformed shoulder injury obtained while surfing. Suspecting a dislocation, which nursing intervention should the nurse initiate immediately?
(a) elevate the extremity
(b) put patient on NPO status
(c) apply ice
(d) provide ice chips
Answer:
(b) put patient on NPO status
Rationale: NPO status is essential for all suspected surgical cases. Elevation is limited with regard to injury. Ice, while therapeutic, would not be a priority intervention.
Objective: Orthopedic
Subobjective: Fractures/Dislocations
Question 37.
Which of the following statements should be included in the discharge instructions for a patient who has been prescribed carbamazepine to control seizures?
(a) Avoid exposure to sunlight.
(b) Limit foods high in vitamin K.
(c) Do not take on an empty stomach.
(d) Use caution when driving or operating machinery.
Answer:
(d) Use caution when driving or operating machinery.
Rationale: Carbamazepine may cause dizziness or drowsiness. The patient should use caution while driving or operating machinery until he understands how the medication will affect him. There is no contraindication to sunlight exposure with this medication. Dietary concerns with carbamazepine are limited to consulting the health care provider before taking with grapefruit juice.
Objective: Neurological Emergencies
Subobjective: Seizure Disorders
Question 38.
The nurse is caring for a patient with a traumatic brain injury who has a Glasgow Coma Scale (GCS) of 7. The nurse should anticipate the need to
(a) bolus with NS via IV.
(b) assist patient to chair.
(c) assist with intubation.
(d) apply 2L 02 via nasal cannula.
Answer:
(c) assist with intubation.
Rationale: A Glasgow Coma Scale (GCS) of 7 indicates that the patient is experiencing deficits in eye-opening, motor response, and verbal response. As the GCS drops, the patient is less alert and able to follow commands. Patients with a GCS of 7 will require intubation to maintain oxygenation.
The lower the GCS, the less likely the patient is to fully recover without permanent deficits. An IV bolus will not negate the need for assisted breathing. This patient will be unable to get up to a chair. As the GCS drops, a nasal cannula becomes ineffective at providing oxygenation.
Objective: Neurological Emergencies
Subobjective: Trauma
Question 39.
The nurse is caring for a patient who just had a lumbar puncture to rule out meningitis. Which assessment finding would prompt the nurse to notify the health care provider?
(a) The patient is drinking fluids.
(b) The patient is lying flat in the bed.
(c) The patient's pain scale is 3 out of 10.
(d) The patient complains of severe headache.
Answer:
(d) The patient complains of severe headache.
Rationale: A severe headache indicates increased intracranial pressure (ICP), a complication of lumbar puncture. The health care provider should be notified immediately. Other indications of increased ICP are nausea, vomiting, photophobia, and changes in LOC. The patient should be encouraged to increase fluid intake unless contraindicated. The patient will remain flat and on bed rest following the procedure, per agency and health care provider guidelines. Minor pain controlled with analgesics is not a concern but should be monitored for changes.
Objective: Neurological Emergencies
Subobjective: Meningitis
Question 40.
A patient presents with signs and symptoms characteristic of myocardial infarction (Ml). Which of the following diagnostic tools should the nurse anticipate will be used to determine the location of the myocardial damage?
(a) electrocardiogram
(b) echocardiogram
(c) cardiac enzymes
(d) cardiac catheterization
Answer:
(a) electrocardiogram
Rationale: The electrocardiogram (ECG) is most commonly used to initially determine the location of myocardial damage. An echocardiogram is used to view myocardial wall function after a myocardial infarction (Ml) has been diagnosed. Cardiac enzymes will aid in diagnosing an Ml but will not determine the location. While not performed initially, cardiac catheterization determines coronary artery disease and would suggest the location of myocardial damage.
Objective: Cardiovascular Emergencies
Subobjective: Acute Coronary Syndrome
Question 41.
The ED nurse is waiting for a bed for a 72-year-old patient with Alzheimer's disease who has episodes of confusion. Which of the following will be included in the plan of care for this patient?
(a) prescribe haloperidol to prevent agitation
(b) provide toileting every 2 hours
(c) use restraints at night to prevent wandering
(d) allow choices when possible to promote feelings of respect
Answer:
(b) provide toileting every 2 hours
Rationale: As Alzheimer's disease progresses, confusion increases. Providing regular toileting can prevent possible falls that result when to hurrying to the bathroom to maintain continence. Haloperidol should be used with extreme caution in geriatric patients with Alzheimer's. Restraints can increase confusion in these patients and should be used only per facility guidelines. Offering too many choices can overwhelm the patient and lead to increased confusion and frustration.
Objective: Neurological Emergencies
Subobjective: Alzheimer's Disease/Dementia
Question 42.
A 16-year-old patient arrives to the ED after ingesting an entire bottle of acetaminophen 4 hours before. The most appropriate intervention is
(a) administration of N-acetylcysteine.
(b) endotracheal intubation.
(c) administration of naloxone.
(d) gastric lavage.
Answer:
(a) administration of N-acetylcysteine.
Rationale: N-acetylcysteine is the antidote for acetaminophen toxicity and is administered to patients with hepatotoxic levels of serum acetaminophen levels. Intubation is not indicated, and naloxone is not the correct antidote. Gastric lavage is not indicated in this circumstance.
Objective: Communicable Diseases
Subobjective: Overdose and Ingestion
Question 43.
A patient with emphysema comes to the ED complaining of dyspnea. The nurse should assist the patient into which of the following positions?
(a) lying flat on the back
(b) in a prone position
(c) sitting up and leaning forward
(d) lying on the side with feet elevated
Answer:
(c) sitting up and leaning forward
Rationale: The patient with emphysema can gain optimal lung expansion by sitting up and leaning forward. Lying in a prone position, flat on the back, or on the side with feet elevated will further potentiate any airway obstruction and effort, exacerbating the problem.
Objective: Respiratory Emergencies
Subobjective: Chronic Obstructive Pulmonary Disease
Question 44.
A patient with severe dementia is brought to the ED for urinary retention. The patient repeatedly asks for her mother, who passed away many years ago. Which technique should the nurse use when the patient asks for her mother?
(a) confrontation
(b) reality orientation
(c) validation therapy
(d) seeking clarification
Answer:
(c) validation therapy
Rationale: Validation therapy is used with patients with severe dementia when reality orientation is not appropriate. The nurse may ask the patient what her mother looks like or what she is wearing but does not argue about whether her mother is living. This allows the nurse to acknowledge the patient's concerns while avoiding confrontation or encouraging further belief that her mother is alive. Confrontation may cause the patient with dementia to react inappropriately and is used only when the nurse has established patient trust. Reality orientation works best with patients in the early stages of dementia. Seeking clarification will only cause more confusion because the nurse is asking the patient to explain something, which can lead to patient frustration.
Objective: Neurological Emergencies
Subobjective: Alzheimer's Disease/Dementia
Question 45.
The nurse sees a bedbug on the personal linens of a child transported from the home setting to the ED via ambulance. What is the most appropriate action?
(a) Place the patient on airborne precautions.
(b) File a report with the local child welfare agency.
(c) Wash the patient thoroughly and replace all linens and clothing items with hospital-provided materials.
(d) Ask the parents to provide new clothing and linen from the home.
Answer:
(c) Wash the patient thoroughly and replace all linens and clothing items with hospital-provided materials.
Rationale: The patient should be thoroughly washed, and all linens and clothing items should be replaced with hospital-provided materials to prevent spread of bedbugs. All home-provided clothing and linens must be double-bagged and either disposed of or placed in a dryer on hot setting for 30 minutes. The presence of bedbugs is not necessarily a sign of abuse or neglect and therefore does not warrant a call to child welfare services. Contact precautions would be most appropriate.
Objective: Environmental
Subobjective: Parasite and Fungal Infestations
Question 46.
The nurse is caring for a patient with suspected diverticulitis. The nurse should anticipate all of the following findings EXCEPT
(a) fever.
(b) anorexia.
(c) lower abdominal pain.
(d) low WBC count.
Answer:
(d) low WBC count.
Rationale: A patient with diverticulitis would be expected to have lower abdominal pain ' with anorexia and fever in addition to an elevated WBC count.
Objective: Gastrointestinal Emergencies
Subobjective: Diverticulitis
Question 47.
A patient presents to the ED with abdominal pain and is found to have an incarcerated hernia. The patient is prepared for surgery. Which assessment finding by the nurse should be reported immediately to the health care provider?
(a) a burning sensation at the site of the hernia
(b) sudden nausea and vomiting with increased pain since arrival
(c) a palpable mass in the abdomen
(d) pain that occurs when bending over or coughing
Answer:
(b) sudden nausea and vomiting with increased pain since arrival
Rationale: An increase in pain with nausea and vomiting are signs that an incarcerated hernia may be causing a bowel obstruction and should be reported immediately. The other findings are expected in a patient with a hernia and do not need to be immediately reported to the health care provider.
Objective: Gastrointestinal Emergencies
Subobjective: Hernia
Question 48.
EMS arrives to the ED with a stable adult patient who has a clear developmental delay. Emergent intervention is not needed upon arrival. What should the ED nurse do before treating the patient?
(a) Call the legal guardian of the patient to obtain consent for care.
(b) Continue to care for the patient.
(c) Obtain consent for care from the patient.
(d) Obtain permission from the hospital legal department to care for the patient.
Answer:
(a) Call the legal guardian of the patient to obtain consent for care.
Rationale: If the patient has diminished decisional capacity due to a developmental delay, the legal guardian must consent to any intervention for the patient unless there is an emergent issue.
Objective: Professional Issues
Subobjective: System (Patient Consent for Treatment)
Question 49.
A patient arrives at the ED complaining of severe pain to the right lower abdominal quadrant. The patient states that the pain is worse with coughing. The nursing assessment reveals that pain is relieved by bending the right hip. The patient has not had a bowel movement in three days. The nurse should anticipate all of the following interventions EXCEPT
(a) IV fluids.
(b) morphine 2mg IV.
(c) STAT MRI of abdomen.
(d) maintain NPO status.
Answer:
(c) STAT MRI of abdomen.
Rationale: This patient is experiencing appendicitis. Pain that is relieved by bending the right hip suggests perforation and peritonitis. The patient would not need an abdominal MRI based on her symptoms. The patient will need surgery, so maintaining NPO status and administering IV fluids are a priority. Morphine will be given for pain.
Objective: Gastrointestinal Emergencies
Subobjective: Acute Abdomen
Question 50.
A patient is admitted to the ED with an acute myocardial infarction (Ml). The nurse is preparing the patient for transport to the cardiac catheterization laboratory. An alarm sounds on the cardiac monitor, and the patient becomes unresponsive. V-fib is noted. The nurse should anticipate doing which of the following first? ,
(a) beginning high-quality CPR
(b) defibrillation at 200 J
(c) administering epinephrine 1 mg
(d) placing an IV
Answer:
(a) beginning high-quality CPR
Rationale: The first priority for an unresponsive patient in V-fib is performing high-quality CPR. The patient should then be prepared to be defibrillated. Epinephrine should be administered after the patient has been defibrillated at least twice. IV access is not the initial priority.
Objective: Cardiovascular Emergencies
Subobjective: Dysrhythmias
Question 51.
A nursing home patient with an enterocutaneous fistula caused by an acute exacerbation of Crohn's disease arrives at the ED. The nursing priority is to
(a) administer antibiotics.
(b) preserve and protect the skin.
(c) apply a wound VAC to the area.
(d) provide quiet times for relaxation.
Answer:
(b) preserve and protect the skin.
Rationale: The nursing priority for patients with fistulas is preserving and protecting the skin. The nurse should inspect the skin frequently and assess for any redness, irritation, or broken areas. The skin should remain dry and intact. Antibiotics may be given but are not the first priority. Wound VACs should not be used simply to manage drainage or in patients with increased bleeding risk. Providing a quiet environment is important, but skin integrity is the first priority with this patient.
Objective: Gastrointestinal Emergencies
Subobjective: Inflammatory Bowel Disease
Question 52.
A patient with cardiogenic shock is expected to have
(a) hypertension; dyspnea.
(b) decreased urine output; warm, pink skin.
(c) increased urine output; cool, clammy skin.
(d) hypotension; weak pulse; cool, clammy skin.
Answer:
(d) hypotension; weak pulse; cool, clammy skin.
Rationale: Classic signs of cardiogenic shock include a rapid pulse that weakens; cool, clammy skin; and decreased urine output. Hypotension is another classic sign.
Objective: Cardiovascular Emergencies
Subobjective: Shock
Question 53.
A patient in the ED with chronic pain is requesting more intravenous pain medication for reported 10/10 pain. The physician will not give any more medication. How should the nurse approach this patient?
(a) Inform the patient that it is the physician's decision.
(b) Discuss chronic pain relief and realistic expectations with the patient.
(c) Ignore the patient's pain complaint.
(d) Discuss drug-seeking concerns with the patient.
Answer:
(b) Discuss chronic pain relief and realistic expectations with the patient.
Rationale: Having a frank, professional conversation regarding chronic pain relief is the nurse's priority. The nurse should not immediately assume the patient is drug-seeking, nor should the nurse ignore the patient's pain complaint.
Objective: Professional Issues
Subobjective: Patient (Pain Management and Procedural Sedation)
Question 54.
Which appearance is most consistent with an avulsion?
(a) open wound with presence of sloughing and eschar tissue
(b) skin tear with approximated edges
(c) shearing of the top epidermal layers
(d) separation of skin from the underlying structures that cannot be approximated
Answer:
(d) separation of skin from the underlying structures that cannot be approximated
Rationale: An avulsion is characterized by the separation of skin from the underlying structures that cannot be approximated.
Objective: Wound
Subobjective: Avulsions
Question 55.
The ED nurse receives a patient with a blunt-force abdominal injury due to a knife wound. On inspection, a common kitchen knife is found in the patient's abdomen in the upper right quadrant. The>patient is rapidly placed on a non-rebreather mask, two large-bore IVs are started, and labs are drawn. No evisceration is noted. Which should the nurse do next?
(a) Notify next of kin.
(b) Estimate blood loss.
(c) Stabilize the knife with bulky dressings.
(d) Attempt to gently pull the knife straight out.
Answer:
(c) Stabilize the knife with bulky dressings.
Rationale: The priority for this patient is to prepare for surgical removal of the knife, so it should be stabilized with bulky dressings to avoid shifting as the patient is transported. The nurse should never attempt to remove an embedded object in a patient, as this is beyond the scope of practice for nursing. Blood loss may be estimated based on how many dressings or towels are saturated. Next of kin should be notified only after the patient is stabilized.
Objective: Gastrointestinal Emergencies
Subobjective: Abdominal Trauma
Question 56.
In a hypothermic patient, hypovolemia occurs as the result of
(a) diuresis and third spacing.
(b) shivering and vasoconstriction.
(c) diaphoresis and dehydration.
(d) tachycardia and tachypnea.
Answer:
(a) diuresis and third spacing.
Rationale: Dysfunction of the renal cells and decreased levels of ADH hormone/ vasopressin lead to diuresis, and fluid leakage into the interstitial spaces further contributes to hypovolemia. Shivering and vasoconstriction mask the symptoms of hypovolemia rather than contribute to it. Diaphoresis, dehydration, tachycardia, and tachypnea are all common symptoms of hyperthermia.
Objective: Environmental
Subobjective: Temperature-Related Emergencies
Question 57.
A 14-year-old male patient is brought to the ED, stating he woke up in the middle of the night with sudden, severe groin pain and nausea. The pain persists despite elevation of the testes. These findings most likely indicate
(a) testicular torsion.
(b) epididymitis.
(c) UTI.
(d) orchitis.
Answer:
(a) testicular torsion.
Rationale: A sudden, severe onset of testicular pain indicates the possibility of testicular torsion and a stat ultrasound should be ordered to confirm. Epididymitis typically presents gradually with unilateral pain and discharge, and pain is relieved with elevation of the testes. Sudden, severe pain is not an indication of UTI or orchitis.
Objective: Genitourinary
Subobjective: Testicular Torsion
Question 58.
A 16-year-old patient is brought to the ED complaining of abdominal pain, nausea, and sharp constant pain on both sides of the pelvis. She has a history of pelvic inflammatory disease and is not sexually active. The nurse notes a purulent vaginal discharge. These signs and symptoms are most indicative of which condition?
(a) ectopic pregnancy
(b) tubo-ovarian abscess
(c) diverticulitis
(d) ruptured appendix
Answer:
(b) tubo-ovarian abscess
Rationale: A purulent vaginal discharge with bilateral pelvic pain and nausea are symptoms of a tubo-ovarian abscess. An ectopic pregnancy would most commonly present with vaginal bleeding, not purulent discharge. A ruptured appendix would typically present as RLQ pain. Diverticulitis may cause abdominal pain and nausea but not purulent vaginal discharge.
Objective: Gynecological
Subobjective: Infection
Question 59.
A patient who is 9 weeks pregnant comes to the ED with complaints of abdominal cramping. During the physical assessment, the nurse notes slight vaginal bleeding and a large, solid tissue clot. These findings most likely indicate
(a) septic spontaneous abortion.
(b) incomplete spontaneous abortion.
(c) threatened abortion.
(d) complete spontaneous abortion.
Answer:
(d) complete spontaneous abortion.
Rationale: Abdominal cramping with vaginal bleeding and expulsion of tissue are signs of a complete spontaneous abortion. An incomplete spontaneous abortion would have retained tissue. Septic abortions are typically febrile. A threatened abortion may progress to a spontaneous abortion but would not result in passing a large solid tissue clot.
Objective: Obstetrical
Subobjective: Threatened/Spontaneous Abortion
Question 60.
A 4-month-old infant is brought to the ED with croup. Which of the following medications will the nurse administer in order to decrease inflammation?
(a) ipratropium
(b) albuterol
(c) corticosteroids
(d) antibiotics
Answer:
(c) corticosteroids
Rationale: Corticosteroids will be administered to decrease inflammation of the airways. Albuterol and ipratropium are bronchodilators and do not address the swelling and inflammation caused by croup. Antibiotics are not indicated for croup.
Objective: Respiratory Emergencies
Subobjective: Infections
Question 61.
A 21-year-old male patient reports to the ED with complaints of burning on urination and urethral itching. During the assessment, the nurse notes a mucopurulent discharge and no lesions. These signs and symptoms are most indicative of which of the following?
(a) chlamydia
(b) syphilis
(c) HPV
(d) herpes simplex virus
Answer:
(a) chlamydia
Rationale: Mucopurulent discharge, burning, and itching are symptoms of chlamydia. A herpes infection would have lesions. Syphilis typically presents with a small, painless sore. HPV typically presents asymptomatically but may also have warts.
Objective: Gynecological
Subobjective: Infection
Question 62.
The mother of a 3-year-old patient diagnosed with varicella asks for the best at-home treatment. Which of the following treatments is NOT appropriate for the nurse to suggest?
(a) oral antihistamines
(b) colloidal oatmeal baths
(c) acetaminophen
(d) aspirin
Answer:
(d) aspirin
Rationale: Aspirin is contraindicated for children with varicella because it can lead to Reye syndrome, a rare form of encephalopathy. Antihistamines, colloidal oatmeal baths, and non-aspirin antipyretics such as acetaminophen are all recommended in-home therapies to relieve symptoms.
Objective: Communicable Diseases
Subobjective: Childhood Diseases
Question 63.
A full-term neonate is delivered in the ED. After stimulation and suctioning, the infant is apneic with strong palpable pulses at 126/minute. The nursing priority is to
(a) rescue breaths at 12 - 20 breaths per minute.
(b) rescue breaths at 40 - 60 breaths per minute.
(c) insert endotracheal intubation.
(d) insert an LMA.
Answer:
(b) rescue breaths at 40 - 60 breaths per minute.
Rationale: Current NRP guidelines (2015) recommend 40 - 60 breaths per minute for rescue breathing in the newborn. Rescue, breaths at a rate of 12 - 20 are not adequate to provide enough ventilation for the neonate. Inserting an LMA or intubation may be indicated but is not the immediate nursing priority.
Objective: Obstetrical
Subobjective: Neonatal Resuscitation
Question 64.
A pediatric patient in cardiopulmonary arrest has had a 40-minute resuscitation attempt in the ED. The ED nurse feels that the resuscitation is reaching the point of concern for medical futility. What is the nurse's responsibility at this time?
(a) Tell the parents to order the resuscitation attempt to be stopped.
(b) Suggest that the team leader consider ending the resuscitation.
(c) Order the team to stop the resuscitation.
(d) Continue with the resuscitation and allow the team leader to decide when to stop.
Answer:
(b) Suggest that the team leader consider ending the resuscitation.
Rationale: As a member of the team the nurse can suggest to the team leader to consider the futility of the resuscitation at that point. The nurse does not have the authority to end the resuscitation and should not advise the patient's parents to make that decision. Ethically, the nurse should speak up if he or she feels that the efforts are futile.
Objective: Professional Issues
Subobjective: Patient (End-of-Life Issues)
Question 65.
After an emergent delivery, a full-term infant is apneic with a pulse rate of 48 bpm. The infant has not responded to chest compressions. The nurse should prepare to administer
(a) atropine 0.5 mg/kg.
(b) epinephrine 0.01 - 0.03 mg/kg.
(c) sodium bicarbonate 1 to 2 mEq/mL.
(d) dobutamine drip.
Answer:
(b) epinephrine 0.01 - 0.03 mg/kg.
Rationale: The current (2015) guidelines for neonatal resuscitation recommend epinephrine to be administered at 0.01 - 0.03mg/kg. The other medication dosages are not appropriate as a first-line medication to be administered to a neonate with bradycardia.
Objective: Obstetrical
Subobjective: Neonatal Resuscitation
Question 66.
Which treatment is appropriate for a minor blunt injury resulting in intact skin, ecchymosis, edema, and localized pain and tenderness?
(a) fasciotomy and opioid pain medications
(b) rest, ice, compression, elevation, and opioid pain medications
(c) rest, ice, compression, elevation, and use of NSAIDs
(d) immobilization and use of NSAIDs
Answer:
(c) rest, ice, compression, elevation, and use of NSAIDs
Rationale: Contusions accompanied by the symptoms mentioned should be treated with rest, ice, compression, and elevation. NSAIDs will provide appropriate pain relief; opioid therapy is not indicated for minor contusions.
Objective: Orthopedic
Subobjective: Trauma
Question 67.
A patient with depression and Alzheimer's disease presents to the ED complaining of abdominal pain. In reviewing the patient's health care orders, which medication should prompt the nurse to notify the health care provider?
(a) sertraline
(b) paroxetine
(c) memantine
(d) amitriptyline
Answer:
(d) amitriptyline
Rationale: Amitriptyline is a tricyclic antidepressant. This class of drugs has anticholinergic effects, which frequently cause serious side effects. In older, confused patients such as those with Alzheimer's disease, amitriptyline can cause increased confusion, constipation, and urinary retention. Paroxetine and sertraline are SSRIs and may be given to patients with Alzheimer's. Memantine is an NMDA receptor antagonist prescribed to slow the progression of Alzheimer's.
Objective: Neurological Emergencies
Subobjective: Alzheimer's Disease/Dementia
Question 68.
A 14-year-old patient arrives to the ED with delirium, respiratory distress, and headache. Upon examination of the airway, the nurse notes a burn to the roof of the patient's mouth. What does the nurse suspect?
(a) ingestion of a hot beverage
(b) inhalation of chemicals from a compressed gas can
(c) ingestion of dry ice
(d) marijuana use
Answer:
(b) inhalation of chemicals from a compressed gas can
Rationale: Adolescent patients presenting with frostbite burns to the roof of the mouth are most likely abusing inhalants, typically in the form of aerosols, glues, paints, and solvents. A hot beverage would not cause the other symptoms, nor would marijuana use. Dry ice would cause tissue injury to the entire mouth.
Objective: Communicable Diseases
Subobjective: Substance Abuse
Question 69.
The nurse is caring for a patient who was brought to the ED with seizures. The patient begins having a seizure. The nursing priority is
(a) padding the bed rails.
(b) inserting a tongue blade.
(c) administering IV diazepam.
(d) turning the patient to his side.
Answer:
(d) turning the patient to his side.
Rationale: Adolescent patients presenting with frostbite burns to the roof of the mouth are most likely abusing inhalants, typically in the form of aerosols, glues, paints, and solvents. A hot beverage would not cause the other symptoms, nor would marijuana use. Dry ice would cause tissue injury to the entire mouth.
Objective: Communicable Diseases
Subobjective: Substance Abuse
Question 70.
A patient who is 32 weeks pregnant is having profuse bright red painless vaginal bleeding after being in a motor vehicle crash (MVC). The nurse should prepare to treat her for
(a) abruptio placentae.
(b) placenta previa.
(c) ectopic pregnancy.
(d) complete abortion.
Answer:
(b) placenta previa.
Rationale: The patient has suffered trauma in the motor vehicle crash (MVC). The bright red painless vaginal bleeding is a sign of placenta previa. Abruptio placentae results in painful bleeding that is typically dark red. An ectopic pregnancy and complete abortion would not occur due to an MVC.
Objective: Obstetrical
Subobjective: Placenta Previa
Question 71.
A 30-week pregnant patient comes to the ED after falling down a flight of steps. She complains of uterine tenderness, and a small amount of dark bloody vaginal drainage is noted. The nurse should suspect
(a) abruptio placenta.
(b) placenta previa.
(c) incomplete spontaneous abortion.
(d) complete spontaneous abortion.
Answer:
(a) abruptio placenta.
Rationale: Abdominal tenderness and dark red vaginal bleeding are signs of abruptio placenta. Placenta previa would present with bright red painless bleeding. Spontaneous abortions typically do not occur after 20 weeks.
Objective: Obstetrical
Subjective: Abruptio Placenta
Question 72.
The ED nurse is caring for a patient with schizophrenia. The patient appears to be looking at someone and asks the nurse, "Aren't you going to speak to Martha?" No one else is in the room. Which response by the nurse is appropriate?
(a) "There's nobody there."
(b) "I will find a blanket for Martha."
(c) "Is Martha going to stay a while?"
(d) "Does Martha ever tell you to hurt yourself or others?"
Answer:
(d) "Does Martha ever tell you to hurt yourself or others?"
Rationale: Safety is the priority for patients with altered mental status. The nurse should ask if the patient is hearing voices telling him to harm himself or others. Simply saying that no one is there dismisses the patient's feelings. Offering to find a blanket validates the delusion that someone is there. Asking if Martha is staying also prevents reality orientation and may worsen the patient's confusion.
Objective: Psychosocial Emergencies
Subobjective: Psychosis
Question 73.
A patient in the ED is having difficulty breathing and is diagnosed with a large pleural effusion. The nurse prepares her for which of the following procedures?
(a) pericardiocentesis
(b) chest tube insertion
(c) thoracentesis
(d) pericardial window
Answer:
(c) thoracentesis
Rationale: A thoracentesis is performed to remove the fluid. A chest tube is used to decompress a hemothorax or pneumothorax and is not indicated m the presence of pleural effusion. A pericardial window is used to drain excess fluid from the pericardium, not the pleural space.
Objective: Respiratory Emergencies
Subobjective: Pleural Effusion
Question 74.
When caring for a patient with esophageal varices, the nurse should first prepare to administer
(a) phenytoin
(b) octreotide
(c) levofloxacin
(d) pantoprazole
Answer:
(b) octreotide
Rationale: Esophageal varices can lead to death via hemorrhage. Octreotide is a vasoconstrictor used to control bleeding before performing endoscopy. Phenytoin is an anticonvulsant, levofloxacin is an antibiotic, and pantoprazole is a proton pump inhibitor; none of these are indicated at this time.
Objective: Gastrointestinal Emergencies
Subobjective: Esophageal Varices
Question 75.
The ED nurse is caring for a patient who is deeply depressed following the death of her mother. She tells the nurse, "I just lost my world when Mom died. She was my anchor, and now I have no one." Which response by the nurse is the most appropriate?
(a) "You will feel better in time."
(b) "You should join a grief support group."
(c) "I felt the same way when my mother died."
(d) "You're feeling lost since your mother died."
Answer:
(d) "You're feeling lost since your mother died."
Rationale: "You're feeling lost since your mother died," Use the therapeutic technique of restating. The nurse repeats the patient's words back to her. This therapeutic communication technique allows the patient to verify that the nurse understood the patient and allows for clarification if needed. It also encourages the patient to continue. Telling the patient that she will feel better in time minimizes the patient's feelings and sounds uncaring. Telling the patient to join a grief support group forces the nurse's decision onto the patient. Stating shared feelings takes the focus from the patient to the nurse.
Objective: Psychosocial Emergencies
Subobjective: Depression
Question 76.
A patient is admitted to the ED with chest pain. A 12-lead ECG is performed with ST elevations noted in leads II, III and aVF. The nurse should prepare to administer
(a) nitrates.
(b) diuretics.
(c) morphine.
(d) IV fluids.
Answer:
(d) IV fluids.
Rationale: The symptoms indicate right¬sided myocardial infarction (Ml), so IV fluids are the priority treatment for this patient. When treating patients with right ventricular infarction, nitrates, diuretics, and morphine are to be avoided due to their pre-load-reducing effects.
Objective: Cardiac Emergencies
Subobjective: Acute Coronary Syndromes
Question 77.
A 20-year-old male college student arrives to the ED during spring break complaining of a headache, fever, nausea, and vomiting. He shows the ED nurse a petechial rash on his trunk and chest. Which of the following should the nurse suspect?
(a) influenza
(b) pertussis
(c) meningitis
(d) scabies
Answer:
(c) meningitis
Rationale: The symptoms are characteristic of meningococcal meningitis, which is commonly contracted in crowded living spaces such as college dorms. Influenza is characterized by upper-respiratory symptoms; scabies is a dermal infection; and pertussis is a respiratory illness.
Objective: Communicable Diseases
Subobjective: Childhood Diseases
Question 78.
A patient comes to the ED with complaints of nausea and vomiting for 3 days. His ECG reading is shown in the exhibit. The nurse should suspect

(a) hyperkalemia.
(b) hypokalemia.
(c) hypercalcemia.
(d) hypocalcemia.
Answer:
(b) hypokalemia.
Rationale: The patient has had nausea and vomiting, which can cause hypokalemia. A U wave can be noted on an ECG or cardiac monitor. Hyperkalemia would show peaked T waves. Hypercalcemia may produce a shortened QT interval, and hypocalcemia may show QT prolongation.
Objective: Medical Emergencies
Subobjective: Electrolyte/Fluid Imbalance
Question 79.
An ED nurse is caring for a patient who was injured during a violent crime. Which of the following is a priority in evidence collection and care?
(a) chain of custody
(b) chain of evidence
(c) photographing of evidence
(d) documenting of evidence
Answer:
(a) chain of custody
Rationale: Chain of custody is the concept of limiting the number of people handling and collecting evidence after a crime is committed. Nurses caring for patients and handling evidence should use local official documents to demonstrate the chain of custody for ' evidence and to document when it is given to authorities.
Objective: Professional Issues
Subobjective: Patient (Forensic Evidence Collection)
Question 80.
A patient is brought to the ED following a motor vehicle crash. He was driving without a seat belt and was hit with the steering wheel on the left side of his chest. He complains of severe chest pain and dyspnea. During assessment, the nurse is unable to hear breath sounds on the left. The nurse should prepare to assist with immediate
(a) endotracheal intubation.
(b) chest compressions.
(c) chest tube insertion.
(d) thoracotomy.
Answer:
(c) chest tube insertion.
Rationale: The patient has a pneumothorax and will need a chest tube. Chest compressions are indicated only for cardiac arrest. Thoracotomy is done when there is severe trauma and impending or present cardiac arrest and is the final effort made to sustain life; it is associated with a low rate of successful outcomes. Endotracheal intubation is not indicated if the patient is able to protect his own airway, as is evidenced by his ability to communicate verbally.
Objective: Respiratory Emergencies
Subobjective: Pneumothorax
Question 81.
Epistaxis occurring from Kiesselbach's plexus is controlled by all methods EXCEPT
(a) cauterization of a visualized vessel.
(b) high Fowler's position leaning forward and applying continuous pressure to the midline septum.
(c) nasal packing with hemostatic material.
(d) endoscopic litigation.
Answer:
(d) endoscopic litigation.
Rationale: Endoscopic litigation is indicated for posterior epistaxis stemming from the ethmoid or sphenopalatine arteries. Kiesselbach's plexus is the most common site of anterior epistaxis that responds to conventional treatments.
Objective: Maxillofacial
Subobjective: Epistaxis
Question 82.
Which of the following interventions is NOT appropriate for a patient with adrenal hypofunction?
(a) peripheral blood draws
(b) low-sodium diet
(c) blood glucose monitoring
(d) hydrocortisone therapy
Answer:
(b) low-sodium diet
Rationale: The patient with adrenal hypofunction should not be on a sodium-restrictive diet, as it may lead to an adrenal crisis. Peripheral blood draws, glucose monitoring and hydrocortisone therapy are all appropriate for adrenal insufficiency.
Objective: Medical Emergencies
Subobjective: Endocrine Conditions
Question 83.
A patient is brought to the ED with dyspnea, headache, light-headedness, and diaphoresis.
A diagnosis of hyperventilation syndrome is made. The nurse is aware that hyperventilation syndrome can present with signs and symptoms similar to which of the following?
(a) pneumonia
(b) bronchitis
(c) pulmonary embolism
(d) pneumothorax
Answer:
(c) pulmonary embolism
Rationale: Patients with hyperventilation syndrome will present with similar signs and symptoms as pulmonary emboli. Patients with a pneumothorax will present with absent breath sounds on the side of the injury, anxiety, and pain on inspiration. Pneumonia is characterized by fever, malaise, and crackles at the base of the lungs.
Objective: Respiratory Emergencies
Subobjective: Pulmonary Embolus
Question 84.
Which test should a nurse expect before a health care provider prescribes risperidone to manage psychotic symptoms?
(a) a cardiac workup
(b) comprehensive metabolic panel (CMP)
(c) creatinine clearance
(d) complete blood count (CBC)
Answer:
(a) a cardiac workup
Rationale: Antipsychotics are used to treat psychotic symptoms such as hallucinations, paranoia, and delusions. They carry an increased risk of mortality, primarily from cardiovascular complications. A cardiac workup identifies any risk factors that would be a contraindication to antipsychotics. A comprehensive metabolic panel (CMP), creatinine clearance, and a CBC do not address the underlying risk of cardiovascular complications.
Objective: Psychosocial Emergencies
Subobjective: Psychosis
Question 85.
The nurse is caring for a patient who says he wants to commit suicide. He has a detailed, concrete plan. The nurse places the patient on suicide precautions, which include a 24-hour sitter. The patient becomes angry and refuses the sitter. Which action is the most appropriate?
(a) place the patient in soft wrist restraints
(b) have security sit outside the patient's door
(c) assign a sitter despite the patient's refusal
(d) allow the patient to leave against medical advice (AMA)
Answer:
(c) assign a sitter despite the patient's refusal
Rationale: The nurse should assign a sitter because the patient's safety is more important than his right to refuse care. Placing the patient in restraints does not guarantee his safety and may escalate the situation. If the patient manages to get out of the restraints, he might hang himself with them. Having security sit outside the door does not provide direct observation of the patient and uses up a limited resource of the facility. Allowing the patient to leave against medical advice (AMA) leaves the nurse and the facility vulnerable to legal action if he commits suicide after leaving.
Objective: Psychosocial Emergencies
Subobjective: Suicidal Ideation
Question 86.
Which laboratory finding indicates that a 62-year-old male patient is at risk for ventricular dysrhythmia?
(a) magnesium 0.8 mEq/L
(b) potassium 4.2 mmol/L
(c) creatinine 1.3 mg/dL
(d) total calcium 2.8 mmol/L
Answer:
(a) magnesium 0.8 mEq/L
Rationale: Abnormalities in magnesium levels may put the patient at risk for ventricular dysrhythmia. A hypomagnesemia level of 0.8 mEq/L would be of concern (normal range is 1.5 - 2.5 mEq/L). The other values are within normal ranges.
Objective: Cardiovascular Emergencies
Subobjective: Dysrhythmias
Question 87.
A patient presents to the ED with chest pain, dyspnea, and diaphoresis. The nurse finds a narrow complex tachycardia with a HR of 210 bpm, BP of 70/42 mm Hg, and a RR of 18. The nurse should anticipate which priority intervention?
(a) administer adenosine 6 mg IV
(b) defibrillate at 200 J
(c) administer amiodarone 300 mg IV
(d) prepare for synchronized cardioversion
Answer:
(d) prepare for synchronized cardioversion
Rationale: The patient is experiencing an unstable supraventricular tachycardia (SVT) with BP of 70/42 mm Hg and requires immediate synchronized cardioversion. Defibrillation is not indicated because the patient is awake and has an organized heart rhythm. Adenosine can be used in patients with stable SVT; however, this patient is not stable. Amiodarone is not indicated for unstable patients in SVT.
Objective: Cardiovascular Emergencies
Subobjective: Dysrhythmias
Question 88.
A patient is brought to the ED in supraventricular tachycardia (SVT) with a rate of 220. EMS has administered 6 mg of adenosine, but the patient remains in SVT. What is the next intervention the nurse should anticipate?
(a) administer 12 mg adenosine IV
(b) administer 1 mg epinephrine IV
(c) administer 300 mg amiodarone IV
(d) administer 0.5 atropine IV
Answer:
(a) administer 12 mg adenosine IV
Rationale: The drug of choice for supraventricular tachycardia (SVT) is adenosine. The first dose of 6 mg has already been given, so the next appropriate dose would be 12 mg. The other options are not the next appropriate intervention for a patient in SVT.
Objective: Cardiovascular Emergencies
Subobjective: Dysrhythmias
Question 89.
A 6-year-old child is admitted to the ED with an acute asthma attack. A pulse oximetry is attached with a reading of 91 %. The nursing priority is to
(a) administer dexamethasone.
(b) provide supplemental oxygen.
(c) prepare for immediate endotracheal intubation.
(d) administer a nebulized albuterol treatment.
Answer:
(b) provide supplemental oxygen.
Rationale: The goal for pulse oximetry readings is 94% - 99%. The nurse should apply supplemental oxygen for an SpO2 below 94%. Albuterol and dexamethasone are appropriate for asthma but are not the priority intervention. Endotracheal intubation is needed only if a patient is unable to maintain their airway.
Objective: Respiratory Emergencies
Subobjective: Asthma
Question 90.
A patient is admitted to the ED with a sickle cell crisis. The nurse should prepare to administer which of the following blood products?
(a) warm packed RBCs
(b) whole blood
(c) fresh frozen plasma (FFP)
(d) cryoprecipitate
Answer:
(a) warm packed RBCs
Rationale: The patient experiencing a sickle cell crisis needs fluid resuscitation with crystalloid solutions and the administration of warmed RBCs. Whole blood contains additional components such as plasma or platelets, which are not needed. Fresh frozen plasma and cryoprecipitate are not indicated for sickle cell crisis.
Objective: Medical Emergencies
Subobjective: Blood Dyscrasias
Question 91.
Which complication of compartment syndrome would the nurse suspect if urinalysis reveals myoglobinuria?
(a) disseminated intravascular coagulation (DIC)
(b) rhabdomyolysis
(c) Volkmann's contracture
(d) sepsis
Answer:
(b) rhabdomyolysis
Rationale: Rhabdomyolysis is characterized by the breakdown of skeletal muscle with the release of myoglobin and other intercellular proteins and electrolytes into the circulation. The presence of myoglobin produces heme¬positive results in the urinalysis.
Objective: Orthopedic
Subobjective: Trauma
Question 92.
A patient presents to the ED with complaints of substernal sharp, tearing knifelike chest pain radiating to the neck, jaw, and face. Morphine sulfate is given with no relief of the pain. These signs and symptoms are most indicative of which of the following?
(a) myocardial infarction (Ml)
(b) pericarditis
(c) pneumonia
(d) acute aortic dissection
Answer:
(d) acute aortic dissection
Rationale: The sharp, tearing knifelike substernal chest pain with no relief from morphine is a hallmark sign of an aortic dissection. Pneumonia presents with pain related to coughing. Pain from a myocardial infarction (Ml) or pericarditis would likely be relieved with doses of morphine sulfate.
Objective: Cardiovascular Emergencies
Subobjective: Aneurysm/Dissection
Question 93.
A patient is admitted to the ED with a potassium level of 6.9. Which of the following medications could have caused her electrolyte imbalance?
(a) bumetanide
(b) captopril
(c) furosemide
(d) digoxin
Answer:
(b) captopril
Rationale: Captopril is an ACE inhibitor, which can cause hyperkalemia. Bumetanide and furosemide are diuretics, which would cause hypokalemia. Digoxin is an antidysrhythmic and can also cause hypokalemia.
Objective: Medical Emergencies
Subobjective: Electrolyte/Fluid Imbalance
Question 94.
A patient presents to the ED with a bleeding laceration to the arm and a history of idiopathic thrombocytopenic purpura (ITP). The nurse should anticipate which treatment to be ordered?
(a) cryoprecipitate
(b) fresh frozen plasma (FFP)
(c) platelets
(d) protamine sulfate
Answer:
(c) platelets
Rationale: Patients with idiopathic thrombocytopenic purpura (ITP) have decreased platelet production, so platelets are the expected treatment. The other options are not indicated for this condition.
Objective: Medical Emergencies
Subobjective: Blood Dyscrasias
Question 95.
Which of the following is usually associated with variant (Prinzmetal's) angina?
(a) cyanide poisoning
(b) gastroesophageal reflux
(c) Raynaud's phenomena
(d) beta-blocker toxicity
Answer:
(c) Raynaud's phenomena
Rationale: Vasospastic disorders such as Raynaud's phenomena and migraine headaches are associated with variant (Prinzmetal's) angina.
Objective: Cardiac Emergencies
Subobjective: Chronic Stable Angina Pectoris
Question 96.
Hyperglycemic hyperosmolar state (HHS) is most often caused by
(a) infection.
(b) dehydration.
(c) noncompliance with insulin therapy.
(d) a breakdown of ketones.
Answer:
(b) dehydration.
Rationale: Infection is the most common cause of HHS. Dehydration may lead to HHS but is more often a symptom. Noncompliance with insulin therapy is not the most common cause of HHS. Breakdown of ketones is characteristic of DKA.
Objective: Medical Emergencies
Subobjective: Endocrine Conditions
Question 97.
Fluoxetine for moderate depression is contraindicated in patients with
(a) arthritis.
(b) migraines.
(c) glaucoma.
(d) appendicitis.
Answer:
(c) glaucoma.
Rationale: Fluoxetine is given cautiously to patients with glaucoma, due to the anticholinergic side effects. There are no current indications that this medication causes side effects with arthritis, migraines, or appendicitis.
Objective: Psychosocial Emergencies
Subobjective: Depression
Question 98.
A patient presents to the ED with severe throbbing fingers after coming home from the gym. Upon observing thin, shiny skin, pallor, and thick fingernails, the nurse should suspect
(a) acute arterial injury.
(b) acute arterial occlusion.
(c) peripheral venous thrombosis.
(d) peripheral vascular disease.
Answer:
(d) peripheral vascular disease.
Rationale: Throbbing fingers or toes after exercise accompanied with thin, shiny skin and thick fingernails are symptoms of peripheral vascular disease. Acute occlusion would present with pain and cyanosis distal to the occlusion. Venous thrombosis occurs more often in the lower extremities, and there is no information suggesting arterial injury.
Objective: Cardiovascular Emergencies
Subobjective: Peripheral Vascular Disease
Question 99.
Which of the following IV solutions should be administered to a patient with diabetic ketoacidosis (DKA) who is placed on an insulin drip?
(a) 1 lactated Ringer's
(b) normal saline
(c) normal saline with potassium
(d) normal saline with dextrose
Answer:
(c) normal saline with potassium
Rationale: Insulin administration shifts potassium into the cells causing hypokalemia, so fluids with potassium are indicated for this patient. The other fluids are not indicated for this patient.
Objective: Medical Emergencies
Subobjective: Endocrine Conditions
Question 100.
EMS brings in a patient with a history of alcohol abuse, homelessness, and poor adherence to antiseizure medications. The patient has experienced 3 seizures in 30 minutes. These findings support the diagnosis of
(a) atonic seizure.
(b) tonic-clonic seizure.
(c) status epilepticus.
(d) simple partial seizure.
Answer:
(c) status epilepticus.
Rationale: Status epilepticus occurs when a person experiences a seizure that lasts more than 5 minutes or has repeated episodes over 30 minutes. This is a medical emergency, as death can result if seizures last more than 10 minutes. Causes of status epilepticus include alcohol or drug withdrawal, suddenly stopping antiseizure medications, head trauma, and infection. Atonic seizures occur when the patient has a sudden loss of muscle tone for a few seconds, followed by postictal confusion. Tonic-clonic (grand mal) seizures last for only a few minutes. With a simple partial seizure, the patient remains conscious during the episode, which may be preceded by auras. Autonomic changes may occur, such as heart rate changes and epigastric discomfort.
Objective: Neurological Emergencies
Subobjective: Seizure Disorders
Question 101.
When taking the history of a patient with suspected pancreatitis, the nurse should expect to find
(a) the patient feels better when lying supine.
(b) the patient has a history of alcohol abuse and peptic ulcer disease.
(c) the pain is described as a sharp, burning sensation.
(d) the pain began gradually and radiated to the right lower abdomen.
Answer:
(b) the patient has a history of alcohol abuse and peptic ulcer disease.
Rationale: Risk factors for pancreatitis include alcohol abuse, peptic ulcer disease, renal failure, vascular disorders, hyperlipidemia, and hyperparathyroidism. Patients often find relief in the fetal position, while the supine position worsens pain. The pain is severe and sudden and feels intense and boring, as if it is going through the body. Pain occurs in the mid-epigastric area or left upper quadrant. Pain can radiate to the left flank, the left shoulder, or the back.
Objective: Gastrointestinal Emergencies
Subobjective: Pancreatitis
Question 102.
A pediatric patient is being resuscitated in a trauma bay, and his father wants to be in the room. What should the nurse do?
(a) Tell the father he may not be in the trauma room during resuscitation.
(b) Allow the father in the trauma room with a knowledgeable staff member for support.
(c) Ask the father to stand just outside the trauma room.
(d) Call the legal department for advice.
Answer:
(b) Allow the father in the trauma room with a knowledgeable staff member for support.
Rationale: Family member at the bedside for resuscitation has been demonstrated in the evidence as a preference for patients and families and should be offered when possible and appropriate. Family members should be present only if they are not disruptive to patient care.
Question 103.
A patient arrives to the ED after an attempted suicide by a self-inflicted gunshot wound. He is determined to be brain dead, but his life can be sustained for organ procurement. The patient is identified as an organ donor. Which of the following is the next step for the ED nurse?
(a) notify local organ procurement organization
(b) remove all life-supporting interventions
(c) perform postmortem care on the patient
(d) complete the death certificate
Answer:
(a) notify local organ procurement organization
Rationale: When an organ donor patient dies in the ED the nurse should first contact the organ procurement organization because of time sensitivity. Life-supporting interventions such as ventilators and medications should be continued until the organ procurement agency arrives. Postmortem care and completing the death certificate can be performed after organ procurement has taken place.
Objective: Professional Issues
Subobjective: Patient (End-of-Life Issues)
Question 104.
When caring for a patient with thyroid storm, the nurse should first prepare to administer which medication?
(a) propylthiouracil (PTU)
(b) epinephrine
(c) levothyroxine
(d) atropine
Answer:
(a) propylthiouracil (PTU)
Rationale: Propylthiouracil (PTU) is the drug of choice in treating thyroid storm, as it inhibits the synthesis of thyroxine. Epinephrine and atropine are contraindicated for thyroid storm, as these patients already have a dangerously high heart rate. Levothyroxine would be indicated for myxedema coma.
Objective: Medical Emergencies
Subobjective: Endocrine Conditions
Question 105.
A patient arrive to the ED with a sheriff's escort after being found in a street acting erratically and shouting. She is unkempt and not appropriately dressed for the weather. She states that she wants to commit suicide. What can the ED nurse expect to happen to the patient?
(a) She will be given benzodiazepines for anxiety and discharged.
(b) She will be medically cleared and brought to jail.
(c) She will be involuntarily committed.
(d) She will be voluntarily admitted to the hospital.
Answer:
(c) She will be involuntarily committed.
Rationale: The patient will be involuntarily committed because she is a threat to her own safety. She has not committed a crime. She will not be admitted voluntarily because she did not come to the hospital of her own volition.
Objective: Professional Issues
Subobjective: Patient (Transitions of Care)
Question 106.
A patient with a blood glucose reading of 475 mg/dL presents to the ED with Kussmaul respirations, nausea, and vomiting, and a pH of 7.3. The nurse should expect to treat which condition?
(a) myxedema coma
(b) hyperosmolar hyperglycemic state (HHS)
(c) pheochromocytoma
(d) diabetic ketoacidosis (DKA)
Answer:
(d) diabetic ketoacidosis (DKA)
Rationale: The patient is in acidosis and has Kussmaul respirations, which are indicative of diabetic ketoacidosis (DKA). Myxedema coma and pheochromocytoma would not cause these symptoms. Hyperosmolar hyperglycemic state (HHS) normally causes higher blood sugar levels and does not present in acidosis.
Objective: Medical Emergencies
Subobjective: Endocrine Conditions
Question 107.
The nurse is using the Glasgow Coma Scale (GCS) to assess a patient who fell in a parking lot. The patient opens his eyes to sound, localizes pain, and makes incoherent sounds when spoken to. Which GCS score will the nurse document?
(a) 9
(b) 10
(c) 11
(d) 12
Answer:
(b) 10
Rationale: The Glasgow Coma Scale (GCS) is calculated as follows: opening eyes to sound (3), localizing pain (5), and making incoherent sounds (2) gives a GCS score of 10.
Objective: Neurological Emergencies
Subobjective: Trauma
Question 108.
A patient arrives to the ED with a complaint of sore throat and fever. Which of the following findings is the most immediate concern?
(a) visualized white abscess on the soft palate
(b) patchy tonsillar exudate
(c) petechiae on the hard palate
(d) lymphedema
Answer:
(a) visualized white abscess on the soft palate
Rationale: The patient is showing signs of peritonsillar abscess. Peritonsillar abscess is an emergent condition that occurs from the accumulation of purulent exudate between the tonsillar capsule and the pharyngeal constrictor muscle. Patchy tonsillar exudate, petechiae, and lymphedema are common findings with viral and bacterial strep throat infections.
Objective: Maxillofacial
Subobjective: Peritonsillar Abscess
Question 109.
A patient in the ED is diagnosed with ulcerative colitis (UC). Which dietary changes can the nurse recommend to help manage symptoms?
(a) Eat a high-fiber diet.
(b) Limit coffee to two cups daily.
(c) Avoid lactose-containing foods.
(d) Consume dried fruit several times a week.
Answer:
(c) Avoid lactose-containing foods.
Rationale: Foods high in lactose may be poorly tolerated by patients with ulcerative colitis (UC) and should be limited or avoided. High-fiber foods can aggravate Gl symptoms in some patients and should be avoided. Caffeine is a stimulant that can increase cramping and diarrhea. Dried fruit stimulates the GI tract and can exacerbate symptoms.
Objective: Gastrointestinal Emergencies
Subobjective: Inflammatory Bowel Disease
Question 110.
A 32-year-old female patient comes to the ED with complaints of abdominal pain. She describes the pain as sharp and states it began suddenly during intercourse. The pain is worse with movement, and there is no vaginal discharge noted. These findings support the diagnosis of
(a) ectopic pregnancy.
(b) ruptured appendix.
(c) ruptured ovarian cyst.
(d) STD.
Answer:
(c) ruptured ovarian cyst.
Rationale: A sudden sharp pain in the pelvic region associated with sexual intercourse and no vaginal discharge is common with an ovarian cyst rupture. An ectopic pregnancy does not typically present with sudden pain, and there is usually vaginal bleeding. A ruptured appendix will cause constant pain to the RLQ and commonly causes a fever. The symptoms are not indicative of an STD.
Objective: Gynecological
Subobjective: Ovarian Cyst
Question 111.
Which of the following signs or symptoms should lead a nurse to suspect septic shock?
(a) WBC of 2,500
(b) serum lactate level of 2.6
(c) decrease in neutrophils
(d) increase in RBCs
Answer:
(b) serum lactate level of 2.6
Rationale: An elevation in serum lactate level will conclude the diagnosis of sepsis. The WBC count and neutrophil count would be increased. RBCs do not give adequate information to suspect sepsis.
Objective: Medical Emergencies
Subobjective: Sepsis and Septic Shock
Question 112.
A patient is admitted to the ED with nausea, vomiting, and diarrhea for 3 days and signs of severe dehydration. The nurse starts an IV and prepares to administer which fluid replacement?
(a) hypertonic solution
(b) isotonic crystalloid
(c) hypotonic solution
(d) colloid solution
Answer:
(b) isotonic crystalloid
Rationale: Dehydration requires an isotonic crystalloid solution, such as normal saline or lactated Ringer's, which will evenly distribute between the intravascular space and cells. Hypertonic solutions pull water from cells into the intravascular space, and hypotonic solutions move fluid from the intravascular space into the cells. Colloid solutions, such as albumin, draw fluid into intravascular compartments and would not be appropriate for this patient.
Objective: Medical Emergencies
Subobjective: Electrolyte/Fluid Imbalance
Question 113.
The nurse is reviewing the history of a patient with heart failure. Which of the following coexisting health problems will cause an increase in the patient's afterload?
(a) diabetes
(b) endocrine disorders
(c) hypertension
(d) Marfan syndrome
Answer:
(c) hypertension
Rationale: A history of hypertension will cause an increase in afterload. Diabetes will cause complications with microvascular disease, leading to poor cardiac function. Endocrine disorders will cause an increase in cardiac workload. Marfan syndrome causes the cardiac muscle to stretch and weaken.
Objective: Cardiac Emergencies
Subobjective: Heart Failure
Question 114.
The nurse is caring for a patient who presented to the ED with a subarachnoid hemorrhage. While taking the patient's history, what symptoms would the nurse expect to see with this patient?
(a) sudden food cravings
(b) rash on the lower trunk
(c) Battle's sign
(d) a severe, sudden headache
Answer:
(d) a severe, sudden headache
Rationale: Patients with subarachnoid hemorrhage commonly describe having the "worst headache of my life." Nausea and vomiting, not food cravings, may occur. There is no rash associated with subarachnoid hemorrhage. Battle's sign is a characteristic symptom of basilar skull fracture.
Objective: Neurological Emergencies
Subobjective: Trauma
Question 115.
The nurse is discharging a patient who has been prescribed medications to control progressive MS. Which statement by the patient indicates a need for further teaching by the nurse?
(a) "I will wear an eye patch on alternating eyes if I have double vision."
(b) "I will clear rugs and extra furniture from my Walking paths at home."
(c) "I hope I feel like going to Disney World this summer with my grandchildren."
(d) "I will call my doctor if I have any signs or symptoms of infection, such as fever."
Answer:
(c) "I hope I feel like going to Disney World this summer with my grandchildren."
Rationale: Several of the medications used to treat MS are immunosuppressants; therefore, the patient is more susceptible to infection while taking them. Patients should avoid crowds and anyone who appears to have an infection, such as the flu. Alternating an eye patch from one eye to the other every few hours can relieve diplopia. Patients with MS have alterations in mobility, and clearing walking paths in the home makes it safer to ambulate, especially with a walker or cane. If the patient suspects infection, he or she should notify the health care provider immediately.
Objective: Neurological Emergencies
Subobjective: Chronic Neurological Disorders
Question 116.
Lower abdominal pain that is worsened with movement, a non-malodorous vaginal discharge, a fever, and tachycardia are usually associated with
(a) appendicitis.
(b) pelvic inflammatory disease.
(c) ectopic pregnancy.
(d) STI.
Answer:
(b) pelvic inflammatory disease.
Rationale:
The signs and symptoms of panic inflammatory disease are lower abdominal pain that worsens with movement, a temperature greater than 101.30F (38.5°C), tachycardia, and non-malodorous vaginal discharge. Appendicitis does not cause vaginal discharge. Ectopic pregnancy * typically causes vaginal bleeding. Most STIs present with malodorous discharge and do not cause fever and tachycardia.
Objective: Gynecological
Subobjective: Infection
Question 117.
Which prescription would the nurse anticipate administering to a patient with no known medication allergies who presents with orofacial edema, halitosis, and a complaint of tasting pus in the mouth?
(a) nystatin
(b) sodium fluoride drops
(c) penicillin V potassium
(d) saliva substitute
Answer:
(c) penicillin V potassium
Rationale: Penicillin V potassium for antibiotic therapy is indicated for the treatment of dental abscesses, a condition indicated by this patient's symptoms. Sodium fluoride drops are a supplement for children, nystatin is used to treat oral Candida albicans infections, and saliva substitute is a rinse for dry mouth.
Objective: Maxillofacial
Subobjective: Dental Conditions
Question 118.
A patient with a myocardial infarction (Ml). The patient has received nitroglycerin sublingual and is still experiencing chest pain. The nurse should prepare to administer
(a) hydromorphone.
(b) meperidine.
(c) morphine sulfate.
(d) acetaminophen.
Answer:
(c) morphine sulfate.
Rationale: Morphine sulfate is the analgesic of choice in acute coronary syndrome (ACS): it provides analgesic and sedation and also decreases preload and afterload. Morphine is administered to relieve pain as well as to decrease pain-related anxiety that can further exacerbate the symptoms of the myocardial infarction (Ml). Meperidine is not indicated for use in Ml. Hydromorphone is more appropriate for patients with no cardiac compromise, and acetaminophen is not indicated in Ml.
Objective: Cardiovascular Emergencies
Subobjective: Acute Coronary Syndrome
Question 119.
A patient presents to the ED with complaints of dizziness and fatigue and a past medical history of HIV. She states she is noncompliant with her antiviral medications. Her temperature is 101.2°F (38.4°C), BP 100/72 mm Hg, HR 130 bpm, RR 22, and 02 96%.
Which of the following orders would be the priority intervention?
(a) administering an antibiotic
(b) administering acetaminophen
(c) administering prescribed antivirals
(d) administering 2 units of packed RBCs
Answer:
(a) administering an antibiotic
Rationale: HIV patients with a fever are considered emergent, and a septic workup is expected. After drawing blood cultures, antibiotics should be the priority intervention. Acetaminophen may be administered but is not the priority. Taking the patient's antivirals after she has been non-compliant is not a priority.
She does not need a blood transfusion.
Objective: Medical Emergencies
Subobjective: Immunocompromised
Question 120.
The nurse is caring for a patient who suffered a head injury following a fall off a ladder. The nurse assesses the patient for signs of increased intracranial pressure (ICP). Which finding by the nurse is a LATE sign of increased ICP?
(a) headache
(b) restlessness
(c) dilated pupils
(d) decreasing LOC
Answer:
(c) dilated pupils
Rationale: Late signs of increased intracranial pressure (ICP) include dilated or pinpoint pupils that are sluggish or nonreactive to light. Headache, restlessness, and decreasing LOC are early signs of increased ICP.
Objective: Neurological Emergencies
Subobjective: Increased Intracranial Pressure (ICP)
Question 121.
An 11-month-old infant is brought to the ED with a barking cough, a respiratory rate of 66, substernal retractions, and copious nasal secretions. Which of the following positions will best facilitate the child's breathing?
(a) sitting upright in a parent's lap
(b) on a stretcher in a prone position
(c) reverse Trendelenburg
(d) semi-Fowler's
Answer:
(a) sitting upright in a parent's lap
Rationale: The child should remain with the parent in an upright position. Taking the child from the parent could cause anxiety and crying and worsen the respiratory distress.
Objective: Respiratory Emergencies
Subobjective: Infections
Question 122.
Which of the following statements would be included in the discharge teaching for a patient with ulcerative colitis (UC)?
(a) "Hemorrhage is a potential complication."
(b) "Patients may have 5-6 loose stools perday."
(c) "Patients with UC are more likely to have fistulas."
(d) "Many times, surgery is needed to treat symptoms."
Answer:
(a) "Hemorrhage is a potential complication."
Rationale: Complications of ulcerative colitis (UC) include hemorrhage and nutritional deficiencies. Patients may have up to 10 - 20 bloody, liquid stools per day. Loose, non-bloody stools and fistulas are more common in patients with Crohn's disease. Surgery is rarely required for these symptoms.
Objective: Gastrointestinal Emergencies
Question 123.
Which pain characteristics are associated with inflammation of the fifth cranial nerve?
(a) progressive onset, bilateral, throbbing
(b) abrupt onset, unilateral, hemifacial spasm
(c) intermittent, circumoral, shooting
(d) paroxysmal, bilateral, paresthesia
Answer:
(b) abrupt onset, unilateral, hemifacial spasm
Rationale: Trigeminal neuralgia pain has an abrupt onset, is unilateral along the branch of the fifth cranial nerve, and causes hemifacial spasms.
Objective: Maxillofacial
Subobjective: Facial Nerve Disorders
Question 124.
Two weeks post-left-sided myocardial infarction (Ml) a patient presents to the ED with dyspnea and cough with hemoptysis. The nurse should suspect the patient has developed
(a) pneumonia.
(b) over-coagulation.
(c) pulmonary edema.
(d) ruptured ventricle.
Answer:
(c) pulmonary edema.
Rationale: The patient is experiencing symptoms of pulmonary edema, a complication of left-sided heart failure. Coagulation is not a secondary effect of myocardial infarction (Ml). Pneumonia is not generally related to post-MI concerns. A ruptured ventricle would present symptoms closer to the time of injury.
Objective: Cardiovascular Emergencies
Subobjective: Heart Failure and Cardiogenic Pulmonary Edema
Question 125.
A patient arrives to the ED with altered mental status, blood pressure of 70/40, and declining vital signs. Her husband states that she does not wish to be resuscitated. What should the EC) nurse do?
(a) Tell the patient that the physician will decide her advance directive status.
(b) Ask the spouse for the advanced directive paperwork.
(c) Document the patient's advanced directive wishes and honor the request in case resuscitation is needed.
(d) Inform the patient that advanced directives are not used in EDs.
Answer:
(b) Ask the spouse for the advanced directive paperwork.
Rationale: Advance directives must be valid, up to date, and documented before they can be honored in the ED. The nurse can document the patient's wishes, but it is not official until the paperwork is present. The physician does not make that decision, and with the correct documentation, EDs will honor advance directives.
Objective: Professional Issues
Subobjective: Patient (End-of-Life Issues)
Question 126.
A family in the ED must decide whether to withdraw care for a family member with no advance directive. Which person would NOT be consulted as a part of a multidisciplinary team to make this decision?
(a) chair of ethics committee
(b) legal department
(c) critical care physician
(d) pharmacist
Answer:
(d) pharmacist
Rationale: A pharmacist would not be consulted in this situation. Other members of the team may include ED physicians, social workers, and hospital religious team members.
Objective: Professional Issues
Subobjective: Patient (End-of-Life Issues)
Question 127.
A 2-year-old child presents to the ED with septal deviation and a visualized foreign body in the right naris. Which nursing intervention is most appropriate?
(a) instructing the parent to perform nasal positive pressure
(b) instructing the child to blow his nose
(c) instructing the parent to perform oral positive pressure
(d) restraining the child for forceps retraction
Answer:
(c) instructing the parent to perform oral positive pressure
Rationale: Instruct the parent to perform oral positive pressure by sealing his or her mouth securely over the child's mouth and providing a short, sharp puff of air while simultaneously occluding the unaffected nostril.
Objective: Maxillofacial
Subobjective: Foreign Bodies
Question 128.
Which treatment is contraindicated for a corneal abrasion?
(a) application of ophthalmic lubricating solution
(b) application of topical anesthetics
(c) patching the affected eye
(d) wearing glasses instead of contact lenses
Answer:
(c) patching the affected eye
Rationale: Patching the affected eye decreases oxygen delivery to the cornea, delays wound healing, and creates an environment that increases the risk for infection.
Objective: Ocular
Subobjective: Abrasions
Question 129.
The ED nurse is caring for a patient with delirium who tells crawling up on my bed." How should the nurse respond?
(a) "That's just the wrinkles in your blanket."
(b) "I will see if I can move you to another room."
(c) "I will call maintenance to come and remove them."
(d) "I know you're scared, but I don't see any snakes on."
Answer:
(d) "I know you're scared, but I don't see any snakes on."
Rationale: When a patient is experiencing hallucinations, the nurse should acknowledge the patient's fear but reinforce reality. Telling the patient that it is the wrinkles in the blanket dismisses the patient's fear and does not reorient the patient. Offering to move the patient to another room accepts the snakes as real and does not help the patient with reality. Offering to call maintenance reinforces the patient's belief that the snakes are real.
Objective: Psychosocial Emergencies
Subobjective: Psychosis
Question 130.
The nurse is caring for a patient who has been prescribed disease. Which medication on the patient's current record the'fiealth care provider?
(a) baclofen
(b) amantadine
(c) benztropine
(d) isocarboxazid
Answer:
(d) isocarboxazid
Rationale: Isocarboxazid and other MAOI inhibitors should not be taken with rasagiline mesylate due to the risk of increased blood pressure and hypertensive crisis. The other medications are not contraindicated for this patient: baclofen relieves muscle spasms, benztropine is an older drug that treats severe motor symptoms such as rigidity and tremors, and amantadine is an antiviral drug often prescribed with carbidopa and levodopa to reduce dyskinesias.
Objective: Neurological Emergencies
Subobjective: Chronic Neurological Disorders
Question 131.
Which medication would the nurse anticipate administering to a patient with a periorbital vesicular rash along the trigeminal nerve?
(a) acyclovir
(b) erythromycin
(c) ketorolac
(d) ciprofloxacin
Answer:
(a) acyclovir
Rationale: Herpes zoster infection of the facial nerves commonly involves the eyelid and surrounding structures. Treatment is palliative, using antiviral medications such as acyclovir.
Objective: Ocular
Subjective: Infections
Question 132.
The nurse is caring for a patient who presents to the ED with the following arterial blood gas (ABG) results:
pH 7.32
PaCO2 47 mm Hg
HCO3 24 mEq/L
PaO2 91 mm Hg
The nurse should expect the patient to present with
(a) chest pain.
(b) nausea and vomiting.
(c) deep, rapid respirations.
(d) hypoventilation with hypoxia.
Answer:
(d) hypoventilation with hypoxia.
Rationale: These ABGs indicate acute respiratory acidosis. Common signs of respiratory acidosis include hypoventilation with hypoxia, disorientation, and dizziness. Untreated respiratory acidosis can progress to ventricular fibrillation, hypotension, seizures, and coma. Deep, rapid respirations and nausea and vomiting are signs of metabolic acidosis. Chest pain is not a symptom of respiratory acidosis.
Objective: Respiratory Emergencies
Subobjective: Chronic Obstructive Pulmonary Disorder
Question 133.
Management of acute iritis includes
(a) topical mydriatic ophthalmic drops and topical corticosteroids.
(b) copious irrigation.
(c) IV mannitol and acetazolamide.
(d) topical anesthetics and topical antibiotics.
Answer:
(a) topical mydriatic ophthalmic drops and topical corticosteroids.
Rationale: Iritis is treated with topical mydriatic ophthalmic drops to dilate the pupil, topical corticosteroids to reduce inflammation, and referral to ophthalmology within 24 hours.
Objective: Ocular
Subobjective: Infections
Question 134.
Discharge teaching for a patient diagnosed with ulcerative keratitis is effective if she states which of the following?
(a) "There is no need to follow up with an ophthalmologist."
(b) "I will stop the antibiotic drops tomorrow if the pain is better."
(c) "I will wear glasses and not contacts for at least two weeks."
(d) "I need to stay home from work until the infection clears because I am highly contagious."
Answer:
(c) "I will wear glasses and not contacts for at least two weeks."
Rationale: Patients with ulcerative keratitis MUST NOT use contact lenses until the infection has resolved and been cleared by an ophthalmologist. The patient should complete the full course of prescribed antibiotics. Not all ulcers are contagious, so she could safely return to work after 24 hours of antibiotic use.
Objective: Ocular
Subobjective: Ulcerations/Keratitis
Question 135.
The nurse is caring for a patient with a history of cirrhosis who arrived at the ED with a new onset of confusion. The patient's skin is jaundiced. Labs are as follows:
Ammonia 130 mcg/dL
ALT 98 U/L
Blood glucose 128
The nurse should prepare to administer
(a) lactulose.
(b) bisacodyl.
(c) mesalamine.
(d) insulin 2 units.
Answer:
(a) lactulose.
Rationale: The patient's ammonia level and ALT are elevated, which is expected with cirrhosis. Lactulose is given to lower ammonia levels in patients with cirrhosis. Bisacodyl is a laxative and is not indicated for this patient. Mesalamine is an anti-inflammatory given for ulcerative colitis. The patient's blood glucose is not elevated enough to require 2 units of insulin.
Objective: Gastrointestinal Emergencies
Subobjective: Cirrhosis
Question 136.
Which of the following is a clinical feature of an open globe rupture?
(a) cherry red macula
(b) rust ring
(c) pale optic disc
(d) afferent pupillary defect
Answer:
(d) afferent pupillary defect
Rationale: Clinical open globe rupture features include afferent pupillary defect, impaired visual acuity, gross deformity of the eye, and prolapsing uvea.
Objective: Ocular
Subobjective: Trauma
Question 137.
Dopamine (Intropin) is ordered for a patient with heart failure because the drug
(a) lowers the heart rate.
(b) opens blocked arteries.
(c) prevents plaque from building up.
(d) increases the amount of oxygen delivered to the heart.
Answer:
(d) increases the amount of oxygen delivered to the heart.
Rationale: Dopamine (Intropin) is a positive inotrope, which will increase cardiac contractility and cardiac output, decrease the myocardial workload, and improve myocardial oxygen delivery.
Objective: Cardiovascular Emergencies
Subobjective: Heart Failure
Question 138.
Which statement regarding tourniquet use to control hemorrhagic bleeding for a partial limb amputation is correct?
(a) A commercially available tourniquet that is at least 2 inches wide with a windlass, a ratcheting device to occlude arterial flow, is recommended.
(b) Tourniquet application is never recommended even when direct pressure does not control blood loss from an extremity.
(c) Tourniquets properly applied in the prehospital setting should always be removed upon arrival to the ED, regardless if there is adequate team support to manage bleeding.
(d) Time of tourniquet application should be noted clearly on the device and should not exceed 4-hour intervals before reassessment of bleeding.
Answer:
(a) A commercially available tourniquet that is at least 2 inches wide with a windlass, a ratcheting device to occlude arterial flow, is recommended.
Rationale: A commercially available tourniquet at least 2 inches wide with a windlass or ratcheting device is recommended for both prehospital and in-hospital use. The nurse should never remove a tourniquet without team support to control hemorrhagic bleeding. Assessment occur? in 2-hour intervals.
Objective: Orthopedic
Subobjective: Amputation
Question 139.
Which of the following will confirm the diagnosis of a pulmonary embolism?
(a) chest X-ray
(b) D-dimer
(c) fibrin split products
(d) CT angiography
Answer:
(d) CT angiography
Rationale: Only the CT angiography will confirm the diagnosis. D-dimer may be increased in the presence of pulmonary embolism (PE) but is not a stand-alone indicator for definitive diagnosis. A chest X-ray will rule out other disease processes but does not rule in a PE. Fibrin split products are measured in the presence of disseminated intravascular coagulation and are not relevant for the concern of PE.
Objective: Respiratory Emergencies
Subobjective: Pulmonary Embolism
Question 140.
The nurse is caring for a patient with a history of schizophrenia, alcohol abuse, bipolar disorder, and noncompliance with treatment and medications. The patient has also been arrested in the past for violent behavior. Which action by the nurse is the most important when caring for a potentially violent patient?
(a) treat the patient with courtesy and respect
(b) always maintain an open pathway to the door
(c) be sure the patient swallows his pills and does not "cheek" them
(d) ask permission from the patient before drawing blood or performing other invasive procedures
Answer:
(b) always maintain an open pathway to the door
Rationale: When caring for mentally unstable or possibly violent patients, staff safety is the primary concern. The nurse should avoid getting blocked into a corner between the patient and the door. If possible, the patient should be in a room near the nurses' station, and the nurse should notify someone before entering the room. Bringing another nurse or patient care technician can also maintain safety. All patients should be treated with courtesy and respect, especially someone who may be prone to paranoia. It may be necessary to observe the patient closely for "cheeking" pills instead of swallowing them. Some medications may be ordered in IV form to ensure that the patient receives the medication if he has surreptitiously avoided swallowing pills in the past. Always ask permission before touching or approaching the patient to avoid startling him. If the patient refuses medications or blood draws, do not argue. Chart the refusal in the medical record and notify the health care provider.
Objective: Psychosocial Emergencies
Subobjective: Aggressive/Violent Behavior
Question 141.
A 13-year-old female arrives to the ED complaining of chest pain. A physical exam reveals tenderness along the fourth, fifth, and sixth ribs. Which diagnosis does the nurse suspect?
(a) myocardial infarction
(b) Ludwig's angina
(c) pleurisy
(d) costochondritis
Answer:
(d) costochondritis
Rationale: Costochondritis occurs from localized inflammation of the joints attaching the ribs to the sternum and most commonly presents in females ages 12 to 14.
Objective: Orthopedic
Subobjective: Costochondritis
Question 142.
Which of the following describes the characteristics of a flail chest?
(a) The chest sinks in with inspiration and out with expiration.
(b) Only the right side of the chest has movement.
(c) Movement is noted on the left side of the chest only.
(d) There is no movement noted on either side of the chest.
Answer:
(a) The chest sinks in with inspiration and out with expiration.
Rationale: In a flail chest there is asymmetrical movement of the chest wall. Ribs are completely broken and cause abnormal movement of the chest wall. As the patient breathes in, the flail segment will sink in as the patient breathes out, the segment will bulge outward.
Objective: Respiratory Emergencies
Subobjective: Trauma
Question 143.
The ED nurse is providing discharge teaching to a patient newly diagnosed with migraines who has been given a prescription for sumatriptan. Which of the following statements indicates the patient understands the discharge teaching?
(a) "This medication is safe to take while pregnant."
(b) "I will report chest pain immediately to my physician."
(c) "I will take my blood pressure medicine before I take sumatriptan."
(d) "I will take this medication 15 minutes after I feel a migraine starting."
Answer:
(b) "I will report chest pain immediately to my physician."
Rationale: Chest pain can occur with the first dose of sumatriptan and should be reported immediately. Sumatriptan may not be safe for pregnant women, so the patient should be coached on using an effective birth control method while taking it. Most triptans are contraindicated with hypertension and would not be prescribed if the patient is taking antihypertensives due to the risk of coronary vasospasm. The medication should be taken as soon as the first symptoms of migraine appear.
Objective: Neurological Emergencies
Subobjective: Headache
Question 144.
A 4-year-old child was in a bicycle accident and presents with oral lacerations and complete dental avulsions to the 2 top front teeth. The best initial management by the health care provider is
(a) immediate replantation of the avulsed teeth.
(b) laceration repair.
(c) replantation of the avulsed tooth after soaking for 30 minutes in Hank's solution.
(d) dental consult.
Answer:
(b) laceration repair.
Rationale: Avulsed primary teeth are not replanted because of the potential for subsequent damage to the developing permanent tooth and the increased frequency of pulpal necrosis. Best initial management would be to repair the lacerations.
Objective: Maxillofacial
Subobjective: Dental Conditions
Question 145.
Diagnostic findings common with gouty arthritis include
(a) hyperammonemia.
(b) hyperbilirubinemia.
(c) hyperuricemia.
(d) hyperhomocysteinemia.
Answer:
(c) hyperuricemia.
Rationale: Gouty arthritis characteristically occurs in patients with hyperuricemia, which causes high levels of uric acid in the blood from breakdown of purines. Hyperammonemia is the presence of an excess of ammonia in the blood. Hyperbilirubinemia is too much bilirubin in the blood. Hyperhomocysteinemia is a marker for the development of heart disease.
Objective: Orthopedic
Subobjective: Inflammatory Conditions
Question 146.
Which dressing would be most appropriate for a patient with a partial thickness wound to the epidermis?
(a) transparent dressing
(b) occlusive dressing
(c) nonstick adherent dressing
(d) bulky dressing
Answer:
(c) nonstick adherent dressing
Rationale: Nonstick adherent dressing such as a Band-Aid or Telfa pad is the appropriate choice.
Objective: Wound
Subobjective: Abrasions
Question 147.
A patient arrives to the ED from a house fire. The nurse notes soot at the opening of her mouth and both nares. What is the primary concern for this patient?
(a) total body surface areas covered in burns
(b) airway edema related to inhalation injury
(c) foreign body ingestion during the fire
(d) trauma as a result of rescue from the fire
Answer:
(b) airway edema related to inhalation injury
Rationale: There should be a high index of suspicion that the patient experienced an inhalation injury, and measures should be taken to protect her airway. Burns and trauma are secondary concerns to airway compromise. Soot at the mouth opening suggests smoke inhalation, not foreign body ingestion.
Objective: Respiratory Emergencies
Subobjective: Inhalation Injuries
Question 148.
Which intervention is contraindicated for a patient with acute angle glaucoma?
(a) administration of ophthalmic beta blocker
(b) maintaining patient in a supine position
(c) dimming lights in the room or providing a blindfold for comfort
(d) administration of IV mannitol
Answer:
(c) dimming lights in the room or providing a blindfold for comfort
Rationale: Dimming lights or providing a blindfold are contraindicated, as low lighting will increase pupillary size, creating an increase in intraocular pressure. Pupil size should remain constricted through use of bright lighting and miotic ophthalmic drops.
Objective: Ocular
Subobjective: Glaucoma
Question 149.
Which of the following chest X-ray readings is consistent with acute respiratory distress syndrome (ARDS)?
(a) bilateral, diffuse white infiltrates without cardiomegaly
(b) bilateral, diffuse infiltrates with cardiomegaly
(c) tapering vascular shadows with hyper lucency and right ventricular enlargement
(d) prominent hilar vascular shadows with left ventricular enlargement
Answer:
(a) bilateral, diffuse white infiltrates without cardiomegaly
Rationale: The typical chest radiography for a patient with adult respiratory distress syndrome (ARDS) is bilateral, diffuse white infiltrates without cardiomegaly. Options C and D show results for abnormal heart tissue but not for lung tissue and do not give any information about infiltrates.
Objective: Respiratory Emergencies
Siibobjective: Respiratory Distress Syndrome
Question 150.
Which positive toxicology result would the nurse suspect in a patient with a MRSA-positive infectious abscess of the right antecubital space?
(a) alcohol
(b) opioid
(c) benzodiazepine
(d) tetrahydrocannabinol (THC)
Answer:
(b) opioid
Rationale: Many opioid substances are commonly injected, resulting in ' abscess formation from use of non-sterile equipment and aseptic technique. Cocaine, amphetamines, and other substances may also be injected. Alcohol, benzodiazepine, and tetrahydrocannabinol use may be co¬occurring in the patient, but these substances are not commonly injected.
Objective: Wound
Subobjective: Infections
Question 151.
A patient arrives to the ED after taking a sedative and subsequently becoming confused and disoriented. His temperature is 96.2°F (35.6°C), pulse is 47 bpm with distant heart tones, and BP is 82/65 mm Hg. He states that he is currently receiving thyroid replacement therapy. The nurse should suspect
(a) allergic reaction to the sedative.
(b) thyroid storm.
(c) myxedema coma.
(d) acute stroke.
Answer:
(c) myxedema coma.
Rationale: The patient is hypotensive, hypothermic, and bradycardic. He has ingested thyroid replacement medications and sedatives, which can lead to a myxedema coma. The symptoms are not indicative of an allergic reaction or an acute stroke. A thyroid storm would show increased heart rate, temperature, and blood pressure.
Objective: Medical Emergencies
Subobjective: Endocrine Conditions
Question 152.
The health care provider orders xylocaine with epinephrine to be prepared for a patient with a
(a) 2 cm laceration to the penile shaft.
(b) 2 cm laceration above the right eyebrow.
(c) 3 cm laceration to the left index finger.
(d) 7 cm laceration to the left forearm.
Answer:
(d) 7 cm laceration to the left forearm.
Rationale: Epinephrine is never used for lacerations of the fingers, toes, face, or penis.
Objective: Wound
Subjective: Lacerations
Question 153.
Which is the most appropriate post-exposure rabies prophylaxis treatment for an animal bite in a patient not previously vaccinated?
(a) rabies vaccine on days 0, 3, 7, and 14
(b) human rabies immune globulin injected into the wound bed
(c) human rabies immune globulin injected into the wound bed and rabies vaccine on days 0, 3, 7, and 14
(d) tetanus 0.5 mL via intramuscular injection
Answer:
(c) human rabies immune globulin injected into the wound bed and rabies vaccine on days 0, 3, 7, and 14
Rationale: Post-exposure prophylaxis in a patient who has not been vaccinated must consist of both immunoglobin and vaccine therapy. While up-to-date tetanus immunization should be considered, it is a targeted vaccine against infection by Clostridium tetani.
Objective: Environmental
Subobjective: Vector-Borne Illnesses
Question 154.
A child is admitted to the ED with wheezing on exhalation, use of accessory muscles, using 1 -word sentences, and tripod positioning. The nurse should suspect
(a) pneumonia.
(b) pneumonitis.
(c) foreign body aspiration.
(d) asthma.
Answer:
(d) asthma.
Rationale: The child is presenting with signs of asthma exacerbation. Symptoms of foreign body aspiration are consistent with acute airway obstruction to include respiratory distress and drooling. Pneumonitis would present with chest pain and dyspnea but not these acute symptoms. Pneumonia is characterized with crackles in the lower lobes and decreased oxygen saturation.
Objective: Respiratory Emergencies
Subobjective: Asthma
Question 155.
Which of the following medications should a nurse anticipate administering to a patient experiencing"; a severe anaphylactic reaction to a bee sting?
(a) epinephrine 1:1000 0.3 - 0.5 ml
(b) diphenhydramine 25 - 50 mg
(c) Solu-Medrol 125 mg
(d) theophylline 6mg/kg
Answer:
(a) epinephrine 1:1000 0.3 - 0.5 ml
Rationale: The patient will need epinephrine administered immediately. Most anaphylactic deaths occur due to a delay in epinephrine administration. Diphenhydramine and Solu-Medrol are indicated for minor allergic reactions. Theophylline is typically used to treat asthma and is not indicated for anaphylaxis.
Objective: Medical Emergencies
Subobjective: Allergic Reactions and Anaphylaxis
Question 156.
The best medical management for carbon monoxide toxicity is
(a) hydroxocobalamin
(b) hyperbaric oxygen
(c) N-acetylcysteine
(d) sodium bicarbonate
Answer:
(b) hyperbaric oxygen
Rationale: Hyperbaric oxygen is used to treat severe carbon monoxide toxicity. Hydroxocobalamin is a cyanide-binding agent. N-acetylcysteine restores depleted hepatic glutathione, reversing effects of acetaminophen toxicity. Sodium bicarbonate is standard treatment for salicylate toxicity.
Objective: Environmental
Subobjective: Chemical Exposure
Question 157.
A patient presents to the ED with complaints of severe headache, irritability, confusion, and lethargy. During triage, he mentions that he has spent the last several days in his shop with a wood-burning stove. The ED nurse should be concerned for which of the following?
(a) migraine headache
(b) stroke
(c) carbon monoxide poisoning
(d) allergic reaction
Answer:
(c) carbon monoxide poisoning
Rationale: Patients presenting with vague neurological symptoms may be difficult to diagnose. The history and information leading up to presentation in the department is vital in determining differential diagnoses. This patient is not presenting with stroke-like symptoms.
The symptoms are similar to those of a migraine; however, the history makes carbon monoxide poisoning more likely. The patient is not demonstrating stroke or allergic reaction symptoms.
Objective: Toxicology
Subobjective: Carbon Monoxide
Question 158.
The nurse is reviewing the laboratory results of a patient with renal failure and notes a serum potassium level of 7.2. The nurse should prepare to administer which of the following medications to protect cardiac status?
(a) aspirin
(b) insulin
(c) calcium gluconate
(d) digoxin
Answer:
(c) calcium gluconate
Rationale: Calcium gluconate is administered to the patient with hyperkalemia for cardiac and neuromuscular protection. Aspirin is used for acute coronary syndrome but would not be a first-line drug for this condition. Insulin and dextrose may be given to lower potassium levels but do not function to protect cardiac status. Digoxin is an antidysrhythmic and is not indicated for hyperkalemia.
Objective: Medical Emergencies
Subobjective: Renal Failure
Question 159.
A college student arrived at the ED with suspected meningitis, and a positive diagnosis was confirmed via lumbar puncture. Which of the following findings suggests that she may have developed hydrocephalus?
(a) sluggish pupillary response
(b) inability to wrinkle the forehead
(c) inability to move the eyes laterally
(d) inability to move the eyes downward
Answer:
(c) inability to move the eyes laterally
Rationale: Monitoring neurological status is the most important nursing intervention for patients with meningitis. Deficits of cranial nerve VI prevent lateral eye movement, which is an indicator of hydrocephalus.
Other indicators of hydrocephalus include urinary incontinence and signs of increased intracranial pressure (ICP). Declining LOC is the first sign of increased ICP, and the nurse must be sensitive to even small changes in LOC. The other findings do not indicate increasing ICP.
Objective: Neurological Emergencies
Subobjective: Increased Intracranial Pressure (ICP)
Question 160.
Appropriate discharge teaching for a patient with diverticular disease includes instructions to
(a) avoid foods high in sodium.
(b) consume clear liquids until pain subsides.
(c) limit alcohol to one glass per day.
(d) include strawberries to get enough vitamin C.
Answer:
(b) consume clear liquids until pain subsides.
Rationale: Patients with diverticular disease should remain on clear liquids until pain has subsided. For maintenance, they will need to eat 25 to 35 grams of fiber daily to provide bulk to the stool. Patients should avoid high-sodium foods and alcohol, which irritates the bowel. Strawberries contain seeds that may block a diverticulum and should be avoided, along with nuts, corn, popcorn, and tomatoes.
Objective: Gastrointestinal Emergencies
Subobjective: Diverticulitis
Question 161.
Which neurological assessment finding commonly occurs in a patient struck by lightning?
(a) tic douloureux
(b) ascending paralysis
(c) Bell's palsy
(d) keraunoparalysis
Answer:
(d) keraunoparalysis
Rationale: Keraunoparalysis is a condition specific to lightning strikes, resulting from vasoconstriction in the tissues surrounding entry and exit points. Ascending paralysis is a common finding in Guillain-Barre syndrome. Bell's palsy and tic douloureux are both facial nerve disorders.
Objective: Environmental
Subobjective: Electrical Injuries
Question 162.
A patient presents to the ED with confusion, anxiety, irritability, and a slight tremor. During assessment, she states she drinks two or more bottles of wine per day. Which of the following questions is important to ask?
(a) Do you drink any other alcoholic drinks on a regular basis?
(b) When was your last drink?
(c) When was your first drink?
(d) Have you ever experienced alcohol withdrawal?
Answer:
(b) When was your last drink?
Rationale: The patient's last drink is important; to determine the possibility of withdrawal or delirium tremens. The other questions are relevant but are not the priority based on the patient's presentation.
Objective: Communicable Diseases
Subobjective: Withdrawal Syndrome
Question 163.
A 34-year-old patient attempted suicide by consuming his grandmother's oral antidiabetic agent. Administration of glucose has been unsuccessful in reversing the effect of the medication. Which antidote should the nurse expect to administer next?
(a) flumazenil
(b) acetylcysteine
(c) octreotide
(d) methylene blue
Answer:
(c) octreotide
Rationale: Octreotide is used for overdoses refractory to glucose administration. It stimulates the release of insulin from the beta islet cells of the pancreas. Flumazenil is the antidote for benzodiazepine overdose. Acetylcysteine is used for acetaminophen overdose, and methylene blue is used for nitrites and anesthetics overdose.
Objective: Communicable Diseases
Subobjective: Overdose and Ingestion.
Question 164.
A patient presents to triage with a complaint of cough lasting three weeks without improvement. The patient confirms recent travel to a developing country, and states she has had fevers and chills for the last three days. The nurse should suspect
(a) herpes zoster.
(b) tuberculosis.
(c) influenza.
(d) hepatitis C.
Answer:
(b) tuberculosis.
Rationale: Tuberculosis is characterized by a cough lasting 2-3 weeks or more, fever, chills, night sweats, and fatigue. The recent travel to a developing country is a concern for potential infectious disease. The other conditions have similar symptoms, but the travel and chronic cough indicate strong concern for pulmonary tuberculosis.
Objective: Communicable Diseases
Subobjective: Tuberculosis
Question 165.
A woman arrives to the ED with her 5-year-old child, whom she discovered eating her nifedipine. She does not know how many pills the child consumed. The nursing priority is to
(a) place a referral to child protective services.
(b) obtain a 12-lead ECG.
(c) place the child on oxygen.
(d) ask the child how many she took.
Answer:
(b) obtain a 12-lead ECG.
Rationale: Calcium channel blockers can cause symptoms in children with doses as low as 1 tablet. Rapid deterioration may occur if the tablets are short-acting. A 5-year-old may not accurately count or recollect the number of tablets consumed. A referral to child protective services should be made if there is a reasonable suspicion for the need but is not a priority intervention. Oxygen should be provided only if pulse oximetry is less than 92%.
Objective: Communicable Diseases
Sutjobjective: Overdose and Ingestion
Question 166.
A 10-year-old child presents to triage with conjunctivitis, cough, and a rash in the back of his mouth. During the assessment, the patient's father indicates that the child is not vaccinated. These findings most likely indicate
(a) varicella.
(b) mumps.
(c) measles.
(d) pertussis.
Answer:
(c) measles.
Rationale: The rash, conjunctivitis, and cough are indicative of measles, and the patient's vaccination status makes this diagnosis even more likely. Varicella is characterized by vesicular rash on the trunk and face; mumps, by nonspecific respiratory symptoms and edema in the parotid gland; and pertussis is a respiratory disease with a specific "whoop"-sounding cough.
Objective: Communicable Diseases
Subobjective: Childhood Diseases
Question 167.
Which of the following medications should the nurse expect to administer to a patient who chronically abuses alcohol?
(a) naloxone
(b) thiamine
(c) flumazenil
(d) vitamin K
Answer:
(b) thiamine
Rationale: People who chronically abuse alcohol are deficient in thiamine and are given IV thiamine. Naloxone blocks opioid receptors and is given for opioid overdose. Flumazenil is a benzodiazepine receptor antagonist and is given for benzodiazepine overdose. Vitamin K is given for warfarin overdose.
Objective: Communicable Diseases
Subobjective: Substance Abuse
Question 168.
A 35-year-old patient in the ED has been diagnosed with herpes zoster. Which of the following statements should the nurse include in her discharge teaching?
(a) Herpes zoster occurs any time after an initial varicella infection and may recur several times.
(b) The varicella vaccine is known to cause latent herpes zoster when administered to children.
(c) Herpes zoster outbreaks are caused by a latent virus, so it is not contagious.
(d) The zoster vaccine should not be given to patients who have had a herpes zoster outbreak.
Answer:
(a) Herpes zoster occurs any time after an initial varicella infection and may recur several times.
Rationale: Herpes zoster, also known as shingles, is caused by the reactivation of dormant varicella virus. It can occur several times over the lifetime of a patient who has had an initial varicella infection. The varicella vaccine is not known to cause herpes zoster. Herpes zoster can be spread by contact with the rash; someone who has never had varicella may contract it from contact with a herpes zoster rash. The zoster vaccine may prevent a second or third outbreak in patients who have had active herpes zoster.
Objective: Communicable Diseases
Subobjective: Herpes Zoster
Question 169.
A 7-year-old unvaccinated child arrives to the ED. The nurse suspects diphtheria, based on which of the following symptoms?
(a) thick gray membrane covering the tonsils and pharynx
(b) temperature of 104°F (40°C) or greater
(c) macular rash on the thorax and back, along the dermatomes
(d) cluster headache with nausea and symptoms of an aura
Answer:
(a) thick gray membrane covering the tonsils and pharynx
Rationale: A pseudomembrane, or thick gray membrane, covering the tonsils, the pharynx, and sometimes the larynx is characteristic of diphtheria infection. Patients with diphtheria may have a low-grade fever; they will not have a macular rash or headache.
Objective: Communicable Diseases
Subobjective: Childhood Diseases
Question 170.
Which of the following statements from a nurse demonstrates that his participation in a Critical Incident Stress Debriefing (CISD) session was effective?
(a) He agrees to meet with the manager regarding the incident.
(b) He agrees to attend future debriefing sessions as needed.
(c) He agrees to schedule an appointment for further counseling.
(d) He provides the incident details before departing the debrief.
Answer:
(c) He agrees to schedule an appointment for further counseling.
Rationale: The nurse demonstrates personal insight that further help is needed via the Critical Incident Stress Management (CISM) system. CISM does not require or recommend that nurses needing debriefing or assistance meet with managers specifically about the event or experience. The nurse should not depart the debriefing before it is complete, and future debrief sessions may or may not occur. Scheduling appointments is a concrete action that demonstrates the nurse's effective participation.
Objective: Professional Issues
Subobjective: Nurse (Critical Incident Stress Management)
Question 171.
The ED nurse's responsibility to practice quality nursing care is achieved through which of the following?
(a) reading research articles
(b) participating in Evidence-Based Practice (EBP) projects
(c) participating in research studies
(d) participating in grand rounds
Answer:
(b) participating in Evidence-Based Practice (EBP) projects
Rationale: Participation and engagement in Evidence-Based Practice (EBP) projects supports an environment of quality and safe care using up-to-date evidence and practices that have been thoroughly researched. Reading research articles is important, but the data must be synthesized through formal processes to implement evidence into practice.
Objective: Professional Issues
Subobjective: Nurse (Evidence-Based Practice)
Question 172.
Nurses managing patient transitions of care in the ED should consider all of the following characteristics EXCEPT
(a) accessibility of services.
(b) safety.
(c) community partnerships.
(d) patient income.
Answer:
(d) patient income.
Rationale: Patient income is not directly relevant to transitions of care and is not appropriate for ED nurses to ask about when managing care transitions. Safety, community partnerships, and accessibility of services are all appropriate considerations.
Objective: Professional Issues
Subobjective: Patient (Transitions of Care)
Question 173.
What is the appropriate ratio of compressions to ventilations for a full-term neonate who is apneic with a pulse rate of 50 bpm?
(a) 30:2
(b) 15:1
(c) 15:2
(d) 3:1
Answer:
(d) 3:1
Rationale: The current (2015) AHA and NRP guidelines for newborn resuscitation is 3 compressions to 1 ventilation. A ratio of 30:2 is appropriate for all adults or a single rescuer infant/child; a ratio of 15:2 is appropriate for 2 rescuers with children and infants. A ratio of 15:1 is not recommended for anyone.
Objective: Obstetrical
Subobjective: Ndonatal Resuscitation
Question 174.
Which of the following interventions is NOT necessary for a patient who has died in the ED and is not in a vegetative state?
(a) maintaining the head of the bed at 20 degrees
(b) instilling artificial tears in eyes to preserve tissue
(c) taping eyes closed with paper tape
(d) inserting Foley catheter to decompress the bladder
Answer:
(d) inserting Foley catheter to decompress the bladder
Rationale: A Foley catheter is not necessary to decompress the bladder in this patient. Typically, these patients are eligible for eye donation, and the head should be at 20 degrees, with artificial tears or saline in the eyes to preserve the tissue. Tape should be used if eyes do not close after death.
Objective: Professional Issues
Subobjective: Patient (End-of-Life Issues)
Question 175.
A 24-year-old male patient arrives at the ED with a complaint of a 1-month history of a rash that is annular, ^/ith raised margins and centralized clearing. Which of the following dermal infections does the nurse expect?
(a) scabies
(b) ringworm
(c) impetigo
(d) cellulitis
Answer:
(b) ringworm
Rationale: Annular lesions with raised borders and cleared central areas of the rash indicate ringworm. Scabies are characterized by red pruritic rashes, and cellulitis and impetigo do not present in this way.
Objective: Environmental
Subobjective: Parasite and Fungal Infestations