Practicing CEN Practice Questions can help you become familiar with the exam's pacing.
Cardiovascular Emergencies CEN Practice Questions - CEN Questions on Cardiovascular Emergencies.
Question 1.
The decrease in cardiac output from right ventricular infarction can be explained by:
(a) vasospasms of coronary arteries.
(b) inflammation and destruction of cardiac muscle.
(c) ventricular dilatation and decreased contractility.
(d) interstitial volume overload.
Answer:
(c) ventricular dilatation and decreased contractility.
Rationale:
Injury to the right ventricle causes right ventricular dilatation and decreased contractility.
The inability to pump venous blood forward into the pulmonary vasculature reduces blood flow to the left ventricle, which leads to a drop in cardiac output. Inflammation and destruction of cardiac muscle is seen in myocarditis. Prinzmetal’s angina (also known as variant angina) is the result of coronary artery vasospasms. Interstitial volume overload is characteristic of heart failure.
Question 2.
Which of the following is the most critical intervention during the first minutes of ventricular fibrillation?
(a) Advanced airway
(b) Epinephrine 0.1 mg IV/IO
(c) Immediate cardiac compressions
(d) Electrical defibrillation
Answer:
(c) Immediate cardiac compressions
Rationale:
CPR performed early can double or triple survival from witnessed sudden cardiac arrest. For every minute that passes between collapse and defibrillation, the chance of survival from a witnessed ventricular fibrillation declines by 7% to 10% per minute if no bystander cardiopulmonary resuscitation is provided.
A major emphasis of the 2015 American Heart Association (AHA) Guidelines Update for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiac Care (ECC) is high-quality chest compressions with minimal interruption and a decreased emphasis on early placement of an advanced airway; providers may defer insertion of an advanced airway until the patient fails to respond to initial CPR and defibrillation attempts or demonstrates return of spontaneous circulation (ROSC).
The optimal number of cycles of CPR and shocks required before starting pharmacologic therapy remains unknown; however, epinephrine should be given when IV/IO access is accomplished. Defibrillation should be performed as soon as it can be accomplished and immediate CPR should be performed while waiting to shock.
Question 3.
Which of the following is a reversible cause of pulseless electrical activity (PEA)?
(a) Hypoglycemia
(b) Hypotension
(c) Hypernatremia
(d) Hypoxia
Answer:
(d) Hypoxia
Rationale:
As less oxygen reaches the heart, the heart rate slows and contractility becomes less effective; placement of an advanced airway is theoretically more important during pulseless electrical activity (PEA) and might be necessary to achieve adequate oxygenation or ventilation. According to the American Heart Association, hypoglycemia, hypotension, and hypernatremia are not reversible causes of pulseless electrical activity.
Question 4.
Which of the following is an absolute contraindication for thrombolytic therapy in acute coronary syndrome?
(a) Seizure at onset with residual neurological impairments
(b) Gastrointestinal hemorrhage within previous 21 days
(c) History of previous intracranial hemorrhage
(d) Major serious trauma within previous 14 days
Answer:
(c) History of previous intracranial hemorrhage
Rationale:
History of previous intracranial hemorrhage is an absolute exclusion criterion for thrombolytic therapy. Seizure at onset with residual neurological impairments, gastrointestinal hemorrhage within previous 21 days, and major serious trauma within previous 14 days are relative exclusion criteria.
A provider with expertise in acute stroke care may elect to treat with thrombolytic therapy after weighing the risks and benefits.
Question 5.
Which of the following would the emergency nurse anticipate for a patient with an aortic dissection?
(a) Emergent surgery
(b) Chest tube insertion
(c) Immediate intubation
(d) Pericardial decompression
Answer:
(a) Emergent surgery
Rationale:
Definitive treatment of an acute aortic dissection consists of surgical repair of the rupture. Chest tube placement is indicated for pneumothoraces or hemothorax. The priority is to move the patient to definitive care; intubation can be accomplished in the operating room. Pericardial decompression is indicated for pericardial tamponade.
There are three major types of aneurysms. A fusiform aneurysm is caused by a weakening of the medial layer, the middle layer, of the artery. This type of aneurysm completely encircles the vessel. A saccular aneurysm, also caused by a weakening of the middle layer, is a dilatation of one area of the circumference of the involved artery. A dissecting aneurysm is caused by a tear in the intima or innermost layer of the vessel, which then creates a false lumen and starts ripping the layers apart as more and more blood fills this false lumen.
Question 6.
Nitroglycerin is a vasodilator that reduces myocardial oxygen demand by decreasing preload and improving coronary blood flow. Contraindications to nitrate administration in acute coronary syndromes include which of the following?
(a) ST-segment depression on electrocardiogram " (ECG)
(b) Dyspnea (respiratory rate greater than 20 breaths/ minute)
(c) Hypotension (systolic blood pressure less than 90 mm Hg)
(d) Tachycardia (heart rate greater than 100 beats/minute)
Answer:
(c) Hypotension (systolic blood pressure less than 90 mm Hg)
Rationale:
Nitroglycerin reduces myocardial oxygen demand by decreasing preload and improving coronary blood flow; therefore, it is contraindicated in patients with inadequate preload, represented by hypotension. It effectively reduces ischemic chest discomfort in coronary syndromes which may include symptoms of ST depression, dyspnea, and tachycardia.
One side effect of nitroglycerin that does not occur very often is reflex tachycardia. This happens because of the vasodilation, thus causing a sympathetic response of tachycardia. The “hose” is too large for the amount of blood that it is holding, so the body identifies it as a shock state and attempts to compensate for the event. Rates in this situation can be as high as 140 to 160 and is short-lived.
Question 7.
A patient is complaining of chest pain, light-headedness, shortness of breath, and sweating. The emergency nurse should suspect which of the following conditions?
(a) Pericarditis
(b) Myocardial ischemia
(c) Heart failure
(d) Endocarditis
Answer:
(b) Myocardial ischemia
Rationale:
Symptoms suggestive of ischemia include chest pain, pressure, discomfort spreading to shoulders, neck, one or both arms, or into the jaw, between the shoulder blades, light-headedness, dizziness, fainting, sweating, nausea or vomiting, and shortness of breath. Patients with pericarditis may present with fever, chest pain that is relieved by sitting forward, pleuritic chest pain, and can have a pericardial friction rub.
Heart failure symptoms include crackles with auscultation, blood-tinged sputum, dyspnea, and extremity swelling. Signs and symptoms of endocarditis would include fever, pleuritic pain, hemoptysis, and arthralgia/myalgias.
Question 8.
A patient arrives with a gunshot wound to the left chest. The patient is alert, complaining of pain, and has difficulty breathing. Objective data includes hypotension, muffled heart sounds, jugular vein distension (JVD), tachycardia, tachypnea, and an open wound to the left chest. Oxygen via a non-rebreather and two large-bore intravenous catheters have been placed.
Vital signs on arrival were as follows:
Blood pressure—80/50 mm Hg
Pulse—125 beats/minute
Respirations—32 breaths/minute
Pulse oximetry—80% on room air
Temperature—98.6° F (37.0° C)
Which of the following should the emergency nurse anticipate to prepare for next?
(a) Assist with a resuscitative thoracotomy.
(b) Prepare for massive blood transfusion.
(c) Assist with a pericardiocentesis.
(d) Prepare for aggressive ventilatory support.
Answer:
(c) Assist with a pericardiocentesis.
Rationale:
Beck’s triad, which consists of hypotension, muffled heart sounds, and jugular venous distension, along with tachycardia, dyspnea, cyanosis, and a history of penetrating trauma are signs of a pericardial tamponade, a collection of blood in the pericardial sac. As blood accumulates in the noncompliant pericardial sac, it exerts pressure on the heart, inhibiting ventricular filling and, therefore, cardiac output.
A pericardiocentesis will aspirate the, blood out of the sac and relieve the pressure on the heart. A resuscitative thoracotomy is indicated with a traumatic cardiac arrest. Massive blood transfusion is not indicated at this point. Ventilatory support may be necessary when the patient goes in for surgical repair, but the first priority is relieving pressure on the heart to improve cardiac output.
When assisting with a pericardiocentesis, the emergency nurse should watch the monitor/ECG for ST elevation and premature ventricular contractions (PVCs) caused by the needle being inserted beyond the pericardial sac into the ventricle. Once the needle is retracted into the sac, these manifestations will go away.
Question 9.
Which of the following is an indication for an emergency resuscitative thoracotomy?
(a) Patients sustaining penetrating abdominal injuries
(b) Blunt trauma with no signs of life
(c) Penetrating thoracic wound with recent loss of vital signs
(d) Qualified trauma surgeon is not available.
Answer:
(c) Penetrating thoracic wound with recent loss of vital signs
Rationale:
Penetrating thoracic wounds with recent loss of vital signs is an indication for an emergency tho-racotomy in order to determine the site of injury and stop persistent hemorrhage. Penetrating abdominal injuries and blunt trauma with no signs of life are not indications for an emergency thoracotomy.
A qualified surgeon who is available as backup is an indication for emergency thoracotomy to take the patient to the operating room for definitive repair.
Question 10.
Which of the following is NOT a classic manifestation of the triad of symptoms that accompanies a right ventricular infarction?
(a) Hypotension
(b) Jugular venous distension
(c) Tachycardia
(d) Clear lungs
Answer:
(c) Tachycardia
Rationale:
Patients with a right ventricular infarction usually have bradycardic rhythms. This malady is associated with inferior myocardial infarctions, which involve the right coronary artery. This artery supplies the inferior myocardial wall as well as the SA and AV nodes. Classic manifestations of a right ventricular infarction, which accompanies an inferior MI at least 30% to 40% of the time, are hypotension, jugular venous dis-tension (JVD), and clear lungs.
Patients experiencing a right ventricular infarction have a decreased preload. Small boluses of fluid will help in this situation. Avoid the use of nitrates, morphine sulfate, or diuretics which would decrease preload even more.
Question 11.
A patient with a history of Marfan’s syndrome presents with the following symptoms: tearing retrosternal back pain, hypertension, right- and left-arm blood pressure variation of 20 mm Hg, and decreased level of consciousness. The emergency nurse should consider which of the following conditions as the primary process?
(a) Pericardial tamponade
(b) Thoracic trauma
(c) Aortic dissection
(d) Ruptured diaphragm
Answer:
(c) Aortic dissection
Rationale:
Past medical history of Marfan’s syndrome, tearing retrosternal back pain, hypertension, right- and left-arm blood pressure variation of 20 mm Hg, and decreased level of consciousness are classic symptoms of acute aortic dissection. Marfan’s syndrome is a genetic connective tissue disorder that predisposes the patient to aortic dissection due to weakening of the aorta.
Pericardial tamponade would present with jugular venous distension, dyspnea, and tachycardia in addition to chest pain. Thoracic trauma is not specific. Ruptured diaphragm would present with chest pain radiating to the left shoulder, abdominal pain, and decreased breath sounds on the affected side.
Question 12.
Which of the following changes on the electrocardiogram would the emergency nurse recognize as being indicative of an acute myocardial infarction?
(a) ST-segment depression
(b) Dynamic T-wave inversion
(c) Nondiagnostic changes in ST segment
(d) ST-segment elevation
Answer:
(d) ST-segment elevation
Rationale:
ST-segment elevation is strongly suspicious for myocardial injury for ST-elevation myocardial infarction (STEMI). ST-segment depression and dynamic T-wave inversion are suspicious or ischemia. Nondiagnostic changes in ST segment or T wave are low/intermediate risk for acute coronary syndrome.
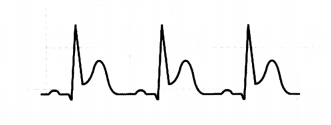
Question 13.
Treatment for the above mentioned rhythm in a symptomatic adult would include which of the following interventions?
(a) Cardioversion at 50 to 100 joules
(b) Beta-blocker or calcium channel blocker
(c) Atropine 0.5 mg bolus given intravenously
(d) Intravenous nitroglycerin, titrate to effect
Answer:
(c) Atropine 0.5 mg bolus given intravenously
Rationale:
Atropine 0.5 mg bolus given intravenously is a first-line treatment for symptomatic bradycardia.
(The clue in this question is the fact that it is symptomatic!) Cardioversion at 50 to 100 joules is recommended for conversion of atrial flutter and supraventricular tachycardia. Beta-blockers and calcium channel blockers will slow the heart rate and are used for symptomatic narrow-complex tachyarrhythmias. Intravenous nitroglycerin is contraindicated in patients with marked bradycardia because nitroglycerin will lower the amount of venous return to the heart. This, in addition to the low heart rate, could compromise cardiac output.
Question 14.
A patient is complaining of chest pain unrelieved with rest. The electrocardiogram shows T-wave inversion and there is no elevation in troponin. The emergency nurse suspects which of the following disease entities?
(a) Stable angina
(b) Unstable angina
(c) Non-ST elevation myocardial infarction (Non-STEMI)
(d) ST-elevation myocardial infarction (STEMI)
Answer:
(b) Unstable angina
Rationale:
Unstable angina is characterized by the classic signs of continued chest pain despite rest or nitro-glycerin and no elevation of troponin. Stable anginal pain goes away with rest. Non-STEMI is defined as ST depression or T-wave inversion with elevation of cardiac biomarkers. STEMI (ST-elevation myocardial infarction) definition requires ST elevation in two or more contiguous leads or new left bundle branch block and troponin elevation beyond the 99th percentile of the upper reference limit.
When talking to patients regarding potential chief complaints of chest pain, always remember to make sure they understand that tightness and heaviness are “equal” to pain. Many will say "Not really” to the question "Are you having chest pain?” but are still rubbing or holding their chest. When the nurse says “But does it feel tight or heavy?” the answer is so often "Yes, that’s how it feels." They need to know that this is considered “pain” to us!
Question 15.
A patient arrives pulseless and apneic. The cardiac monitor shows asystole. Which of the following medications would the emergency nurse anticipate?
(a) Amiodarone (Cordarone)
(b) Epinephrine (Adrenaline)
(c) Atropine sulfate
(d) Dopamine (Intropin)
Answer:
(b) Epinephrine (Adrenaline)
Rationale:
Epinephrine 1 mg every 3 to 5 minutes is recommended for asystole in addition to beginning high-quality cardiopulmonary compressions and iden-tifying a reversible cause. Amiodarone is the first-line antiarrhythmic drug given in ventricular fibrillation or pulseless ventricular tachycardia. Atropine and then do-pamine are indicated for symptomatic bradycardia.
Question 16.
The emergency nurse realizes that the student nurse understands premature atrial contractions when the student makes which of the following statements?
(a) “Premature atrial complexes may precede supraventricular tachycardia, atrial flutter, or atrial fibrillation.”
(b) “Premature atrial complexes may occur in a saw-toothed pattern and are called flutter waves.”
(c) “Premature atrial complexes are characterized by a chaotic atrial rhythm and an irregular ventricular response. ”
(d) “Premature atrial complexes occur with accessory conduction system pathways that predispose to reentrant rhythms.”
Answer:
(a) “Premature atrial complexes may precede supraventricular tachycardia, atrial flutter, or atrial fibrillation.”
Rationale:
Premature atrial complexes may precede supraventricular tachycardia, atrial flutter, or atrial fibrillation. These complexes appear on the electrocardiogram as identical to the patient’s PQRST complexes but are “premature” or early in the pattern. Flutter waves occur in atrial flutter and appear as a sawtooth pattern which can be variable.
Atrial fibrillation is characterized by a chaotic atrial rhythm associated with an irregular ventricular response. Supraventricular tachycardia is common in the pediatric population, some of whom are born with accessory conduction system pathways that predispose them to reentrant rhythms.
Question 17.
Atrial fibrillation is clinically significant for which of the following reasons?
(a) Atrial fibrillation may initiate ventricular fibrillation when it is multifocal.
(b) There is a complete absence of conduction between the atria and the ventricles.
(c) This increases the risk of life-threatening ventricular dysrhythmias.
(d) The loss of atrial contraction causes stroke volume to decrease by 20% to 30%.
Answer:
(d) The loss of atrial contraction causes stroke volume to decrease by 20% to 30%.
Rationale:
The loss of normal atrial contraction and atrial “kick” causes stroke volume to decrease by 20% to 30%. The atria are unable to expel the normal amount of blood during an episode of atrial fibrillation. Atrial “kick” provides for an increase in blood volume in the left ventricle at the end of diastole. Without this extra “kick” at the end of the filling time, there is loss of volume and, therefore, decreased cardiac output.
Premature ventricular contractions (PVCs) may initiate ventricular fibrillation when they are multifocal and also increase the risk for life-threatening ventricular dysrhythmias or sudden cardiac death. Absence of conduction between the atria and the ventricles is called third-degree heart block.
Another major problem with atrial fibrillation is the development of thrombi in the atria and the potential for a major cerebrovascular accident (CVA) event. This occurs because the atria never completely empty and blood pools causing clotting and embolic release. Anticoagulation is a must for these patients.
Question 18.
Which of the following is the first intervention for new-onset third-degree atrioventricular block with serious signs and symptoms?
(a) Initiate a dopamine (Intropin) infusion 2 to 20 //g/minute.
(b) Application of a transcutaneous pacemaker
(c) Administer adenosine (Adenocard) 6 mg intravenously.
(d) Prepare for amiodarone (Cordarone) 300 mg intravenous.
Answer:
(b) Application of a transcutaneous pacemaker
Rationale:
New-onset third-degree atrioventricular block with manifestations (especially with a wide-QRS complex) is an indication for insertion of a transvenous pacemaker; transcutaneous pacing is a temporizing measure until the transvenous pacemaker is placed.
Dopamine or epinephrine infusions are also temporizing measures before insertion of a transvenous pacemaker, but application of a transcutaneous pacemaker should be done first. Adenosine is indicated, for stable narrow-complex supraventricular tachycardia. Amiodarone is indicated as second-line treatment for ventricular fibrillation or pulseless ventricular tachycardia after shock, CPR, and a vasopressor.
Question 19.
A pediatric patient is unstable, with poor perfusion, hypotension, and supraventricular tachycardia with a rate of 300 beats/minute. Immediate treatment would include which of the following?
(a) Administer adenosine intravenously using the port closest to the infusion site.
(b) Apply ice to the child’s face for 10 to 15 seconds.
(c) If the child is older, consider vagal maneuvers, such as coughing.
(d) Initiate synchronized cardioversion with 0.5 to 1 joules/kg.
Answer:
(d) Initiate synchronized cardioversion with 0.5 to 1 joules/kg.
Rationale:
Initiating synchronized cardioversion with 0.5 to 1 joules/kg is initial treatment for unstable infants or children with supraventricular tachycardia. The patient in this scenario is hypotensive and has evidence of poor perfusion. Adenosine, application of ice to the face, and other vagal maneuvers are attempted in children (and adults) who are hemodynamically stable.
Question 20.
Immediate post-cardiac arrest care in comatose patients after return of spontaneous circulation (ROSC) includes which of the following?
(a) Maintaining a ventilatory PETC02 between 55 and 60 mm Hg
(b) Maintaining a minimum systolic blood pressure of 80 mm Hg
(c) Maintaining a target temperature of 32° C to 36° C (89.6° F to 96.8° F)
(d) Maintaining arterial oxygen saturation of 90% or greater
Answer:
(c) Maintaining a target temperature of 32° C to 36° C (89.6° F to 96.8° F)
Rationale:
Maintaining a constant target temperature between 32° C and 36° C (89.6° F to 96.8° F) for 24 hours has been demonstrated to improve neurologic recovery. Ventilation should be titrated to a PETC02 of 35 to 45 mm Hg or a PaC02 of 40 to 45 mm Hg. Hypotension (blood pressure £ 90 mm Hg) should be treated with fluid bolus or vasopressor infusion. Oxygen delivery should be titrated to the lowest Fi02 required to achieve an arterial oxygen saturation of 94% to 99% to avoid potential oxygen toxicity.
Question 21.
Magnesium sulfate 1 to 2 g mixed in 50 mL of 0.9% sodium chloride and administered over 5 to 60 minutes intravenously is recommended in which of the following situations?
(a) Alternative to amiodarone with pulseless ventricular tachycardia or ventricular fibrillation
(b) Second-line drug of choice for treatment of symptomatic bradycardia
(c) First-line drug of choice for most forms of narrow-complex supraventricular tachycardia
(d) Only if torsade de pointes, digitalis toxicity, or suspected hypomagnesemia is present
Answer:
(d) Only if torsade de pointes, digitalis toxicity, or suspected hypomagnesemia is present
Rationale:
Administration of magnesium is recommended only if torsades de pointes, digitalis toxicity, or suspected hypomagnesemia is present. Hypomagnesemia can cause a prolonged Q-T interval and the magnesium will help shorten the Q-T interval to its normal.
In digitalis toxicity, the administration of magnesium for replacement may be vital to decrease dysrhythmias and can act indirectly as an antagonist of digoxin. Lidocaine 1 to 1.5 mg/kg is an alternative to amiodarone in cardiac arrest from pulseless ventricular tachycardia or ventricular fibrillation. Dopamine infusion is the second-line drug for symptomatic bradycardia after atropine. Adenosine 6 mg given rapidly over 1 to 3 seconds followed by a normal saline bolus of 20 mL is the first drug for narrow-complex supraventricular tachycardia.
Question 22.
Anginal equivalents, particularly in women, diabetics, and the elderly may include which of the following sets of symptoms?
(a) Shortness of breath, fatigue, palpitations, near-syncope, nausea, vomiting
(b) Chest burning, pressure, tightness, discomfort, distress
(c) Prior myocardial infarction, stent placement, pacemaker presence
(d) Altered level of consciousness, muffled heart sounds, jugular venous distension.
Answer:
(a) Shortness of breath, fatigue, palpitations, near-syncope, nausea, vomiting
Rationale:
In the three populations listed, chest pain can be absent or atypical. Shortness of breath, fatigue, palpitations, near-syncope, nausea, and vomiting are anginal equivalents and may be present in women, diabetics, and the elderly instead of the classic chest pain that is usually expected. Burning, pressure, tightness, discomfort, and distress are words patients use to describe chest pain of cardiac origin, and so is not a “set of symptoms.”
Prior myocardial infarction, stent placement, and pacemaker presence are risk factors for cardiovascular disease, not symptoms. Altered level of consciousness, muffled heart sounds, and jugular venous distension are signs of an aortic arch dissection.
Question 23.
A 65-year-old patient complains of nocturnal dyspnea, orthopnea, dyspnea on exertion, and ankle swelling. The emergency nurse knows these may be signs of a/an:
(a) impending myocardial infarction.
(b) episode of unstable angina.
(c) mild to moderate heart failure.
(d) spontaneous pneumothorax.
Answer:
(c) mild to moderate heart failure.
Rationale:
Nocturnal dyspnea, orthopnea, dyspnea on exertion, and ankle swelling are signs of mild-to-moderate heart failure. Severe heart failure occurs when patients are unable to perform their usual physical activity and have symptoms at rest. Increased physical activity causes increased symptomatology.
Although dyspnea on exertion may be present with myocardial infarction, unstable angina and pneumothorax, ankle swelling, nocturnal dyspnea, and orthopnea would not be expected in these disease processes.
Question 24.
A patient is brought to the emergency department by emergency medical services in asystole. Cardiopulmonary resuscitation (CPR) was performed en route. Which of the following are the recommended interventions for asystole?
(a) CPR and atropine
(b) Defibrillation and atropine
(c) CPR and epinephrine
(d) Defibrillation and epinephrine
Answer:
(c) CPR and epinephrine
Rationale:
CPR and epinephrine are recommended for asystole. Available evidence suggests that the routine use of atropine during pulseless electrical activity (PEA) or asystole is unlikely to have a therapeutic benefit and has been removed from the Adult Cardiac Arrest Algorithm.
Likewise, in all outcomes studied, including return of spontaneous circulation (ROSC) and survival, there was a worse outcome for shock delivery with asystole; there-fore, electrical delivery is not recommended for asystole.
Question 25.
A patient complains of a headache, drowsiness, confusion, and chest pain. Vital signs are as follows:
Blood pressure—220/130 mm Hg
Pulse—120 beats/minute
Respirations—22 breaths/minute
Pulse oximetry—95% on room air
Temperature—98.6° F (37° C)
The nurse suspects which of the following conditions?
(a) Pericarditis
(b) Acute arterial occlusion
(c) Hypertensive emergency
(d) Decompensated heart failure
Answer:
(d) Decompensated heart failure
Rationale:
Hypertensive emergency is defined as a systolic blood pressure over 180 mm Hg or a diastolic blood pressure over 120 mm Hg with evidence of impending end-organ damage, in this case cerebrovascular impairment.
Signs of pericarditis are cardiac in nature, along with a possible elevated body temperature and a friction rub. Acute arterial occlusion would result in pain, pallor, pulselessness, paresthesia, or paralysis of the affected limb. Decompensated heart failure may have hypertension present, but symptoms would also include possible jugular venous distension, dyspnea, peripheral edema, nausea, and crackles.
Remember that not all hypertension is dropped immediately! There are some disease processes in which the blood pressure must be decreased quickly, such as with an aneurysm or aortic dissection; however, in instances of cerebrovascular accident (CVA), the blood pressure is maintained at a higher level to perfuse the brain and not cause an increase in the size of the infarct. Cerebral perfusion pressure must be maintained at a level of at least 60 to 70 in the adult to perfuse the brain.
The formula is CPP = MAP - ICP. The mean arterial pressure (MAP) must keep up with the intracranial pressure (ICP) to maintain the cerebral perfusion pressure.
Question 26.
A 75-year-old patient arrives with symptoms of dizziness, near-syncope, shortness of breath, and chest pain. There is a history of an implantable electronic device. The nurse should prepare for immediate:
(a) stat 12-lead electrocardiogram.
(b) magnet applicatioh.
(c) interrogation of the pacemaker.
(d) cardiology consult.
Answer:
(a) stat 12-lead electrocardiogram.
Rationale:
All of the interventions may be required; however, an emergent 12-lead electrocardiogram (ECG) and rhythm strip to determine whether the implantable cardioverter defibrillator (ICD) is functioning correctly should be done initially.
The magnet inactivates the sensing function so that during magnet mode, the pacemaker will pace asynchronously. Magnet application may be done later to identify battery depletion or malfunction of the ICD. Interrogation of the ICD should be done by the emergency department, cardiology department, or the device manufacturer. A consult to cardiology would be needed also.
Question 27.
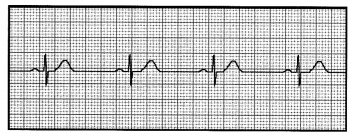
The emergency nurse recognizes the above rhythm as:
(a) first-degree heart block.
(b) second-degree heart block, Type I.
(c) second-degree heart block, Type II.
(d) third-degree heart block.
Answer:
(c) second-degree heart block, Type II.
Rationale:
Second-degree heart block, Type II is characterized by a constant PR interval that is followed by a nonconducted P wave. First-degree heart block is the most common conduction disturbance and is characterized by a PR interval that is greater than 0.20 seconds and rarely requires treatment.
Type I second-degree heart block (Mobitz 1 or Wenckebach) is slower and slower impulse conduction through the AV node and is seen as gradual prolongation of the PR interval until one depolarization from the atria is completely blocked. Third-degree heart block results from injury to the cardiac conduction system, so that no impulses are conducted from the atria to the ventricles; the atrial contractions are faster and independent of the slower beating ventricles.
Plan on identifying a few heart dysrhythmias on the test. They may be embedded within the question or simply asked such as in this question. Become proficient in identifying rhythms. It will be good for your test taking and important for your patients!
Question 28.
A patient complains of acute shortness of breath, frothy pink-tinged sputum, and chest pain. Crackles and wheezes are present. Past medical history includes diabetes,
hypertension, and heart failure. The emergency nurse suspects which of the following disease processes?
(a) Pericardial tamponade
(b) Pneumothorax
(c) Pulmonary embolus
(d) Pulmonary edema
Answer:
(d) Pulmonary edema
Rationale:
The symptoms presented are typical of acute pulmonary edema related to heart failure. Pericardial tamponade has muffled heart sounds, distended neck veins, and hypotension (Beck’s triad). Breath sounds would be decreased on the affected side in a pneumothorax. Pulmonary embolus causes nonspecific signs, but dyspnea, tachypnea, syncope, or cyanosis are most common.
Pulmonary edema is associated with left-sided heart failure. It causes a backup of fluid in the pulmonary system. Edema of the ankles and feet is associated with right-sided heart failure because it causes a backup of fluid in the venous system.
Think about how the flow of blood goes through the heart. That will help you remember the manifestations of right- and left-sided heart failure. Blood returns to the heart through the superior and inferior vena cava and empties into the right atrium. After entering the right ventricle, the deoxygenated blood flows into the pulmonary system through the pulmonary artery.
Once oxygen is picked up (and carbon dioxide is dropped off to be breathed off), blood reenters the heart via the pulmonary veins into the left atrium. It then is passed into the left ventricle and pumped out to the body through the aorta Therefore, right-sided heart failure is manifested by a back up of blood into the venous system and left-sided heart failure presents as pulmonary edema as it backs up fluid in the lungs. Usually, these symptoms occur simultaneously due to how interconnected the right and left sides of the heart function.
Question 29.
A patient arrives in the emergency department complaining of a low-grade fever, weight loss, night sweats, fatigue, and pleuritic-type chest pain. He has a past medical history of rheumatic heart disease, intravenous drug abuse, and has several body piercings and tattoos. The nurse notices Janeway lesions on the palms of both hands and clubbing. The emergency nurse suspects which of the following problems?
(a) Cardiac vessel disease
(b) Infective endocarditis
(c) Pericarditis
(d) Myocarditis
Answer:
(b) Infective endocarditis
Rationale:
Low-grade fever, weight loss, night sweats, fatigue, arthralgia, and pleuritic chest pain are signs and symptoms of infective endocarditis. Risk factors include a history of rheumatic heart disease, intrave-nous drug use, body piercings, and tattoos. Janeway lesions (small reddened macular like nodules found on the hands and feet) and clubbing are classic signs of infective endocarditis. Cardiac vessel disease is not spe-cific for these signs and symptoms.
Pericarditis presents with pleuritic chest pain that radiates to the left shoulder, causes increased pain in the supine position, and may be relieved by sitting up and leaning forward. Viral infection is the most common cause of myocarditis, including parvovirus, herpesvirus 6, and coxsackievirus B. Clinical myocarditis often is self-limiting unless the host immune response is overwhelming or inappropriate.
The potential for endocarditis which causes infection and destruction of the heart valves is the reason that those patients who are IV drug abusers are not considered good candidates for cardiac organ donation.
Question 30.
The emergency nurse anticipates which of the following interventions for a patient with cardiomegaly?
(a) B-type natriuretic peptide (BNP), chest radiograph, ECG, furosemide
(b) Metabolic panel, chest radiograph, ECG, nitroprusside
(c) Troponin, chest radiograph, ECG, metoprolol
(d) Coagulation profile, chest radiograph, ECG, anticoagulants
Answer:
(a) B-type natriuretic peptide (BNP), chest radiograph, ECG, furosemide
Rationale:
B-type natriuretic peptide (BNP), chest radiograph, ECG, and furosemide is the plan of care for a patient with cardiomegaly. Patients with cardiomegaly present with symptoms of heart failure, manifested by a reduction in left ventricular contractility and cardiac output.
Metabolic panel, chest radiograph, ECG, and nitroprusside are recommended for hypertensive crisis. Troponin, chest radiograph, ECG, and metoprolol are indicated in myocardial infarction. Coagulation profile, chest radiograph, ECG, and anticoagulants are treatment for venous thromboembolisms. ’
Question 31.
Which of the following would indicate successful use of thrombolytic therapy?
(a) T-wave inversion
(b) Decreased ST segment
(c) Prolonged QT intervals
(d) Pathologic Q waves
Answer:
(b) Decreased ST segment
Rationale:
Thrombolytic therapy should open closed coronary arteries and reperfuse the heart. Reperfusion would be indicated by ST segments falling back to normal levels. Elevated ST segments indicate injury to the heart muscle. T-wave inversion would demonstrate ischemia. Prolonged QT intervals are a negative finding and can be a forerunner of torsade de pointes. Pathologic Q waves are indicative of necrosis in the heart wall.
Question 32.
Objective assessment of an acute aortic dissection would include which of the following?
(a) Manual blood pressure taken in both arms
(b) Inspection for petechial rash to extremities
(c) Inspection for extremity edema, anasarca, and ascites
(d) Auscultation of heart sounds for prominent apical pulse / S3, S4
Answer:
(a) Manual blood pressure taken in both arms
Rationale:
Manual blood pressures taken in both arms would be the correct objective assessment parameter. The primary event in an aortic dissection is a tear in the aortic intima which allows blood to pass into the aortic media, thereby creating a false lumen; pressure within this false channel can compress the true aortic lumen and reduce blood flow.
A considerable variation greater than 20 mm Hg systolic may be seen when comparing the, blood pressure in the arms with this diagnosis. Inspection for petechiae related to microemboli is performed for a suspected acute arterial occlusion. Edema of the extremities, anasarca (generalized swelling), or ascites would be assessed for heart failure. Prominent apical pulse and the presence of S3 or S4, is found in hypertensive crises cases.
Question 33.
Complete the following statement with the appropriate phrase. Myocarditis is a/an:
(a) narrowing or occlusion of arteries caused by arteriosclerosis.
(b) inflammation and destruction of cardiac muscle.
(c) disease of the endocardium and heart valves.
(d) inflammation of the pericardium that is frequently idiopathic.
Answer:
(b) inflammation and destruction of cardiac muscle.
Rationale:
Myocarditis causes an inflammation and destruction of the actual cardiac muscle. Patients may present nearly asymptomatic, in severe heart failure, or with sudden death from dysrhythmias. Causes of myocarditis are numerous and include infectious, toxic, and immunologic. Arteriosclerosis can cause both peripheral vascular disease which contains the arteries outside of the heart and cardiac disease within the coronary arteries.
Endocarditis is an infection that generally affects normal heart valves and can be caused by many different bacteria, fungi, mycobacteria, and other organisms. Pericarditis, an inflammation of the pericardium, is most frequently idiopathic; however, it can develop as a result of bacterial, viral or fungal infections, autoimmune diseases, myocardial infarction, systemic lupus, and others.
Question 34.
A patient arrives in the emergency department with the following signs and symptoms: worsening dyspnea, tachypnea, cough, edema, fatigue, and distended neck veins. The emergency nurse suspects which of the following as a primary diagnosis?
(a) Pulmonary embolism
(b) Heart failure
(c) Cardiac tamponade
(d) Tension pneumothorax
Answer:
(b) Heart failure
Rationale:
Heart failure is the result of structural and functional impairment of ventricular filling or ejection of blood. Most patients have impairment of myocardial function, ranging from normal ventricular size and function to marked dilation and reduced function. Worsening dyspnea is a cardinal symptom of heart failure and dyspnea at rest is often mentioned by patients.
The symptoms stated in the question reflect pulmonary congestion. Pulmonary embolism occurs with an occlusion of pulmonary blood vessels and the patient may have dyspnea, but pleuritic chest pain, pleural friction rub, and signs and symptoms of a deep vein thrombosis would also be expected; edema would not occur with a pulmonary embolism.
Cardiac tamponade is the collection of blood in the pericardial sac, which limits ventricular filling and thus decreases cardiac output; signs and symptoms would include chest pain and Beck’s triad: distended neck veins (JVD), distant heart sounds (muffled), and hypotension.
Tension pneumothorax occurs when air enters the pleural space during inspiration and is unable to escape during exhalation. This leads to a rising intrathoracic pressure which compresses the lungs, heart, and great vessels in the chest. It is preceded by blunt or penetrating trauma and causes severe respiratory distress and absent breath sounds on the affected side.
Question 35.
Which of the following explanations is true regarding Raynaud’s disease?
(a) A narrowing or occlusion of the arteries outside the heart as a result of thickening of the intimal wall
(b) Severely reduced blood flow as a result of vasospasm of the digits in response to cold, stress, and/or smoking
(c) An inflammatory disorder that decreases blood flow first in the hands and feet that results in ischemia and pain
(d) A type of hardening caused by the accumulation of fats and cholesterol that creates plaque in the arteries
Answer:
(b) Severely reduced blood flow as a result of vasospasm of the digits in response to cold, stress, and/or smoking
Rationale:
Raynaud’s disease, by definition, severely reduces blood flow by vasospasm following a stimulus, such as extreme cold, stress, or smoking. This causes pallor, cyanosis, coldness, numbness, and tingling in the affected hand. Peripheral artery disease is a narrowing or occlusion of arteries outside the heart as a result of thickening of the intimal wall, caused primarily by atherosclerosis.
Buerger’s disease is an occlusive, chronic, inflammatory disorder of the arteries, veins, and surrounding nerves; decreased blood flow in the hands and feet leads to ischemia and pain initially, intermittent claudication, and decreased or absent peripheral pulses later. This may lead to infection, skin ulcers, and gangrene. Atherosclerosis is a type of hardening caused by the accumulation of fats and cholesterol that creates plaque in the arteries and reduces blood flow.
Raynaud’s disease is one of the processes where a formerly “male-only” medication is finding indications for use. Sildenafil (Viagra) can be used to treat this malady due to its vasodilatory effects. So be sure to ask both genders about the use Viagra before administration of nitroglycerin during epi-sodes of chest pain! Nitroglycerin can also be used on the fingertips to heal skin ulcers that can develop after multiple episodes.
Other vasodilators such as losartan (Cozaar) can also be used, as well as prostaglandins. Repeated episodes 5f Raynaud’s disease can cause gangrene. Other treatment options that can be help are to avoid smoking, decrease stress, exercise, and try to avoid rapid, extreme changes in temperature.
Question 36.
An unrestrained driver arrives in the emergency department after a rollover crash at 80 miles/hour. Which of the following are the most common causes of pulseless electrical activity (PEA) rhythm for this patient?
(a) Hypovolemia and hypoxia
(b) Thrombosis and toxins
(c) Hydrogen ion acidosis and hypothermia
(d) Hypoglycemia and syncope
Answer:
(a) Hypovolemia and hypoxia
Rationale:
Hypovolemia and hypoxia are the two most common underlying and potentially reversible causes of pulseless electrical activity (PEA) in the trauma patient. Uncontrolled bleeding and resultant hypovolemia may occur after a crash of an unrestrained driver at high speeds.
Although thrombosis, toxins, acidosis, and hypothermia are causes of pulseless electrical activity according to the American Heart Association, they are not necessarily implicated in a car crash at high speeds. Hypoglycemia and syncope are not common causes of pulseless electrical activity according to the American Heart Association.
Question 37.
Cardiogenic shock is the result of myocardial pump failure, decreased cardiac output (CO), and inadequate tissue perfusion, most commonly caused by myocardial infarction (MI) or ischemia. Signs and symptoms would include which of the following?
(a) Tachypnea, crackles, hypotension, and pale, clammy skin
(b) Dyspnea, stridor, wheezing, bronchospasm, erythema
(c) Bradycardia, hypotension, and warm, dry skin
(d) Tachycardia, altered level of consciousness, uncontrolled external bleeding
Answer:
(a) Tachypnea, crackles, hypotension, and pale, clammy skin
Rationale:
Most patients who present with cardiogenic shock do so in conjunction with a myocardial infarc-tion. Clinical manifestations of cardiogenic shock re-flect heart failure and inadequate tissue perfusion, that is, tachypnea, crackles, hypotension, and pale, clammy skin.
Anaphylactic shock from allergic reaction presents with dyspnea, stridor, wheezing, bronchospasm, and erythema. Neurogenic shock includes signs/symptoms of bradycardia, hypotension, and warm, dry skin. Tachycardia, altered level of consciousness, and uncontrolled external bleeding are signs of hypovolemic shock.
Circulating blood volume, from hemorrhage after trauma, extensive burns, or gastrointestinal bleeding. Cardiogenic shock results from ineffective perfusion caused by inadequate contractility of the heart from myocardial infarction, blunt cardiac injury, mitral valve insufficiency, dysrhythmias, and cardiac failure. Neurogenic shock results from injury to the spinal cord in the cervical or upper thoracic region.
Hypovolemic shock can occur for an absolute loss of volume as listed earlier with uncontrolled external bleeding and with a relative loss of fluid such as with bums and ascites. The fluid is present in the body, but it is not useful at this time. Third spacing can be another cause of hypovolemic shock.
Question 38.
Pericardial tamponade and tension pneumothorax are examples of which type of shock?
(a) Hypovolemic
(b) Cardiogenic
(c) Neurogenic
(d) Obstructive
Answer:
(d) Obstructive
Rationale:
Obstructive shock results from an inadequate circulating blood volume because of an obstruction or compression of the great veins, aorta, pulmonary arteries, or the heart itself. Cardiac tamponade compresses the heart so that the atria cannot fill, leading to a decrease in stroke volume and then circulating blood volume. Tension pneumothorax may displace the inferior vena cava and obstruct venous return to the right atrium, also decreasing circulating blood volume.
Hypovolemic shock is a decrease in circulating blood Volume from hemorrhage after trauma, extensive burns, or gastrointestinal bleeding. Cardiogenic shock results from ineffective prefusion caused by inadequate contractility of the heart from myocardial infraction, blunt cardiac injury, mitral valve insufficiency, dysrhythmias, and cardiac failure.
Question 39.
Which of the following is a true statement regarding the diagnosis of Spontaneous Coronary Artery Dissection (SCAD)?
(a) SCAD usually occurs in young women.
(b) SCAD is associated with atherosclerotic heart disease.
(c) SCAD usually occurs at rest.
(d) SCAD requires thrombolytic therapy.
Answer:
(a) SCAD usually occurs in young women.
Rationale:
SCAD is a disease process that usually occurs in young women—many times associated with peripartum women. However, this can present in women younger than age 50 and has been seen in postmenopausal women as well. SCAD stands for spontaneous coronary artery dissection and involves the tearing and separation of two layers of a coronary artery, which then develops a hematoma within the wall of the artery causing subsequent compression of the lumen.
Atherosclerosis is not present. The myocardial infarction occurs during episodes of extreme exercise, severe coughing/vomiting, or intense stress. It can also occur during the delivery process and has been seen with illicit drug use, such as cocaine and amphetamines. Thrombolytic therapy is contraindicated in the treatment of SCAD.
Yes! This one was a bit unfair, wasn’t it! Sorry ' about that! But now you know what SCAD is— an sudden cardiac death event for mostly young women that has recently come to the forefront.
Question 40.
A construction worker fell from the 10th floor at work. He arrives restless, with severe chest discomfort, hypotension, tachycardia, tachypnea, chest wall ecchymosis, and paraplegia. The emergency nurse anticipates which of the following plans for appropriate tests and subsequent intervention?
(a) Transesophageal echo, computed tomography (CT) scan, surgery
(b) Echocardiography, pericardiocentesis or pericardial window
(c) Chest radiograph, chest tube insertion, and closed chest drainage
(d) Chest radiograph, cover open wound, needle thoracentesis
Answer:
(a) Transesophageal echo, computed tomography (CT) scan, surgery
Rationale:
Motor vehicle crashes and falls are the most common causes of aortic injury. When the aorta is subjected to accelerating, decelerating, horizontal, or vertical traumatic forces, it may tear. Signs and symptoms include decreased level of consciousness, hypotension, tachycardia, tachypnea, chest wall ec- chymosis, and paraplegia. Paraplegia can occur due to the ischemia of the anterior spinal artery which is fed by branches of the aorta.
Diagnosis is suspected by the history of rapid deceleration forces and chest radiograph, and confirmed by arteriography, transesophageal echo, or computed tomography (CT) scan. Surgical intervention is indicated. Pericardial tamponade occurs most often with penetrating injury; classic signs are hypotension, distended neck veins, and muffled heart sounds, and is treated with pericardiocentesis or pericardial window.
Hemothorax is an accumulation of blood in the pleural space and signs/symptoms are dyspnea, tachypnea, chest pain, signs of shock, and decreased breath sounds on the affected side; treatment is chest tube insertion and closed chest drainage system. Tension pneumothorax would present with severe re-spiratory distress, diminished or absent breath sounds, hypotension, distended neck veins, and tracheal devia-tion. Treatment is immediately preparing for a needle thoracentesis.
Question 41.
Signs and symptoms of acute arterial occlusion include which of the following symptoms?
(a) Pain, pallor, pulselessness, paresthesia, paralysis
(b) Chest pain, tachycardia, tachypnea, elevated temperature
(c) Severe pain, blood pressure variation in arms, peripheral cyanosis
(d) Chest pain, dyspnea, nausea, diaphoresis, fatigue
Answer:
(a) Pain, pallor, pulselessness, paresthesia, paralysis
Rationale:
The signs1, of acute arterial occlusion are referred as the “5 Ps”: Pain, Pallor, Pulselessness, Paresthesia, and Paralysis. Chest pain, tachycardia, tachypnea, and elevated temperature may be seen in pericarditis. Severe pain, blood pressure variations in the arm and peripheral cyanosis are seen in aortic injuries. Chest pain, dyspnea, nausea, diaphoresis, and fatigue are seen in myocardial infarctions.
Question 42.
Long QT syndrome may precipitate which of the following?
(a) Torsade de pointes
(b) Atrial fibrillation
(c) Complete heart block
(d) Supraventricular tachycardia
Answer:
(a) Torsade de pointes
Rationale:
The long QT syndrome is a disorder of myocardial repolarization characterized by a prolonged QT interval on the electrocardiogram. This syndrome is associated with an increased risk of polymorphic ventricular tachycardia, a characteristic life-threatening cardiac dysrhythmia also known as torsades de pointes. The primary symptoms include palpitations, syncope, seizures, and sudden cardiac death. Atrial fibrillation, complete heart block, and supraventricular tachycardia are not precipitated by long QT syndrome.
Question 43.
Cardiac output (CO) is a product of which of the following formulas?
(a) Preload x Afterload
(b) Zone 1 x Zone 2
(c) Heart rate x Stroke volume
(d) (Age in years)/ 4 + 4
Answer:
(c) Heart rate x Stroke volume
Rationale:
Cardiac output (CO) is defined as a product of heart rate (HR) times stroke volume (SV) (CO = HR x SV). Preload is the passive stretching force of the ventricles during diastole; afterload is the resistance of the system that the ventricles must overcome to eject blood. Zone 1 and Zone 2 are anatomic landmarks of the neck and serve to identify structures in each zone. (Age in years) /4 + 4 is the formula to estimate pediatric endotracheal tube size.
Children have a fixed stroke volume. Because the stroke volume cannot change, they can only compensate by increasing their heart rates to augment their cardiac output. Tachycardia is often the first manifestation that something is wrong!
Question 44.
The emergency nurse identifies a condition that precipitates sudden cardiac death from blunt trauma to the left anterior chest wall that occurs predominantly in young, healthy, male athletes as:
(a) long QT syndrome.
(b) commotio cordis.
(c) point of maximal impulse.
(d) Kawasaki disease.
Answer:
(b) commotio cordis.
Rationale:
Commotio cordis causes sudden cardiac death from blunt trauma to the left anterior chest wall, usually from a thrown or batted ball, and occurs predominantly in young, male athletes. The cause of death is ventricular fibrillation due to the blow to the chest occurring during a critical point in the cardiac cycle.
The long QT syndrome (LQTS) is a disorder of myocardial repolarization characterized by a prolonged QT interval on the electrocardiogram and results from many things, including medications, electrolyte disorders, and congenital defects. The point of maximal impulse (PMI) is located in the fifth intercostal space at the midclavicular line.
PMI is where the cardiac impulse can be best palpated. The PMI may be displaced with increased right ventricular pressure (large right pleural effusion, right tension pneumothorax) and volume overload (heart failure). Kawasaki disease affects children younger than 5 years with vasculitis that affects medium and small arteries, notably the coronary arteries.
It is self-limiting and resolves within 1 to 2 months, although the mortality rate is 1 % to 2 %.
Advocate for automatic external defibrillators (AED) at school ball games! Commotio cordis (which means “commotion of the heart”) causes ventricular fibrillation in these young athletes. Immediate defibrillation can save their lives!
Question 45.
The most common cause of trauma-related cardiogenic shock is:
(a) uncontrolled external hemorrhage.
(b) pneumothorax and cardiac tamponade.
(c) injury or ischemia to cardiac tissue.
(d) spinal cord injury and loss of vascular tone.
Answer:
(c) injury or ischemia to cardiac tissue.
Rationale:
Blunt cardiac injury or ischemia to myocardial tissue or the conduction system could cause dysrhythmias and affect cardiac output. This is the most common cause of trauma-related cardiogenic shock, and goal-directed therapy includes inotropic support, anti-dysrhythmic medications, and correction of the underlying cause.
Uncontrolled external hemorrhage would result in hypovolemic shock. Pneumothorax and cardiac tamponade would cause obstructive shock. Spinal cord injury and loss of vascular tone would result in neurogenic shock.
Question 46.
All of the following would indicate reperfusion after thrombolytic therapy EXCEPT:
(a) relief of chest pain.
(b) onset of dysrhythmia.
(c) ST-segment normalization.
(d) Osborn wave.
Answer:
(d) Osborn wave.
Rationale:
An Osborn wave, also called a J wave, is an extra positive deflection between the QRS and the ST segment that accompanies hypothermia. It has nothing to do with cardiac reperfusion status post-thrombolytic administration. Patients who have successful reperfusion will have relief of chest pain and ST-segment normalization. The most common reperfusion dysrhythmia is accelerated idioventricular.
Question 47.
A patient arrives with a history of surgery 3 weeks ago and now has complaints of leg swelling, redness, warmth, and tenderness. The emergency nurse suspects which of the following?
(a) Post-thrombotic syndrome (PTS)
(b) Thromboangiitis obliterans (Buerger’s disease)
(c) Peripheral venous thrombosis
(d) Raynaud’s disease
Answer:
(c) Peripheral venous thrombosis
Rationale:
Peripheral venous thrombosis (also known as deep vein thrombosis or DVT) is an occlusion of a vein by a thrombus restricting blood outflow. The majority of DVTs involves the lower extremities and triggers include hypercoagulable/immobility states such as cancer, pregnancy, sepsis, surgery, and/or trauma.
Signs and symptoms vary, but include swelling, pain, tenderness, and warm, red, or discolored skin. Post-thrombotic syndrome is considered the most common long-term complication of a DVT and manifests up to 2 years later as chronic venous insufficiency varying from minor leg discomfort or swelling up to venous claudication and skin ulcerations.
Thromboangiitis obliterans or Buerger’s disease is an occlusive, chronic, inflammatory disorder of the arteries, veins, and surrounding nerves that triggers decreased blood flow in the hands and feet, resulting in ischemia and pain. Intermittent claudication and decreased or absent peripheral pulses lead to ulcers, and gangrene may develop.
Raynaud’s disease produces vasospasms that reduce blood flow to the arteries of the hands and feet in response to a trigger such as cold temperatures or smoking; symptoms are pallor and numbness/tingling that returns to normal after the stimulus is removed.
Lack of arterial blood flow results in a unique absence of hair on the toes of those who have this disease process!!
Question 48.
Diaphragmatic injury most often results from penetrating injury to the thorax or from high-speed deceleration forces common in motor vehicle crashes. With which of these signs and symptoms for diaphragmatic injury would the nurse have a high index of suspicion with that history?
(a) Initially asymptomatic, Kehr’s sign, dyspnea
(b) Impending doom, severe chest pain, severe dyspnea
(c) Increasing restlessness, tachycardia, tachypnea, hypoxia
(d) Anxiety, signs of shock, decreased breath sounds
Answer:
(a) Initially asymptomatic, Kehr’s sign, dyspnea
Rationale:
Signs and symptoms of diaphragmatic injury may not be evident initially. This rarely occurs alone and concurrent chest, abdomen, or long-bone fractures may be present; a high index of suspicion for diaphragmatic tear should be maintained along with these other injuries so that it is not missed. Abdominal contents may herniate into the chest cavity and cause compression of the lungs and mediastinum.
Although the patient may present with many signs, Kehr’s sign referred pain to the left shoulder or sub-clavicular area and dyspnea are symptoms associated with diaphragmatic injury. Impending doom, severe chest pain, and severe dyspnea are signs and symptoms of a tension pneumothorax. Increasing restlessness, tachycardia, tachypnea, and hypoxia may occur with a pulmonary contusion. Hemothorax signs and symptoms include al-tered level of consciousness along with signs of shock, hypotension, tachycardia, tachypnea, and decreased breath sounds on the affected side.
Question 49.
Injury to the aorta would require which of the following types of medications as an emergent intervention?
(a) Vasopressors to maintain systolic blood pressure greater than 100 mm Hg
(b) Beta-blockers to decrease heart rate and mean arterial pressure
(c) Antiarrythmics to prevent development of rhythm disturbances
(d) Antibiotics as prophylaxis for infectious processes
Answer:
(b) Beta-blockers to decrease heart rate and mean arterial pressure
Rationale:
Administration of beta-blockers will decrease heart rate and mean arterial pressure to decrease the risk of extending the injury and rupture. Calcium channel blockers and antihypertensive medications can also be used with a goal of maintaining systolic blood pressure around 100 mm Hg and a pulse rate of less than 100 beats/minute. Vasopressors to increase blood pressure would be contraindicated. Ahtiarryth- mics would not be necessary as prophylaxis for potential rhythm disturbances; and although antibiotics might be given, they would not be an emergent intervention.
Question 50.
Cardiac tamponade occurs when blood or fluid accumulates in the pericardial sac. The emergency nurse would anticipate assisting with which of the following interventions?
(a) Needle thoracentesis
(b) Chest tube insertion
(c) Pericardiocentesis
(d) Thoracotomy
Answer:
(c) Pericardiocentesis
Rationale:
The accumulation of blood or fluid in the mostly nondistensible pericardial sac compresses the heart and leads to a decrease in stroke volume and cardiac output, as well as decreased venous return and cardiac filling. A pericardiocentesis may be done to temporarily decompress the heart and allow for transfer to the operating room for definitive treatment.
A needle thoracentesis is treatment for a tension pneumothorax. Chest tube insertion is indicated for a loss of negative intrapleural pressure and subsequent collapse of a lung. Although a thoracotomy could be done to temporarily repair an open wound in the heart, a pericardiocentesis would be attempted first.
Question 51.
Treatment for a patient with venous thrombosis would include:
(a) calcium channel blockers or adrenergic blocking agents and nonnarcotic analgesia.
(b) inotropic support with dobutamine if 1 to 2 L of fluid fails to improve cardiac output
(c) heparin, low-molecular-weight heparin, analgesia, compression stockings.
(d) anti-inflammatory agents, antipyretics, antibiotics, and colchicine.
Answer:
(c) heparin, low-molecular-weight heparin, analgesia, compression stockings.
Rationale:
The mainstay of therapy for deep vein thrombosis (DVT) is anticoagulation. Folldwing initial anticoagulation, patients with DVT are anticoagulated further; the primary objective of anticoagulation is the prevention of further thrombosis and of early and late complications including further clot extension, acute pulmonary embolus, major bleeding, and death.
Calcium channel blockers or adrenergic blocking agents and non-narcotic analgesia is treatments for peripheral vascular disease. Inotropic support with dobutamine, if 1 to 2 L of fluid does not improve blood pressure, is treatment for right ventricular infarction. Anti-inflammatory agents, antipyretics, antibiotics, and colchicine are recommended treatments for pericarditis.
Question 52.
A patient arrives with a persistent narrow, regular tachyarrhythmia causing hypotension, altered mental- status, signs of shock, and ischemic chest discomfort. Which of the following is the recommended intervention?
(a) Synchronized cardioversion starting at 50 to 100 joules
(b) Vagal maneuvers, adenosine, beta-blocker, or calcium channel blocker
(c) Adenosine 6 mg rapid intravenous push, followed with a 20 mL normal saline flush
(d) Amiodarone 150 mg over 10 minutes, repeat as needed
Answer:
(a) Synchronized cardioversion starting at 50 to 100 joules
Rationale:
The management of an unstable narrow-complex tachycardia is immediate synchronized cardioversion at 50 to 100 joules. The American Heart Association cautions that if the symptoms are caused by the tachycardia, it is unstable and therefore requires immediate synchronized cardioversion. Vagal maneuvers, adenosine, beta-blockers, or calcium channel blockers are recommended for stable narrow-complex tachycardias. Amiodarone 150 mg over 10 minutes is indicated for stable wide-QRS tachycardia.
Question 53.
Which of the following is a true statement regarding synchronized shocks?
(a) Electrical shock will be delivered as soon as the operator pushes the shock button.
(b) Caution is needed because these shocks use higher energy levels.
(c) Used for an unstable patient when polymorphic ventricular fibrillation is present
(d) The actual shock avoids delivery during cardiac repolarization.
Answer:
(d) The actual shock avoids delivery during cardiac repolarization.
Rationale:
Synchronized cardioversion uses a sensor to deliver a shock that avoids delivery during cardiac repolarization, a period of vulnerability during which a shock can precipitate ventricular fibrillation. There will likely be a delay before the defibrillator delivers a synchronized shock because the device will look for the peak of the R wave in the QRS complex and avoid cardiac repolarization, represented by the T wave on the electrocardiogram (ECG).
With unsynchronized shocks, the shock will be delivered as soon as the operator pushes the shock button, and these shocks should use higher energy levels. Unsynchronized shocks are recommended when polymorphic ventricular fibrillation is present. Remember to read your questions very carefully. There is a huge difference between synchronized and unsynchronized shocks! Read every word in both the stem and the options! Also, when delivering synchronized shocks, the nurse must hold the buttons down until the shock is actually delivered.
Remember to read your questions very carefully. There is a huge difference between synchronized and unsynchronized shocks! Read every word in both the stem and the options! Also, when delivering synchronized shocks, the nurse must hold the buttons down until the shock is actually delivered.
Question 54.
When a post-cardiac arrest, comatose patient achieves return of spontaneous circulation (ROSC), which of the following would the emergency nurse anticipate performing immediately?
(a) Elevate the head of the bed.
(b) Maintain administration of 100% oxygen.
(c) Hyperventilate the patient via ET tube.
(d) Administer warm fluid boluses.
Answer:
(a) Elevate the head of the bed.
Rationale:
The American Heart Association recommends elevating the head of the bed to reduce cerebral edema, aspiration, and ventilator-associated pneumonia immediately after return of spontaneous circulation (ROSC).
Although 100% oxygen may have been used during the initial resuscitation, the lowest oxygen level needed to achieve an arterial oxygen saturation of 94% to 99% is recommended to avoid potential oxygen toxicity. Avoid-ance of hyperventilation is recommended by the American Heart Association standards. Targeted temperature management (TTM) is the only intervention demonstrated to improve neurologic recovery, and administration of cold fluids may be helpful for initial induction of hypothermia.
Question 55.
The emergency nurse recognizes which of the following as common causes or precipitants of supraventricular tachycardia?
(a) Digoxin, beta-blockers and calcium channel blockers
(b) Hypoxia, ischemia, heart failure, myocardial infarction, caffeine, and alcohol
(c) Hypertension, atherosclerosis, chronic cocaine use, and cardiac surgery
(d) Thrombosis, vasospasm, cocaine use, and chemotherapeutic agents
Answer:
(b) Hypoxia, ischemia, heart failure, myocardial infarction, caffeine, and alcohol
Rationale:
Common causes of supraventricular tachycardia include hypoxia, ischemia, heart failure, myocardial infarction, mitral valve prolapse, caffeine, alcohol, recreational drugs, and hyperthyroidism.
Digoxin, beta-blockers, calcium channel blockers, increased vagal tone on the sinoatrial node; and myocardial ischemia or infarction (depending on the vessel occluded) are common causes of sinus pause or sinus arrest. Hypertension, atherosclerosis, chronic cocaine use, and cardiac surgery may lead to aortic aneurysm. Thrombosis, vasospasm, cocaine use, and chemotherapeutic agents, as well as serotonin receptor agonists are risk factors for ST-elevation myocardial infarction.
Question 56.
Patients with cardiomyopathy may present with a past medical history of hypertension, angina, coronary artery disease, anemia, thyroid dysfunction, or breast cancer. The emergency nurse would expect to see which of the following symptoms?
(a) Chest pain, changes on electrocardiogram (ECG), and aphasia
(b) Fatigue, dyspnea on exertion, orthopnea, and edema
(c) Fever, night sweats, arthralgia, dyspnea, cough, pain
(d) Hypotension, clear lung sounds, increased jugular venous pressure
Answer:
(b) Fatigue, dyspnea on exertion, orthopnea, and edema
Rationale:
Fatigue, dyspnea on exertion, orthopnea, and edema are symptoms of dilated cardiomyopathy and reflect the left ventricle’s inability to pump blood effectively, causing reduced cardiac output. Common current or preexisting conditions include hypertension, angina, coronary artery disease, anemia, thyroid dysfunction, or breast cancer.
Hypertensive emergency presents with symptoms indicating organ damage such as ischemic stroke (with symptoms such as aphasia or loss of sensation or power of an extremity), encephalopathy, signs of myocardial infarction such as chest pain and changes on the electrocardiogram, or pulmonary edema.
Fever, night sweats, arthralgia, dyspnea, cough, and chest pain are symptoms of infective endocarditis. The clinical triad of hypotension, clear lung sounds, and increased jugular venous pressure are suggestive of right ventricular infarction and indicates the right ventricle’s inability to pump venous blood efficiently into the pulmonary vasculature, thereby reducing blood flow to the left ventricle.
Question 57.
The patient with a past medical history of atrial fibrillation arrives with complaints of sudden-onset severe lower limb pain and paresthesia. The emergency nurse palpates the limb and finds it pale, pulseless, and cold. Which of the following plans of care would the nurse expect the provider to prescribe?
(a) Smoking cessation, daily exercise, healthy diet, control blood pressure
(b) Compression leg garments, exercise therapy, prevent tissue injury
(c) Systemic anticoagulation, intravenous fluid therapy, intra-arterial thrombolysis
(d) Anticoagulation, ambulation, rest, and D-dimer and other laboratory studies
Answer:
(c) Systemic anticoagulation, intravenous fluid therapy, intra-arterial thrombolysis
Rationale:
In acute arterial occlusion, the objectives are to preserve limb and life, and prevent recurrent thrombosis or embolism. Anticoagulation may prevent clot extension, recurrent embolization, venous thrombosis, microthrombi distal to the obstruction, and reocclusion after reperfusion.
The vascular surgeon will choose between catheter-directed intra-arterial thrombolysis, percutaneous mechanical thrombectomy, and revascularization with percutaneous transluminal angioplasty or standard surgery for definitive treatment.
Lifestyle changes such as smoking cessation, daily exercise, health diet, and control of blood pressure would be important teaching before discharge, but not first-line treatment. Compression leg garments, exercise, and preventing tissue injury are treatments for chronic venous insufficiency. Anticoagulation, ambulation, rest, and D-dimer and other laboratory studies would be indicated for ve-nous thromboembolism treatment.
Question 58.
A patient presents with a narrow-complex tachycardia. Vital signs are as follows:
Blood pressure—110/82 mm Hg
Pulse—180 beats/minute
Respirations—20 breaths/minute
Pulse oximetry—95 % on room air
Temperature—98.6° F (37° C)
Which of the following initial outcomes will be expected with the successful use of the proper medication to treat this patient?
(a) Third-degree AV block
(b) Burst of atrial fibrillation
(c) Ventricular tachycardia
(d) Period of asystole
Answer:
(d) Period of asystole
Rationale:
The drug of choice for stable narrow-complex tachycardia is Adenocard (adenosine). This medication will cause a short period of asystole before conversion to normal sinus rhythm. The other options are not expected outcomes.
When giving Adenocard (adenosine), be sure to place the intravenous access in the AC space. Adenocard has a very short half-life and must be given extremely fast. 1\vo nurses are needed to push this medication, one to push the Adenocard quickly at the closest port and one to push 20-30 mL of normal saline behind it to get it into the circulation as soon as possible. Raise the arm and run normal saline fluids wide open after the administration.
Inform the patient (and any family members in the room) that there will be a short period of uncomfortableness. Be present for the patient. Hold the patient’s hand because this period of asystole is very distressing. Normal sinus rhythm should occur after a brief about 6 seconds period of time. Family members can become very upset if they are not prepared for the aystolic period.
Question 59.
The emergency nurse recognizes that cardiac resynchronization therapy (CRT) is/uses:
(a) an extracorporeal mechanical pump implanted to assist or replace the function of either the left or right ventricle.
(b) an electronic device that delivers low-voltage pacing pulses to relieve or prevent symptomatic bradycardia. .
(c) a biventricular pacemaker to treat the conduction defects that cause uncoordinated contraction of the ventricles.
(d) an electronic device that monitors heart rhythm and sends a shock to the heart if the rhythm detected is ventricular fibrillation.
Answer:
(c) a biventricular pacemaker to treat the conduction defects that cause uncoordinated contraction of the ventricles.
Rationale:
Cardiac resynchronization therapy (CRT) uses biventricular pacemakers to treat the conduction defects or ventricular dyssynchrony that cause uncoordinated contraction of the ventricles, thereby increasing cardiac output. Studies have shown that CRT is safe and effective, with patients demonstrating significant improvement in clinical symptoms, functional status, exercise capacity, quality of life, and reduction of sudden cardiac death. Pacemakers are electronic devices that deliver low-voltage electrical stimuli to relieve or prevent symptomatic bradycardia.
Ventricular assist devices (VADs) are extracorporeal mechanical pumps implanted to either assist or replace the function of either the right or left ventricle either as temporary placement as a bridge-to-transplant until a heart becomes available or as long-term support (destination therapy). An implantable cardioverter defibrillator (ICD) delivers shocks to terminate ventricular fibrillation or to convert ventricular tachycardia.
Question 60.
Current recommendations for acute coronary syndrome reperfusion therapy include which of the following?
(a) Door-to-needle time of 30 minutes for fibrinolytic therapy and door-to-balloon time of 90 minutes for percutaneous coronary perfusion.
(b) Fibrinolytics should be administered within 24 hours of presentation with qualifying electrocardiogram (ECG), if PCI is not available within 90 minutes of first medical contact.
(c) PCI can be offered to patients presenting to non-PCI-capable centers if PCI can be initiated within 3 hours of first medical contact.
(d) Patients who present more than 3 hours after the onset of symptoms or patients with ST-segment depression are ineligible for fibrinolytics.
Answer:
(a) Door-to-needle time of 30 minutes for fibrinolytic therapy and door-to-balloon time of 90 minutes for percutaneous coronary perfusion.
Rationale:
The standard of care, initially set by the American Heart Association, recommends a door-to-needle time of 30 minutes for fibrinolytic therapy and door-to-balloon time of 90 minutes for percutaneous coronary perfusion in recognition that reperfusion therapy reduces mortality and saves heart muscle; the shorter the time to reperfusion, the greater the benefit.
A 47% reduction in mortality was noted when fibrinolytic therapy was provided in the first hour after onset of symptoms. The time limit for fibrinolytic administration is onset of symptoms within 12 hours, not 24. Percutaneous coronary intervention (PCI) can be offered to patients presenting to non-PCI-capable centers if PCI can be initiated within 2 hours of first medical contact, not 3 hours. Fibrinolytics are generally not recommended for patients presenting more than 12 hours after onset of symptoms.
Remember that troponin stays elevated for a longer period of time up to 10 days when considering the cardiac biomarkers. CK-MB (creatinine kinase-muscle/brain) is also used, but troponin has greater specificity and sensitivity.
Question 61.
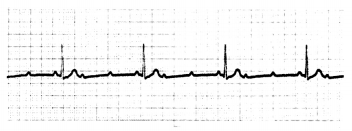
Which of the following identifies the significance of the above rhythm?
(a) Hyperkalemia; tall, peaked T waves; early hyperacute sign
(b) T-wave inversion, ischemia, T wave appears deep and symmetrical
(c) Injury pattern, elevation above the isoelectric line indicates acuteness of injury
(d) Pathologic Q wave, appears within 24 hours of infarct, may remain permanent
Answer:
(c) Injury pattern, elevation above the isoelectric line indicates acuteness of injury
Rationale:
ST elevation myocardial infarction (STEMI) is characterized by ST-segment elevation in two or more contiguous leads and threshold values of J-point elevation greater than 2 mm in leads V2 and V3 and 1 mm or more in all other leads. This is ST elevation, not peaked or inverted waves; tall T waves can signify hyperkalemia, cerebrovascular injury, and left ventricular volume loads resulting from mitral or aortic regurgitation.
T-wave inversion can have various causes including ischemia or evolving myocardial infarction or cerebrovascular accidents. Pathologic Q waves appear within 24 hours of infarction at greater than 0.04 seconds in duration or greater than 25% of the R wave in depth. These indicate necrosis in the heart muscle and can be permanent.
Question 62.
Which of the following would be a red flag regarding the potential for long QT syndrome in youth?
(a) Dysrhythmias associated with rest
(b) Difficulty with palpating radial pulses
(c) Sudden syncope with exercise
(d) Sudden death during sleep
Answer:
(c) Sudden syncope with exercise
Rationale:
An abrupt and transient loss of consciousness might indicate long QT syndrome in young people.
Symptoms in the young athletes that are suggestive of QT prolongation include exercise-induced palpitations, chest pains, syncope, and dizziness. Intense exercise can trigger arrhythmogenic sudden cardiac death (SCD) in student-athletes with occult cardiac disease. Risk assessment guidelines from the American Heart Association and American College of Cardiology advocate the use of a 14-point pre-participation history and physical examination, including eliciting information regarding unexplained syncope or near-syncope. Arteriosclerotic changes in the aorta may make it difficult to palpate pulses in the aging population but not in the young athlete.
Question 63.
A pulsus paradoxus greater than 12 mm Hg in a patient with a large pericardial effusion predicts cardiac tamponade with sensitivity of 98 % and specificity of 83 %. Which of the following is a definition of pulsus paradoxus?
(a) Beat-to-beat variability of the pulse amplitude on waveform
(b) Fall in systolic pressure of greater than 10 mm Hg with inspiration
(c) A difference of less than 10 mm Hg between simultaneous blood pressure measurement in both arms
(d) A fall in blood pressure of more than 20 mm Hg systolic when moving from supine to standing position
Answer:
(b) Fall in systolic pressure of greater than 10 mm Hg with inspiration
Rationale:
Pulsus paradoxus, a fall in systolic pressure of more than 10 mm Hg during inspiration, is considered pathologic and caused by decreased venous return. Pulses paradoxus is detected by noting the difference between the systolic blood pressure at which the Korotkoff sounds are first heard during expiration and the systolic blood pressure at which the Korotkoff sounds are heard with each beat, independent of the respiratory phase. Pulsus paradoxus is a sign of pericardial tamponade, but it also may be present with pulmonary embolus, hemorrhagic shock, severe obstructive lung disease, or tension pneumothorax.
Pulsus alternans is defined by the beat-to-beat variability of the pulse amplitude and occurs in severe aortic regurgitation, hypertension, and hypovolemic states. A difference of less than 10 mm Hg between simultaneous BP measurements in both arms is a normal finding. A fall in blood pressure of more than 20 mm Hg systolic when moving from supine to standing position is the definition of orthostatic hypotension and may occur in patients with diabetes and Parkinson’s disease and depends on age, hydration, medications, food, conditioning, and ambient temperature and humidity.
Question 64.
A patient arrives in the emergency department with complaints of a viral infection within the past 2 weeks, now complaining of fever, fatigue, dyspnea, chest pain, and malaise. Electrocardiogram (ECG) reveals sinus tachycardia with decreased QRS amplitude and transitory Q-wave development. Vital signs are as follows:
Blood pressure —90/60 mm Hg
Heart rate—135 beats/minute
Respiratory rate—28 breaths/minute
Pulse oximetry—95% on room air
Temperature—100.4° F (38.0° C)
Which of the following disease processes should the emergency nurse suspect?
(a) ST-segment myocardial infarction
(b) Myocarditis
(c) Pericarditis
(d) Endocarditis
Answer:
(b) Myocarditis
Rationale:
Myocarditis is characterized by inflammation and destruction of myocardial tissue with viruses being the predominant cause in North America. Fever, myalgias, headache, sinus tachycardia, and electrocardiogram (ECG) changes including nonspecific ST-T-wave changes are common symptoms.
The most common symptom of acute pericarditis is sharp or stabbing precordial or retrosternal chest pain. Referral of pain to the left trapezoidal ridge is a distinguishing feature. Chest pain may be aggravated by inspiration or movement and relieved when sitting up and leaning forward.
A pericardial friction rub is the most common and important physical finding in pericarditis. Bacteria are the predominant cause of endocarditis and most cases occur with a predisposing identifiable cardiac structural abnormality, prosthetic valve, or a recognized risk factor such as intravenous drug use, intravascular devices, poor dental hygiene, and hemodialysis or human immunodeficiency virus (HIV).
Tachycardia that is disproportionate to the degree of fever should alert the clinician to the possibility of myocarditis. In severe cases, heart failure can develop. Treatment is supportive, although antibiotics are needed for myocarditis complicating rheumatic fever, diphtheria, or meningococcemia.
Question 65.
Ninety percent of acute aortic dissections occur in the ascending aorta. The emergency nurse knows that the most important predisposing risk factor for this process is which of the following?
(a) Trauma
(b) Cardiac surgery
(c) Hypertension
(d) Cocaine use
Answer:
(c) Hypertension
Rationale:
Hypertension is the primary risk factor for acute aortic dissections, seen in 72% of cases. Patients tend to be 60- to 80-year-old men and were significantly more likely to have atherosclerosis. The incidence of aortic injury is estimated between 1.5% and 2 % of patients who sustain blunt thoracic trauma.
Aortic instrumentation or cardiac surgery can be complicated by aortic dissection, but is reported at 2 % of patients. Cocaine use, which may cause a transient hypertension due to catecholamine release, accounted for 37% of dis-sections in a report of an inner-city population.
Question 66.
Labetalol (Normodyne) would be contraindicated in all of the following patients EXCEPT:
(a) a 68-year-old with congestive heart failure.
(b) a 45-year-old with blood pressure of 210/118 mm Hg.
(c) an 82-year-old with heart rate of 40 beats/minute.
(d) a 28-year-old with recent asthmatic attack.
Answer:
(b) a 45-year-old with blood pressure of 210/118 mm Hg.
Rationale:
Labetalol (Normodyne) is a beta-blocker that is used to decrease the blood pressure in hypertensive disorders. It is contraindicated in patients with heart failure, bradycardias, and reactive airway disease.
Some medications were meant to be given slowly. Be careful with medications that have the potential to significantly lower blood pressure and pulse rates. It is also a good practice to take vital signs during the process of administering medications such as labetalol (Normodyne) and diltiazem (Cardizem) so that every effort is taken to document that proper precautions were taken during the administration.
Question 67.
Which of the following is a potential complication of nitroprusside (Nipride) administration?
(a) Hypertension
(b) Asthma attack
(c) Restless leg syndrome
(d) Cyanide toxicity
Answer:
(d) Cyanide toxicity
Rationale:
The administration of nitroprusside (Ni-pride) can cause cyanide toxicity. Nipride itself contains five cyanide groups and a nitrous oxide group. When placed into contact with blood, it can react with hemoglobin to produce thiocyanate and cyanide. This usually happens with high doses or prolonged use. Nitroprusside works through the process of vasodilation to reduce blood pressure and is therefore used in hypertensive situations that require immediate attention. Nitroprusside does not have any association with asthma or restless leg syndrome.
Question 68.
Which of the following medications should be avoided in a patient with a right ventricular myocardial infarction?
(a) Opioids, diuretics
(b) Aspirin, clopidogrel (Plavix)
(c) Atropine, statin therapy
(d) Dopamine (Intropin), dobutamine
Answer:
(a) Opioids, diuretics
Rationale:
Opioids and diuretics as well as nitrates should be avoided with a right ventricular infarction because of their preload reducing effects which will reduce cardiac output further and result in hypotension. Instead, these patients should be treated with volume loading with boluses of fluid and, if that fails, inotropic support with dobutamine. Aspirin, clopidogrel, and statin therapy should be given to these patients and atropine, dopamine, or dobutamine if needed.
Question 69.
Which of the following statements made by a patient being discharged with a diagnosis of Raynaud’s phenomenon would indicate that the discharge instructions were understood?
(a) “I will wear gloves to keep warm and. work hard on stopping smoking.”
(b) “I will keep my arm elevated on a pillow and apply ice to my hand.”
(c) “I have an elastic bandage at home that I can wear when I am on the computer.”
(d) “I will drink plenty of fluids and take aspirin for the pain.”
Answer:
(a) “I will wear gloves to keep warm and. work hard on stopping smoking.”
Rationale:
Raynaud’s phenomenon is a circulatory disease of the arteries that severely reduces blood flow as the result of episodic intense vasospasm of the digits in response to extreme cold, emotional stress, and/or smoking. Treatment is aimed at decreasing pain and vasospastic events. The patient should be advised to keep warm, wear gloves, not smoke, and avoid cold medicines and diet pills due to their vasoconstrictive effects. Elevating the arm and applying ice would worsen the vasoconstriction. Wrist splints or applying an elastic bandage would not help and may increase vasoconstriction. Fluids and aspirin would not help.
Question 70.
A patient arrives in the emergency department with complaints of chest pain for the past 30 minutes after mowing the lawn. He also reports nausea, dyspnea, and dizziness. The 12-lead electrocardiogram shows greater than 2 mm ST elevation in leads Vu V2, and V3. This indicates injury to which of the following areas of the heart? (a) Inferior
(b) Lateral
(c) Anterior
(d) Posterior
Answer:
(c) Anterior
Rationale:
ST-segment elevation in leads V„ V2, and V3 are indicative of damage to the anterior aspect of the heart. These leads look directly at the anterior heart wall. Inferior myocardial infarctions are noted with changes in leads II, III, and AVF. The lateral leads are I, AVL, V5, and V6. Posterior Mis are noted as reciprocal changes in the anterior leads—V, and V2. To see the ST- segment elevation changes in this MI, posterior leads— V7, V8, and V9 would need to be performed.
Posterior leads are accomplished by taking leads V4, V5, and V6 and placing them on the left posterior aspect to create V7, V8, and V9. These should be on the same plane as the original V6. V7 is placed at the posterior axillary line, V8 at the tip of the scapula, and V9 at the left spinal border. Relabel these leads as the graph paper exits the machine— V4 is now V7; V5 is now Vs; V6 is now V9. ST-segment elevation should now be seen in these leads if a posterior MI is in progress.
Question 71.
Which of the following would be the proper lead placement to definitively diagnosis a right ventricular infarct?
(a) Fourth intercostal space left sternal border
(b) Fifth intercostal space right midclavicular line
(c) Fifth intercostal space posterior axillary line
(d) Fourth intercostal space right sternal border
Answer:
(b) Fifth intercostal space right midclavicular line
Rationale:
A right-sided electrocardiogram (ECG) is performed when concern is present for a right ventricular infarct. V4R to V6R are the leads that will show the ST-segment elevation, with V4R being the best. The lead placement for V4R is in the fifth intercostal space at the right midclavicular line. The left side is mimicked on the right side of the chest. Lead placement in the fourth intercostal space at the left sternal border and at the right sternal border would be proper placement for V! and V2. A lead placed at the fifth intercostal space posterior axillary line would be correct for the posterior lead, V7.
Be sure to label the ECG as “right-sided" and label the leads as V,R, V2R, V3R, V4R, VSR, and VJl. Often, only V4R is done because this lead demonstrates the ST elevation best.
Question 72.
Which of the following is NOT a cardiovascular consequence of cocaine use?
(a) Acute myocardial infarction
(b) Aortic dissection
(c) Hypertensive crisis
(d) Pericarditis
Answer:
(d) Pericarditis
Rationale:
Pericarditis occurs due to a viral infection that may have started as a respiratory infection. The clinical cardiovascular consequences of cocaine use include hypertensive crises, acute myocardial infarction (AMI), aortic dissection, myocarditis, and stroke. Cocaine is a powerful sympathomimetic that increases heart rate, mean arterial pressure, and left ventricular contractility by stimulation of both alpha- and beta-adrenergic receptors. Cocaine use causes coronary artery vasospasm and also causes vasoconstriction, which enhances the development of hypertension.
Question 73.
Which of the following is the most common and concerning electrolyte imbalance associated with digoxin toxicity?
(a) Hyponatremia
(b) Hypercalcemia
(c) Hypomagnesemia
(d) Hyperkalemia
Answer:
(d) Hyperkalemia
Rationale:
The most common and concerning electrolyte abnormality associated with acute digoxin toxicity is hyperkalemia that occurs due to the binding affinity for digoxin on the Na/K pump site on each cell. Hyponatremia, hypercalcemia, and hypomagnesemia are not electrolyte disturbances that occur with digoxin toxicity.
Digoxin has been shown to reduce mortality and hospitalization in older patients with heart failure; however, the therapeutic window is narrowed in older adults. Because of decreases in renal elimination, glomerular filtration rate, and body mass, lower doses of digoxin are generally required. The therapeutic serum concentration of digoxin is 0.5 to 0.9 ng/mL.
Question 74.
Which of the following should be potentially withheld in an infant with a patent ductus arteriosus?
(a) Formula
(b) Breast milk
(c) Warmth
(d) Oxygen
Answer:
(d) Oxygen
Rationale:
An infant with a patent ductus arteriosus can become seriously harmed with the application of high-dose oxygen in the presence of a low pulse oximetry reading. Oxygen can close the ductus arteriosus before the required surgery has been performed. These infants become “ductal dependent” and hyperoxia can create a deadly situation. Formula and breast milk have no bearing on a patent ductus arteriosus, and all babies should be kept warm.
Always listen to parents of infants who have chronic illness or congenital anomalies! When caring for infants with congenital heart defects, ask the parents: “What is normal for your baby?" They will know!
A baby with a patent ductus arteriosus may have a normal pulse oximetry reading in the 60s or 70s. If a patent ductus arteriosus becomes closed prematurely, the medication to use is PSE or prostaglandin E. This will dilate the ductus open and, reestablish the patency. This is given as a continuous infusion and should not be piggybacked into another line. Maximal effects will be seen within 30 minutes.
Question 75.
Which of the following is the most common area of rupture in traumatic cardiac injury?
(a) Aortic arch
(b) Pulmonary vein
(c) Ligamentum arteriosum
(d) Right coronary artery
Answer:
(c) Ligamentum arteriosum
Rationale:
Traumatic thoracic injury can cause aortic injury and the tear most commonly occurs at the ligamentum arteriosum (80% to 90%). This is a band of tissue that forms about 3 weeks after birth and is a vestige of the fetal ductus arteriosus. It connects the aorta to the pulmonary artery and when torn has usually fatal outcomes. If a complete tear does not occur and the adventitial layer of the vessel (the outermost layer) remains intact, an aneurysm can develop.